Published online Jul 26, 2015. doi: 10.4330/wjc.v7.i7.404
Peer-review started: February 26, 2015
First decision: March 20, 2015
Revised: April 9, 2015
Accepted: April 28, 2015
Article in press: April 30, 2015
Published online: July 26, 2015
The role of blood cholesterol levels in coronary heart disease (CHD) and the true effect of cholesterol-lowering statin drugs are debatable. In particular, whether statins actually decrease cardiac mortality and increase life expectancy is controversial. Concurrently, the Mediterranean diet model has been shown to prolong life and reduce the risk of diabetes, cancer, and CHD. We herein review current data related to both statins and the Mediterranean diet. We conclude that the expectation that CHD could be prevented or eliminated by simply reducing cholesterol appears unfounded. On the contrary, we should acknowledge the inconsistencies of the cholesterol theory and recognize the proven benefits of a healthy lifestyle incorporating a Mediterranean diet to prevent CHD.
Core tip: Traditional efforts to prevent cardiovascular disease have emphasized the benefits of cholesterol lowering and statin drugs. Often overlooked is the fact that numerous studies of cholesterol lowering have failed to demonstrate a mortality benefit and the benefits of statins may have been overstated. The Mediterranean diet has consistently lowered cardiovascular events and mortality in numerous studies and does not typically lower cholesterol levels. Alternative theories of atherosclerosis are independent of cholesterol metabolism and may provide the key to future preventive strategies.
- Citation: DuBroff R, de Lorgeril M. Cholesterol confusion and statin controversy. World J Cardiol 2015; 7(7): 404-409
- URL: https://www.wjgnet.com/1949-8462/full/v7/i7/404.htm
- DOI: https://dx.doi.org/10.4330/wjc.v7.i7.404
Nearly twenty years ago two landmark randomized clinical trials appeared in The Lancet which forever changed the course of medicine for patients with coronary heart disease (CHD). The 4S study employed a cholesterol-lowering statin drug and reported a 30% mortality reduction[1]. The Lyon Diet Heart Study utilized the Mediterranean diet and reported a 70% mortality reduction[2]. Subsequent studies of the Mediterranean diet have confirmed these findings and also shown a reduced risk of cancer, diabetes, and Alzheimer’s disease[3-6]. Subsequent statin studies have led the United States Food and Drug Administration to issue warnings regarding the increased risk of diabetes and decreased cognition with statin drugs. Paradoxically, statins have gone on to become a multi-billion dollar industry and the foundation of many cardiovascular disease prevention guidelines while the Mediterranean diet has often been ignored. We believe this statin-centric cholesterol-lowering approach to preventing CHD may be misguided.
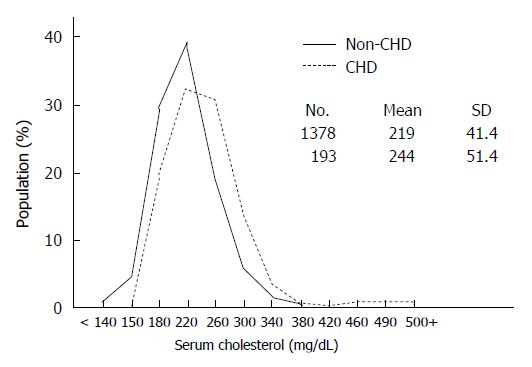
The cholesterol hypothesis links cholesterol intake and blood levels to cardiovascular disease. Because cholesterol is considered a risk factor for atherosclerosis many believe that lowering cholesterol in the blood is the best way to prevent CHD. Ideally, risk factors should help us distinguish those who will develop a disease from those who will not. However, if one examines the original Framingham Heart Study data (as an example) it is clear that the cholesterol levels of those who developed CHD and those who did not overlap except when the total cholesterol level exceeded 380 mg/dL or was less than 150 mg/dL (Figure 1). Moreover, cholesterol may be associated with CHD but that does not prove causation. Despite the fact that high triglycerides and low HDL have long been associated with CHD, studies designed to raise HDL or lower triglycerides have failed to reduce CHD mortality. Similarly, cholesterol should not automatically become a treatment target. It may be a leap of faith to assume that lowering cholesterol is the best way to prevent CHD.
