Abstract
Purpose
In this study, kinetic parameters of the cellular proliferation tracer 18F-3′-deoxy-3′-fluoro-l-thymidine (FLT) and the amino acid probe 3,4-dihydroxy-6-18F-fluoro-l-phenylalanine (FDOPA) were measured before and early after the start of therapy, and were used to predict the overall survival (OS) of patients with recurrent malignant glioma using multiple linear regression (MLR) analysis.
Methods
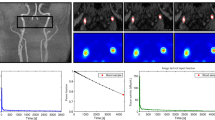
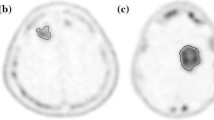
High-grade recurrent brain tumors in 21 patients (11 men and 10 women, age range 26 – 76 years) were investigated. Each patient had three dynamic PET studies with each probe: at baseline and after 2 and 6 weeks from the start of treatment. Treatment consisted of biweekly cycles of bevacizumab (an angiogenesis inhibitor) and irinotecan (a chemotherapeutic agent). For each study, about 3.5 mCi of FLT (or FDOPA) was administered intravenously and dynamic PET images were acquired for 1 h (or 35 min for FDOPA). A total of 126 PET scans were analyzed. A three-compartment, two-tissue model was applied to estimate tumor FLT and FDOPA kinetic rate constants using a metabolite- and partial volume-corrected input function. MLR analysis was used to model OS as a function of FLT and FDOPA kinetic parameters for each of the three studies as well as their relative changes between studies. An exhaustive search of MLR models using three or fewer predictor variables was performed to find the best models.
Results
Kinetic parameters from FLT were more predictive of OS than those from FDOPA. The three-predictor MLR model derived using information from both probes (adjusted R 2 = 0.83) fitted the OS data better than that derived using information from FDOPA alone (adjusted R 2 = 0.41), but was only marginally different from that derived using information from FLT alone (adjusted R 2 = 0.82). Standardized uptake values (either from FLT alone, FDOPA alone, or both together) gave inferior predictive results (best adjusted R 2 = 0.25).
Conclusion
For recurrent malignant glioma treated with bevacizumab and irinotecan, FLT kinetic parameters obtained early after the start of treatment (absolute values and their associated changes) can provide sufficient information to predict OS with reasonable confidence using MLR. The slight increase in accuracy for predicting OS with a combination of FLT and FDOPA PET information may not warrant the additional acquisition of FDOPA PET for therapy monitoring in patients with recurrent glioma.





Similar content being viewed by others
References
CBTRUS. CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2005–2009. Hinsdale, IL: Central Brain Tumor Registry of the United States; 2013. www.cbtrus.org. (2013)
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29.
Foltz G. New hope for battling brain cancer. Sci Am Mind. 2010;21:50–7.
Clarke JL, Chang SM. Neuroimaging: diagnosis and response assessment in glioblastoma. Cancer J. 2012;18:26–31.
Schwarzenberg J, Czernin J, Cloughesy TF, Ellingson BM, Pope WB, Geist C, et al. 3′-deoxy-3′-18F-fluorothymidine PET and MRI for early survival predictions in patients with recurrent malignant glioma treated with bevacizumab. J Nucl Med. 2012;53:29–36.
Walter F, Cloughesy T, Walter MA, Lai A, Nghiemphu P, Wagle N, et al. Impact of 3,4-dihydroxy-6-18F-fluoro-L-phenylalanine PET/CT on managing patients with brain tumors: the referring physician’s perspective. J Nucl Med. 2012;53:393–8.
Clarke JL, Chang S. Pseudoprogression and pseudoresponse: challenges in brain tumor imaging. Curr Neurol Neurosci Rep. 2009;9:241–6.
Phelps ME. PET: molecular imaging and its biological applications. New York: Springer; 2004.
Phelps ME, Mazziotta JC, Schelbert HR. Positron emission tomography and autoradiography: principles and applications for the brain and heart. New York: Raven; 1986.
Phelps ME. PET: the merging of biology and imaging into molecular imaging. J Nucl Med. 2000;41:661–81.
Phelps ME. Positron emission tomography provides molecular imaging of biological processes. Proc Natl Acad Sci U S A. 2000;97:9226–33.
Phelps ME, Huang SC, Hoffman EJ, Selin C, Sokoloff L, Kuhl DE. Tomographic measurement of local cerebral glucose metabolic rate in humans with (F-18)2-fluoro-2-deoxy-D-glucose: validation of method. Ann Neurol. 1979;6:371–88.
Phelps ME, Mazziotta JC. Positron emission tomography: human brain function and biochemistry. Science. 1985;228:799–809.
Phelps ME, Schelbert HR, Mazziotta JC. Positron computed tomography for studies of myocardial and cerebral function. Ann Intern Med. 1983;98:339–59.
