|
Case Report
Microvascular injury in the appendix of a pediatric patient with history of COVID-19 infection: A case report
1 Senior Histopathology resident, Pathology Department, Salmaniya Medical Complex, Manama, Kingdom of Bahrain
2 Senior Histopathology consultant, Pathology Department, Salmaniya Medical Complex, Manama, Kingdom of Bahrain
Address correspondence to:
Maryam Fadhel Hammad
Villa 2006, Road 5059, Block 450, Manama,
Kingdom of Bahrain
Message to Corresponding Author
Article ID: 100101Z06MH2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Hammad MF, Malik AK. Microvascular injury in the appendix of a pediatric patient with history of COVID-19 infection: A case report. Case Rep Int 2021;10:100101Z06MH2021.ABSTRACT
Introduction: A novel coronavirus (SARS-CoV-2) infection has emerged in the world causing a pandemic disease with severe forms of acute respiratory failure along with other organs manifestations. Besides, frequent association with multisystem inflammatory syndrome in children (MIS-C) as complication after the recovery has been recorded. Hereby we report the histological findings in the appendix of a female pediatric patient with history of COVID-19 infection.
Case Report: In our case, an 8-year-old female patient presented to the emergency department of our main tertiary hospital in Bahrain with two days history of low grade fever, lower abdominal pain, nausea, and vomiting. She was admitted to the pediatric surgical unit for a suspected acute appendicitis. A diagnostic laparoscopy and laparoscopic appendectomy was performed. The appendix was sent to the histopathology examination which confirmed the diagnosis of acute suppurative appendicitis with focal endarteritis obliterans. Retrospectively history revealed the child was COVID-19 positive three months back.
Conclusion: Microvascular injury in the appendix of our case adds to the preliminary available evidences in the literature indicating that endarteritis obliterans of the gastrointestinal (GI) tract organs could be a complication of the COVID-19 virus infection like in MIS-C which is a known post-infectious complication of the virus.
Keywords: Acute respiratory failure, Appendicitis, Appendectomy, COVID-19, Laparoscopy, Multisystem inflammatory syndrome in children (MIS-C), Safety, SARS-CoV-2, Surgery
INTRODUCTION
In late November to December 2019, in Wuhan (China), healthcare workers in some local hospitals noticed increase cases of interstitial pneumonia of unknown cause. In early January2020, the Chinese Center for Disease Control announced the case of the reported cases with these symptoms and it was the identification of a novel coronavirus (SARS-CoV-2) [1], after that, in March 11, World Health Organization declared it as a new pandemic disease (COVID-19) [1].
COVID-19 in more prevalent in male patients (around 60%), with a median age of about 50 years; most of them (40%) develops a severe form of acute respiratory distress syndrome leading to acute respiratory failure, with 5% of the patients requiring intensive care [2],[3]. The most common initial symptoms are fever followed by dry cough, upper respiratory tract infection symptoms, loss of smell and Taste, along with shortness of breath, dyspnea, chest pain, fatigue, and myalgia [4]. Less common symptoms include headache, dizziness, abdominal pain, diarrhea, nausea, and vomiting [4].
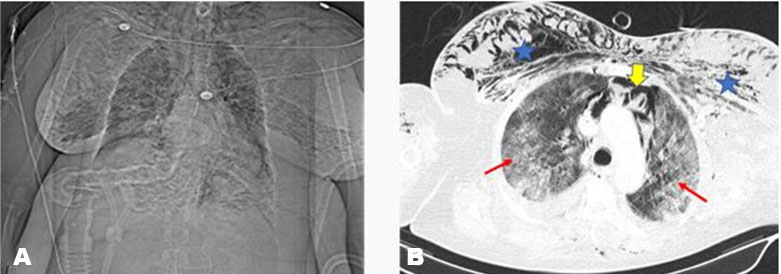
Approximately 75% of patients show bilateral lung infiltrates on chest X-ray and eventually developing what is called a COVID pneumonia [5].
In children, COVID-19 infection is usually causing mild symptoms similar to common cold or acute gastroenteritis. However, in rare cases, children can be exhibit severe symptoms, and their clinical manifestations may differ from adults. In some children, COVID-19 viral infection may present with a picture similar to incomplete Kawasaki disease (KD) or toxic shock syndrome [1],[3],[6] with sudden and un-explained vasculitis, myocarditis, or ischemic bowel syndrome. This condition has been labeled as multisystem inflammatory syndrome in children (MIS-C) which refers to a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 either at the time of the infection or after recovery with time range of 3–4 weeks.
