Published online Jun 14, 2022. doi: 10.3748/wjg.v28.i22.2509
Peer-review started: December 22, 2021
First decision: January 8, 2022
Revised: January 14, 2022
Accepted: April 28, 2022
Article in press: April 28, 2022
Published online: June 14, 2022
Probiotics are a promising solution for managing irritable bowel syndrome (IBS). Saccharomyces cerevisiae (S. cerevisiae) I-3856 has already demonstrated beneficial effects in IBS subjects, particularly in IBS with predominant constipation (IBS-C).
To confirm the efficacy of S. cerevisiae I-3856 in the management of gastrointestinal symptoms in IBS-C.
A randomized, double-blind, placebo-controlled clinical study was performed in a total of 456 subjects. After a run-in period, subjects were randomly assigned to the group receiving S. cerevisiae I-3856 (8 × 109 CFU daily) or the placebo for 8 wk, and they performed daily self-evaluations of gastrointestinal symptoms. The primary objective was to assess the effect of the probiotic on abdominal pain. The secondary objectives were the evaluation of other gastrointestinal symptoms, bowel movement frequency and consistency, and quality of life (QOL).
A significantly higher proportion of abdominal pain responders was reported in the Probiotic group (45.1% vs 33.9%, P = 0.017). A nonsignificant difference in the area under the curve for abdominal pain over the second month of supplementation was observed in subjects receiving probiotic vs placebo [P = 0.073, 95%CI: -0.59 (-1.23; 0.05)]. No statistically significant differences were reported in the evolution of bowel movement frequency and stool consistency between the groups. After 8 wk of supplementation, the overall QOL score was significantly higher in the Probiotic group than in the Placebo group [P = 0.047, 95%CI: 3.86 (0.52; 7.20)]. Furthermore, exploratory analyses showed statistically significant and clinically relevant improvements in QOL scores in abdominal pain responders vs nonresponders.
The results of this clinical study confirmed the abdominal pain alleviation properties of S. cerevisiae I-3856 in IBS-C. Abdominal pain relief was associated with improved QOL. ClinicalTrials.gov identifier: NCT03150212.
Core Tip: The gut microbiota has been proposed as central in irritable bowel syndrome (IBS) pathophysiology, and microbiota-directed intervention has therefore drawn considerable interest. Probiotics have been recognized as a potential solution for acting on the multifactorial causes and clinical symptoms of IBS. Among them, Saccharomyces cerevisiae (S. cerevisiae) CNCM I-3856 is a probiotic yeast that has shown beneficial effects on gastrointestinal symptoms of individuals with IBS, especially in IBS subjects with predominant constipation. This clinical study confirmed the abdominal pain alleviation properties of S. cerevisiae I-3856 in IBS with predominant constipation and showed improvements in quality of life in the group receiving the probiotic.
- Citation: Mourey F, Decherf A, Jeanne JF, Clément-Ziza M, Grisoni ML, Machuron F, Legrain-Raspaud S, Bourreille A, Desreumaux P. Saccharomyces cerevisiae I-3856 in irritable bowel syndrome with predominant constipation. World J Gastroenterol 2022; 28(22): 2509-2522
- URL: https://www.wjgnet.com/1007-9327/full/v28/i22/2509.htm
- DOI: https://dx.doi.org/10.3748/wjg.v28.i22.2509
Irritable bowel syndrome (IBS) is a disorder of gut-brain interaction[1] that affects approximately one in ten people globally[2]. This chronic condition is characterized by recurrent abdominal pain related with altered bowel habits. In addition to the patient’s suffering, it represents a significant burden from both economic and social perspectives. It has indeed been associated with important psychosocial consequences as well as considerable costs to health care systems and society[3,4]. Limitations and impairment of social and emotional daily functioning of IBS patients is demonstrated by the consistently reported profound reductions in quality of life (QOL) compared with the general population[5,6]. QOL impairments in IBS are of similar magnitude to those in more severe diseases, such as inflammatory bowel diseases or depression[5,7,8]. The high prevalence of IBS, as well as its significant morbidity, result in substantial health care utilization and loss of work productivity that represent considerable direct and indirect costs to society[4,9,10].
IBS is a complex and heterogenous condition. Although abdominal pain is the cardinal feature, IBS patients can be classified into different subtypes depending on their predominant stool pattern: IBS with predominant constipation (IBS-C), IBS with predominant diarrhoea (IBS-D), IBS with mixed bowel habits (IBS-M) and IBS unclassified. The pathogenesis of IBS has been described as multifactorial and involves a combination of factors related to motility, visceral hypersensitivity, mucosal immune dysregulation, alterations of gut microbiota, and central and enteric nervous system dysregulation[1]. However, interventions remain symptom-driven, and available pharmacological treatment options are of limited efficacy[11]. Complementary and alternative solutions to achieving satisfactory control of gastrointestinal symptoms and improve QOL in IBS patients are therefore of great interest. The gut microbiota has been proposed as central in IBS pathophysiology and has therefore drawn considerable interest[12,13]. Among microbiota-directed interventions, probiotics have been recognized as a potential solution for acting on the multifactorial causes and clinical symptoms of IBS[14,15]. A meta-analysis of fifty-three randomized controlled trials (RCTs) involving a total of 5545 patients was recently performed. It demonstrated overall beneficial effects of probiotics on global IBS symptoms and abdominal pain with favourable safety profiles, although conclusions were drawn for probiotics in general[16]. Due to the important heterogeneity of both the tested strains and study designs, identifying which probiotics are relevant for IBS management remains a challenge[17]. However, a recently conducted meta-analysis provided further evidence to determine which probiotic strains are effective in IBS symptom management. Among the probiotics analysed, Saccharomyces cerevisiae (S. cerevisiae) CNCM I-3856 emerged as a recognized solution[18].
S. cerevisiae CNCM I-3856 provides statistically significant and clinically relevant benefits for individuals with IBS, as demonstrated in three RCTs[19-21] performed in a total of 679 subjects and an individual patient data (IPD) meta-analysis[22]. This meta-analysis confirmed previous observations linking S. cerevisiae CNCM I-3856 supplementation to improvement in gastrointestinal symptoms in all IBS subpopulations. Nevertheless, the strongest effects were reported in IBS with predominant constipation. Considering these results, we designed a clinical study to confirm the efficacy of S. cerevisiae CNCM I-3856 on gastrointestinal symptom management in an IBS population with predominant constipation.
A large-scale, multicentric, placebo-controlled, randomized, double-blind, clinical study was conducted between March 2017 and May 2019. The study was approved by the Ethics Committee Ouest VI of Brest (France) and performed according to International Conference on Harmonization Good Clinical Practice and the ethical principles of the Declaration of Helsinki. Signed written informed consent for the study was obtained from all subjects before protocol-specific procedures were carried out.
The clinical trial was registered in a clinical trials registration system at ClinicalTrials.gov with the identifier NCT03150212.
Subjects with IBS were recruited by ten French general practitioners across France and in four clinical investigation centres, including Biofortis Mérieux Nutrisciences as the principal investigational centre. Females and males aged 18-75 years were eligible to participate if they met the Rome IV criteria[23] for IBS-C with a baseline score for abdominal pain ≥ 2 and < 6 assessed on a 7-point Likert scale scored from 0 (null) to 7 (severe pain) and had an IBS history between 1 and 10 years. All volunteers agreed to maintain their lifestyle behaviours during their participation in the study. Participants were excluded if they had chronic gastrointestinal conditions other than IBS, including inflammatory bowel diseases, lactose intolerance, and celiac disease. Individuals with a metabolic disorder affecting intestinal transit function or nutrient absorption, such as diabetes or unbalanced thyroid dysfunction, were excluded. Volunteers undergoing symptomatic drug treatments acting on intestinal sensitivity or motility, such as opioids and narcotic analgesics, were not eligible. Antibiotic or antifungal therapies in progress or prescribed 4 or 2 wk before randomization, respectively, were also considered an exclusion criterion. The use of probiotics, prebiotics, symbiotics or any dietary supplement that, according to the investigator, could affect study outcomes in the four weeks preceding randomization was prohibited. However, laxatives, antibloating agents, antispasmodics, anxiolytics, antidepressants, analgesics and nonsteroidal anti-inflammatory drugs were authorized if consumed for longer than three months and maintained at a stable dosage for the entire study duration.