Weissleder R. Molecular imaging: principles and practice. Shelton: People’s Medical Publishing House; 2009.
Huang SC, Phelps ME, Hoffman EJ, Sideris K, Selin CJ, Kuhl DE. Noninvasive determination of local cerebral metabolic rate of glucose in man. Am J Physiol. 1980;238:E69–82.
Huang SC. Role of kinetic modeling in biomedical imaging. J Med Sci. 2008;28:57–63.
Shields AF, Grierson JR, Dohmen BM, Machulla HJ, Stayanoff JC, Lawhorn-Crews JM, et al. Imaging proliferation in vivo with [F-18]FLT and positron emission tomography. Nat Med. 1998;4:1334–6.
Heiss WD, Wienhard K, Wagner R, Lanfermann H, Thiel A, Herholz K, et al. F-Dopa as an amino acid tracer to detect brain tumors. J Nucl Med. 1996;37:1180–2.
Herholz K, Langen KJ, Schiepers C, Mountz JM. Brain tumors. Semin Nucl Med. 2012;42:356–70.
Heiss WD, Raab P, Lanfermann H. Multimodality assessment of brain tumors and tumor recurrence. J Nucl Med. 2011;52:1585–600.
Olivero WC, Dulebohn SC, Lister JR. The use of PET in evaluating patients with primary brain tumours: is it useful? J Neurol Neurosurg Psychiatry. 1995;58:250–2.
Ricci PE, Karis JP, Heiserman JE, Fram EK, Bice AN, Drayer BP. Differentiating recurrent tumor from radiation necrosis: time for re-evaluation of positron emission tomography? AJNR Am J Neuroradiol. 1998;19:407–13.
Chen W. Clinical applications of PET in brain tumors. J Nucl Med. 2007;48:1468–81.
Bading JR, Shields AF. Imaging of cell proliferation: status and prospects. J Nucl Med. 2008;49 Suppl 2:64S–80S.
Chen W, Cloughesy T, Kamdar N, Satyamurthy N, Bergsneider M, Liau L, et al. Imaging proliferation in brain tumors with 18F-FLT PET: comparison with 18F-FDG. J Nucl Med. 2005;46:945–52.
Fueger BJ, Czernin J, Cloughesy T, Silverman DH, Geist CL, Walter MA, et al. Correlation of 6-18F-fluoro-L-dopa PET uptake with proliferation and tumor grade in newly diagnosed and recurrent gliomas. J Nucl Med. 2010;51:1532–8.
Chen W, Silverman DH, Delaloye S, Czernin J, Kamdar N, Pope W, et al. 18F-FDOPA PET imaging of brain tumors: comparison study with 18F-FDG PET and evaluation of diagnostic accuracy. J Nucl Med. 2006;47:904–11.
Wardak M, Schiepers C, Dahlbom M, Cloughesy T, Chen W, Satyamurthy N, et al. Discriminant analysis of 18F-fluorothymidine kinetic parameters to predict survival in patients with recurrent high-grade glioma. Clin Cancer Res. 2011;17:6553–62.
Zdanowicz MM. Concepts in pharmacogenomics. Bethesda: American Society of Health-System Pharmacists; 2010.
Walsh JC, Padgett HC, Ysaguirre T. Method for preparing radiolabeled thymidine having low chromophoric byproducts. Siemens Medical Solutions USA, Inc.; 2008
Namavari M, Bishop A, Satyamurthy N, Bida G, Barrio JR. Regioselective radiofluorodestannylation with [18F]F2 and [18F]CH3COOF: a high yield synthesis of 6-[18F]fluoro-L-dopa. Int J Rad Appl Instrum A. 1992;43:989–96.
Hudson HM, Larkin RS. Accelerated image reconstruction using ordered subsets of projection data. IEEE Trans Med Imaging. 1994;13:601–9.
Nuyts J, Michel C, Dupont P. Maximum-likelihood expectation-maximization reconstruction of sinograms with arbitrary noise distribution using NEC-transformations. IEEE Trans Med Imaging. 2001;20:365–75.
Schiepers C, Hoh CK, Nuyts J, Wu HM, Phelps ME, Dahlbom M. Factor analysis in prostate cancer: delineation of organ structures and automatic generation of in- and output functions. IEEE Trans Nucl Sci. 2002;49:2338–43.
Schiepers C, Hoh CK, Dahlbom M, Wu HM, Phelps ME. Factor analysis for delineation of organ structures, creation of in- and output functions, and standardization of multicenter kinetic modeling. Proc SPIE. 1999;3661:1343–50.
Sitek A, Di Bella EV, Gullberg GT. Factor analysis with a priori knowledge – application in dynamic cardiac SPECT. Phys Med Biol. 2000;45:2619–38.
