Mental health problems among hotline callers during the early stage of COVID-19 pandemic
- Published
- Accepted
- Received
- Academic Editor
- Bao-Liang Zhong
- Subject Areas
- Psychiatry and Psychology, Public Health, Mental Health, COVID-19
- Keywords
- COVID-19 Pandemic, Hotline, Mental health
- Copyright
- © 2022 An et al.
- Licence
- This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, reproduction and adaptation in any medium and for any purpose provided that it is properly attributed. For attribution, the original author(s), title, publication source (PeerJ) and either DOI or URL of the article must be cited.
- Cite this article
- 2022. Mental health problems among hotline callers during the early stage of COVID-19 pandemic. PeerJ 10:e13419 https://doi.org/10.7717/peerj.13419
Abstract
Background
The study aims to explore the mental health of the hotline callers during the COVID-19 pandemic in China.
Methods
Callers (N = 10,490) from the Beijing Psychological Support Hotline from January 21st to June 30th in 2019 and 2020 were enrolled and divided into two groups (during (2020) and before (2019) COVID-19 pandemic). The severity of depressive symptoms, psychological distress, hopefulness, and suicidal ideation (SI) was assessed. Demographic characteristics and major concerns were also collected. Mann-Whitney U and chi-square test were used to compare the differences in mental health conditions and major concerns between two years and between different age groups. The multivariable logistic regression was used to explore whether mental health conditions were associated with pandemic and demographic factors.
Results
Results from multivariable logistic regression analysis indicated that the change in suicidal ideation (OR = 1.52, 95% CI: 1.21–1.92) was significantly different across age groups. Callers during the pandemic reported a higher level of hopefulness (OR = 1.13, 95% CI [1.03–1.24]), a lower level of depressive symptoms (OR = 0.81, 95% CI [0.74–0.89]) and psychological distress (OR = 0.89, 95% CI [0.81–0.98]), and were less likely to report SI (OR = 0.69, 95% CI [0.61–0.77]) compared with callers before the pandemic.
Conclusions
Compared with callers before the pandemic, hotline callers during the early stage of COVID-19 pandemic did not present significant mental health problems. Younger callers during the pandemic were more vulnerable for the presence of suicidal ideation. Hotline-based crisis interventions might provide specific psychological support to cope with troubles during the pandemic.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic poses a significant threat to the mental health in the general population (Cooke et al., 2020; Debowska et al., 2020; Brooks et al., 2020; Shi et al., 2020; Luo et al., 2020). Anxiety, depression, stress, and sleep problems are commonly reported among the public during the pandemic (Cooke et al., 2020; Debowska et al., 2020; Brooks et al., 2020; Shi et al., 2020; Luo et al., 2020). During the pandemic, higher suicidal risk at population level was one of the most important concerns, given people were widely exposed to social isolation, financial recession, and barriers to accessing mental health care (Gunnell et al., 2020). Previous online surveys found that 4.6% to 17.5% of individuals reported suicide ideation (SI), 1.2% to 4.9% had attempted suicide in the last month (Ammerman et al., 2021; Bryan, Bryan & Baker, 2020), and 7.6% of the respondents were found to have higher suicide risk during the pandemic (Caballero-Dominguez, Jimenez-Villamizar & Campo-Arias, 2020). Previous epidemics, as Severe Acute Respiratory Syndromes (SARS) in 2003 has also shown to be associated with the increase in suicide (Zortea et al., 2020).
Individuals in different age groups seem to be impacted psychologically in different tendencies during the pandemic. Previous evidence suggests a relatively higher severity of mental health problems, such as anxiety and depression in younger adults during the COVID-19 pandemic (Huang & Zhao, 2020; Liu et al., 2020a; Liu et al., 2020b; Jia et al., 2020). Younger adults have the highest level, while the older have the lowest level of SI during the pandemic (O’Connor et al., 2020; Czeisler et al., 2020; Iob, Steptoe & Fancourt, 2020). However, the evidence from the SARS epidemic suggested that the suicide rate increased greatly among older adults in Hong Kong (Cheung, Chau & Yip, 2008; Chan et al., 2006).