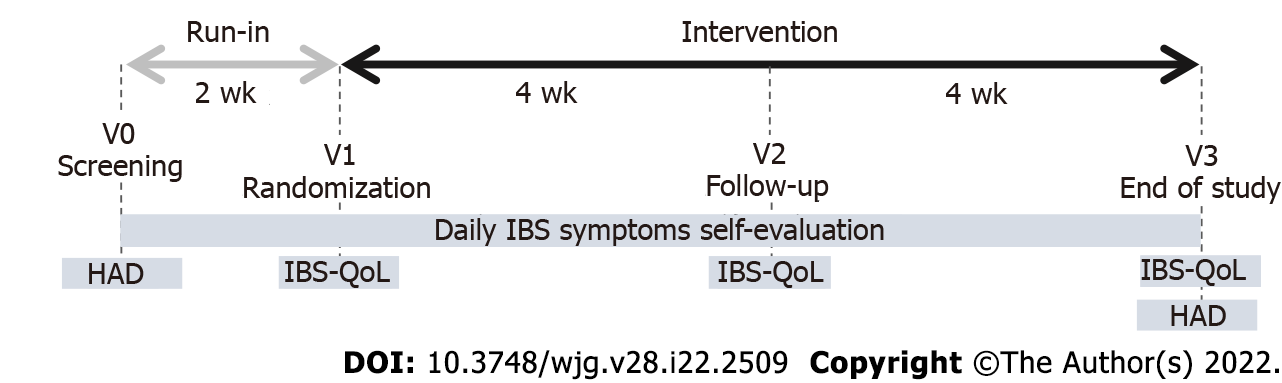
This study consisted of a 2-wk run-in period followed by an 8-wk treatment period. Subjects visited the clinical investigation centre or general practitioner four times: V0 (screening visit), V1 (randomization visit, 2 wk after V0), V2 (follow-up visit, 4 wk after V1) and V3 (end-of-study visit, 8 wk after V1) (Figure 1). Screening visits (V0) were planned to assess whether inclusion and exclusion criteria were met and to explain study instructions. Additionally, recommendations were given to volunteers to avoid changes in lifestyle behaviours (including dietary and physical activity habits), and volunteers were asked to perform a daily evaluation of the intensity of IBS symptoms and bowel movements. At the randomization visit (V1), investigators confirmed the eligibility (including the Rome IV diagnostic criteria for IBS-C) of the volunteers by integrating the daily evaluation of abdominal pain and bowel movement consistency. Eligible subjects were randomized to receive daily S. cerevisiae CNCM I-3856 (Probiotic group) or placebo (Placebo group) for 8 wk. The product allocation list was prepared using SAS® software (version 9.3, SAS Institute Inc., Cary, NJ, United States) before the study started and stored confidentially by a person not related to the clinical phase or data management. The product allocation list was generated using a dynamic randomization algorithm designed to minimize imbalance between the two supplemented groups within each investigational site. Blinding of allocation was maintained until the completed study database was locked.
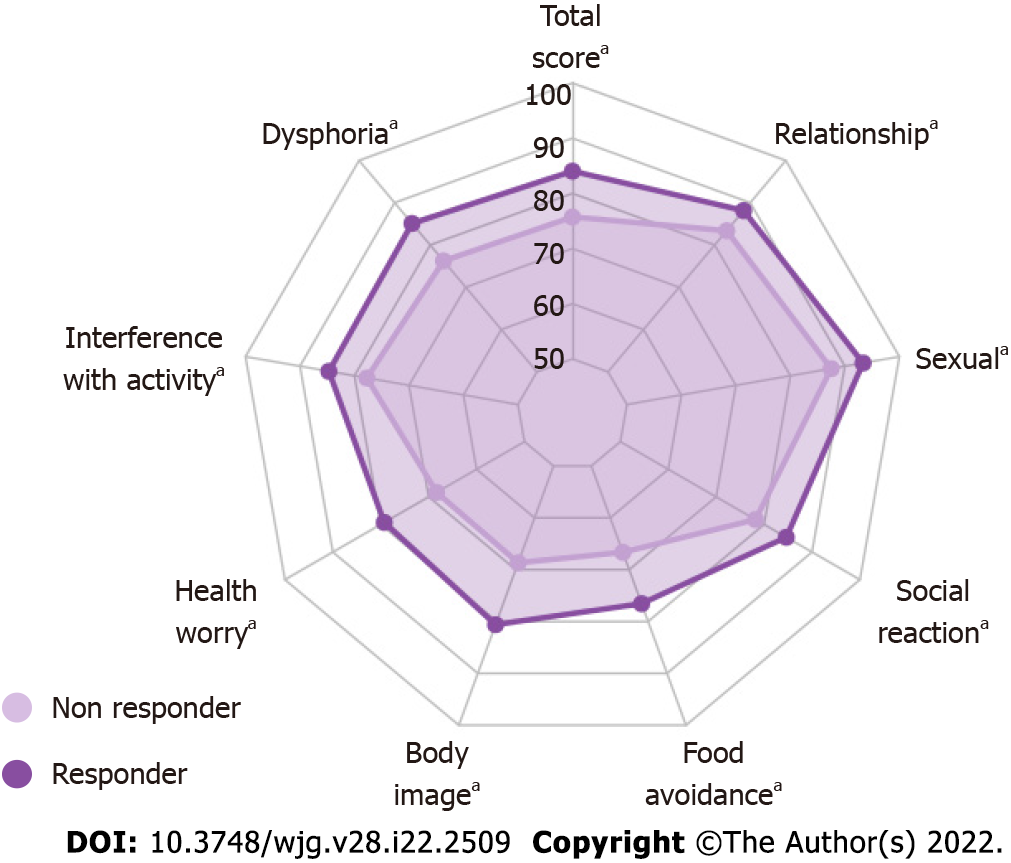
During the baseline and intervention periods, volunteers were asked to perform a daily evaluation of the intensity of IBS symptoms (abdominal pain, bloating, and flatulence/borborygmi) on a 7-point Likert scale rated from 0 (null) to 7 (severe). Bowel movement consistency assessed on the Bristol stool scale (BSS) was recorded daily. Volunteers completed an IBS-specific quality of life questionnaire (IBS-QOL) at randomization (V1), follow-up (V2) and the end of the intervention (V3). The IBS-QOL is a 34-item instrument that yields an overall QOL score as well as scores for eight domains (dysphoria, interference with activity, body image, health worry, food avoidance, social reaction, sexual, relationships). Final scores were normalized to a 100-point scale, with 0 indicating the worst QOL and 100 indicating the best QOL. Anxiety and depression symptoms were also assessed using the hospital anxiety and depression questionnaire at screening (V0) and end-of-study visits (V3).
The study evaluated the probiotic yeast S. cerevisiae CNCM I-3856. This strain is a proprietary, well-characterized strain of Lesaffre registered in the French National Collection of Cultures of Microorganisms. The S. cerevisiae species was characterized using phenotypic (API® ID32C, Biomerieux SAS) and genotypic referenced methods (genetic amplification and sequencing of 26S DNA)[24,25]. Moreover, strain I-3856 can be identified via a polymerase chain reaction interdelta typing technique[26] and complete genome sequencing. The dose tested was of 8 × 109 CFU provided daily in two capsules of 500 mg each. The probiotic dietary supplement was provided by Gnosis by Lesaffre (a business unit of Lesaffre Group, France) and comprised S. cerevisiae CNCM I-3856 entirely and exclusively. The comparative product was a placebo comprising inactive ingredients, i.e., maize starch and magnesium stearate. All capsules were made from hydroxypropyl methylcellulose of the same size, weight, colour and taste regardless of the group and prepared according to good manufacturing practices. Every subject consumed two capsules of 500 mg per day in the morning, just before breakfast with a glass of water. Compliance was determined through the assessment of returned packaging and interviews of the subjects at each visit.