Ell PJ, Gambhir SS. Nuclear medicine in clinical diagnosis and treatment. 3rd ed. Edinburgh: Churchill Livingstone; 2004.
Schiepers C, Chen W, Dahlbom M, Cloughesy T, Hoh CK, Huang SC. 18F-fluorothymidine kinetics of malignant brain tumors. Eur J Nucl Med Mol Imaging. 2007;34:1003–11.
Muzi M, Vesselle H, Grierson JR, Mankoff DA, Schmidt RA, Peterson L, et al. Kinetic analysis of 3′-deoxy-3′-fluorothymidine PET studies: validation studies in patients with lung cancer. J Nucl Med. 2005;46:274–82.
Reske SN, Deisenhofer S. Is 3′-deoxy-3′-(18)F-fluorothymidine a better marker for tumour response than (18)F-fluorodeoxyglucose? Eur J Nucl Med Mol Imaging. 2006;33 Suppl 1:38–43.
Shields AF. PET imaging of tumor growth: not as easy as it looks. Clin Cancer Res. 2012;18:1189–91.
Huang SC, Yu DC, Barrio JR, Grafton S, Melega WP, Hoffman JM, et al. Kinetics and modeling of L-6-[18F]fluoro-dopa in human positron emission tomographic studies. J Cereb Blood Flow Metab. 1991;11:898–913.
Schiepers C, Chen W, Cloughesy T, Dahlbom M, Huang SC. 18F-FDOPA kinetics in brain tumors. J Nucl Med. 2007;48:1651–61.
Beuthien-Baumann B, Bredow J, Burchert W, Fuchtner F, Bergmann R, Alheit HD, et al. 3-O-methyl-6-[18F]fluoro-L-DOPA and its evaluation in brain tumour imaging. Eur J Nucl Med Mol Imaging. 2003;30:1004–8.
Huang SC. Anatomy of SUV. Standardized uptake value. Nucl Med Biol. 2000;27:643–6.
Visvikis D, Francis D, Mulligan R, Costa DC, Croasdale I, Luthra SK, et al. Comparison of methodologies for the in vivo assessment of 18F-FLT utilisation in colorectal cancer. Eur J Nucl Med Mol Imaging. 2004;31:169–78.
Huang SC, Barrio JR, Yu DC, Chen B, Grafton S, Melega WP, et al. Modelling approach for separating blood time-activity curves in positron emission tomographic studies. Phys Med Biol. 1991;36:749–61.
Petrie A, Sabin C. Medical statistics at a glance. 3rd ed. Chichester: Wiley-Blackwell; 2009.
Dietz T, Kalof L. Introduction to social statistics: the logic of statistical reasoning. Chichester: Wiley-Blackwell; 2009.
Yamamoto Y, Ono Y, Aga F, Kawai N, Kudomi N, Nishiyama Y. Correlation of 18F-FLT uptake with tumor grade and Ki-67 immunohistochemistry in patients with newly diagnosed and recurrent gliomas. J Nucl Med. 2012;53:1911–5.
Plotnik DA, McLaughlin LJ, Chan J, Redmayne-Titley JN, Schwartz JL. The role of nucleoside/nucleotide transport and metabolism in the uptake and retention of 3′-fluoro-3′-deoxythymidine in human B-lymphoblast cells. Nucl Med Biol. 2011;38:979–86.
Grierson JR, Schwartz JL, Muzi M, Jordan R, Krohn KA. Metabolism of 3′-deoxy-3′-[F-18]fluorothymidine in proliferating A549 cells: validations for positron emission tomography. Nucl Med Biol. 2004;31:829–37.
Lammertsma AA, Hume SP. Simplified reference tissue model for PET receptor studies. Neuroimage. 1996;4:153–8.
Lammertsma AA, Bench CJ, Hume SP, Osman S, Gunn K, Brooks DJ, et al. Comparison of methods for analysis of clinical [11C]raclopride studies. J Cereb Blood Flow Metab. 1996;16:42–52.
Khalil MM. Basic sciences of nuclear medicine. Heidelberg: Springer; 2011.
Acknowledgments
The authors are grateful to all the patients who participated in this study as well as to their families. In addition, the authors thank David Truong, Dat Vu, and Weber Shao for their computer and database support, the UCLA Cyclotron staff for help with FLT and FDOPA preparation, and the UCLA Nuclear Medicine staff for acquisition of the PET scans. This work was supported by the US Department of Energy contract DEFG02-06ER64249 and NIH grants P50-CA086306 and R01-EB001943.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 2574 kb)
Rights and permissions
About this article
Cite this article
Wardak, M., Schiepers, C., Cloughesy, T.F. et al. 18F-FLT and 18F-FDOPA PET kinetics in recurrent brain tumors. Eur J Nucl Med Mol Imaging 41, 1199–1209 (2014). https://doi.org/10.1007/s00259-013-2678-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-013-2678-2