The rapid transmission of COVID-19 led to a halt in delivering face-to-face psychological services, and as a result, online mental health service resources, such as the internet and telephone hotlines were widely used to provide psychological assessment and interventions (Feinstein et al., 2020; Wang, Wei & Zhou, 2020; Liu et al., 2020a; Liu et al., 2020b). Hotlines, in particular, have become a popular way for individuals seeking for psychological help during COVID-19. Beijing Psychological Support Hotline (BPSH) is a national 24-hour toll-free crisis hotline in China, and provides psychological services for hundreds of thousands of callers every year. More than half of the BPSH callers reported SI before the pandemic (Zhao et al., 2021). Considering the fact that more individuals exposed to the suicide risk factors during the pandemic, it is vital to understand whether mental health problems of hotline callers among different age groups increased during the pandemic, in order to guide decisions on further effective allocation of psychological service resources in the hotline.
The present study compared the mental health status of the BPSH callers between the callers before the COVID-19 pandemic (the first half-year of 2019) and during the pandemic (the first half of year of 2020). The findings of our study would be helpful to discuss whether the impacts of the COVID-19 pandemic on the mental health of hotline callers. It will contribute to the development of hotline-based psychological interventions during public health emergencies in the future.
Materials & Methods
Subjects
The study was conducted at the BPSH, which provided psychological intervention for Mandarin-speaking callers before and during the COVID-19 pandemic. COVID-19 was confirmed as a human-to-human transmitted virus on January 20th, 2020, and remained a national epidemic in mainland China until summer 2020. Thus, in the present study, callers from January 21st to June 30th, 2020 were enrolled as participants during the early stage of the pandemic. In addition, callers in the same time period in 2019 were enrolled as pre-pandemic participants.
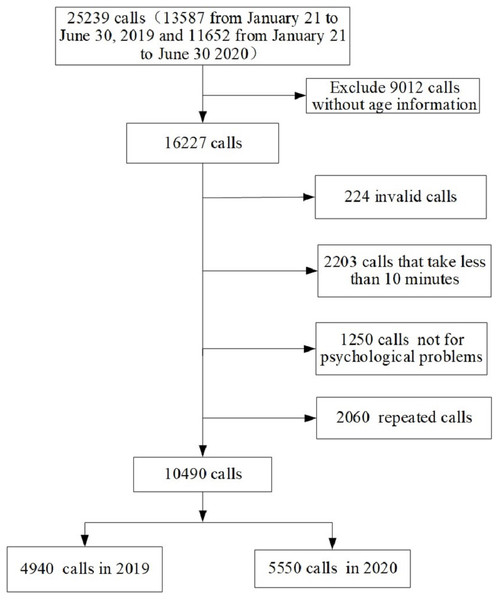
A total of 25,239 calls were answered in that periods of 2019 and 2020 in the BPSH. Exclusion criteria were: (1) the caller’s main purpose was not seeking psychological services (e.g., only asking for information), (2) “null” calls (i.e., silence, harassing, or hoax calls), or (3) calls lasting for less than 10 min. For repeat calls from the same caller, only the first call was included in the analysis. Finally, 10,490 calls were enrolled into the study (4,940 in 2019, accounting for 47.1% and 5,550 in 2020, accounting for 52.9%).
The study was approved by the Institutional Review Board of Beijing Huilongguan Hospital (2020-19-Science). Each caller was informed by a voice message that the call would be tape-recorded, data would be collected, deidentified, and analyzed.
Measurements
In the BPSH, mental health factors included severity of depression, psychological distress, level of hopefulness, and the presence of SI (Bell et al., 2015; Walker, McGee & Druss, 2015; Davidson et al., 2009). For depression, a structured assessment questionnaire (Phillips et al., 2007) was used to determine the severity and duration of each of nine depressive symptoms in the last 2 weeks prior to the index call. The assessment has excellent inter-rater reliability (ICC = 1.00), test-retest reliability (ICC = 0.91) and consistency with Structured Clinical Interview for DSM-IV (SCID), (Kappa = 0.87) (Li et al., 2007). The score was calculated by the item severity multiplied by duration of the symptom. The total score of depressive symptoms was converted into 0 to 100, with a higher score indicating more severe depressive symptoms.
