Abstract
Background
The thiazolidinedione (TZD) class of oral antidiabetic agents are used to treat type 2 diabetes mellitus (DM). This meta-analysis aimed to understand the protective effect of TZD on Parkinson’s disease (PD) in people with diabetes.
Method
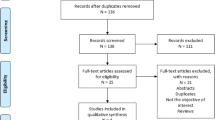
A literature search was performed in PubMed, Embase, and Cochrane central from inception to until 30 September 2019. We included all real-world evidence studies assessing the use of TZD class of drugs and the risk of PD in people with diabetes. Quality of the studies was evaluated using the Newcastle-Ottawa scale. The primary outcome was the pooled hazard ratio (HR) of PD among type 2 DM TZD users as compared with TZD non-users in people with diabetes. The secondary outcome was the HR of PD among type 2 DM TZD users as compared with non-users (include both diabetic and nondiabetic population). Meta-analysis was performed using RevMan software.
Results
Out of five studies selected for inclusion, four studies fulfilled the criteria for primary outcomes. The participants’ mean age and follow-up duration were 66.23 ± 9.59 years and 5.25 years (2.97–7.9 years), respectively. There was a significant reduction in the risk of PD (pooled adjusted HR of 0.81 [95% CI 0.70–0.93, p = 0.004]) in TZD users compared with non-TZD users in people with diabetes. A significant protective effect of TZD was observed in Caucasian population (3 studies) (HR 0.78 (95% CI 0.66–0.92), p = 0.003).
Conclusion
This meta-analysis demonstrates a potential neuroprotective effect of TZD for PD risk in the population with DM.




Similar content being viewed by others
References
Hirsch L, Jette N, Frolkis A, Steeves T, Pringsheim T (2016) The incidence of Parkinson’s disease: a systematic review and meta-analysis. Neuroepidemiology 46:292–300
Hobson P, Meara J (2018) Mortality and quality of death certification in a cohort of patients with Parkinson’s disease and matched controls in North Wales, UK at 18 years: a community-based cohort study. BMJ Open 8:e018969
Statistics. Parkinson’s Foundation. Available at: https://www.parkinson.org/Understanding-Parkinsons/Statistics. Accessed on 10th July 2019
Moisan F, Kab S, Mohamed F, Canonico M, le Guern M, Quintin C, Carcaillon L, Nicolau J, Duport N, Singh-Manoux A, Boussac-Zarebska M, Elbaz A (2016) Parkinson disease male-to-female ratios increase with age: French nationwide study and meta-analysis. J Neurol Neurosurg Psychiatry 87:952–957
Johnson SJ, Diener MD, Kaltenboeck A, Birnbaum HG, Siderowf AD (2013) An economic model of Parkinson’s disease: implications for slowing progression in the United States. Mov Disord 28:319–326
Kowal SL, Dall TM, Chakrabarti R, Storm MV, Jain A (2013) The current and projected economic burden of Parkinson’s disease in the United States. Mov Disord 28:311–318
Velikova G, Valderas JM, Potter C et al (2017) Proceedings of Patient Reported Outcome Measure’s (PROMs) Conference Oxford 2017: advances in patient reported outcomes research. Health Qual Life Outcomes 15:185
Breidert T, Callebert J, Heneka MT, Landreth G, Launay JM, Hirsch EC (2002) Protective action of the peroxisome proliferator-activated receptor-gamma agonist pioglitazone in a mouse model of Parkinson’s disease. J Neurochem 82:615–624
Dehmer T, Heneka MT, Sastre M, Dichgans J, Schulz JB (2004) Protection by pioglitazone in the MPTP model of Parkinson’s disease correlates with I kappa B alpha induction and block of NF kappa B and iNOS activation. J Neurochem 88:494–501
Hunter RL, Choi DY, Ross SA, Bing G (2008) Protective properties afforded by pioglitazone against intrastriatal LPS in Sprague-Dawley rats. Neurosci Lett 432:198–201