The primary endpoint was the area under the curve, i.e., the sum of weekly means of daily scores of abdominal pain calculated with the trapezoidal method (interpolation of scores between weeks) from week 5 to week 8 [area under the curve (AUC) (W5-W8)], and it was determined based on previously reported data on the strain[22]. Prespecified secondary endpoints were the total AUC (W0-W8) of IBS symptoms (abdominal pain, bloating, and flatulence/borborygmi) and AUC (W5-W8) of bloating and flatulence/borborygmi scores. Mean weekly scores of gastrointestinal symptoms (abdominal pain, bloating and flatulence/borborygmi) were analysed at each week of the intervention. The evolution of abdominal pain was also assessed through the analysis of the percentage of responders. Abdominal pain response was set according to recommended guidelines[27,28]. Responders were defined as subjects who experienced a reduction of at least 30% of the mean daily abdominal pain score reported at baseline (week 0) from week 5 to week 8. The global QOL score and the eight derived subscores corresponding to the different domains of QOL were assessed at V1 and V2 and at the end of the intervention. Mean stool consistency (BSS scores) and the mean daily number of bowel movements were assessed at each week of the intervention.
The safety of the intervention was assessed considering the occurrence of adverse events and the follow-up of vital signs.
Sample size: Based on previous studies performed on IBS-C subjects, considering a 5% type-one error rate and 80% power, 205 subjects per arm would allow the detection of a 1 arbitrary unit (a.u.) difference between groups in AUC (W5-W8) of abdominal pain scores (12% difference) assuming a standard deviation of 3.6 a.u./d.wk. Enrolling a total of 456 subjects would allow for a 10% drop-out.
Efficacy analyses: Efficacy analyses were performed for the intention-to-treat (ITT) population (including all randomized subjects in the study) and for the per-protocol population (ITT population who completed the study and presented no major protocol deviations). The primary endpoint, i.e., the AUC (W5-W8) for abdominal pain, and the other AUCs of IBS symptoms were analysed using an analysis of covariance (ANCOVA) model. Repeated measurements such as the mean daily number of bowel movements, the mean stool consistency and IBS-QOL questionnaire were analysed using ANOVA models. The percentage of abdominal pain responders was analysed by a Chi2 test. IBS-QOL scores were additionally examined in exploratory analyses that focused on abdominal pain responders. These analyses were conducted through ANCOVA models for repeated measurements with the baseline (V1) as the cofactor. For all statistical tests, the 5% level of significance was used to justify a claim of a statistically significant effect and standardized mean difference (SMD) was calculated. Hochberg adjustments were used to correct for multiple testing.
Safety analyses: The safety population included all subjects who had consumed at least one dose of the products. For each term of severity and causality, the proportion of subjects showing at least an adverse event was compared between groups using a Chi2 or Fisher’s exact test. The number of events was compared between groups using a Poisson regression model.
Software: Statistical analyses were performed using SAS® software version 9.4 (SAS Institute Inc., Cary, NC, United States). Exploratory analyses were performed using R software version 4.0.3.
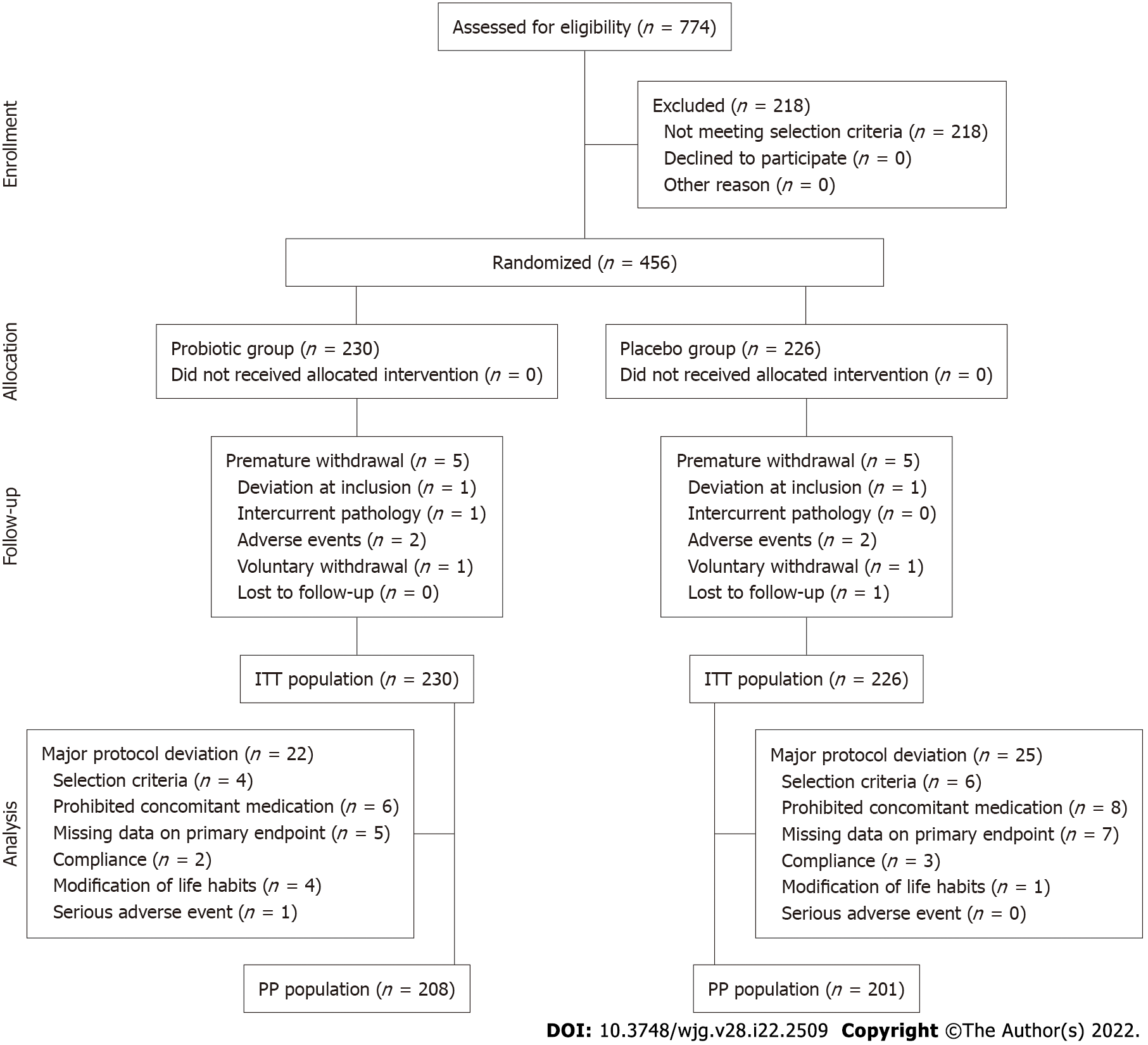
A total of 456 IBS subjects (392 females, 64 males) with predominant constipation matching the Rome IV criteria were included in this study and randomly assigned to the Probiotic group (n = 230) or the Placebo group (n = 226). The flowchart of subjects throughout the study is presented in Figure 2. The baseline characteristics of the subjects are presented in Table 1. The quantitative variables are described through the mean ± SD, and qualitative variables are described through the number of subjects and percentages (%).