Psychological distress was assessed by asking callers “To what extent do you feel psychological distressed?”. Callers were instructed that a score of 0 means completely no psychological distress and 100 means feeling completely distressed (Tong et al., 2020). Hopefulness was assessed by asking callers “To what extent do you feel hopeful?”. Callers were instructed that a score of 0 means absolutely hopeless and 100 means completely hopeful (Tong et al., 2020).
SI was assessed by asking the caller “Have you repeatedly thought about taking your life or hurting yourself in the last two weeks?” or “Have you felt too tired and without meaning to continue to live in the last two weeks?”. If a caller responded “yes” to any of the above two questions, he/she would be regarded as having suicidal ideation (Tong et al., 2020).
During the routine counselling of hotline, the operator and the caller would work together on the identification and coping with major concern of the caller. The identification of the major concern was based on whether the caller had a history of being diagnosed as psychiatric illness or receiving outpatient or inpatient psychiatric treatments (medication, psychotherapy, and other therapies such as ECT), caller’s complaints on psychological disturbance or life events, and severity of depression assessed by structured questionnaire. The concerns were categorized into seven categories or sources of distress: (1) family relationship problems, e.g., conflicts with family members; (2) non-family relationship problems, e.g., interpersonal conflicts with non-family members, such as friends and colleagues; (3) financial problems, e.g., debts, failed investments, etc.; (4) work-related problems, e.g., work pressure, losing the job, setback in career advancement; (5) clinically significant depression, based on a structured assessment (Phillips et al., 2007); (6) other negative life events, e.g., caller was distressed by events other than the five categories listed above; (7) other psychiatric problems, e.g., caller reported a history of any mental disorder other than depression.
The demographic characteristics were collected by the hotline counsellor at the beginning of answering the call.
Statistical analysis
The final sample of callers was split into two groups, namely, calls during the pandemic (January–June 2020) and before the pandemic (January–June 2019). Mann–Whitney U and chi-square tests were used to compare the differences in mental health conditions and major concerns of callers between two years and different age groups. The multivariable logistic regression was used to explore whether mental health conditions were associated with demographic factors and the pandemic. Gender, marital status, education levels, age group, year of index call (2019 and 2020), and an interaction term between age group by before/during pandemic (namely, year of index call) were entered into the model to test whether the effect of age groups on mental health conditions was different between the two pandemic periods (before/during) (Altman & Bland, 2003). Dependent variables included depression and psychological distress severity, level of hopefulness, and SI. All dependent variables were dichotomized and analyzed separately. The score for the hopefulness, psychological distress, and depressive symptoms were respectively dichotomized by the median scores, namely, 30, 80, 68. Data analyses were conducted using SPSS 18.0.
Results
A total of 10,490 calls from 2019 January 21st to June 30th and in the same period in 2020 were included in the final data analysis. A detailed overview of enrolling and screening hotline callers is shown in Fig. 1. As seen in Table 1, there was no significant difference in marital status between callers before and during pandemic (p = 0.070), however, callers during the COVID-19 pandemic were more likely to be female (p < 0.001), over 30 years (p = 0.048) and highly educated (p < 0.001) than callers before the pandemic.
Figure 1: Flow chart for recruitment of final sample.
| Characteristics | Before pandemic (n = 4940) n (%) | During pandemic (n = 5550) n (%) | χ2 | p |
|---|---|---|---|---|
| Gender | 66.14 | 0.000 | ||
| Female | 2604 (52.7) | 3364 (60.6) | ||
| Male | 2334 (47.3) | 2186 (39.4) | ||
| Age group | 3.91 | 0.048 | ||
| <30 years old | 3756 (76.0) | 4127 (74.4) | ||
| ≥30 years old | 1184 (24) | 1423 (25.6) | ||
| Marital status | 3.29 | 0.070 | ||
| Unmarried | 3791 (76.7) | 4175 (75.2) | ||
| Married | 1149 (23.3) | 1375 (24.8) | ||
| Education years | 41.99 | 0.000 | ||
| 0–9 | 657 (13.3) | 700 (12.6) | ||
| 10–12 | 1417 (28.7) | 1307 (23.5) | ||
| ≥13 | 2866 (58.0) | 3543 (63.8) |
Notes:
Each variable contains missing values, so the sum of the callers of each variable is less than the total number of callers.
