Abstract
Context:
Hypertension (HTN) is a well-known modifiable risk factor for cardiovascular disease (CVD), chronic kidney disease and mortality. Positive effects of blood pressure (BP) lowering for prevention of CVD and death have been documented in several meta-analyses of randomized controlled trials.Evidence Acquisition:
This review focuses on the key findings derived from the Tehran lipid and glucose study (TLGS) papers on different aspects of BP and HTN.Results:
A prevalence of 23% for HTN has been reported in the TLGS population, aged ≥ 20 years. Over a decade long follow-up, the crude incidence rate (95% CI) of new-onset HTN defined as systolic BP (SBP) ≥ 140 mmHg and/or diastolic BP (DBP) ≥ 90 mmHg, and not using antihypertensive medication was 33.63 (32.0 - 35.3) per 1000 person-years. Age, baseline SBP and body mass index were significant risk factors for development of isolated systolic HTN; regarding isolated diastolic HTN, baseline DBP and waist circumference were recognized as important risk factors whereas age, female gender and marriage were shown to be protective factors. SBP decreased significantly in both diabetic and non-diabetic participants; DBP showed a non-significant decrease in diabetic men and a statistically significant decrease in non-diabetic men. Among women, both those with and without diabetes (DM) generally experienced statistically significant decreases in DBP. Cox proportional hazard models showed that neither SBP nor DBP were associated with incident DM in the total population and in either gender, separately. All BP components were associated with CVD and all-cause mortality in the middle-aged population. Contribution of HTN to cerebrovascular events was also documented in the TLGS participants, aged ≥ 50 years.Conclusions:
Several important findings regarding BP/HTN have been derived from the TLGS. According to data regarding the prevalence and incidence of preHTN and HTN and their contribution to cardiovascular morbidity and mortality in the TLGS population as a representative sample of Tehranian population, it is recommended that interventions be prioritized for lifestyle modifications for the prevention and appropriate management of preHTN/HTN.Keywords
Blood Pressure Hypertension Prehypertension Type 2 Diabetes Cardiovascular Mortality
1. Context
Hypertension (HTN) as a well-known modifiable risk factor (RF) for cardiovascular disease (CVD), chronic kidney disease and mortality (1), is one of the most prevalent non-communicable diseases worldwide. The overall prevalence of HTN was reported to be 26.4% in 2000 (2), and 24.1% in men and 20.1% in women in 2015 (3), and is estimated to reach 29.2% by 2025 (2). Data from the Iranian survey of risk factors of non-communicable diseases (SuRFNCD)-2011 reported that 25.6% and 39.8% of adults, aged 25 - 70 years had HTN and preHTN, respectively (4).
Associations of systolic and/or diastolic HTN with increased risk of CVD and mortality has been reported in several observational studies (5, 6). Positive effects of BP lowering for prevention of CVD and death have been documented in several meta-analyses of RCTs (7, 8).
This review focuses on the key findings derived from the Tehran Lipid and Glucose Study (TLGS) data documented on different aspects of blood pressure (BP) and HTN.
2. Evidence Acquisition
All TLGS articles related to BP parameters and/or HTN were searched using PubMed, Scopus and Web of Science with appropriate keywords since January 1999 up to December 2017.
3. Results
3.1. Prevalence
Table 1 shows mean ± SD of SBP and DBP also prevalence of hypertension in different age groups studied in the TLGS phase 1.
| Age, y | SBP | DBP | HTN [% (95% CI)] | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Total | Male | Female | Total | Male | Female | Total | |
| 3 - 19d | - | - | - | - | - | - | 12.7 (11.3 - 14.1) | 10.9 (9.6 - 12.2) | 11.7 (10.8 - 12.6) |
| 10 - 14e | 103 ± 11 | 102 ± 11 | - | 69.5 ± 9 | 70 ± 10 | - | - | - | - |
| 15 - 19e | 110 ± 12 | 106 ± 11 | - | 72.3 ± 9 | 72.9 ± 9 | - | - | - | - |
| ≥ 20d | 120 ± 17 | 116 ± 17 | - | 77 ± 11 | 77 ± 10 | - | 20.4 (19.2 - 21.6) | 25.1 (24 - 26.2) | 22.9 (22.1 - 23.7) |
| ≥ 60f | 136 ± 23 | 141 ± 23 | 138 ± 23 | 80 ± 13 | 82 ± 12 | 81 ± 12 | 42.5 | 51.7 | 47 |
| 60 - 64f | 134 ± 23 | 138 ± 22 | 136 ± 22 | 82 ± 13 | 83 ± 12 | 83 ± 12 | 38.4 | 49.8 | 44.7 |
| 65 - 69f | 137 ± 24 | 141 ± 23 | 139 ± 24 | 80 ± 12 | 82 ± 12 | 81 ± 12 | 42.9 | 50.7 | 46.6 |
| ≥ 70f | 139 ± 22 | 144 ± 23 | 141 ± 22 | 78 ± 14 | 80 ± 11 | 79 ± 13 | 46.9 | 57.1 | 51.1 |
3.2. Incidence and Predicting Risk Factors of HTN
During a median follow-up of 6 years, 4656 individuals with 26,846 person-years were followed; new onset HTN events were documented in 805 individuals. Incidence rate of HTN (per 1000 person-years) was 29.3 [95% confidence interval (CI) 26.7 - 32.1]) and 30.9 (95% CI 27.8 - 34.3) for women and men, respectively. Age [HR (95% CI): 0.904 (0.826 - 0.990)], waist circumference (WC) [HR (95% CI): 1.014 (1.006 - 1.023)], diastolic BP (DBP) [HR (95% CI): 1.042 (1.025 - 1.060)], systolic BP (SBP) [HR (95% CI): 0.985 (0.950 - 1.021)], and family history of premature CVD [HR (95% CI): 1.625 (1.235 - 2.137)] predicted incident hypertension in females, while age [HR (95% CI): 1.136 (1.039 - 1.241)], DBP [HR (95% CI): 1.027 (1.010 - 1.044)], SBP [HR (95% CI): 1.086 (1.046 - 1.127)] and smoking [HR (95% CI): 1.264 (0.983 - 1.626)] were shown as predictors in males (12).