Recently, more studies are being done over the histopathological findings of the resected organs from patients with history of COVID-19 infection. The emphasis is on the inflammatory response and the microvascular injury that can be seen in these organs such as the appendix, gallbladder, and even brain in patients who are affected or has been affected by COVID-19 virus [2]. In our case report, we demonstrate the histological findings of the appendix in a pediatric patient who had a history of a COVID-19 infection prior to the operation with three months.
CASE REPORT
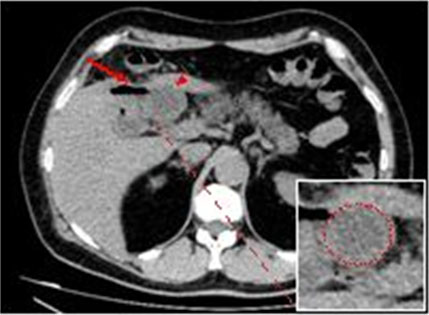
On 23rd January 2020, an 8-year-old female (26 kg of actual body weight) a known case of B-Thalassemia trait was admitted in our main tertiary care hospital (Salmaniya Medical Complex) with two days history of lower abdominal pain, mainly in right iliac fossa, fever, nausea, and vomiting. She was admitted to the pediatric surgical unit for a suspected acute appendicitis. The patient initial labs were as the following: white blood cell (WBC) count (12.25×109/L), red blood cell (RBC) count (5.45×1012/L), hemoglobin (11.0g/dL), neutrophils (80.8%), and neutrophils absolute count (10×109/L), glucose (random) 4.0 mmol/L, urea 6.3 mmol/L, creatinine 33.00 μmol/L. Her electrolytes were within normal limits and her urine test was normal as well. She was taken for an abdominal and a pelvic ultrasound scan and the test concluded that the patient has a dilated appendix surrounded by minimal fluid, fat stranding, and mesenteric lymphadenopathy (Figure 1), these findings are consistent with acute appendicitis.
After that, the patient was admitted to the pediatric surgical ward, kept on intravenous (IV) hydration and antibiotics and due to worsening symptoms, a laparoscopy was performed the next day and intraoperative findings confirm the diagnosis of acute appendicitis with no gangrene or perforation. Laparoscopic appendectomy was performed without complications. The appendix was sent for the histopathology examination.
Before surgery, nasopharyngeal swabs for detection of SARS-CoV-2 were performed. All swabs resulted negative for SARS-CoV-2 infection.
However, the patient history was significant for a SARS-CoV-2 infection on September 26, 2020. The patient had mild upper respiratory tract symptoms which required no hospitalization at that time. She recovered from the infection uneventfully.
Histological and immunohistochemistry studies and morphometrical assay
The histological diagnosis was made on hematoxylin & eosin-stained slides along with periodic acid–Schiff (PAS), Grocott methenamine silver (GMS), and elastic stained slides. Sections of the sampled tissue were evaluated through light microscopy (Olympus, CX41).
Histological findings
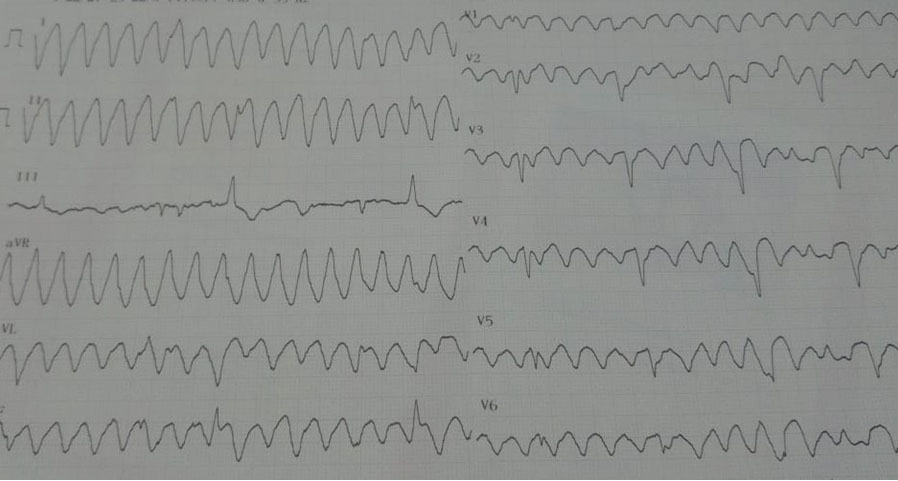
Hematoxylin & eosin-stained slides display appendix with focal mucosal ulcerations, transmural neutrophilic infiltration with extension to serosa and mesoappendiceal fat. Submucosal appendicular vessels and the medium-sized vessels in the mesoappendix reveal acute neutrophilic inflammation with fibrinoid necrosis in their walls (Figure 2A, Figure 2B, Figure 2C). No parasite, viral cytopathy, or granuloma is noted.
Slides with special stains also add on the diagnosis of acute suppurative appendicitis with focal endarteritis obliterans as evident by fibrin thrombus and focal inflammation in the media of the blood vessels.
DISCUSSION
Coronaviruses are enveloped, nonsegmented, single-stranded, RNA viruses named after their corona- or crown-like surface projections seen with electron microscopy corresponding to large surface spike proteins [7].
There are four distinct genera: Alphacoronavirus, Betacoronavirus, Gammacoronavirus, and Deltacoronavirus.
SARS-CoV-2 is a recently described member of the Betacoronoravirus family (lineage B). All strains of this virus are known to bind and fuse with angiotensin converting enzyme-2 (ACE-2) receptors. These receptors are expressed throughout the respiratory tract as well as the GI tract, hence the common pulmonary and less frequent GI manifestations [7],[8]. The disease pathogenesis is currently thought to be explained by activation of the spike proteins at the receptor sites [7] and subsequent immune system activation, followed by the appearance of the symptoms.
In the literature, many experiments confirmed that SARS-CoV-2 can infect and replicate in enterocytes [9], and also SARS-CoV-2 was demonstrated in stool specimen. In one study, SARS-CoV-2 was detected within enterocytes in biopsies taken from the esophagus, stomach, duodenum, and rectum of COVID-19 patients with severe disease [9]. But there is limited information regarding COVID-19 and acute appendicitis.
