A large malignant thymomas of the anterior mediastinum
Introduction
Complex mediastinal tumors are rare in clinical settings, and associated with a variety of intrasurgical and postoperative complications. A patient with a large anterior mediastinal tumor underwent surgery in our hospital, and the outcome was satisfactory.
Case report
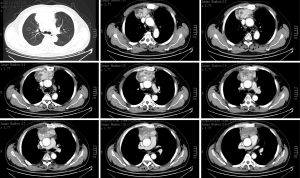
The 59-year-old man, married, born in Jiangyin, was admitted for “a space-occupying mass of the mediastinum spotted more than a year ago.” The patient had cough with blood stained sputum in February 2012. Anteroposterior chest X-ray revealed right upper lobe infection with possible atelectasis. A chest CT scan showed a space-occupying mass of the anterior mediastinum and upper right lung infection. Later, an enhanced CT and magnetic resonance imaging (MRI) showed a space-occupying mass of the anterior superior mediastinum, which was highly likely an invasive thymoma (Figures 1,2). CEA was 5.79 mg/mL. On February 20, 2013, a mediastinal biopsy could not rule out epithelioid cell tumor and thymoma, and thus immunohistochemistry tests would be needed for confirmation of the diagnosis and treatment. On February 22, 2013, immunohistochemistry showed a thymoma with epithelioid cells, which were mildly to moderately deformed; lymphocytes were reduced in it. The condition needed to be differentiated from type A thymoma and atypical type B2 thymoma. An ultrasound-guided biopsy of the mediastinal mass showed a mediastinal thymoma. Relevant examinations showed no obvious contraindications. Hence, the patient underwent chemotherapy from February 26 to March 19, 2013. The regimen was docetaxel 129 mg D1 and cisplatin 140 mg D1. After chemotherapy, a repeat chest CT showed no significant changes compared with the previous condition. The patient was admitted for further treatment this time.

A sternal incision of about 25 cm was made to open the layers. The mediastinal tumor had invaded tissue under the sternum, so the sternum was sawed in the middle for extensive thymic tumor resection. The tumor was removed from the sternum using blunt dissection and electric cutting. The tumor had invaded bilateral pleural tissue, bilateral lung tissue, bilateral phrenic nerves, and the right internal mammary artery. Bilateral lung tissue was removed from the tumor using a XF closer and a linear straight cutter. In view of the pericardial invasion, an incision was made around the normal pericardial tissue to cut invaded areas along the normal tissue. Bilateral phrenic nerves were separated from inside the tumor. Bilateral upper corners of the thymus were separated. The right internal mammary artery wrapped in the tumor was separated at the proximal end and ligated. The tumor was removed from the left and right innominate veins. The inferior wall of the left innominate vein was invaded, so the tumor was removed from the vessel using a noninvasive vascular clamp. The left innominate vein was closed with 5-0 prolence continuous suture. The lower tumor was removed from the superior vena cava and the aorta membrane, and the invaded pleura was cut. The tumor invaded through the pericardium, the opening of the pulmonary artery and the right ventricular outflow. The pericardial involvement was resected. The invaded pulmonary artery was clamped and the tumor and pericardium were completely removed, in a size of about 11 cm × 8 cm × 6 cm. The pulmonary artery was closed with padded 4-0 prolence suture.
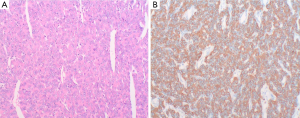
Pathological diagnosis was (mediastinum) thymoma (type B3), tumor tissue infiltration in adipose tissue and pleural tissue (Figure 3). A tumor in the size of 13 cm × 8 cm × 3 cm was seen, with nodular profile and solid margins in light red with medium texture. Many small cysts containing clear pink liquid could be seen regionally, with regional bleeding. Muscle tissue was attached outside of the tumor.
Two weeks after surgery, a repeat chest radiograph showed good recovery, and the patient was free of chills, fever, and chest tightness. His eating and sleeping was fine, and bowel movement was normal. Physical examination: conscious, general condition was good; neck was soft, coarse breath sounds were heard in both lungs, no dry and wet rales. Chest incision healed well. Heart rate was 86 beats/min, and rhythm was regular. No pathological murmurs were heard. The abdomen was soft without tenderness. Bowel sounds could be heard. Limb muscle strength and muscle tone were normal. The patient was then discharged. Postoperative follow-up revealed satisfying breathing activity and good outcome. After his condition was stable, he underwent radiotherapy.