During a median 9.5 year follow-up (F/U) of the TLGS population (13), the crude incidence rate (95% CI) of isolated systolic hypertension (ISH) in the total population was reported to be 5.7 (5.0 - 6.5) per 1000 person-years of F/U. The highest incidence of ISH among age categories was observed in the older population (≥ 60 years), at 37.5 (30.6 - 46.0) per 1000 person-years, compared to younger adults (aged 20 - 39 years), at 0.8 (0.5 - 1.3) per 1000 person-years of F/U. The crude incidence rate (95% CI) of isolated diastolic hypertension (IDH) was 10.9 (10.0 - 12.0) per 1000 person-years. The incidence of IDH was higher in subjects aged 40 - 59 years, at 13.67 (11.8 - 15.8) per 1000 person years, and a lower rate was observed in the population aged ≥ 60 years, at 6.4 (3.8 - 10.9) per 1000 person-years of F/U. The crude incidence rate (95% CI) of new-onset HTN defined as SBP ≥ 140 mmHg and DBP ≥ 90 mmHg, and not using antihypertensive medication, was 33.63 (32.0 - 35.3) per 1000 person-years; the crude incidence rate for both high SBP and DBP was 6.3 (5.6 - 7.0) per 1000 person-years. In this study, age, baseline SBP and body mass index (BMI) were significant RFs for development of ISH; regarding IDH, baseline DBP and WC were identified as important RFs whereas age, female gender and marriage were shown to be protective factors (13).
3.3. Incidence and Predicting Risk Factors of Prehypertension
Based on the results of a study by Hadaegh et al. during median F/U of 9.2 years, 1440 new cases of preHTN (735 women and 705 men) were identified and the incidence rate was 593/10000 person-years (95% CI: 564 - 625). The incidence rate of preHTN among women [489/10000 person-years (95% CI: 455 - 526)] was significantly lower than men [764/10000 person-years, (95% CI: 709 - 822)], (P < 0001). During a median F/U of 5.9 years, 872 (432 women and 440 men) individuals had new events of preHTN, resulting in an incidence rate of 546/10000 person-years (95% CI: 511 - 584); incident rates for women and men were 443/10000 (95% CI: 404 - 487) and 715/10000 (95% CI: 651 - 786) person-years, respectively. Participants who developed incident preHTN were older and had higher numbers of cardiovascular RFs in both genders (14). Age, BMI and SBP were significant predictors of preHTN in the TLGS population and also in the sex-adjusted analysis. In both males and females, incident preHTN developed in those who were older, had higher body mass index (BMI), SBP, DBP, triglyceride (TG), total cholesterol (TC), fasting plasma glucose (FPG), and homeostasis model assessment-insulin resistance (HOMA-IR), but who had lower eGFR; 2-hour post-challenge plasma glucose (2h-PCPG) was an independent predictor only in men [HR (95% CI): 1.06 (1.01 - 1.12)], while waist-to-hip ratio (WHpR) and DBP were significant predictors only in women [HRs (95% CIs): 1.24 (1.11 - 1.39) and 1.04 (1.03 - 1.06), respectively]. Also, in the sex-adjusted model, female gender showed lower risk for incident preHTN [HR (95% CI): 0.81 (0.69 - 0.94)] Incident preHTN developed in women with lower HDL-C, compared to the non-incident group (14).
3.4. Dietary Intake of Nitrate and Nitrite and the Risk of Hypertension
In a median 5.8 year F/U of 2799 adults aged ≥ 20 years, multivariate logistic regression model was used to calculate the odds ratios of HTN across tertile categories of residual energy-adjusted NO3- and NO2- intakes. Mean (SD) intakes of dietary NO3- and NO2- were 455 (188) and 9.4 (3.6) mg/day, respectively. Overall, no significant relationship was found between dietary intake of NO3- and the risk of HTN. The highest intake (median intake ≥ 12.7 mg/day) of dietary NO2- was associated with reduced risk of HTN in comparison to the lowest tertile category (median intake < 6.04 mg/day) with an odds ratio (OR) of 0.58 (95% CI = 0.33 - 0.98; p for trend = 0.054) in a fully adjusted model (15).
3.5. Predictors of early Adulthood Hypertension
In the TLGS, 1579 subjects, aged 10 - 19 years were considered to evaluate the effects of adolescent anthropometric indices and some cardio metabolic risk factors on the development of adult HTN during 10 years of F/U (16). During F/U, 65 out of 1579 individuals developed HTN in their adulthood, indicating a cumulative incidence of 0.04 (95% CI: 0.03 - 0.05). Of these, 5 individuals were using antihypertensive drugs and 92.3% had systolic and/or diastolic HTN as unknown hypertensive subjects. Individuals who developed early adulthood HTN were one year older at baseline and had higher BMI, WC, wrist and hip circumferences, SBP, DBP, TGs and TC.
