Single-incision video-assisted thoracic surgery lobectomy in the treatment of adult communicating bronchopulmonary foregut malformation with large aberrant artery
Introduction
Since single-incision thoracoscopic surgery (SITS) was introduced for lobectomies, SITS has been applied in various types of complex thoracic surgery (1,2). However, SITS is not yet widely used for the treatment of pulmonary sequestration; most thoracic surgeons prefer the conventional three-port video-assisted thoracic surgery (VATS) due to the difficulty of manipulating the aberrant systemic artery or working around inflamed tissue through a single incision (3,4). We improved the SITS lobectomy technique so that surgeons can manipulate the aberrant systemic artery and safely work around inflamed tissue.
Surgical technique
Case
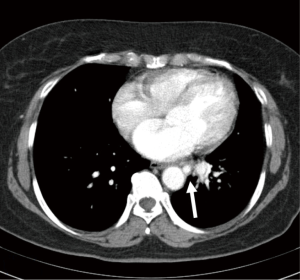
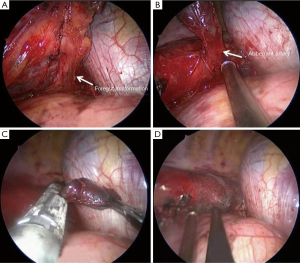
A 59-year-old female was admitted complaining of hemoptysis for 1 month and frequent lower respiratory infections. Chest computed tomography showed intralobar sequestration with the systemic blood supply arising directly from the descending thoracic aorta via a 1-cm aberrant artery in the left lower lobe (Figure 1). We opted to perform a left lower lobectomy and excision of the aberrant systemic artery using SITS. In the operation, a single <4 cm incision was made, and an extra-small wound retractor was inserted through the fifth intercostal space at the anterior axillary line. All of the procedures were performed through the one incision without additional ports. First, the interlobar fissure was dissected to expose the pulmonary artery. Then, the inferior pulmonary ligament was dissected, except around the aberrant artery. During dissection of the inferior pulmonary ligament, a foregut communication arising from the lower esophagus was found incidentally (Figure 2A). The foregut communication was subsequently divided using an Endo GIA stapler. Then, the pulmonary artery, lower lobe bronchus, and inferior pulmonary vein were excised in order. First, the lung around the aberrant artery was stapled, instead of directly stapling the aberrant artery (Figure 2B). After extracting the lung and securing the surgical field, additional stapling and clipping were done to remove the remaining lung tissue and to shorten the stalk of the aberrant artery (Figure 2C). After sealing the excision site with a polyglycolic acid sheet and fibrin glue, a 24-Fr chest tube was inserted, and the incision was closed (Figure 2D, Figures 3,4). The patient was discharged 11 days later with no postoperative complications.

Discussion
The first consideration with the SITS lobectomy was the order of anatomical structure resection. Because the first anatomical structure seen in the thoracoscopic view in conventional VATS is the aberrant artery, it should be excised first, followed by the inferior pulmonary vein, pulmonary artery, and lower lobe bronchus in sequence. However, the SITS lobectomy is generally performed through a single incision in the fifth anterior intercostal space, and most of the anatomical structures are located below the incision. Specifically, the aberrant artery is the lowest anatomical structure in the thoracoscopic view. Therefore, excising the aberrant artery last is the optimal order in SITS. Consequently, we resected the anatomical structures in the order viewed through the thoracoscope to facilitate the SITS lobectomy, and performed the resection in the order of pulmonary artery, lower lobe bronchus, inferior pulmonary vein, and aberrant artery.
The second consideration is the method of resecting the aberrant artery. Various procedures have been used to resect aberrant arteries safely. Currently, direct excision with a vascular endo-stapler is preferred (7,8). Although most authors feel that endovascular stapling is sufficient for excising the aberrant artery, we should not overlook the possibility of artery rupture during the stapling process. With conventional VATS, various directional instrument accesses are possible for controlling the bleeding if the artery ruptures during stapling, and rapid bleeding control is possible. In some cases, it is even possible to repair the rupture directly via VATS without conversion to a thoracotomy. In SITS, however, any rapid blood suctioning, rapid compression of the bleeding focus, and clamping of the bleeding site must be performed through the single incision. Consequently, rapid bleeding control is impossible due to the limited movement and collision of instruments. Therefore, it is necessary to improve the surgical technique to overcome this SITS limitation. We introduced a two-stage stapling technique for easy, safe resection of the aberrant artery. First, the lung around the aberrant artery is stapled to remove the lung from the thoracic cavity without touching the aberrant artery. This ensures a good view of the aberrant artery for its excision in SITS. After extracting the lung, the aberrant artery is also directly stapled.
In conclusion, single-port VATS is an acceptable method for major pulmonary resection for the treatment of intrapulmonary sequestration. It does not pose difficulties in the manipulation and division of an aberrant systemic artery, if present. We believe that our two modifications will increase the suitability of SITS pulmonary lobectomy for the treatment of pulmonary sequestration.
Acknowledgements
This study was supported by the Research Institute for the Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wan IY, Lee TW, Sihoe AD, et al. Video-assisted thoracic surgery lobectomy for pulmonary sequestration. Ann Thorac Surg 2002;73:639-40. [PubMed]
- Klena JW, Danek SJ, Bostwick TK, et al. Video-assisted thoracoscopic resection for intralobar pulmonary sequestration: single modality treatment with video-assisted thoracic surgery. J Thorac Cardiovasc Surg 2003;126:857-9. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fieira E, et al. Single-incision video-assisted thoracoscopic lobectomy: initial results. J Thorac Cardiovasc Surg 2012;143:745-7. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Kim CW, Kim DH. The order of anatomical structure resection as seen through the thoracoscope. Asvide 2016;3:055. Available online: http://www.asvide.com/articles/806
- Kim CW, Kim DH. The two-stage stapling technique for easy, safe resection of the aberrant artery. Asvide 2016;3:056. Available online: http://www.asvide.com/articles/807
- Kestenholz PB, Schneiter D, Hillinger S, et al. Thoracoscopic treatment of pulmonary sequestration. Eur J Cardiothorac Surg 2006;29:815-8. [PubMed]
- Goto T, Toya K, Wakaki M, et al. Resection of intralobar pulmonary sequestration after coil embolization of aberrant arteries: report of a case. Surg Today 2013;43:923-5. [PubMed]