Swanson CR, Joers V, Bondarenko V, Brunner K, Simmons HA, Ziegler TE, Kemnitz JW, Johnson JA, Emborg ME (2011) The PPAR-gamma agonist pioglitazone modulates inflammation and induces neuroprotection in parkinsonian monkeys. J Neuroinflammation 8:91
Brakedal B, Flønes I, Reiter SF, Torkildsen Ø, Dölle C, Assmus J, Haugarvoll K, Tzoulis C (2017) Glitazone use associated with reduced risk of Parkinson’s disease. Mov Disord 32:1594–1599
Connolly JG, Bykov K, Gagne JJ (2015) Thiazolidinediones and Parkinson disease: a cohort study. Am J Epidemiol 182:936–944
Kmietowicz Z (2015) Glitazones are associated with reduced risk of Parkinson’s disease. Bmj 351:h3949
Lin H-L, Lin H-C, Tseng Y-F, Chao JC-J, Hsu C-Y (2018) Association of thiazolidinedione with a lower risk of Parkinson’s disease in a population with newly-diagnosed diabetes mellitus. Ann Med 50:430–436
Brauer R, Bhaskaran K, Chaturvedi N, Dexter DT, Smeeth L, Douglas I (2015) Glitazone treatment and incidence of Parkinson’s disease among people with diabetes: a retrospective cohort study. PLoS Med 12:e1001854
Wu H-F, Kao L-T, Shih J-H et al (2018) Pioglitazone use and Parkinson’s disease: a retrospective cohort study in Taiwan. BMJ Open 8:e023302
NINDS Exploratory Trials in Parkinson Disease (NET‐PD) FS‐ZONE Investigators (2015) Pioglitazone in early Parkinson’s disease: a phase 2, multicentre, double-blind, randomised trial. The Lancet Neurology 14:795–803
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151:264–269
Hussain S, Singh A, Rahman SO, Habib A, Najmi AK (2018) Calcium channel blocker use reduces incident dementia risk in elderly hypertensive patients: a meta-analysis of prospective studies. Neurosci Lett 671:120–127
Singh A, Hussain S, Najmi AK (2017) Number of studies, heterogeneity, generalisability, and the choice of method for meta-analysis. J Neurol Sci 381:347
Carta AR, Simuni T (2015) Thiazolidinediones under preclinical and early clinical development for the treatment of Parkinson’s disease. Expert Opin Investig Drugs 24:219–227
Ghosh A, Tyson T, George S et al (2016) Mitochondrial pyruvate carrier regulates autophagy, inflammation, and neurodegeneration in experimental models of Parkinson’s disease. Science Translational Medicine 8:368ra174
Wang Y, Zhao W, Li G et al (2017) Neuroprotective effect and mechanism of thiazolidinedione on dopaminergic neurons in vivo and in vitro in Parkinson’s disease. PPAR Res 2017:4089214
Schernhammer E, Hansen J, Rugbjerg K, Wermuth L, Ritz B (2011) Diabetes and the risk of developing Parkinson’s disease in Denmark. Diabetes Care 34:1102–1108
Santiago JA, Potashkin JA (2013) Shared dysregulated pathways lead to Parkinson’s disease and diabetes. Trends Mol Med 19:176–186
Aviles-Olmos I, Limousin P, Lees A, Foltynie T (2013) Parkinson’s disease, insulin resistance and novel agents of neuroprotection. Brain 136:374–384
Athauda D, Foltynie T (2016) Insulin resistance and Parkinson’s disease: a new target for disease modification? Progress in Neurobiology 145–146:98–120
Hogg E, Athreya K, Basile C, Tan EE, Kaminski J, Tagliati M (2018) High prevalence of undiagnosed insulin resistance in non-diabetic subjects with Parkinson’s disease. J Park Dis 8:259–265
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 29 kb)
Rights and permissions
About this article
Cite this article
Hussain, S., Singh, A., Baxi, H. et al. Thiazolidinedione use is associated with reduced risk of Parkinson’s disease in patients with diabetes: a meta-analysis of real-world evidence. Neurol Sci 41, 3697–3703 (2020). https://doi.org/10.1007/s10072-020-04494-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04494-3