3.6. Trend of BP and HTN
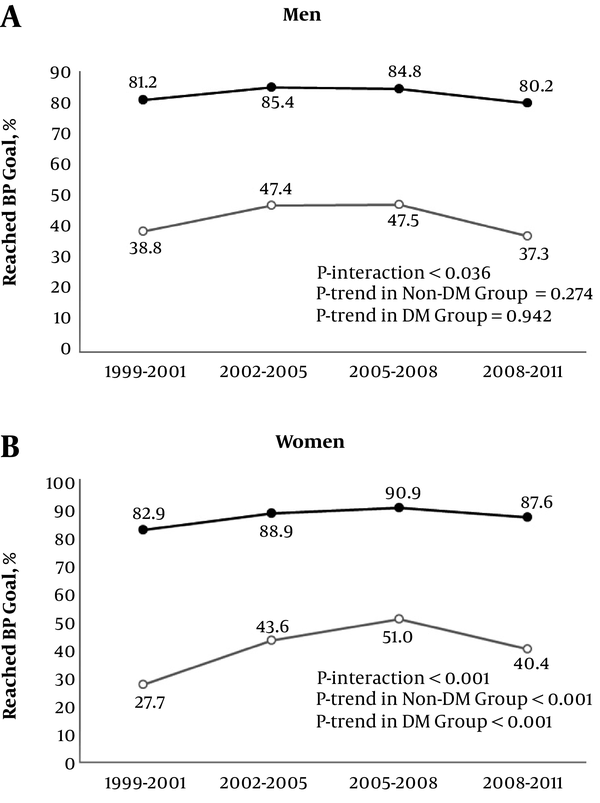
In 6181 participants, including 1045 individuals with DM, sex-stratified generalized estimation equation models were used to investigate trends of CVD risk factors during a decade long F/U from TLGS phase 1 to phase 4 (17). SBP decreased significantly in both diabetic (age-adjusted mean SBP of 134.81 and 137.92 mmHg in phase 1 vs. mean SBP of 130.27 and 130.32 mmHg in phase 4 for men and women, respectively) and non-diabetic participants (mean SBP of 120.97 and 118.51 mmHg in phase 1 vs. mean SBP of 118.12 and 111.74 mmHg in phase 4 for men and women, respectively). DBP showed a non-significant decrease in diabetic men and a statistically significant decrease in non-diabetic men. Among women, both individuals with and without DM generally experienced statistically significant decreases in DBP. Regarding BP control, both diabetic and non-diabetic men did not have any statistically significant changes in the BP control rates; however, women demonstrated 1.46 (27.67% to 40.43%) and 1.05 (82.94% to 87.58%) fold increases in the rate of BP control in diabetic and non-diabetic subjects, respectively (17). Figure 1 shows the age-adjusted prevalence of reached BP goal for diabetic and non-diabetic men and women.
Age-adjusted prevalence of controlled hypertension among diabetic and non-diabetic men and women in phases I-IV of the TLGS. Age-adjusted prevalence of controlled hypertension for diabetic and non-diabetic men (A) and women (B) were derived from data presented by Jahangiri-Noudeh, et al. (17). White circle = diabetic group; black circle = non-diabetic group; BP goal: systolic BP < 140 mmHg and diastolic BP < 90 mmHg (< 80 mmHg in diabetic subjects). DM, diabetes mellitus; BP, blood pressure; phase I (1999 - 2001), phase II (2002 - 2005), phase III (2005 - 2008), phase IV (2008 - 2012); TLGS, Tehran lipid and glucose study.
In a study by Hosseini-Esfahani et al. (10) data from 3 phases of the TLGS on 10 - 19 y/o adolescents was analysed to assess trends of CVD risk factors in this age group. Based on the findings of this study, mean SBP and DBP decreased from 1999 - 2001 to 2006 - 2008 in both age groups (10 - 14 year and 15 - 19 year) and both genders. In 10 - 14 y/o males, prevalence of high DBP and in 15 - 19 y/o ones, prevalence of high SBP decreased significantly over time. In females, prevalence of high DBP decreased significantly in both age groups.
Finally, regarding the older population of the TLGS, sex-stratified generalized estimation equation models were fitted in 1490 subjects, aged ≥ 60 years. During 8.76 years, age-adjusted mean SBP remained stable, while DBP levels increased in both genders. Meanwhile, the age-adjusted prevalence of HTN showed a remarkable upward trend in both genders, from 43% to 56% in men and 57% to 71% in women. However, at the end of F/U, 35% of hypertensive men and 23% of hypertensive women were not using antihypertensive medications (18).
3.7. Blood Pressure, Insulin Resistance and Type 2 Diabetes
Findings of a decade long study showed that neither SBP nor DBP were associated with insulin resistance and β-cell dysfunction in both genders (19). Likewise, both SBP and DBP were not determined as potential RFs for the incidence of prediabetes or its phenotypes in the TLGS population (20).
Considering RFs of incidence of type 2 diabetes (T2DM), Cox proportional hazard model showed that neither SBP nor DBP were associated with incident DM in the total population or in either gender separately (21). A principal component analysis regarding the effects of components of metabolic syndrome on the incident T2DM over 10 years of F/U (22), conducted on 1861 men and 2706 women aged 20 - 60 years, identified BP as one of three contributing RFs for the incidence of T2DM, which was 7.14% and 7.57% in men and women, respectively. Multivariate ORs (95% CI) of incident T2DM for the third versus the first tertile of BP were 2.23 (1.31 - 3.78) and 2.13 (1.34 - 3.40) in men and women, respectively. Regarding dichotomized definitions, high BP (≥ 130/85 mmHg) also had multivariate ORs (95% CI) of 1.47 (1.11 - 1.96) and 1.36 (1.02 - 1.81) for incident T2DM in men and women, respectively.