| Total included subjects (n = 456) | Placebo group (n = 226) | Probiotic group (n = 230) | |
| Female | 392 (86) | 190 (84.1) | 202 (87.8) |
| Age (yr) | 40.5 ± 14.26 | 39.9 ± 14.56 | 41.2 ± 13.96 |
| Abdominal pain score | 3.98 ± 1.05 | 3.98 ± 1.07 | 3.97 ± 1.04 |
| Bloating score | 4.01 ± 1.17 | 4.04 ± 1.18 | 3.99 ± 1.15 |
| Flatulence/borborygmi score | 3.64 ± 1.37 | 3.62 ± 1.46 | 3.66 ± 1.28 |
| IBS-QOL global score | 68.0 ± 17.02 | 67.2 ± 17.17 | 68.8 ± 16.86 |
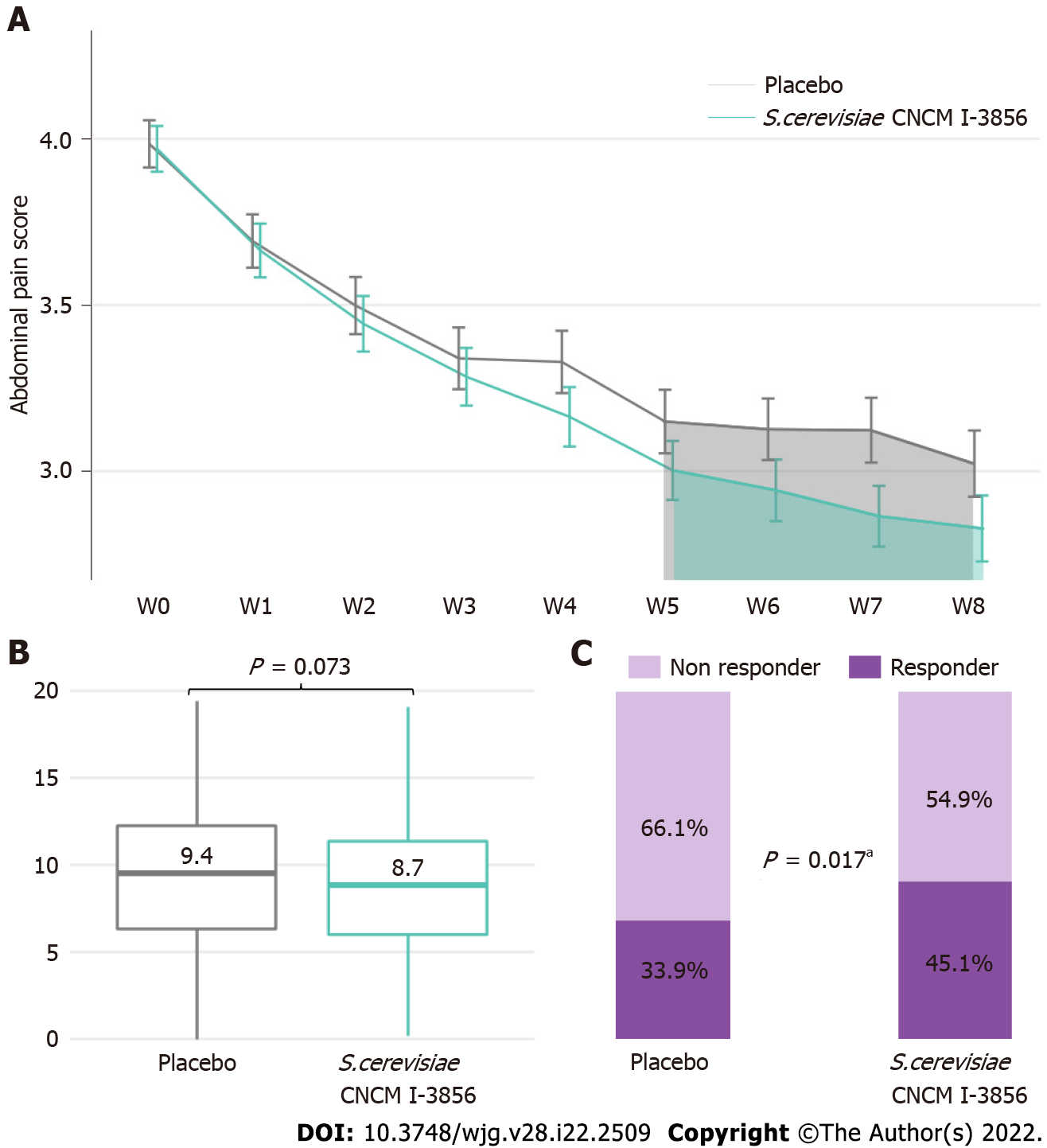
The abdominal pain scores were similar at baseline in the Probiotic (3.97 ± 1.04 a.u.) and the Placebo (3.98 ± 1.07 a.u.) groups. Significant reductions in abdominal pain scores throughout the 8 wk of supplementation were observed in the Placebo group and in the Probiotic group, with reductions of 24.1% and 28.7%, respectively, from baseline at the end of the intervention (P < 0.001 in both groups). The abdominal pain over the 8-wk intervention period decreased similarly to previously reported results. A nonsignificant difference was observed in the AUC for abdominal pain over the second month of supplementation in subjects receiving probiotic vs placebo [-6.3%, P = 0.073, 95%CI: -0.59 (-1.23; 0.05)], between-group difference from ANCOVA model) (Figure 3). Similarly, no difference was reported in the AUC over the 8 wk of intervention.
A significant difference between groups was found in the percentage of responders. The percentage of responders was significantly higher in the group receiving S. cerevisiae CNCM I-3856 (45.1%, 101 subjects among 224 subjects with available data) than in the Placebo group (33.9%, 74 subjects among 218 subjects with available data), resulting in an increase of 33% in the proportion of responders in the treated group vs placebo (Figure 3, Supplementary Figure 1) (P = 0.017, Chi2 test).
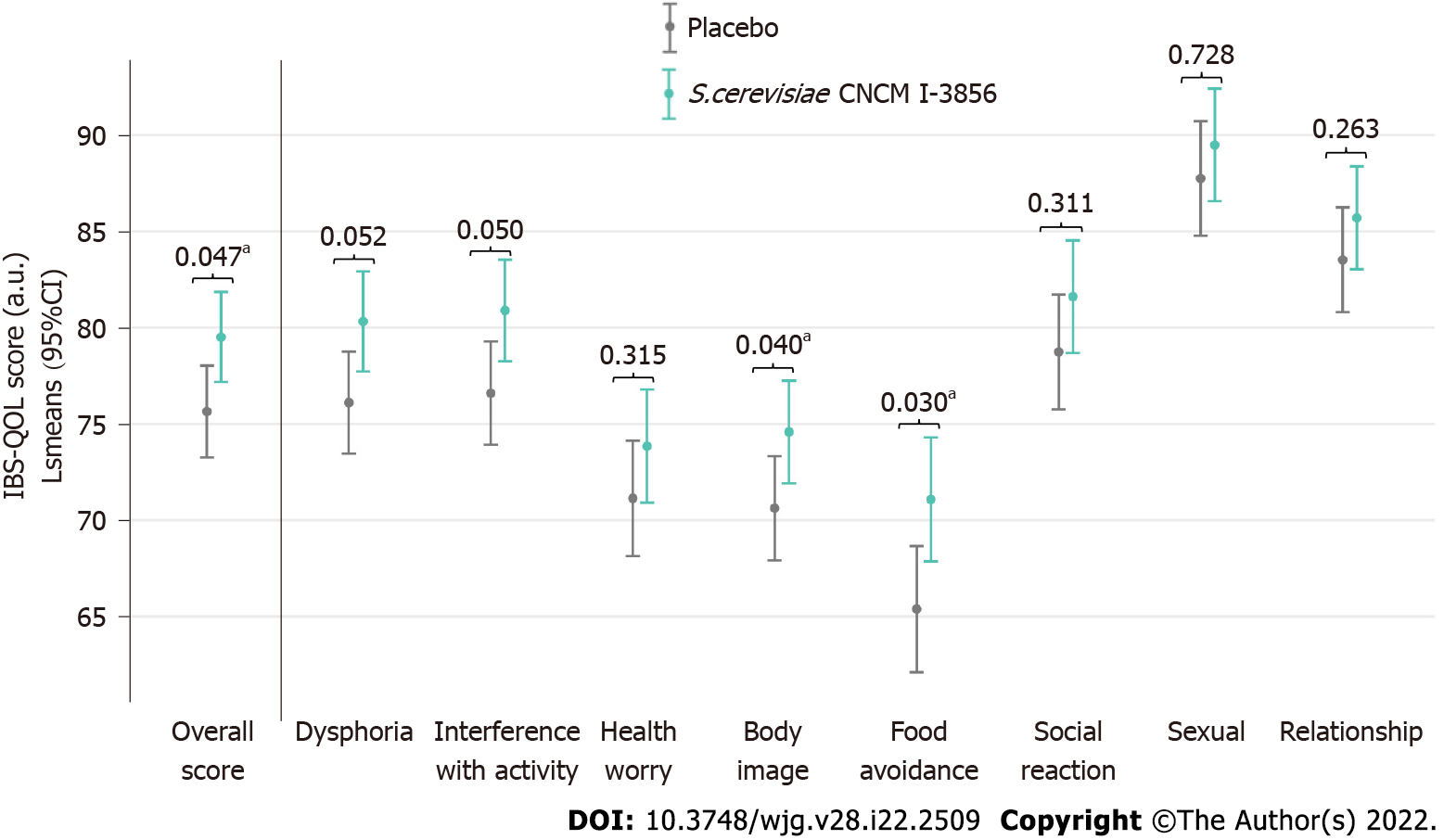
A higher overall IBS-QOL score, indicative of better QOL, was reported at the end of the intervention in the Probiotic group (79.51 ± 2.34 a.u.) compared with the Placebo group (75.65 ± 2.39 a.u.) in the PP population [P = 0.047, 95%CI: 3.86 (0.52; 7.20), SMD = 0.18]. Improved QOL in the Probiotic group translated into a mean increase in the overall IBS-QOL score of 11.9% from baseline. The analysis of the eight domains of the IBS-QOL questionnaire showed statistically significant differences in favour of the Probiotic group for 3 domains, i.e., interference with activity [P = 0.05, 95%CI: 4.30 (0.54; 8.05), SMD = 0.18)], body image [P = 0.040, 95%CI: 3.96 (0.17; 7.75), SMD = 0.17)], and food avoidance [P = 0.030, 95%CI: 5.69 (1.10; 10.28), SMD = 0.22)] (Figure 4, Supplementary Figure 2, Supplementary Table 1). Exploratory analyses of IBS-QOL scores were conducted to evaluate the evolution of the QOL among the responders during the time of supplementation with S. cerevisiae CNCM I-3856. The QOL was significantly more improved in the abdominal pain responder group than in the nonresponder group; these differences in improvement following eight weeks of intervention with S. cerevisiae CNCM I-3856 were observed for the overall score and for the eight subscores of the IBS-QOL questionnaire. The improvements with the largest difference between responders and nonresponders were for the body image score [between-group difference from ANOVA model: P < 0.001, 95%CI: 11.94 (8.53; 15.35), SMD = 0.56], health worry score [P < 0.001, 95%CI: 10.91 (7.16; 14.66), SMD = 0.43], food avoidance score [P < 0.001, 95%CI: 9.90 (5.14; 14.66), SMD = 0.38] and dysphoria score [P < 0.001, 95%CI: 8.86 (5.79; 11.92), SMD = 0.42] (Figure 5, Supplementary Figure 3, Supplementary Table 2).
At baseline, the bloating scores were similar in both groups (3.99 ± 1.52 a.u. in the Probiotic group vs 4.04 ± 1.83 a.u. in the Placebo group). Kinetic profiles of the bloating score over the 8-wk supplementation period showed a statistically significant decrease in both groups corresponding to a bloating score reduction of 28.4% (95%CI: 23.9-33.0) and 24.5% (95%CI: 19.7-29.5) in the Probiotic and Placebo groups, respectively (between W0 and W8, P < 0.001 in both groups, within-group differences from the ANCOVA model). A similar decrease in the flatulence/borborygmi score was observed in both the Placebo and Probiotic groups. The bowel movement frequency and BSS scores increased in Probiotic and Placebo groups between W0 and W8 (P < 0.01 from W1 to W8), but no statistically significant differences were found between the groups.