Callers before the pandemic were more likely to report SI (78.7% vs. 73.4%, χ2=31.29, p < 0.001), higher depression score (Z = − 3.57, p < 0.001), lower level of hopefulness (Z = − 3.03, p = 0.002) than callers during pandemic (Table 2). Callers during the pandemic were more likely to endorse depression problems (25.6% vs 21.3%, χ2 = 26.49, p < 0.001) and family relationship problems (23.2% vs 20.1%, χ2 = 14.85, p < 0.001), and less likely to encounter other negative events (5.7% vs 7.0%, χ2 = 6.94, p = 0.008), financial problems (8.0% vs 10.3%, χ2 = 16.24, p < 0.001), and relationship problems (28.1% vs 30.3%, χ2 = 5.69, p = 0.017) than callers before the pandemic (Table 2).
| Variables | Before pandemic (n = 4940) | During pandemic (n = 5550) | Younger (n = 7883) | Older (n = 2607) | ||
|---|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Z | Median (IQR) | Median(IQR) | Z | |
| Hopefulness | 30 (2,50) | 30 (5,50) | −3.03** | 30 (5,50) | 35 (5,60) | −5.03*** |
| Psychological distress | 80 (70,95) | 80 (70,95) | −1.82 | 80 (70,95) | 80 (70,95) | −1.33 |
| Depression severity | 69 (53,81) | 67 (52,80) | −3.57*** | 68 (53,81) | 67 (49,81) | −2.92** |
| n (%) | n (%) | χ2 | n (%) | n (%) | χ2 | |
| Presence of suicidal ideation | 2909 (78.7) | 3165 (73.4) | 31.29*** | 4816 (78.9) | 1258 (66.1) | 130.66*** |
| n (%) | n (%) | χ2 | n (%) | n (%) | χ2 | |
| Family relationship problems | 992 (20.1) | 1287 (23.2) | 14.85*** | 1525(19.3) | 754 (28.9) | 105.66*** |
| Non-family relationship problems | 1495 (30.3) | 1562 (28.1) | 5.69* | 2646 (33.6) | 411 (15.8) | 300.62*** |
| Financial problems | 509 (10.3) | 446 (8.0) | 16.24*** | 606 (6.7) | 349 (13.4) | 76.91*** |
| Work problems | 344 (7.0) | 367 (6.6) | 0.51 | 530 (6.7) | 181 (6.9) | 0.15 |
| Depression | 1052 (21.3) | 1419 (25.6) | 26.49*** | 1846(23.4) | 625 (24) | 0.34 |
| Other negative events | 345 (7.0) | 318 (5.7) | 6.94** | 414 (5.3) | 52 (9.6) | 61.16*** |
| Psychiatric problems | 833 (16.9) | 906 (16.3) | 0.55 | 1278 (16.2) | 461 (17.7) | 3.07 |
There were also significant differences between the two age groups in mental health status, specifically in hopefulness (Z = − 5.03, p < 0.001), the severity of depressive symptoms (Z = − 2.92, p = 0.004), presence of SI (χ2 = 130.66, p < 0.001) (Table 2). Proportions of major concerns varied across the two age groups of callers reached statistical significance (Table 2). Young adult callers were more likely to report non-family relationship problems (χ2 = 300.62, p < 0.001), while older callers were more likely to have concerns about family relationship problems (χ2 = 105.66, p < 0.001), financial problems (χ2 = 76.91, p < 0.001) and other negative events (χ2 = 61.16, p < 0.001).