To investigate the impact of different combinations of glucose tolerance and BP status on the development of T2DM, 8231 individuals without diabetes at baseline were recruited (23). During a median follow-up of > 10 years, the overall incidence rate for T2DM was 12.2 per 1000 person-years. Compared to normal glucose tolerance/normal BP (NGT/NBP) as reference, multivariate adjusted HRs (95% CI) for incident T2DM were 1.34 (1.06 - 1.69), 6.44 (5.17 - 8.01), 7.22 (5.71 - 9.12) and 1.65 (1.26 - 2.17) for NGT/PreHTN, PreDM/PreHTN, PreDM/HTN and NGT/HTN, respectively. Results of the sensitivity analysis with multiple imputed baseline missing data and inverse probability weighting in the Cox regression analysis were approximately the same as the primary analyses.
3.8. Blood Pressure, Cardiovascular Disease and Mortality
Table 2 represents data regarding the associations of BP components as continuous variables (24) and different HTN phenotypes (25) with CVD and mortality in the middle-aged and older TLGS population, followed-up until March 2009. During a median F/U of 8.7 years in 5991 subjects, aged ≥ 30 years without baseline CVD or use of antihypertensive medication (24), after multivariate adjustment, except for DBP and mean arterial pressure [MAP: 1/3 (SBP + 2 × DBP)] with regard to all-cause mortality in individuals, aged ≥ 60 years, all BP components were predictive of CVD events and total mortality in middle-aged and elderly individuals. The discriminatory powers of all BP measures in multivariate models for CVD events and all-cause mortality, calculated by the C index, generally declined with increasing age. Regarding the fitness and discrimination of models, DBP, pulse pressure (PP: the difference between SBP and DBP) and MAP were not superior to SBP, supporting SBP predictability for CVD events and all-cause mortality, compared with other BP measures (24).
Multivariate-Adjusted Cox Proportional Hazard Ratios (95% CI) of a 1SD Increase in Each BP Components and HTN Phenotypes for Incident CVD and Mortality Outcomes in the Middle-Aged and Elderly Populationa,b,c
| CVD | All-Cause Mortality | CVD Mortality | |
|---|---|---|---|
| Middle-aged | |||
| SBP | 1.43 (1.26 - 1.61) | 1.67 (1.35 - 2.06) | NA |
| DBP | 1.24 (1.08 - 1.42) | 1.47 (1.11 - 1.94) | NA |
| PP | 1.39 (1.23 - 1.57) | 1.55 (1.24 - 1.93) | NA |
| MAP | 1.37 (1.20 - 1.56) | 1.62 (1.24 - 2.10) | NA |
| ISH | 1.52 (1.08 - 2.14) | 1.03 (0.50 - 2.09) | 0.96 (0.33 - 2.79) |
| IDH | 1.31 (0.90 - 1.91) | 2.01 (1.11 - 3.65) | 1.26 (0.38 - 4.15) |
| SDH | 1.52 (1.12 - 2.05) | 1.62 (0.95 - 2.75) | 1.70 (0.76 - 3.80) |
| CBP | 1.36 (0.85 - 2.18) | 1.10 (0.43 - 2.78) | 1.17 (0.27 - 5.06) |
| UBP | 3.09 (2.31 - 4.14) | 2.95 (1.78 - 4.88) | 5.67 (2.93 - 11.00) |
| Elderly | |||
| SBP | 1.38 (1.18 - 1.63) | 1.28 (1.04 - 1.56) | NA |
| DBP | 1.20 (1.00 - 1.44) | 1.05 (0.85 - 1.28) | NA |
| PP | 1.29 (1.10 - 1.51) | 1.29 (1.07 - 1.56) | NA |
| MAP | 1.33 (1.11 - 1.60) | 1.17 (0.95 - 1.44) | NA |
| ISH | 1.97 (1.33 - 2.91) | 1.45 (0.96 - 2.18) | 2.24 (1.19 - 4.21) |
| IDH | 1.65 (0.66 - 4.13) | 3.23 (1.46 - 7.16) | 3.80 (1.11 - 13.02) |
| SDH | 1.89 (1.20 - 2.98) | 2.01 (1.26 - 3.20) | 3.20 (1.60 - 6.42) |
| CBP | 1.14 (0.59 - 2.19) | 1.87 (1.04 - 3.37) | 2.86 (1.21 - 6.76) |
| UBP | 1.81 (1.17 - 2.80) | 1.15 (0.70 - 1.87) | 1.44 (0.65 - 3.17) |
During > 10 years F/U of 6974 participants aged 30 to < 65 years and 882 participants aged ≥ 65 years, 490 and 194 CVD events also 152 and 183 deaths occurred, respectively (25). In both middle-aged and elderly populations, ISH, systolic-diastolic HTN (SDH), and uncontrolled BP (UBP) increased CVD risk. Regarding mortality, findings revealed significant discrepancies; for all-cause mortality in the middle-aged group, IDH and UBP were significant predictors, whereas in the elderly group, IDH, SDH, and controlled BP (CBP) increased the risk. In middle-aged participants, only UBP was associated with incident CVD mortality and was the sole phenotype that was not an independent predictor of CVD death in the elderly. The notable finding of this study was the increased mortality risk in elderly patients with CBP (25).