The number of adverse events per subject showed no statistically significant difference between the groups [P = 0.50, 95%CI: 1.10 (0.83; 1.46)], between-group difference from Poisson regression model). Similarly, there was no statistically significant difference between groups regarding the proportion of subjects with at least one adverse event (assessed for each term of severity and for adverse events whose causality with the study product or with the research was considered “not excluded”) (Table 2). Descriptive statistics of the adverse events by body system are presented in Supplementary Table 3. Three serious adverse events occurred during the study (1 in the Probiotic group and 2 in the Placebo group). The relationship with the study product was considered “not excluded” for one serious adverse event in the placebo group (bowel obstruction).
| Placebo group (n = 226) | Probiotic group (n = 230) | |
| Causality with the study product not excluded | 13 (5.8) | 15 (6.5) |
| Causality with the research not excluded | 1 (0.4) | 2 (0.9) |
| Serious | 2 (0.9) | 1 (0.4) |
| Severe | 12 (5.3) | 17 (7.4) |
| Moderate | 55 (24.3) | 74 (32.2) |
| Mild | 39 (17.3) | 46 (20.0) |
The beneficial properties of S. cerevisiae CNCM I-3856 for gastrointestinal symptom management in the IBS population have been reported in three RCTs conducted in a total of 679 participants[19-21]. An individual patient data meta-analysis reported the strongest effects of the strain in IBS with predominant constipation[22]. To validate these observations, the effect of S. cerevisiae CNCM I-3856 was specifically investigated in this population in the present clinical study.
The evolution of abdominal pain reported in IBS-C with moderate symptom severity in this study was consistent with previous findings. Lower abdominal pain intensity over the second month of supplementation was observed in the Probiotic group than in the Placebo group, although the difference was not significant. Abdominal pain alleviation during supplementation with S. cerevisiae CNCM I-3856 was confirmed by the higher proportion of abdominal pain responders in the Probiotic group than in the Placebo group. The definition of abdominal pain responder used in this study is aligned with current recommendations and corresponds to a reduction of abdominal pain intensity from baseline of at least 30%[27,28]. The higher rate of responders observed in this study during daily supplementation with S. cerevisiae CNCM I-3856 compared with placebo is consistent with previously reported results[19,22]. Pineton de Chambrun et al[19] reported a significantly higher percentage of responders in the probiotic group than in the placebo group (63% vs 47%, P = 0.04). The IPD meta-analysis conducted on S. cerevisiae CNCM I-3856 further confirmed this finding. Participants in the probiotic group had 1.51 higher odds of being a responder than participants in the placebo group (P = 0.02)[22]. The abdominal pain responder definition used in previous studies was slightly different. Responders were defined as subjects experiencing a decrease in abdominal pain intensity greater than or equal to 1 a.u. of abdominal pain score, assessed on a 7-point Likert scale, for at least 50% of the second month of supplementation. Based on the mean level of abdominal pain intensity reported at baseline in this study, a decrease of 1 a.u. would correspond to a mean 25% decrease in abdominal pain intensity. The stricter definition of the responders used in our study likely contributes to the lower percentage of abdominal pain responders reported here. However, when using a more demanding definition, the present study confirmed the beneficial effect of S. cerevisiae CNCM I-3856 on abdominal pain. This result is of great clinical interest as it meets the clinically relevance threshold previously proposed[29]. Therefore, the relevance of S. cerevisiae CNCM I-3856 in addressing abdominal pain in IBS-C is confirmed. Effective solutions to managing abdominal pain may be even more critical in this subpopulation, as recent findings have shown that individuals with IBS-C experience more bothersome, frequent and diffuse abdominal pain[30].
Importantly, this clinical study also showed improvements in QOL in the probiotic group. Indeed, significant differences were found at the end of the intervention period in the overall IBS-QOL score as well as in several domains. Notwithstanding, the magnitudes of these differences were relatively low. The consequences of IBS on daily function in addition to physical symptoms were further investigated in abdominal pain responders to provide a more accurate understanding of the overall impact of diet supplementation with S. cerevisiae CNCM I-3856.