In general, vasculitis involving the gastrointestinal tract is most commonly associated with medium-vessel vasculitis, such as polyarteritis nodosa, and usually occurs as part of the systemic vasculitis process [5]. In children, vasculitis in the appendix is mainly associated with other systemic diseases such as systemic lupus erythematosus (SLE) or other autoimmune diseases [1]. Anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV) is being the most probable disease that can manifest with such histopathological picture as we have in our case. However, it is unlikely the case where the patient had negative previous history of the disease and in the absence of an overt vasculitic process in other organs.
Another probable cause of the focal endarteritis obliterans with fibrin thrombus and focal inflammation in the media of the blood vessels observed in our case that this is a part of the severe acute inflammation taking part in the appendix. However, in the recent outbreaks of the COVID-19 pandemic, many countries reported cases with vasculitis or a microvascular injury in the GI tract and the various organs of the body including brain [10], in patients whom has a history of COVID-19 virus infection with an average of three- to four-week lag—can be up to 12 weeks lag, like in our case—between the infection and the manifestation of the vasculitis episode [1]. Moreover, the findings of acute vasculitis with fibrinoid necrosis in the medium vessels of the submucosa and the mesentery of the appendix indicate that this is a systemic response [11] and it could be not only a local response to the severe appendicular inflammation that the patient is going through. This observation drags the attention to the new evolving syndrome referred as MIS-C.
Multisystem inflammatory syndrome in children (MIS-C) is uncommon but serious disease with multisystem involvement and a hallmark of microvascular injuries in multiple organs which can cause sudden death or a long term disability in some cases. It is an evolving syndrome that is observed to develop in patients who are affected by severe acute respiratory syndrome caused by coronavirus 2 (SARS-CoV-2), or who have recovered from it [11].
Clinical findings of this syndrome are similar to that of Kawasaki’s disease, with sudden fever—most of the time of unknown origin—and multisystem inflammation including heart, lungs, kidneys, liver, skin, eyes, brain, and the GI tracts [3],[5],[12],[13],[14]. As of now, GI involvement appears to be the predominate pattern in MIS-C and seen in 92% of patients [9]. These GI symptoms sometimes mimic infectious GI etiologies, as well as inflammatory bowel diseases, or ischemic bowel disease.
The diagnosis of MIS-C has critical and specific criteria, developed by the WHO. However, it is not very specific in most of the cases [1] leading to underestimation of the prevalence of this disease worldwide albeit the increased number of suspected cases with this diagnosis in many countries of the world that have raised COVID-19 incidence in the pediatric population.
The treatment of the syndrome is not concrete. Supportive medical treatment can sometimes help subside the patient’s symptoms if it is manageable. However, if the patient is presenting with a condition needs surgical intervention—acute appendicitis or acute ischemic bowel—the medical treatment will no longer be the choice. So definite treatment of MIS-C depends on the presenting symptoms of the patient.
Pathologic examination of the resected specimen is crucial. In our case, the appendix revealed histological findings that were concordant with the diagnosis of acute suppurative appendicitis. However, the microvascular injury which was found in the submucosal blood vessels was unusual for the patient’s age and unremarkable medical history for any autoimmune or rheumatic diseases and it is probably more related to her past infection with COVID-19 virus.
CONCLUSION
The histopathological features and specifically the microvascular injury of the appendectomy specimen of our case is in concordance and adds to the preliminary available evidences in the literature indicating that endarteritis obliterans or a microvascular injury of the GI tract organs in general, specially the appendix and the gallbladder could be a complication of the COVID-19 virus infection. It also could be a contributory element in the MIS-C which is known as a post-infectious complication of the virus in children age group.
REFERENCE
1.
2.
Hammoud H, Bendari A, Bendari T, Bougmiza I. Histopathological findings in COVID-19 cases: A systematic review. medRxiv 2020. [CrossRef]