The rare occurrence of CHD in isolated, rural societies such as Tukisenta, New Guinea has been attributed to low cholesterol levels[7]. However, it is equally plausible that the diets and lifestyles of these individuals may protect them from CHD. While we may never be certain if low cholesterol or a healthy lifestyle (or both) are responsible for preventing CHD in these societies, there is ample evidence that lowering cholesterol does not consistently lower CHD mortality. Reducing cholesterol blood levels by reducing dietary saturated fats is commonly recommended, but an exhaustive review and meta-analysis of 72 dietary studies concluded that reduced consumption of saturated fat does not reduce cardiovascular mortality[8]. Many drugs such as niacin, fibrates, and bile acid sequestrants can lower cholesterol levels, but the recent AHA/ACC guidelines on cholesterol concluded that these drugs do not lower CHD mortality rates[9]. Moreover, the results of cholesterol-lowering statin trials, as will be discussed and analyzed later, do not consistently lower mortality rates[10]. Consider also the dramatic mortality benefit of the Mediterranean diet in the Lyon Diet Heart Study which was achieved without a reduction in cholesterol levels[2-4]. Thus, the hypothesis that lowering cholesterol lowers mortality from CHD is not supported by many clinical research studies.
Early statin trials reported significant mortality benefits, yet serious concerns have been raised in some studies regarding biased results, premature trial terminations, under reporting of adverse events, high numbers of patients lost to follow-up and oversight by the pharmaceutical company sponsor[10]. Heightened awareness within the scientific community regarding problems in clinical trial conduct and analysis - exemplified by the unreported risk of heart attacks in patients taking the pain killers Vioxx and Celebrex - led to new regulatory rules for clinical trials in 2005[11]. Curiously, statin trials conducted after 2005 have failed to demonstrate a consistent mortality benefit[10].
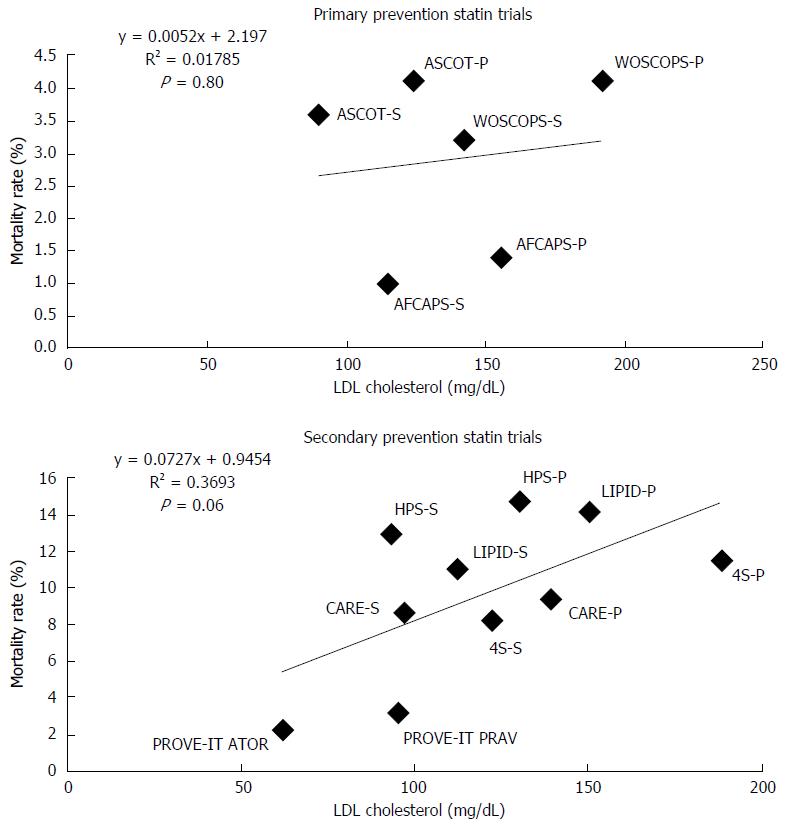
Cholesterol-lowering statin trials are often viewed as supporting the cholesterol hypothesis by reporting significant reductions in combined clinical endpoints. Clinical endpoints are valuable and should not be ignored, but the ultimate measure of efficacy is total mortality that reflects both the treatment effect and potentially fatal side effects. Utilizing combined endpoints may lead to an exaggeration of perceived benefit by assigning equal importance to disparate clinical events such as a hospital admission for angina and death from a heart attack[12,13]. Some have argued that there is a linear relation between low-density lipoprotein (LDL) levels and CHD events[14]. This analysis may be inaccurate because it combines different types of CHD events from diverse studies into one endpoint even though each study defines CHD events differently. A more meaningful analysis compares total mortality rates to LDL cholesterol levels. When we performed such an analysis on these same statin trials - those analyzed in reference 14 - we found no statistically significant relationship (Figure 2).