Specific tools have been developed to capture emotional, social and physical functions. The IBS-QOL is currently the most validated self-reported QOL measure[31-33]. Here, we showed that the abdominal pain alleviation reported in responders was accompanied by significant and clinically relevant improvements in IBS-QOL. A strong association between abdominal pain and QOL has been previously described, and a causality relation has been suggested[34]. Moreover, it has also been shown that IBS patients attributed their impairment in daily functioning directly to IBS symptoms[35].
QOL improvements appeared to be mainly driven by specific domains of QOL: dysphoria, food avoidance, health worry and body image. Improvement in the food avoidance subscale of the IBS-QOL is of interest, as perceived restrictions in lifestyle related to gastrointestinal symptoms are commonly reported in the literature and encountered in clinical practice[33,35]. A considerable proportion of IBS patients report an association between food and gastrointestinal symptoms[36]. Food-related gastrointestinal symptoms have been associated with more severe IBS symptoms and lower QOL[37]. Individuals with IBS have been reported to experience emotional dysphoria, which can also be described as feeling helpless, out of control and depressed. It may therefore not be surprising that individuals experiencing significant abdominal pain alleviation also reported improvement in the dysphoria subscale of the IBS-QOL. In addition, significant improvement was seen in the body image subscale of the IBS-QOL. This result also appears consistent with the literature, as individuals with IBS-C have been described as more likely to internalize their distress and to feel self-conscious about their body image[38].
In contrast with previous findings, no significant between-group differences were observed in the AUC for gastrointestinal symptoms. Although the clinical studies conducted on S. cerevisiae CNCM I-3856 in IBS present consistent designs, a significant change here is the use of Rome IV criteria to select the participants. A worldwide comparison of IBS prevalence by Rome IV and Rome III diagnostic criteria demonstrated that individuals diagnosed by Rome IV criteria exhibit higher IBS severity. Consistently, a higher level of abdominal pain was reported at baseline in this study than in previous clinical trials conducted on S. cerevisiae CNCM I-3856. Among factors associated with response to placebo in IBS-C, higher baseline symptom severity was reported as an important predictor of placebo response[40]. Differences in the studied population could therefore have contributed to the lower between-group size effect reported in this study.
Previous studies have reported statistically significant effects of this probiotic on bowel transit in IBS-C, IBS-D and IBS-M, assessed by daily reporting of bowel movement frequency and consistency[22,21]. In contrast, we did not find between-group differences in bowel movement frequency or consistency in this study. Spiller et al[20] highlighted the possible role of accelerated bowel transit as central in the relief of abdominal pain and bloating in IBS-C. Instead, the absence of a significant effect on bowel transit in this study as well as the reported improvements in abdominal pain in all IBS subtypes suggest that other mechanisms of action may be involved and participate in the clinical benefits.
Several putative mechanisms of action of S. cerevisiae CNCM I-3856 can be hypothesized. First, the anti-inflammatory effects of S. cerevisiae CNCM I-3856 have been reported in several preclinical models[41-45]. The immune-modulating properties of the strain may be relevant in IBS, as chronic low-grade intestinal mucosal inflammation has been implicated in IBS pathophysiology. Second, interactions with the gut microbiota might influence the multiple factors involved in IBS pathophysiology[12,46]. The results from trials conducted in a Simulator of the Human Intestinal Microbial Ecosystem (SHIME®) suggest that S. cerevisiae CNCM I-3856 can modulate gut microbiota activity towards an increase in short-chain fatty acids (SCFAs)[47]. This result may be of particular importance, as a recently published longitudinal multiomics study showed significantly lower levels of SCFAs in the stool samples of IBS-C patients than in those of healthy controls[48]. In addition, several lines of evidence suggest that increased levels of SCFAs, such as butyrate, may be beneficial in IBS management[49-51]. Nevertheless, these possible mechanisms of action remain speculative and would need to be addressed separately. Differences in microbiota composition and function between abdominal pain responders and nonresponders may provide a mechanistic basis for the beneficial effects of S. cerevisiae CNCM I-3856 in IBS management and warrant further exploration.
In conclusion, the results of this large-scale clinical study are consistent with previous findings and confirm the safety and efficacy of S. cerevisiae CNCM I-3856 for abdominal pain management in IBS-C. In addition, abdominal pain alleviation was associated with significant improvements in IBS-related QOL. Dietary supplementation with S. cerevisiae CNCM I-3856 therefore appears to be an interesting complementary or alternative solution for IBS management with positive implications for the day-to-day life of individuals with IBS-C.
The gut microbiota has been proposed as central in irritable bowel syndrome (IBS) pathophysiology, and microbiota-directed intervention has therefore drawn considerable interest. Among them, Saccharomyces cerevisiae (S. cerevisiae) CNCM I-3856 is a probiotic yeast that has emerged as a recognized solution for managing IBS.
S. cerevisiae I-3856 has demonstrated beneficial effects in IBS subjects, particularly in IBS with predominant constipation.
To confirm the efficacy of S. cerevisiae CNCM I-3856 on gastrointestinal symptom management in an IBS population with predominant constipation.
A total of 456 subjects were enrolled in a randomized, double-blind, placebo-controlled trial. After a run-in period to confirm IBS diagnosis, subjects were randomly assigned to the group receiving the probiotic or the placebo for 8 wk and performed daily self-evaluations of gastrointestinal symptoms. The primary objective was to assess the effect of the probiotic on abdominal pain. The secondary objectives were the evaluation of other gastrointestinal symptoms, bowel movement frequency and consistency, and quality of life (QOL).
Abdominal pain alleviation during supplementation with S. cerevisiae CNCM I-3856 was confirmed by the higher proportion of abdominal pain responders in the probiotic group than in the placebo group. Importantly, this clinical study also showed improvements in QOL in the probiotic group.
The results of this large-scale clinical study are consistent with previous findings and confirm the safety and efficacy of S. cerevisiae CNCM I-3856 for abdominal pain management in IBS population. In addition, abdominal pain alleviation was associated with significant improvements in IBS-related QOL.
Dietary supplementation with S. cerevisiae CNCM I-3856 appears to be an interesting complementary or alternative solution for IBS management with positive implications for the day-to-day life of individuals with IBS with predominant constipation. Differences in microbiota composition and function between abdominal pain responders and nonresponders may provide a mechanistic basis for the beneficial effects of S. cerevisiae CNCM I-3856 in IBS management and warrant further exploration.