3.
Campanile FC, Podda M, Arezzo A, et al. Acute cholecystitis during COVID-19 pandemic: A multisocietary position statement. World J Emerg Surg 2020;15(1):38. [CrossRef]
[Pubmed]

4.
Ahsan T, Rani B. A case of multisystem inflammatory syndrome post-COVID-19 infection in an adult. Cureus 2020;12(12):e11961. [CrossRef]
[Pubmed]

5.
Leaver PJ, Jang HS, Wong MG, Soh HC, Fernando SL. ANCA-associated vasculitis of the appendix. Rheumatol Adv Pract 2019;3(2):rkz037. [CrossRef]
[Pubmed]

6.
Bruni A, Garofalo E, Zuccalà V, et al. Histopathological findings in a COVID-19 patient affected by ischemic gangrenous cholecystitis. World J Emerg Surg 2020;15(1):43. [CrossRef]
[Pubmed]

7.
Ma Y, Deutsch G, Van Tassel D, et al. SARS-CoV-2 related ischemic colitis in an adolescent with trisomy 21: Diagnostic pitfalls and considerations. Pediatr Dev Pathol 2021:10935266211015666. [CrossRef]
[Pubmed]

8.
Trottein F, Sokol H. Potential causes and consequences of gastrointestinal disorders during a SARS-CoV-2 Infection. Cell Rep 2020;32(3):107915. [CrossRef]
[Pubmed]

9.
Wolf B, Pietsch C, Radosa MP, Horn LC, Liebert UG, Aktas B. No SARS-CoV-2 detected in the vermiform appendix of a COVID-19 patient with appendicitis: A case report. 2020. [CrossRef]

10.
Lee MH, Perl DP, Nair G, et al. Microvascular injury in the brains of patients with Covid-19. N Engl J Med 2021;384(5):481–3. [CrossRef]
[Pubmed]

11.
Jackson RJ, Chavarria HD, Hacking SM. A case of multisystem inflammatory syndrome in children mimicking acute appendicitis in a COVID-19 pandemic area. Cureus 2020;12(9):e10722. [CrossRef]
[Pubmed]

12.
Hanley B, Naresh KN, Roufosse C, et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: A post-mortem study. Lancet Microbe 2020;1(6):e245–53. [CrossRef]
[Pubmed]

13.
AbdulRahman A, AlAli S, Yaghi O, et al. COVID-19 and sickle cell disease in Bahrain. Int J Infect Dis 2020;101:14–6. [CrossRef]
[Pubmed]

14.
Deshmukh V, Motwani R, Kumar A, Kumari C, Raza K. Histopathological observations in COVID-19: A systematic review. J Clin Pathol 2021;74(2):76–83. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Acknowledgement
Acknowledgments for the I-Seha System technical staff and radiology department for the contribution of retrieving labs and reports.
Author ContributionsMaryam Fadhel Hammad - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ashok Kumar Malik - Conception of the work, Design of the work, Acquisition of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Maryam Fadhel Hammad et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.