Although a number of statin trials have reported a mortality benefit, quite a few have not. A corollary to the cholesterol hypothesis posits that patients at highest risk should derive the greatest benefit from cholesterol lowering. However, statin trials in the elderly (PROSPER), in patients with heart failure (CORONA, GISSI-HF), and in patients with renal failure (4D, AURORA, SHARP) have all failed to demonstrate a mortality benefit[10,15]. A Cochrane meta-analysis of 18 cholesterol-lowering trials (some with statins) in patients with peripheral arterial disease also failed to demonstrate a mortality benefit[16]. A separate meta-analysis of 11 statin trials for high-risk primary prevention similarly failed to demonstrate a mortality benefit[17]. Another Cochrane meta-analysis of statin usage after acute coronary syndromes concluded there was no mortality benefit[18]. The Cholesterol Treatment Trialists (CTT) performed a meta-analysis of 27 statin trials and concluded that statins were clearly beneficial in reducing cardiovascular events[19]. However, when the same 27 trials were assessed for mortality outcomes, no benefit was seen[20]. The coronary calcium score is considered to be one of the best predictors of cardiovascular risk, yet the St. Francis Heart Study showed no clinical benefit in asymptomatic patients with coronary calcium scores > 80th percentile randomized to statin therapy[21]. Finally, diabetes mellitus is considered a CHD risk equivalent, but the three randomized controlled trials specifically designed and powered to assess the effect of statins in diabetes all failed to demonstrate a mortality benefit (CARDS, 4D, ASPEN)[22-24].
The dramatic benefits of the Mediterranean diet are likely due to multiple mechanisms which do not directly involve cholesterol. Independent of cholesterol metabolism are the true fatal complications of coronary atherosclerosis - thrombotic coronary occlusion, acute myocardial ischemia, left ventricular dysfunction, and malignant arrhythmias. The hemostatic system appears to be a principal modulator of atherosclerotic plaque formation and progression and the Mediterranean diet can favorably alter elements of the coagulation cascade[25,26]. Plaque rupture and intra-plaque hemorrhage leads to progressive atherosclerosis, thrombosis causes acute coronary syndromes, and sudden cardiac death is the main cause of cardiac mortality. At the genetic level large scale, genome-wide association studies have identified 46 loci directly linked to CHD, yet a majority of these loci have no apparent relation to cholesterol or traditional risk factors[27]. Although we can’t change our genes, epigenetic studies have shown that the Mediterranean diet can favorably alter the expression of atherogenic genes[28], whereas a recent cholesterol-lowering statin trial failed to demonstrate a similar effect[29]. At the cellular level we now know that atherosclerosis is an inflammatory disease where macrophages and T lymphocytes likely play a dominant role. Whether or not specific anti-inflammatory therapies will be successful remains to be determined, but prior experience with Vioxx and Celebrex, which unexpectedly increased cardiovascular deaths, emphasizes the importance of proceeding cautiously. Recent studies have demonstrated that the Mediterranean diet can reduce markers of inflammation[26]. Accumulating evidence also implicates sugar in the pathogenesis of atherosclerosis. Diabetes is considered a coronary artery disease equivalent yet diabetics typically have average cholesterol levels. Other studies indicate that those who drink sugar-sweetened beverages are at much higher risk for CHD[30]. How elevated levels of blood glucose lead to atherosclerosis and why cholesterol lowering statins increase the risk of diabetes remains enigmatic, yet the totality of evidence suggests molecular mechanisms of