Considering age-stratified analyses, the independent risk of CVD according to BP categories during 9.3 years of F/U, was assessed among 5064 middle-aged (30 to < 60 years) and 1209 elderly (≥ 60 years) participants of TLGS with no baseline CVD (26). Both high normal BP (SBP 130 - 139 mmHg or DBP 85 - 89 mmHg) and HTN were associated with incident CVD in the middle-aged participants [multivariate HRs (95% CI, P value): 1.62 (1.11 - 2.37, 0.013) and 2.20 (1.57 - 3.09, < 0.001), respectively]; however, in the eldely, high normal BP was not a CVD risk factor [HR (95% CI): 0.89 (0.51 - 1.54)], while HTN was associated with a HR (95% CI) of 2.09 (1.36 - 3.21) for CVD.
Parizadeh et al. investigated the association of changes in BP components between baseline examination (1999 - 2001) of the TLGS and the second examination (2002 - 2005) with incident CVD up to March 2012 (27). During a median F/U of 6 years after the second visit, 303 CVD events occurred among 3569 individuals. Each 1 SD increase in SBP, DBP and MAP was significantly associated with 21%, 22%, and 95% increased CVD risk after adjustments for baseline value of each BP component, SBP/DBP/PP/MAP change, and several other covariates (27).
During 9.3 years of F/U of 2548 participants without a history of CVD, aged ≥ 50 years, high BP as a component of the metabolic syndrome (MetS) was found to be associated with the incident CHD after adjustment for all MetS components (28); corresponding HRs (95% CI, P value) were 1.89 (1.42 - 2.51, < 0.001), 1.87 (1.44 - 2.43, < 0.001) and 1.89 (1.49 - 2.41, < 0.001), based on JIS, IDF and WHO definitions of MetS, respectively.
Two studies from the TLGS investigated HRs and population attributable fraction (PAF) of risk factors of CHD or CVD (29, 30); in 2889 men and 3803 women, aged 30 - 74 years, with no history of CVD at baseline, 11.9 and 6.5 CHD events per 1000 person-years occurred in men and women, respectively, during a median F/U duration of 10.3 years. HRs (95% CI) of HTN (SBP ≥ 140 mmHg or DBP ≥ 90 mmHg or taking HTN medication) for incident CHD were 1.8 (1.4 - 2.2) and 2.1 (1.6 - 2.8) in men and women, respectively. Average hypertension-related PAFs for CHD were 9.4 and 17.0% in men and women, respectively (29). With extension of F/U duration up to 2012, among 8108 participants without prevalent CVD, 827 first CVD events, including stroke, and 551 deaths occurred. Using multivariate Cox proportional hazard models with obesity mediators (DM, HTN, lipid profile and CKD), preHTN was not determined as a potential CVD or all-cause mortality RF; however, HTN had HRs (95% CI, P value) of 1.79 (1.46 - 2.19, < 0.0001) and 1.43 (1.11 - 1.84, 0.005) for CVD and all-cause mortality, respectively. Corresponding PAFs (95% CI) were 21.62% (14.49 - 28.79) and 17.13% (5.25 - 27.84) for CVD and all-cause mortality events, respectively (30).
In a recently-published article from the TLGS (31), sex-specific incidence rates and RFs of premature CVD, defined as having a CVD event before the age of 55 and 65 years in men and women, respectively, have been investigated during a median period of 11.74 years. Reported HRs (95% CI, P value) and PAFs (95% CI) related to HTN were 1.65 (0.97 - 2.81, 0.06) and 8.7% (-0.5% - 19.3%) in men and 1.54 (1.01 - 2.34, 0.04) and 16.8% (0.4% - 32.1%) in women. PreHTN was not recognized as a significant RF for premature CVD, either in men or in women.
Finally, results of a Cox proportional hazard model evaluating the effect of different combinations of BP and glucose tolerance status on CVD and all-cause mortality in 7619 participants, aged ≥ 30 years (32) reported that in a median F/U of 11.3 years, 696 CVD and 412 all-cause mortality events occurred in these participants with no baseline CVD. Based on the calculated multivariate HRs, all hypertensive phenotypes were significantly associated with CVD, CHD and mortality events, with the highest risk in participants with both HTN and DM. Moreover, preHTN and DM phenotype increased CVD risk by 71%. These findings underscore the importance of HTN with regard to CVD and mortality, regardless of glucose tolerance status (32).
3.9. Blood Pressure and Stroke
When looking at the findings of studies from TLGS related to BP and stroke in this section, it should be taken into account that in all of the above-mentioned studies about CVD events, stroke was included as one of the CVD outcomes. Here, we present data available on cerebrovascular events as a separate outcome.
In a study aimed at determining RFs for stroke, 1089 men and 1289 women aged ≥ 50 years were followed for 9.3 years (33). All cases of definite or possible stroke or transient ischemic attack (TIA) were included in the cerebrovascular accident (CVA/stroke) definition. For 69 CVA events, multivariate Cox proportional HR (95% CI, P value) and PAF related to HTN were 3.03 (1.76 - 5.22, < 0.001) and 48.6%, respectively. Cox analysis considering continuous variables revealed that each mmHg increase in SBP and DBP was associated with 13% and 55% increased risk of stroke, respectively. Similar results were reported for ischemic stroke (IS). Overall, among different modifiable and non-modifiable RFs, HTN showed the greatest PAF for stroke events.
During 9.3 years of F/U of 2548 participants, aged ≥ 50 years, without a history of CVD, high BP as a component of the metabolic syndrome (MetS) was associated with incident CVA after adjustment for all MetS components. Corresponding HRs (95% CI, P value) were 3.05 (1.46 - 6.34, 0.003), 3.48 (1.72 - 7.02, < 0.001) and 2.87 (1.63 - 5.06, < 0.001) based on JIS, IDF and WHO definitions of MetS, respectively (28).