Discussion
A mediastinal tumor (1) occurs between both sides of the pleural cavity, and can compress the surrounding tissue with the increase of the volume. The symptoms are generally not typical. However, once diagnosed, a mediastinal tumor requires immediate surgical treatment. Complex medinastinal tumors are generally large, compressing the lungs and surrounding tissue and organs. Poor preoperative cardiopulmonary function will give rise to a greater surgical risk. Appropriate imaging studies provide good clinical guidance for the treatment of this disease. Chest X-ray and CT are the most fundamental examinations for large mediastinal tumors. Chest X-ray often shows large areas of dense shadows in the chest, which can be often misdiagnosed as pleural effusion. Fluroscopic examination of the chest should be combined. CT scans can accurately reveal the tumor size, location, and relationship with the surrounding organs. Enhanced scans may further clarify the relationship between the tumor and great vessels to guide surgery. This patient received an enhanced CT scan to clarify the nature of the tumor and its relationship with the heart and great vessels, and the MRI was also performed as the tumor had invaded major vessels and was close to the heart. MRI would be more accurate in revealing vascular and cardiac invasion compared with CT (2). Meanwhile, the patient’s T2WI and fat signals were the same, which provided assistance for the choice of surgical techniques. The ultrasound-guided subcutaneous tumor biopsy also helped confirm the pathological diagnosis and surgical approach. However, there has been controversy over the use of ultrasound-guided biopsy, mainly due to the fear of tumor spread. It is not a routine clinical examination method for unresectable thymic tumors highly suspected lymphomas. This patient had confirmed pathology via the biopsy, but was not well responsive to chemotherapy. Upon completion of the relevant examinations, there were no contraindications, so he underwent surgical resection.
The patient’s confirmed preoperative diagnosis was thymic tumor. Complete resection of thymic tumors is the key to successful surgical treatment (3). Even at a pathological stage of III-IV, complete resection can also result in satisfying outcomes. Due to the movement and traction, a large mediastinal tumor is likely to form adhesions to the surrounding tissue, leading to varying anatomic relationships. Therefore, the relationship between the tumor and adjacent organs should be clarified in surgery (4). Exploratory surgery should be comprehensive and detailed, to make clear the relationship with the surrounding organs, especially large vessels and bronchi, before surgical resection. In this patient, the anterior and middle mediastinal tumor tended to grow on both sides. Due to the mediastinal infiltration and oppression, and resultant anatomic variations made it easy for misjudgment of the organizational structure, leading to wrong resection or surgery difficulty. For good surgical exposure, an incision was made through the middle of the sternum, which was conducive to the tumor removal and extended neck incision for vena cava branch exploration to establish an artificial channel back to the heart. Meanwhile, it also facilitated the management in case of an emergency situation in surgery. During surgery, we performed from superficial to the depth layers, making part of the tumor loose, dividing it on the surface layer by layer, and finally separating the root. No obvious damage occurred during the surgery. A large solid tumor tends to block the surgical field, and has very rich blood supply. When one-time resection is difficult, the tumor can be partially cut and sutured one block after another, or the tumor body can be removed first before separating the pedicle, so as to completely resect the whole tumor without any residue to avoid recurrence. If tumor infiltrating growth is found during surgery and large vessels are freeze-like, leaving no anatomical space for surgery, the procedure should not be performed forcefully. In this case, the tumor was completely resected with the aid of cardiopulmonary bypass, achieving a good cure effect. During surgery, caution should be paid to protect bilateral phrenic nerves, especially the left phrenic nerve when both phrenic nerves are involved. Postoperative radiotherapy can achieve satisfying long-term therapeutic effect.
The tumor should be resected as completely as possible, unless it is closely related to vessels and nerves, making complete resection impossible. After surgery, chemotherapy is still required to avoid recurrence. The patient’s family should be informed of the condition in detail to enhance their risk awareness and avoid a possible medical dispute, and have them prepared for the potential costs.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Rendina EA, Venuta F, De Giacomo T, et al. Biopsy of anterior mediastinal masses under local anesthesia. Ann Thorac Surg 2002;74:1720-2; discussion 1722-3.
- Seki S, Koyama H, Ohno Y, et al. Diffusion-weighted MR imaging vs. multi-detector row CT: Direct comparison of capability for assessment of management needs for anterior mediastinal solitary tumors. Eur J Radiol 2014;83:835-42. [PubMed]
- Kumar V, Kaminski HJ. Treatment of myasthenia gravis. Curr Neurol Neurosci Rep 2011;11:89-96. [PubMed]
- Singla S, Litzky LA, Kaiser LR, et al. Should asymptomatic enlarged thymus glands be resected? J Thorac Cardiovasc Surg 2010;140:977-83. [PubMed]