As for the younger callers, there was no significant difference in the hopefulness, the severity of depressive symptoms, and psychological distress (p > 0.05); while older callers had higher level of hopefulness (Z = − 2.74, p = 0.006) and lower level of psychological distress (Z = − 2.02, p < 0.043) and depression (Z = − 3.95, p < 0.001). The prevalence of SI in 2019 is higher than that in 2020 no matter among the younger (Z = 7.14, p = 0.008) or the older callers (Z = 35.73, p < 0.001). Callers were inclined to report depression problems during the pandemic for both the younger (Z = 9.07, p = 0.003) and older callers (Z = 25.54, p < 0.001) (Table 3). Callers were less likely to report financial problems during the pandemic for both the younger (Z = 7.46, p = 0.006) and older callers (Z = 11.61, p = 0.001).
| Variables | Younger (n = 7883) | Older (n = 2607) | ||||
|---|---|---|---|---|---|---|
| Before pandemic (n = 3,756) | During pandemic (n = 4,127) | Before pandemic (n = 1,184) | During pandemic (n = 1,423) | |||
| Median (IQR) | Median (IQR) | Z | Median (IQR) | Median(IQR) | Z | |
| Hopefulness | 26 (2,50) | 30 (5,50) | −1.91 | 35 (0,55) | 40 (10,60) | −2.74** |
| Psychological distress | 80 (70,95) | 80 (70,95) | −0.92 | 85 (70,99) | 80 (70,95) | −2.02* |
| Depression severity | 68 (54,81) | 68 (53,80) | −1.76 | 69 (52,82) | 65 (46,80) | −3.95*** |
| n (%) | n (%) | χ2 | n (%) | n (%) | χ2 | |
| Presence of suicidal ideation | 2282 (80.4) | 2534 (77.6) | 7.14** | 627 (73.2) | 631 (60.2) | 35.73*** |
| n (%) | n (%) | χ2 | n (%) | n (%) | χ2 | |
| Family relationship problems | 639 (17.0) | 886 (21.5) | 25.02*** | 353 (29.8) | 401 (28.2) | 0.84 |
| Non-family relationship problems | 1302 (34.7) | 1344 (32.6) | 3.88* | 193 (16.3) | 218 (15.3) | 0.47 |
| Financial problems | 321 (8.5) | 285 (6.9) | 7.46** | 188 (15.9) | 161 (11.3) | 11.61** |
| Work problems | 260 (6.9) | 270 (6.5) | 0.45 | 84 (7.1) | 97 (6.8) | 0.08 |
| Depression | 823 (21.9) | 1023 (24.8) | 9.07** | 229 (19.3) | 396 (27.8) | 25.54*** |
| Other negative events | 222 (5.9) | 192 (4.7) | 6.26* | 123 (10.4) | 126 (8.9) | 1.76 |
| Psychiatric problems | 622 (16.6) | 656 (15.9) | 0.64 | 211 (17.8) | 250 (17.6) | 0.03 |
Results of multivariable logistic regression analysis revealed that callers during the pandemic were less likely to report SI (OR = 0.69, 95% CI [0.61–0.77]). Callers who were married (OR = 0.78, 95% CI [0.67–0.90]) and had higher education level (OR = 0.79, 95% CI [0.73–0.85]) were less likely to report SI. Callers who were married (OR = 1.21, 95% CI [1.07–1.36]), had higher education level (OR = 1.14, 95% CI [1.08–1.20]) and during the pandemic (OR = 1.13, 95% CI [1.03–1.24]) were inclined to report higher level of hopefulness. Callers who were male (OR = 0.84, 95% CI [0.77–0.91]), had higher education level (OR = 0.92, 95% CI [0.87–0.98]) and during the pandemic (OR = 0.89, 95% CI [0.81–0.98]) were not inclined to report severe psychological distress. While callers who were married were more inclined to report severe psychological distress (OR = 1.23, 95% CI [1.09–1.29]). Callers during the pandemic (OR = 0.81, 95% CI [0.74–0.89]) and had higher education level (OR = 0.91, 95% CI [0.86–0.96]) were less likely to report higher level of depression (Table 4).