The authors want to acknowledge Biofortis Merieux Nutrisciences and all the investigators for conducting the study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: France
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Dumitrascu DL, McFarland LV S-Editor: Zhang H L-Editor: A P-Editor: Zhang H
| 1. | Drossman DA. Functional Gastrointestinal Disorders: History, Pathophysiology, Clinical Features and Rome IV. Gastroenterology. 2016;. [PubMed] [DOI] [Cited in This Article: ] |
| 2. | Black CJ, Ford AC. Global burden of irritable bowel syndrome: trends, predictions and risk factors. Nat Rev Gastroenterol Hepatol. 2020;17:473-486. [PubMed] [DOI] [Cited in This Article: ] |
| 3. | Hungin AP, Whorwell PJ, Tack J, Mearin F. The prevalence, patterns and impact of irritable bowel syndrome: an international survey of 40,000 subjects. Aliment Pharmacol Ther. 2003;17:643-650. [PubMed] [DOI] [Cited in This Article: ] |
| 4. | Canavan C, West J, Card T. Review article: the economic impact of the irritable bowel syndrome. Aliment Pharmacol Ther. 2014;40:1023-1034. [PubMed] [DOI] [Cited in This Article: ] |
| 5. | El-Serag HB, Olden K, Bjorkman D. Health-related quality of life among persons with irritable bowel syndrome: a systematic review. Aliment Pharmacol Ther. 2002;16:1171-1185. [PubMed] [DOI] [Cited in This Article: ] |
| 6. | Halder SL, Locke GR 3rd, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ 3rd. Impact of functional gastrointestinal disorders on health-related quality of life: a population-based case-control study. Aliment Pharmacol Ther. 2004;19:233-242. [PubMed] [DOI] [Cited in This Article: ] |
| 7. | Simrén M, Svedlund J, Posserud I, Björnsson ES, Abrahamsson H. Health-related quality of life in patients attending a gastroenterology outpatient clinic: functional disorders versus organic diseases. Clin Gastroenterol Hepatol. 2006;4:187-195. [PubMed] [DOI] [Cited in This Article: ] |
| 8. | Aziz I, Palsson OS, Törnblom H, Sperber AD, Whitehead WE, Simrén M. The Prevalence and Impact of Overlapping Rome IV-Diagnosed Functional Gastrointestinal Disorders on Somatization, Quality of Life, and Healthcare Utilization: A Cross-Sectional General Population Study in Three Countries. Am J Gastroenterol. 2018;113:86-96. [PubMed] [DOI] [Cited in This Article: ] |
| 9. | Tack J, Stanghellini V, Mearin F, Yiannakou Y, Layer P, Coffin B, Simren M, Mackinnon J, Wiseman G, Marciniak A; IBIS-C Study group. Economic burden of moderate to severe irritable bowel syndrome with constipation in six European countries. BMC Gastroenterol. 2019;19:69. [PubMed] [DOI] [Cited in This Article: ] |
| 10. | Frändemark Å, Törnblom H, Jakobsson S, Simrén M. Work Productivity and Activity Impairment in Irritable Bowel Syndrome (IBS): A Multifaceted Problem. Am J Gastroenterol. 2018;113:1540-1549. [PubMed] [DOI] [Cited in This Article: ] |
| 11. | Camilleri M, Ford AC. Pharmacotherapy for Irritable Bowel Syndrome. J Clin Med. 2017;6. [PubMed] [DOI] [Cited in This Article: ] |
| 12. | Carco C, Young W, Gearry RB, Talley NJ, McNabb WC, Roy NC. Increasing Evidence That Irritable Bowel Syndrome and Functional Gastrointestinal Disorders Have a Microbial Pathogenesis. Front Cell Infect Microbiol. 2020;10:468. [PubMed] [DOI] [Cited in This Article: ] |
| 13. | Bhattarai Y, Muniz Pedrogo DA, Kashyap PC. Irritable bowel syndrome: a gut microbiota-related disorder? Am J Physiol Gastrointest Liver Physiol. 2017;312:G52-G62. [PubMed] [DOI] [Cited in This Article: ] |
| 14. | Simrén M, Barbara G, Flint HJ, Spiegel BM, Spiller RC, Vanner S, Verdu EF, Whorwell PJ, Zoetendal EG; Rome Foundation Committee. Intestinal microbiota in functional bowel disorders: a Rome foundation report. Gut. 2013;62:159-176. [PubMed] [DOI] [Cited in This Article: ] |
| 15. | Hungin APS, Mitchell CR, Whorwell P, Mulligan C, Cole O, Agréus L, Fracasso P, Lionis C, Mendive J, Philippart de Foy JM, Seifert B, Wensaas KA, Winchester C, de Wit N; European Society for Primary Care Gastroenterology. Systematic review: probiotics in the management of lower gastrointestinal symptoms - an updated evidence-based international consensus. Aliment Pharmacol Ther. 2018;47:1054-1070. [PubMed] [DOI] [Cited in This Article: ] |
| 16. | Ford AC, Harris LA, Lacy BE, Quigley EMM, Moayyedi P. Systematic review with meta-analysis: the efficacy of prebiotics, probiotics, synbiotics and antibiotics in irritable bowel syndrome. Aliment Pharmacol Ther. 2018;48:1044-1060. [PubMed] [DOI] [Cited in This Article: ] |
| 17. | Preidis GA, Weizman AV, Kashyap PC, Morgan RL. AGA Technical Review on the Role of Probiotics in the Management of Gastrointestinal Disorders. Gastroenterology. 2020;159:708-738.e4. [PubMed] [DOI] [Cited in This Article: ] |
| 18. | McFarland LV, Karakan T, Karatas A. Strain-specific and outcome-specific efficacy of probiotics for the treatment of irritable bowel syndrome: A systematic review and meta-analysis. EClinicalMedicine. 2021;41:101154. [PubMed] [DOI] [Cited in This Article: ] |
| 19. | Pineton de Chambrun G, Neut C, Chau A, Cazaubiel M, Pelerin F, Justen P, Desreumaux P. A randomized clinical trial of Saccharomyces cerevisiae versus placebo in the irritable bowel syndrome. Dig Liver Dis. 2015;47:119-124. [PubMed] [DOI] [Cited in This Article: ] |
| 20. | Spiller R, Pélerin F, Cayzeele Decherf A, Maudet C, Housez B, Cazaubiel M, Jüsten P. Randomized double blind placebo-controlled trial of Saccharomyces cerevisiae CNCM I-3856 in irritable bowel syndrome: improvement in abdominal pain and bloating in those with predominant constipation. United European Gastroenterol J. 2016;4:353-362. [PubMed] [DOI] [Cited in This Article: ] |
| 21. | Gayathri R, Aruna T, Malar S, Shilpa B, Dhanasekar KR. Efficacy of Saccharomyces cerevisiae CNCM I-3856 as an add-on therapy for irritable bowel syndrome. Int J Colorectal Dis. 2020;35:139-145. [PubMed] [DOI] [Cited in This Article: ] |
| 22. | Cayzeele-Decherf A, Pélerin F, Leuillet S, Douillard B, Housez B, Cazaubiel M, Jacobson GK, Jüsten P, Desreumaux P. Saccharomyces cerevisiae CNCM I-3856 in irritable bowel syndrome: An individual subject meta-analysis. World J Gastroenterol. 2017;23:336-344. [PubMed] [DOI] [Cited in This Article: ] |
| 23. | Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R. Bowel Disorders. Gastroenterology. 2016;. [PubMed] [DOI] [Cited in This Article: ] |
| 24. | Kurtzman CP, Robnett CJ. Identification of clinically important ascomycetous yeasts based on nucleotide divergence in the 5' end of the large-subunit (26S) ribosomal DNA gene. J Clin Microbiol. 1997;35:1216-1223. [PubMed] [DOI] [Cited in This Article: ] |
| 25. | Kurtzman CP, Robnett CJ. Identification and phylogeny of ascomycetous yeasts from analysis of nuclear large subunit (26S) ribosomal DNA partial sequences. Antonie Van Leeuwenhoek. 1998;73:331-371. [PubMed] [DOI] [Cited in This Article: ] |
| 26. | European Committee for Standardization. CEN/TS 15790:2008-Animal feeding stuffs-PCR typing of probiotic strains of Saccharomyces cerevisiae (yeast). [cited 2021 Dec 12]. Available from: https://standards.iteh.ai/catalog/standards/cen/c4e77d66-4f75-4955-a168-bd50a4845cb1/cen-ts-15790-2008. [Cited in This Article: ] |