Recently, a sophisticated survival tree model was used to explore interactions between risk factors of IS in 3088 TLGS participants, aged ≥ 50 years with 106 IS events during 12 years of F/U (34). Multivariate Cox proportional hazard model documented DBP as one of the RFs [1.04 (1.02 - 1.05)]. Based on the survival tree analysis, DBP was the most important predictor of IS not only in the middle aged but also in the elderly, such that the highest risk among both age groups was attributed to DBP ≥ 97 mmHg and DBP ≥ 100 mmHg, respectively. Overall, the highest and lowest risks identified by the survival tree were related to subjects ≥ 60.5 years with DBP ≥ 100 mmHg and subjects < 60.5 years with DBP < 97 mmHg, respectively (34).
3.10. Studies on BP in the Elderly as a Special Population
In addition to above-mentioned data regarding different aspects of BP and HTN in older adults of the TLGS as an age subgroup, there are a few studies considering the elderly as the only study population.
Mohebi et al. investigated CVD and mortality risk in 1845 participants, aged ≥ 60 years, free of baseline CVD, according to different BP categories (35). During a median F/U of 10 years, 380 CVD and 260 mortality events occurred. Cox proportional hazard regression was used with adjustment for age, sex, TC, HDL-C, current smoking, fasting plasma glucose, BMI, and WC. Compared to the reference group (those with SBP < 120 mmHg and DBP < 80 mmHg), individuals with 140 mmHg < SBP < 150 mmHg and DBP < 90 mmHg [HR (95% CI, P value): 1.79 (1.17 - 2.74), 0.007] and those with SBP ≥ 150 mmHg and/or DBP ≥ 90 mmHg mmHg [HR (95% CI, P value): 1.73 (1.24 - 2.42), 0.001] showed increased risk of CVD events (35). These findings emphasize the importance of SBP levels of 140 - 150 mmHg in the elderly population with regard to CVD outcomes.
To investigate the relationship between different anthropometric measures and their mediating factors with CVD and mortality in the elderly, 881 TLGS participants, aged ≥ 65 years and free of CVD at baseline were selected (36). During a median F/U of 9.5 years, 193 CVD events and 183 deaths occurred. The confounder- and mediator-adjusted Cox proportional hazard analysis showed that only central adiposity measures were associated with a significantly increased risk of CVD/CHD and among all of the mediators including hypercholesterolemia, DM and HTN, HTN had the most impact, accounting for 30% - 45% of the excess risk of central adiposity measures for CVD events.
3.11. BP and Chronic Kidney Disease
Based on the Tohidi et al. study regarding the incidence and RFs of CKD (eGFR < 60 mL/min/1.73 m2) in the TLGS population during a mean F/U of 9.9 years, high normal BP and HTN were determined as significant RFs for incident CKD, only in men; corresponding ORs (95% CI, P value) were 1.74 (0.99 - 3.04, 0.05) and 2.20 (1.38 - 3.52, 0.001), respectively (36).
4. Conclusions
According to data regarding the prevalence and incidence of preHTN and HTN reported in the aforementioned studies and their contribution to cardiovascular morbidity and mortality in the TLGS population as a representative sample of Tehranian population, it is recommended that interventions be prioritized for lifestyle modifications for the prevention and appropriate management of preHTN/HTN.
Moreover, further studies considering the associations between BP in adolescents and the long term incidence of hard outcomes as well as randomized controlled trials on the effects of control of modifiable risk factors of HTN and proper management and monitoring of BP are warranted.
Acknowledgements
References
-
1.
Global Burden of Metabolic Risk Factors for Chronic Diseases Collaboration. Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: A comparative risk assessment. Lancet Diabetes Endocrinol. 2014;2(8):634-47. [PubMed ID: 24842598]. [PubMed Central ID: PMC4572741]. https://doi.org/10.1016/S2213-8587(14)70102-0.
-
2.
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: Analysis of worldwide data. Lancet. 2005;365(9455):217-23. [PubMed ID: 15652604]. https://doi.org/10.1016/S0140-6736(05)17741-1.
-
3.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population-based measurement studies with 19.1 million participants. Lancet. 2017;389(10064):37-55. [PubMed ID: 27863813]. [PubMed Central ID: PMC5220163]. https://doi.org/10.1016/S0140-6736(16)31919-5.
-
4.
Esteghamati A, Etemad K, Koohpayehzadeh J, Abbasi M, Meysamie A, Khajeh E, et al. Awareness, Treatment and Control of Pre-hypertension and Hypertension among Adults in Iran. Arch Iran Med. 2016;19(7):456-64. [PubMed ID: 27362238].
-
5.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903-13. [PubMed ID: 12493255]. https://doi.org/10.1016/S0140-6736(02)11911-8.
-
6.
Rapsomaniki E, Timmis A, George J, Pujades-Rodriguez M, Shah AD, Denaxas S, et al. Blood pressure and incidence of twelve cardiovascular diseases: Lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet. 2014;383(9932):1899-911. [PubMed ID: 24881994]. [PubMed Central ID: PMC4042017]. https://doi.org/10.1016/S0140-6736(14)60685-1.
-
7.
Ninomiya T, Perkovic V, Turnbull F, Neal B, Barzi F; Blood Pressure Lowering Treatment Trialists' Collaboration, et al. Blood pressure lowering and major cardiovascular events in people with and without chronic kidney disease: Meta-analysis of randomised controlled trials. BMJ. 2013;347:f5680. [PubMed ID: 24092942]. [PubMed Central ID: PMC3789583]. https://doi.org/10.1136/bmj.f5680.
-
8.
Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. Lancet. 2016;387(10022):957-67. [PubMed ID: 26724178]. https://doi.org/10.1016/S0140-6736(15)01225-8.
-
9.
Azizi F, Rahmani M, Emami H, Mirmiran P, Hajipour R, Madjid M, et al. Cardiovascular risk factors in an Iranian urban population: Tehran lipid and glucose study (phase 1). Soz Praventivmed. 2002;47(6):408-26. [PubMed ID: 12643001]. https://doi.org/10.1007/s000380200008.
-
10.
Hosseini-Esfahani F, Mousavi Nasl Khameneh A, Mirmiran P, Ghanbarian A, Azizi F. Trends in risk factors for cardiovascular disease among Iranian adolescents: The Tehran lipid and glucose study, 1999-2008. J Epidemiol. 2011;21(5):319-28. [PubMed ID: 21804294]. [PubMed Central ID: PMC3899430]. https://doi.org/10.2188/jea.JE20100162.
-
11.
Azizi F, Emami H, Salehi P, Ghanbarian A, Mirmiran P, Mirbolooki M, et al. Cardiovascular risk factors in the elderly: The Tehran lipid and glucose study. J Cardiovasc Risk. 2003;10(1):65-73. [PubMed ID: 12569239]. https://doi.org/10.1097/01.hjr.0000050202.47754.1b.
-
12.
Bozorgmanesh M, Hadaegh F, Mehrabi Y, Azizi F. A point-score system superior to blood pressure measures alone for predicting incident hypertension: Tehran lipid and glucose study. J Hypertens. 2011;29(8):1486-93. [PubMed ID: 21720268]. https://doi.org/10.1097/HJH.0b013e328348fdb2.
-
13.
Asgari S, Khalili D, Mehrabi Y, Kazempour-Ardebili S, Azizi F, Hadaegh F. Incidence and risk factors of isolated systolic and diastolic hypertension: A 10 year follow-up of the Tehran Lipids and Glucose Study. Blood Press. 2016;25(3):177-83. [PubMed ID: 26643588]. https://doi.org/10.3109/08037051.2015.1116221.
-
14.
Hadaegh F, Hasheminia M, Abdi H, Khalili D, Bozorgmanesh M, Arshi B, et al. Prehypertension tsunami: A decade follow-up of an Iranian adult population. PLoS One. 2015;10(10). e0139412. [PubMed ID: 26439847]. [PubMed Central ID: PMC4595371]. https://doi.org/10.1371/journal.pone.0139412.
-
15.
Bahadoran Z, Mirmiran P, Ghasemi A, Carlstrom M, Azizi F, Hadaegh F. Association between dietary intakes of nitrate and nitrite and the risk of hypertension and chronic kidney disease: Tehran lipid and glucose study. Nutrients. 2016;8(12). [PubMed ID: 28009811]. [PubMed Central ID: PMC5188466]. https://doi.org/10.3390/nu8120811.
-
16.
Kalantari S, Khalili D, Asgari S, Fahimfar N, Hadaegh F, Tohidi M, et al. Predictors of early adulthood hypertension during adolescence: A population-based cohort study. BMC Public Health. 2017;17(1):915. [PubMed ID: 29183297]. [PubMed Central ID: PMC5706303]. https://doi.org/10.1186/s12889-017-4922-3.
-
17.
Jahangiri-Noudeh Y, Akbarpour S, Lotfaliany M, Zafari N, Khalili D, Tohidi M, et al. Trends in cardiovascular disease risk factors in people with and without diabetes mellitus: A Middle Eastern cohort study. PLoS One. 2014;9(12). e112639. [PubMed ID: 25461381]. [PubMed Central ID: PMC4251920]. https://doi.org/10.1371/journal.pone.0112639.
-
18.
Eslami A, Lotfaliany M, Akbarpour S, Azizi F, Hadaegh F. Trend of cardiovascular risk factors in the older Iranian population: 2002-2014. Geriatr Gerontol Int. 2018;18(1):130-7. [PubMed ID: 28857406]. https://doi.org/10.1111/ggi.13154.
-
19.
Derakhshan A, Tohidi M, Hajebrahimi MA, Saadat N, Azizi F, Hadaegh F. Sex-specific incidence rates and risk factors of insulin resistance and beta-cell dysfunction: A decade follow-up in a Middle Eastern population. Diabet Med. 2017;34(2):245-52. [PubMed ID: 26996519]. https://doi.org/10.1111/dme.13117.
-
20.
Hadaegh F, Derakhshan A, Zafari N, Khalili D, Mirbolouk M, Saadat N, et al. Pre-diabetes tsunami: Incidence rates and risk factors of pre-diabetes and its different phenotypes over 9 years of follow-up. Diabet Med. 2017;34(1):69-78. [PubMed ID: 26606421]. https://doi.org/10.1111/dme.13034.
-
21.
Derakhshan A, Sardarinia M, Khalili D, Momenan AA, Azizi F, Hadaegh F. Sex specific incidence rates of type 2 diabetes and its risk factors over 9 years of follow-up: Tehran lipid and glucose study. PLoS One. 2014;9(7). e102563. [PubMed ID: 25029368]. [PubMed Central ID: PMC4100911]. https://doi.org/10.1371/journal.pone.0102563.
-
22.
Ayubi E, Khalili D, Delpisheh A, Hadaegh F, Azizi F. Factor analysis of metabolic syndrome components and predicting type 2 diabetes: Results of 10-year follow-up in a Middle Eastern population. J Diabetes. 2015;7(6):830-8. [PubMed ID: 25492310]. https://doi.org/10.1111/1753-0407.12252.
-
23.