| Having suicidal ideation | High hopefulness | Severe Psychological distress | High depressive score | |||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Male | ||||||||
| (ref: female) | 0.91 | 0.82-1.01 | 1.00 | 0.92-1.09 | 0.84*** | 0.77-0.91 | 1.03 | 0.95-1.12 |
| Marital status | ||||||||
| (ref: unmarried) | 0.78** | 0.67–0.90 | 1.21** | 1.07–1.36 | 1.23** | 1.09–1.39 | 0.97 | 0.86–1.09 |
| Education years | 0.79*** | 0.73–0.85 | 1.14*** | 1.08–1.20 | 0.92** | 0.87–0.98 | 0.91** | 0.86–0.96 |
| Pandemic (2020) | ||||||||
| (ref: Pre-pandemic) | 0.69*** | 0.61–0.77 | 1.13** | 1.03–1.24 | 0.89* | 0.81–0.98 | 0.81*** | 0.74–0.89 |
| Age groups | ||||||||
| (ref: ≥30 years old) | ||||||||
| <30 years old | 0.85 | 0.57–1.26 | 1.02 | 0.75–1.39 | 0.97 | 0.70–1.35 | 0.74 | 0.54–1.01 |
| Age* year interaction | ||||||||
| <30 years old during pandemic | 1.52*** | 1.21–1.92 | 0.89 | 0.74–1.08 | 1.07 | 0.88–1.30 | 1.15 | 0.95–1.39 |
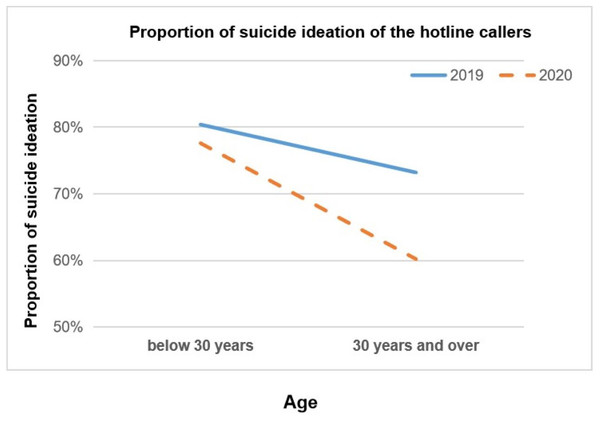
The interaction terms of age-group by pandemic period (before and during pandemic) were statistically significant for SI (OR=1.52, 95% CI [1.21–1.92]) (Table 4). It indicated that the change in suicidal ideation is significantly different across age groups. As shown in the Fig. 2, among callers aged 30 or above, the proportion of SI decreased in 2020, compared with same period in 2019, however, the proportion of SI almost unchanged in 2019 and 2020 among the young callers under 30 years old.
Discussion
Hotlines have emerged as one of the most popular—and safest from a viral transmission standpoint—ways to deliver psychological services during the pandemic (Feinstein et al., 2020; Liu et al., 2020a; Liu et al., 2020b; Wang, Wei & Zhou, 2020). Our study offers an examination of the mental health of callers before and during the early stage of COVID-19 pandemic. Results showed that the overall prevalence of SI among callers was lower during the early stage of pandemic (2020) than before (2019), which was consistent with previous studies on crisis helplines during the COVID-19 pandemic (Brülhart et al., 2021; Zalsman et al., 2021; Batchelor et al., 2021). Meanwhile, different age groups of callers showed different trends in the SI during the pandemic, which suggested that the pandemic seldom caused impact on younger callers, while older adult callers reported less SI during the pandemic, comparing with that in pre-pandemic.
Figure 2: Proportion of suicide ideation of the hotline callers.
Comparisons of mental health status of hotline callers during pandemic and before pandemic, moderated by age groups.Although there were significant concerns about suicide during the pandemic due to more exposures to suicide risk factors such as social isolation, financial stress, and limited access to treatment (Moutier, 2021; Reger, Stanley & Joiner, 2020; Gunnell et al., 2020), data from 21 countries and regions showed that numbers of suicide in high- and upper-middle-income regions remained stable and even declined in the early month of the pandemic (Pirkis et al., 2021; Hawton et al., 2021). Our study adds to this growing body of research, suggesting that the prevalence of SI among hotline callers during the early stage of pandemic was lower than that in 2019. Hopefulness and depression are important factors related to suicide (Davidson et al., 2009; Bell et al., 2015; Walker, McGee & Druss, 2015). Higher level of hopefulness and lower level of depression of callers during the pandemic, compared with pre-pandemic in our study may contribute to lower prevalence of SI among callers. Though lockdown and financial stress were regarded as suicide risk factors during the pandemic (Moutier, 2021; Reger, Stanley & Joiner, 2020; Gunnell et al., 2020), our study found that callers reported fewer financial problems during the pandemic, besides, lockdown may only occur in specific residential districts which affected by infected cases, which may seldom affect the SI of callers in our study during the early stage of the pandemic.