| 27. | European Medicines Agency. Guideline on the evaluation of medicinal products for the treatment of irritable bowel syndrome. [cited 2021 Dec 12]. Available from: https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-evaluation-medicinal-products-treatment-irritable-bowel-syndrome-revision-1_en.pdf. [Cited in This Article: ] |
| 28. | Food and Drug Administration. Guidance for Industry on Irritable Bowel Syndrome-Clinical Evaluation of Drugs for Treatment. [cited 2021 Dec 12]. Available from: https://www.federalregister.gov/documents/2012/05/31/2012-13143/guidance-for-industry-on-irritable-bowel-syndrome-clinical-evaluation-of-drugs-for-treatment. [Cited in This Article: ] |
| 29. | Chang L, Lembo A, Sultan S. American Gastroenterological Association Institute Technical Review on the pharmacological management of irritable bowel syndrome. Gastroenterology. 2014;147:1149-72.e2. [PubMed] [DOI] [Cited in This Article: ] |
| 30. | Shah ED, Almario CV, Spiegel BM, Chey WD. Presentation and Characteristics of Abdominal Pain Vary by Irritable Bowel Syndrome Subtype: Results of a Nationwide Population-Based Study. Am J Gastroenterol. 2020;115:294-301. [PubMed] [DOI] [Cited in This Article: ] |
| 31. | Patrick DL, Drossman DA, Frederick IO, DiCesare J, Puder KL. Quality of life in persons with irritable bowel syndrome: development and validation of a new measure. Dig Dis Sci. 1998;43:400-411. [PubMed] [DOI] [Cited in This Article: ] |
| 32. | Drossman DA, Patrick DL, Whitehead WE, Toner BB, Diamant NE, Hu Y, Jia H, Bangdiwala SI. Further validation of the IBS-QOL: a disease-specific quality-of-life questionnaire. Am J Gastroenterol. 2000;95:999-1007. [PubMed] [DOI] [Cited in This Article: ] |
| 33. | Drossman D, Morris CB, Hu Y, Toner BB, Diamant N, Whitehead WE, Dalton CB, Leserman J, Patrick DL, Bangdiwala SI. Characterization of health related quality of life (HRQOL) for patients with functional bowel disorder (FBD) and its response to treatment. Am J Gastroenterol. 2007;102:1442-1453. [PubMed] [DOI] [Cited in This Article: ] |
| 34. | Cain KC, Headstrom P, Jarrett ME, Motzer SA, Park H, Burr RL, Surawicz CM, Heitkemper MM. Abdominal pain impacts quality of life in women with irritable bowel syndrome. Am J Gastroenterol. 2006;101:124-132. [PubMed] [DOI] [Cited in This Article: ] |
| 35. | Ballou S, Keefer L. The impact of irritable bowel syndrome on daily functioning: Characterizing and understanding daily consequences of IBS. Neurogastroenterol Motil. 2017;29. [PubMed] [DOI] [Cited in This Article: ] |
| 36. | Simrén M, Månsson A, Langkilde AM, Svedlund J, Abrahamsson H, Bengtsson U, Björnsson ES. Food-related gastrointestinal symptoms in the irritable bowel syndrome. Digestion. 2001;63:108-115. [PubMed] [DOI] [Cited in This Article: ] |
| 37. | Böhn L, Störsrud S, Törnblom H, Bengtsson U, Simrén M. Self-reported food-related gastrointestinal symptoms in IBS are common and associated with more severe symptoms and reduced quality of life. Am J Gastroenterol. 2013;108:634-641. [PubMed] [DOI] [Cited in This Article: ] |
| 38. | Ballou S, McMahon C, Lee HN, Katon J, Shin A, Rangan V, Singh P, Nee J, Camilleri M, Lembo A, Iturrino J. Effects of Irritable Bowel Syndrome on Daily Activities Vary Among Subtypes Based on Results From the IBS in America Survey. Clin Gastroenterol Hepatol. 2019;17:2471-2478.e3. [PubMed] [DOI] [Cited in This Article: ] |
| 39. | Ford AC, Moayyedi P. Meta-analysis: factors affecting placebo response rate in the irritable bowel syndrome. Aliment Pharmacol Ther. 2010;32:144-158. [PubMed] [DOI] [Cited in This Article: ] |
| 40. | Ballou S, Beath A, Kaptchuk TJ, Hirsch W, Sommers T, Nee J, Iturrino J, Rangan V, Singh P, Jones M, Lembo A. Factors Associated With Response to Placebo in Patients With Irritable Bowel Syndrome and Constipation. Clin Gastroenterol Hepatol. 2018;16:1738-1744.e1. [PubMed] [DOI] [Cited in This Article: ] |
| 41. | Foligné B, Dewulf J, Vandekerckove P, Pignède G, Pot B. Probiotic yeasts: anti-inflammatory potential of various non-pathogenic strains in experimental colitis in mice. World J Gastroenterol. 2010;16:2134-2145. [PubMed] [DOI] [Cited in This Article: ] |
| 42. | Zanello G, Berri M, Dupont J, Sizaret PY, D'Inca R, Salmon H, Meurens F. Saccharomyces cerevisiae modulates immune gene expressions and inhibits ETEC-mediated ERK1/2 and p38 signaling pathways in intestinal epithelial cells. PLoS One. 2011;6:e18573. [PubMed] [DOI] [Cited in This Article: ] |
| 43. | Jawhara S, Habib K, Maggiotto F, Pignede G, Vandekerckove P, Maes E, Dubuquoy L, Fontaine T, Guerardel Y, Poulain D. Modulation of intestinal inflammation by yeasts and cell wall extracts: strain dependence and unexpected anti-inflammatory role of glucan fractions. PLoS One. 2012;7:e40648. [PubMed] [DOI] [Cited in This Article: ] |
| 44. | Sivignon A, de Vallée A, Barnich N, Denizot J, Darcha C, Pignède G, Vandekerckove P, Darfeuille-Michaud A. Saccharomyces cerevisiae CNCM I-3856 prevents colitis induced by AIEC bacteria in the transgenic mouse model mimicking Crohn's disease. Inflamm Bowel Dis. 2015;21:276-286. [PubMed] [DOI] [Cited in This Article: ] |
| 45. | Roussel C, Sivignon A, de Vallée A, Garrait G, Denis S, Tsilia V, Ballet N, Vandekerckove P, Van de Wiele T, Barnich N, Blanquet-Diot S. Anti-infectious properties of the probiotic Saccharomyces cerevisiae CNCM I-3856 on enterotoxigenic E. coli (ETEC) strain H10407. Appl Microbiol Biotechnol. 2018;102:6175-6189. [PubMed] [DOI] [Cited in This Article: ] |
| 46. | Gu Y, Zhou G, Qin X, Huang S, Wang B, Cao H. The Potential Role of Gut Mycobiome in Irritable Bowel Syndrome. Front Microbiol. 2019;10:1894. [PubMed] [DOI] [Cited in This Article: ] |
| 47. | Roussel C, De Paepe K, Galia W, de Bodt J, Chalancon S, Denis S, Leriche F, Vandekerkove P, Ballet N, Blanquet-Diot S, Van de Wiele T. Multi-targeted properties of the probiotic saccharomyces cerevisiae CNCM I-3856 against enterotoxigenic escherichia coli (ETEC) H10407 pathogenesis across human gut models. Gut Microbes. 2021;13:1953246. [PubMed] [DOI] [Cited in This Article: ] |
| 48. | Mars RAT, Yang Y, Ward T, Houtti M, Priya S, Lekatz HR, Tang X, Sun Z, Kalari KR, Korem T, Bhattarai Y, Zheng T, Bar N, Frost G, Johnson AJ, van Treuren W, Han S, Ordog T, Grover M, Sonnenburg J, D'Amato M, Camilleri M, Elinav E, Segal E, Blekhman R, Farrugia G, Swann JR, Knights D, Kashyap PC. Longitudinal Multi-omics Reveals Subset-Specific Mechanisms Underlying Irritable Bowel Syndrome. Cell. 2020;182:1460-1473.e17. [PubMed] [DOI] [Cited in This Article: ] |
| 49. | Zhang J, Song L, Wang Y, Liu C, Zhang L, Zhu S, Liu S, Duan L. Beneficial effect of butyrate-producing Lachnospiraceae on stress-induced visceral hypersensitivity in rats. J Gastroenterol Hepatol. 2019;34:1368-1376. [PubMed] [DOI] [Cited in This Article: ] |
| 50. | Banasiewicz T, Krokowicz Ł, Stojcev Z, Kaczmarek BF, Kaczmarek E, Maik J, Marciniak R, Krokowicz P, Walkowiak J, Drews M. Microencapsulated sodium butyrate reduces the frequency of abdominal pain in patients with irritable bowel syndrome. Colorectal Dis. 2013;15:204-209. [PubMed] [DOI] [Cited in This Article: ] |
| 51. | El-Salhy M, Valeur J, Hausken T, Gunnar Hatlebakk J. Changes in fecal short-chain fatty acids following fecal microbiota transplantation in patients with irritable bowel syndrome. Neurogastroenterol Motil. 2021;33:e13983. [PubMed] [DOI] [Cited in This Article: ] |