Derakhshan A, Bagherzadeh-Khiabani F, Arshi B, Ramezankhani A, Azizi F, Hadaegh F. Different combinations of glucose tolerance and blood pressure status and incident diabetes, hypertension, and chronic kidney disease. J Am Heart Assoc. 2016;5(8). [PubMed ID: 27543801]. [PubMed Central ID: PMC5015306]. https://doi.org/10.1161/JAHA.116.003917.
-
24.
Hadaegh F, Shafiee G, Hatami M, Azizi F. Systolic and diastolic blood pressure, mean arterial pressure and pulse pressure for prediction of cardiovascular events and mortality in a Middle Eastern population. Blood Press. 2012;21(1):12-8. [PubMed ID: 21679012]. https://doi.org/10.3109/08037051.2011.585808.
-
25.
Lotfaliany M, Akbarpour S, Mozafary A, Boloukat RR, Azizi F, Hadaegh F. Hypertension phenotypes and incident cardiovascular disease and mortality events in a decade follow-up of a Middle East cohort. J Hypertens. 2015;33(6):1153-61. [PubMed ID: 25699976]. https://doi.org/10.1097/HJH.0000000000000540.
-
26.
Hadaegh F, Mohebi R, Khalili D, Hasheminia M, Sheikholeslami F, Azizi F. High normal blood pressure is an independent risk factor for cardiovascular disease among middle-aged but not in elderly populations: 9-year results of a population-based study. J Hum Hypertens. 2013;27(1):18-23. [PubMed ID: 22217674]. https://doi.org/10.1038/jhh.2011.112.
-
27.
Parizadeh D, Ghahvehchian H, Asgari S, Momenan AA, Azizi F, Hadaegh F. The association between changes in blood pressure components and incident cardiovascular diseases. Blood Press. 2017;26(6):341-9. [PubMed ID: 28708028]. https://doi.org/10.1080/08037051.2017.1353882.
-
28.
Hadaegh F, Mohebi R, Cheraghi L, Tohidi M, Moghaddam NB, Bozorogmanesh M, et al. Do different metabolic syndrome definitions predict cerebrovascular events and coronary heart disease independent of their components?: 9 years follow-up of the tehran lipid and glucose study. Stroke. 2012;43(6):1669-71. [PubMed ID: 22382161]. https://doi.org/10.1161/STROKEAHA.112.650812.
-
29.
Khalili D, Sheikholeslami FH, Bakhtiyari M, Azizi F, Momenan AA, Hadaegh F. The incidence of coronary heart disease and the population attributable fraction of its risk factors in Tehran: A 10-year population-based cohort study. PLoS One. 2014;9(8). e105804. [PubMed ID: 25162590]. [PubMed Central ID: PMC4146560]. https://doi.org/10.1371/journal.pone.0105804.
-
30.
Sardarinia M, Akbarpour S, Lotfaliany M, Bagherzadeh-Khiabani F, Bozorgmanesh M, Sheikholeslami F, et al. Risk factors for incidence of cardiovascular diseases and all-cause mortality in a Middle Eastern population over a decade follow-up: Tehran lipid and glucose study. PLoS One. 2016;11(12). e0167623. [PubMed ID: 27930696]. [PubMed Central ID: PMC5145170]. https://doi.org/10.1371/journal.pone.0167623.
-
31.
Eslami A, Mozaffary A, Derakhshan A, Azizi F, Khalili D, Hadaegh F. Sex-specific incidence rates and risk factors of premature cardiovascular disease. A long term follow up of the Tehran lipid and glucose study. Int J Cardiol. 2017;227:826-32. [PubMed ID: 27829526]. https://doi.org/10.1016/j.ijcard.2016.10.037.
-
32.
Hajebrahimi MA, Akbarpour S, Eslami A, Azizi F, Hadaegh F. Different combinations of glucose tolerance and blood pressure status and incident cardiovascular disease and all-cause mortality events. J Hum Hypertens. 2017;31(11):744-9. [PubMed ID: 28748918]. https://doi.org/10.1038/jhh.2017.49.
-
33.
Fahimfar N, Khalili D, Mohebi R, Azizi F, Hadaegh F. Risk factors for ischemic stroke; results from 9 years of follow-up in a population based cohort of Iran. BMC Neurol. 2012;12:117. [PubMed ID: 23031547]. [PubMed Central ID: PMC3517457]. https://doi.org/10.1186/1471-2377-12-117.
-
34.
Parizadeh D, Ramezankhani A, Momenan AA, Azizi F, Hadaegh F. Exploring risk patterns for incident ischemic stroke during more than a decade of follow-up: A survival tree analysis. Comput Methods Programs Biomed. 2017;147:29-36. [PubMed ID: 28734528]. https://doi.org/10.1016/j.cmpb.2017.06.006.
-
35.
Mohebi R, Mohebi A, Ghanbarian A, Momenan A, Azizi F, Hadaegh F. Is systolic blood pressure below 150 mm Hg an appropriate goal for primary prevention of cardiovascular events among elderly population? J Am Soc Hypertens. 2014;8(7):491-7. [PubMed ID: 25064771]. https://doi.org/10.1016/j.jash.2014.04.010.
-
36.
Kazempour-Ardebili S, Ramezankhani A, Eslami A, Akbarpour S, Azizi F, Hadaegh F. Metabolic mediators of the impact of general and central adiposity measures on cardiovascular disease and mortality risks in older adults: Tehran lipid and glucose study. Geriatr Gerontol Int. 2017;17(11):2017-24. [PubMed ID: 28349639]. https://doi.org/10.1111/ggi.13015.