atherosclerosis that are independent of cholesterol metabolism. The Mediterranean diet has been shown to reduce the risk of developing diabetes and the metabolic syndrome[31,32]. Elegant research into the gut microbiota is also providing an alternative theory of atherosclerosis[33]. Consider that L-carnitine, a component of red meat, is metabolized by the gut microbiota into trimethylamine oxide (TMAO). TMAO, in turn, promotes atherosclerosis and has been associated with a higher risk of cardiovascular events independent of traditional risk factors such as cholesterol. The gut microbiota can also adapt to changes in diet, which may explain why some vegans do not produce any TMAO after an L-carnitine challenge and how the Mediterranean diet may exert its anti-inflammatory and anti-atherosclerotic effects[34].
If statins have failed to consistently reduce mortality one must ask if statins improve the quality of life. Serious or fatal statin adverse events are rare, but side effects are not. The incidence of muscular aches and weakness in statin trials is highly variable, and real world experiences may differ from clinical trial reports. Consider that the adherence rates for statins in the elderly are poor with nearly 75% of primary prevention patients stopping the drug within the first two years[35]. More recently a cohort study of statin users reported a 53% discontinuation rate although a very high percentage were able to continue statin therapy after being rechallenged[36]. In the largest statin survey ever conducted, the National Lipid Association observed that roughly 30% of statin patients reported experiencing muscle pain and weakness and 57% of surveyed patients reported stopping the drug due to side effects[37]. One may debate the relationship of statins to diabetes and dementia, but the fact remains that the FDA now requires disclosure of these warnings. Most distressing is the recent report of gluttonous behavior among statin users who mistakenly believe they are “protected” by taking statins and can eat whatever they want[38].
The debate over the cholesterol hypothesis and statins has raged for decades. Some may point to the recent decline in cardiovascular deaths in the United States as proof of statin effectiveness, but this view fails to incorporate the impact of smoking cessation, lifestyle changes, and dramatic improvements in heart attack survival rates due to timely reperfusion and the availability of external and implantable defibrillators. Others may argue that statins are started too late in life to be effective (the horse may already be out of the barn) and reference Mendelian randomization studies which show that rare individuals with genetically low cholesterol levels have a much lower incidence of CHD[39]. However, this concept should not be extrapolated to the 99.99% of us who lack these genes and also fails to explain how the Mediterranean diet reduces mortality within months of initiation[2-4]. In 1996 Nobel laureates Brown and Goldstein anticipated the eradication of coronary disease in their Science editorial, “Exploitation of recent breakthroughs - proof of the cholesterol hypothesis, discovery of effective drugs, and better definition of genetic susceptibility factors - may well end coronary disease as a major public health problem early in the next century”[40]. History has proven otherwise, and the global prevalence of CHD, despite worldwide statin usage and cholesterol lowering campaigns, has reached pandemic proportions. Coronary heart disease is an extremely complex malady and the expectation that it could be prevented or eliminated by simply reducing cholesterol appears unfounded. After twenty years we should concede the anomalies of the cholesterol hypothesis and refocus our efforts on the proven benefits of a healthy lifestyle incorporating a Mediterranean diet to prevent CHD[2-4,41,42].