Relatively better mental health status among older adult callers during the early stage of the pandemic could be attributed to various factors. First, higher level of hopefulness is helpful for improving coping strategies which may in turn decrease the suicidality (Snyder et al., 1996). In the present study, older adult callers reported higher hopefulness during the pandemic than the pre-pandemic, which may be a protective factor for SI and depression. Second, economic recession and unemployment appear to be specific pandemic-related suicide risk factors (Kawohl & Nordt, 2020). However, in our study, older adult callers were less likely to be involved in financial difficulties during the pandemic, which may have decreased their risk Third, older adults may be well-equipped to seek alternative modes of contact, and maintain relationships through the internet and telephone (Chen & Schulz, 2016), which may be useful for dealing with the concerns that social distancing and other lockdown measures may result in greater loneliness and social isolation and worsened mental health among older adults (Goethals et al., 2020; Wu, 2020). Fourth, better emotional regulation, more adaptive coping styles, and experience to deal with stressors were found among older adults (Lee et al., 2019).
Relatively worse mental health status among younger hotline callers during the early stage of the COVID-19 pandemic in our study is consistent with previous studies, in which younger people are at higher risk for mental problems (Liu et al., 2020a; Liu et al., 2020b; Huang & Zhao, 2020; Shi et al., 2020), even suicide risk (Iob, Steptoe & Fancourt, 2020; Czeisler et al., 2020). Worse mental health problems among younger adults may be attributable to the fact that young adults have more exposure to social media (Gao et al., 2020; Zhao & Zhou, 2020; The Lancet, 2019), more psychological pressure from the unemployment financial concerns during the pandemic (Liu et al., 2020a; Liu et al., 2020b; Jia et al., 2020; Gratz et al., 2020). Our study found that younger callers reported more family relationship, and depression problems during the pandemic, suggesting younger callers may be obsessed with economic and unemployment difficulties, which may also explain the result.
In our study, we found that callers had more concerns about their depression problems, which maybe due to the barriers to accessing mental health care (Gunnell et al., 2020), suggesting more convenient access to mental health care, such as remote medical service, delivering medicine by the hospital to patients would be needed during the pandemic. we also found demographic factors were associated with mental health of callers. Unmarried, females and lower educational level were identified as correlated factors for poor mental health outcomes, which was consistent with previous researches (Shi et al., 2020; Lee et al., 2015; Gunnell et al., 2020).
There are several limitations in the present study. First, our study sample included hotline callers who actively seeking psychological help, and older adults may be less likely to use hotlines compared with youngers. Special subgroups of older adults, such as those living in the nursing homes, were not included in our study. Therefore, caution should be used in generalizing our findings to all older adults in China. Second, the year 2020 and 2019 was used as an indicator of exposure to pandemic-related stress or not; however, we did not ask about specific pandemic-related stressors, such as whether callers were exposed to the virus or knew someone affected by the virus. Third, our data relied on callers’ self-report. Future studies may use comprehensive, gold-standard standardized assessments to determine the presence and severity of psychiatric conditions. Fourth, the severity of COVID-19 infection differed regionally, e.g., in Wuhan and other regions in China. However, we could not identify the location of callers via hotline, which limits our ability to investigate this important issue in this study.
Conclusions
Though our findings implied that during the early stage of the COVID-19 pandemic, callers did not appear more severe mental health problems compared with callers before the pandemic. However, we need to remain vigilant to respond to the long-term mental health effect of the pandemic, as the pandemic is ongoing. The unmarried, females and those with a lower educational level were identified as correlated factors for poor mental health outcomes during the pandemic. Younger callers were more vulnerable to mental health problems compared with the older age groups. Thus, some age-specific mental health prevention should be provided through the hotline during public health emergencies in the future.