P- Reviewer: Ji G, Swierczynski J S- Editor: Ji FF L- Editor: A E- Editor: Wang CH
| 1. | Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994;344:1383-1389. [PubMed] [Cited in This Article: ] |
| 2. | de Lorgeril M, Renaud S, Mamelle N, Salen P, Martin JL, Monjaud I, Guidollet J, Touboul P, Delaye J. Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet. 1994;343:1454-1459. [PubMed] [Cited in This Article: ] |
| 3. | de Lorgeril M, Salen P, Martin JL, Monjaud I, Boucher P, Mamelle N. Mediterranean dietary pattern in a randomized trial: prolonged survival and possible reduced cancer rate. Arch Intern Med. 1998;158:1181-1187. [PubMed] [Cited in This Article: ] |
| 4. | de Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99:779-785. [PubMed] [Cited in This Article: ] |
| 5. | Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279-1290. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3157] [Cited by in F6Publishing: 2747] [Article Influence: 249.7] [Reference Citation Analysis (0)] |
| 6. | Sofi F, Abbate R, Gensini GF, Casini A. Accruing evidence on benefits of adherence to the Mediterranean diet on health: an updated systematic review and meta-analysis. Am J Clin Nutr. 2010;92:1189-1196. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1105] [Cited by in F6Publishing: 1038] [Article Influence: 74.1] [Reference Citation Analysis (0)] |
| 7. | Sinnett PF, Whyte HM. Epidemiological studies in a total highland population, Tukisenta, New Guinea. Cardiovascular disease and relevant clinical, electrocardiographic, radiological and biochemical findings. J Chronic Dis. 1973;26:265-290. [PubMed] [Cited in This Article: ] |
| 8. | Chowdhury R, Warnakula S, Kunutsor S, Crowe F, Ward HA, Johnson L, Franco OH, Butterworth AS, Forouhi NG, Thompson SG. Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis. Ann Intern Med. 2014;160:398-406. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 871] [Cited by in F6Publishing: 760] [Article Influence: 76.0] [Reference Citation Analysis (0)] |
| 9. | Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2889-2934. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2683] [Cited by in F6Publishing: 2918] [Article Influence: 265.3] [Reference Citation Analysis (0)] |
| 10. | de Lorgeril M. In: Souccar T, editor. Cholesterol and statins. Vergèze, France: Sham science and bad medicine 2014; . [Cited in This Article: ] |
| 11. | Miossec M, Miossec P. New regulatory rules for clinical trials in the United States and the European Union: key points and comparisons. Arthritis Rheum. 2006;54:3735-3740. [PubMed] [Cited in This Article: ] |
| 12. | Ferreira-González I, Busse JW, Heels-Ansdell D, Montori VM, Akl EA, Bryant DM, Alonso-Coello P, Alonso J, Worster A, Upadhye S. Problems with use of composite end points in cardiovascular trials: systematic review of randomised controlled trials. BMJ. 2007;334:786. [PubMed] [Cited in This Article: ] |
| 13. | Kip KE, Hollabaugh K, Marroquin OC, Williams DO. The problem with composite end points in cardiovascular studies: the story of major adverse cardiac events and percutaneous coronary intervention. J Am Coll Cardiol. 2008;51:701-707. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 212] [Cited by in F6Publishing: 220] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 14. | O’Keefe JH, Cordain L, Harris WH, Moe RM, Vogel R. Optimal low-density lipoprotein is 50 to 70 mg/dl: lower is better and physiologically normal. J Am Coll Cardiol. 2004;43:2142-2146. [PubMed] [Cited in This Article: ] |
| 15. | Reiner Z, Catapano AL, De Backer G, Graham I, Taskinen MR, Wiklund O, Agewall S, Alegria E, Chapman MJ, Durrington P. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J. 2011;32:1769-1818. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1871] [Cited by in F6Publishing: 1926] [Article Influence: 148.2] [Reference Citation Analysis (0)] |
| 16. | Aung PP, Maxwell HG, Jepson RG, Price JF, Leng GC. Lipid-lowering for peripheral arterial disease of the lower limb. Cochrane Database Syst Rev. 2007;CD000123. [PubMed] [Cited in This Article: ] |
| 17. | Ray KK, Seshasai SR, Erqou S, Sever P, Jukema JW, Ford I, Sattar N. Statins and all-cause mortality in high-risk primary prevention: a meta-analysis of 11 randomized controlled trials involving 65,229 participants. Arch Intern Med. 2010;170:1024-1031. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 279] [Cited by in F6Publishing: 279] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 18. | Vale N, Nordmann AJ, Schwartz GG, de Lemos J, Colivicchi F, den Hartog F, Ostadal P, Macin SM, Liem AH, Mills EJ. Statins for acute coronary syndrome. Cochrane Database Syst Rev. 2014;9:CD006870. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 19. | Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, Voysey M, Gray A, Collins R, Baigent C. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet. 2012;380:581-590. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1891] [Cited by in F6Publishing: 1792] [Article Influence: 149.3] [Reference Citation Analysis (0)] |
| 20. | Abramson JD, Rosenberg HG, Jewell N, Wright JM. Should people at low risk of cardiovascular disease take a statin? BMJ. 2013;347:f6123. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 123] [Cited by in F6Publishing: 132] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 21. | Arad Y, Spadaro LA, Roth M, Newstein D, Guerci AD. Treatment of asymptomatic adults with elevated coronary calcium scores with atorvastatin, vitamin C, and vitamin E: the St. Francis Heart Study randomized clinical trial. J Am Coll Cardiol. 2005;46:166-172. [PubMed] [Cited in This Article: ] |
| 22. | Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA, Neil HA, Livingstone SJ, Thomason MJ, Mackness MI, Charlton-Menys V, Fuller JH. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet. 2004;364:685-696. [PubMed] [Cited in This Article: ] |
| 23. | Wanner C, Krane V, März W, Olschewski M, Mann JF, Ruf G, Ritz E. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med. 2005;353:238-248. [PubMed] [Cited in This Article: ] |
| 24. | Knopp RH, d’Emden M, Smilde JG, Pocock SJ. Efficacy and safety of atorvastatin in the prevention of cardiovascular end points in subjects with type 2 diabetes: the Atorvastatin Study for Prevention of Coronary Heart Disease Endpoints in non-insulin-dependent diabetes mellitus (ASPEN). Diabetes Care. 2006;29:1478-1485. [PubMed] [Cited in This Article: ] |
| 25. | Borissoff JI, Spronk HM, ten Cate H. The hemostatic system as a modulator of atherosclerosis. N Engl J Med. 2011;364:1746-1760. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 382] [Cited by in F6Publishing: 363] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 26. | Chrysohoou C, Panagiotakos DB, Pitsavos C, Das UN, Stefanadis C. Adherence to the Mediterranean diet attenuates inflammation and coagulation process in healthy adults: The ATTICA Study. J Am Coll Cardiol. 2004;44:152-158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 513] [Cited by in F6Publishing: 517] [Article Influence: 25.9] [Reference Citation Analysis (0)] |
| 27. | Miller CL, Assimes TL, Montgomery SB, Quertermous T. Dissecting the causal genetic mechanisms of coronary heart disease. Curr Atheroscler Rep. 2014;16:406. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Camargo A, Delgado-Lista J, Garcia-Rios A, Cruz-Teno C, Yubero-Serrano EM, Perez-Martinez P, Gutierrez-Mariscal FM, Lora-Aguilar P, Rodriguez-Cantalejo F, Fuentes-Jimenez F. Expression of proinflammatory, proatherogenic genes is reduced by the Mediterranean diet in elderly people. Br J Nutr. 2012;108:500-508. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 92] [Cited by in F6Publishing: 87] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 29. | Holven KB, Narverud I, Lindvig HW, Halvorsen B, Langslet G, Nenseter MS, Ulven SM, Ose L, Aukrust P, Retterstøl K. Subjects with familial hypercholesterolemia are characterized by an inflammatory phenotype despite long-term intensive cholesterol lowering treatment. Atherosclerosis. 2014;233:561-567. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 30. | Huang C, Huang J, Tian Y, Yang X, Gu D. Sugar sweetened beverages consumption and risk of coronary heart disease: a meta-analysis of prospective studies. Atherosclerosis. 2014;234:11-16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 126] [Cited by in F6Publishing: 130] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 31. | Grosso G, Stepaniak U, Micek A, Topor-Mądry R, Stefler D, Szafraniec K, Bobak M, Pająk A. A Mediterranean-type diet is associated with better metabolic profile in urban Polish adults: Results from the HAPIEE study. Metabolism. 2015;64:738-746. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 32. | Ros E, Martínez-González MA, Estruch R, Salas-Salvadó J, Fitó M, Martínez JA, Corella D. Mediterranean diet and cardiovascular health: Teachings of the PREDIMED study. Adv Nutr. 2014;5:330S-336S. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 237] [Cited by in F6Publishing: 230] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 33. | Bäckhed F. Meat-metabolizing bacteria in atherosclerosis. Nat Med. 2013;19:533-534. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 34. | Marlow G, Ellett S, Ferguson IR, Zhu S, Karunasinghe N, Jesuthasan AC, Han DY, Fraser AG, Ferguson LR. Transcriptomics to study the effect of a Mediterranean-inspired diet on inflammation in Crohn’s disease patients. Hum Genomics. 2013;7:24. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 122] [Cited by in F6Publishing: 118] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 35. | Jackevicius CA, Mamdani M, Tu JV. Adherence with statin therapy in elderly patients with and without acute coronary syndromes. JAMA. 2002;288:462-467. [PubMed] [Cited in This Article: ] |
| 36. | Zhang H, Plutzky J, Skentzos S, Morrison F, Mar P, Shubina M, Turchin A. Discontinuation of statins in routine care settings: a cohort study. Ann Intern Med. 2013;158:526-534. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 382] [Cited by in F6Publishing: 396] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 37. | About the USAGE Survey. Available from: http://www.statinusage.com/Pages/about-the-survey.aspx. [Cited in This Article: ] |
| 38. | Sugiyama T, Tsugawa Y, Tseng CH, Kobayashi Y, Shapiro MF. Different time trends of caloric and fat intake between statin users and nonusers among US adults: gluttony in the time of statins? JAMA Intern Med. 2014;174:1038-1045. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 96] [Cited by in F6Publishing: 96] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 39. | Ference BA, Yoo W, Alesh I, Mahajan N, Mirowska KK, Mewada A, Kahn J, Afonso L, Williams KA, Flack JM. Effect of long-term exposure to lower low-density lipoprotein cholesterol beginning early in life on the risk of coronary heart disease: a Mendelian randomization analysis. J Am Coll Cardiol. 2012;60:2631-2639. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 524] [Cited by in F6Publishing: 561] [Article Influence: 46.8] [Reference Citation Analysis (0)] |
| 40. | Brown MS, Goldstein JL. Heart attacks: gone with the century? Science. 1996;272:629. [PubMed] [Cited in This Article: ] |
| 41. | Chiuve SE, Fung TT, Rexrode KM, Spiegelman D, Manson JE, Stampfer MJ, Albert CM. Adherence to a low-risk, healthy lifestyle and risk of sudden cardiac death among women. JAMA. 2011;306:62-69. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 97] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 42. | Akesson A, Larsson SC, Discacciati A, Wolk A. Low-risk diet and lifestyle habits in the primary prevention of myocardial infarction in men: a population-based prospective cohort study. J Am Coll Cardiol. 2014;64:1299-1306. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 150] [Cited by in F6Publishing: 142] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 43. | Kannel WB, Castelli WP, Gordon T. Cholesterol in the prediction of atherosclerotic disease. New perspectives based on the Framingham study. Ann Intern Med. 1979;90:85-91. [PubMed] [Cited in This Article: ] |