Published online Mar 7, 2015. doi: 10.3748/wjg.v21.i9.2854
Peer-review started: August 2, 2014
First decision: August 15, 2014
Revised: October 30, 2014
Accepted: November 30, 2014
Article in press: December 1, 2014
Published online: March 7, 2015
Fibrin glue is widely used in clinical practice and plays an important role in reducing postoperative complications. We report a case of a 65-year-old man, whose common bile duct was injured by fibrin glue, with a history of failed laparoscopic cholecystectomy and open operation for uncontrolled laparoscopic bleeding. In view of the persistent liver dysfunction, xanthochromia and skin itching, the patient was admitted to us for further management. Ultrasound, computed tomography, and magnetic resonance cholangiopancreatography (MRCP) revealed multiple stones in the common bile duct, and liver function tests confirmed the presence of obstructive jaundice and liver damage. Endoscopic retrograde cholangiopancreatography was unsuccessfully performed to remove choledocholithiasis, but a small amount of tissue was removed and pathologically confirmed as calcified biliary mucosa. This was followed by open surgery for suspicious cholangiocarcinoma. There was no evidence of cholangiocarcinoma, but the common bile duct wall had a defect of 8 mm × 10 mm at Calot’s triangle. A hard, grid-like foreign body was removed, which proved to be solid fibrin glue. Subsequently, the residual choledocholithiasis was removed by a choledochoscopic procedure, and the common bile duct deletion was repaired by liver round ligament with T-tube drainage. Six months later, endoscopy was performed through the T-tube fistula and showed a well-repaired bile duct wall. Eight months later, MRCP confirmed no bile duct stenosis. A review of reported cases showed that fibrin glue is widely used in surgery, but it can also cause organ damage. Its mechanism may be related to discharge reactions.
Core tip: Fibrin glue is a biodegradable and absorbable biological agent, which can be used to close wounds and fistulous tracts, reducing leakage and bleeding, promoting wound healing, and preventing adhesion. It is widely used in surgery. In our case, fibrin glue resulted in obstructive jaundice and injury of the common bile duct wall, which was repaired by liver round ligament without bile duct stricture. Its mechanism may be related to discharge reactions.
- Citation: Yang YL, Zhang C, Zhang HW, Wu P, Ma YF, Lin MJ, Shi LJ, Li JY, Zhao M. Common bile duct injury by fibrin glue: Report of a rare complication. World J Gastroenterol 2015; 21(9): 2854-2857
- URL: https://www.wjgnet.com/1007-9327/full/v21/i9/2854.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i9.2854
Fibrin glue is a biodegradable and absorbable biological agent, which is widely used in abdominal operations to close the wound and fistulous tract, reduce leakage and bleeding, promote wound healing, and prevent adhesion[1-3]. Several studies have reported the use of fibrin glues in neurosurgery, otolaryngology, cardiothoracic surgery, and gynecology[4-9]. Several recent studies have suggested that the use of fibrin glue can reduce the time required to control intraoperative bleeding from the raw liver surface after liver resection, but there is no solid evidence that their routine use reduces the incidence of postoperative hemorrhage or bile leakage compared with other treatments[10,11]. We now report a case of common bile duct injury, associated with fibrin glue used in the failure of laparoscopic cholecystectomy and open surgery for uncontrolled laparoscopic bleeding.
A 65-year-old man presented to our hospital for further evaluation of icteric skin and sclera. The patient had a history of cholecystolithiasis three years ago, for which he underwent failed laparoscopic cholecystectomy, and reverted to open surgery for uncontrollable laparoscopic bleeding. One year after cholecystectomy, he had choledocholithiasis and endoscopic retrograde cholangiopancreatography (ERCP) was performed; all the stones were removed. Three days prior to admission, he had symptoms of icteric skin and sclera with persistent pain under the xiphoid.
On admission, routine laboratory evaluation showed a total bilirubin level of 107.9 μmol/L (reference range: 3-22 μmol/L); conjugated bilirubin 40.2 μmol/L (reference range: 0-5 μmol/L); unconjugated hyperbilirubinemia 37.6 μmol/L (reference range: 0-19 μmol/L); alanine aminotransferase 154 U/L (reference range: 0-40 U/L) aspartate aminotransferase 69 U/L (reference range: 0-40 U/L); alkaline phosphatase 284 U/L (reference range: 38-126 U/L); and γ-glutamyl transferase 616 U/L (reference range: 6-35 U/L). Routine blood analysis showed normal serum amylase/lipase, blood clotting, and tumor markers including α-fetoprotein, carcinoembryonic antigen, cancer antigen (CA)-125 and CA19-9.
Abdominal ultrasound demonstrated mild intrahepatic and extrahepatic bile duct dilatation, bile duct diameter 12 mm, and nonhomogeneous echo of the common bile duct. Biliary sludge, sand-like stones, and bile duct cancer were excluded. Computed tomography (CT) demonstrated intrahepatic bile duct dilatation, fatty liver, and splenomegaly (Figure 1). Magnetic resonance cholangiopancreatography (MRCP) demonstrated multiple stones in the extrahepatic bile duct and common bile duct, dilated intrahepatic bile duct, and cholecystectomy change (Figure 2).
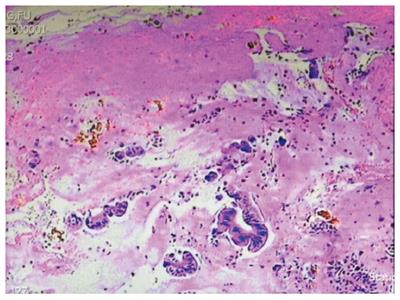
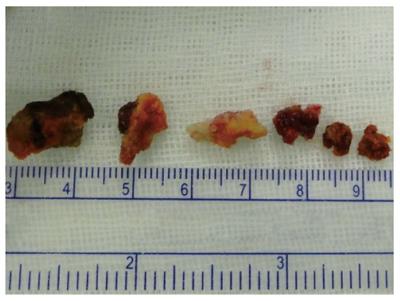
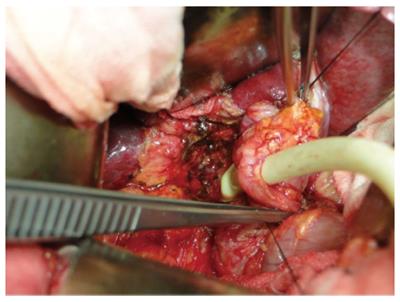
ERCP was performed to treat the choledocholithiasis, but only some stones were removed, and the common bile duct was rigid, with some tissue removed. Pathological analysis confirmed calcified biliary mucosa (Figure 3), which was followed by open surgery for suspicious cholangiocarcinoma. There was no evidence of cholangiocarcinoma, but the common bile duct wall had a defect of 8 mm × 10 mm at Calot’s triangle. A hard, grid-like foreign body was removed, which proved to be solid fibrin glue (manufacturer unknown) (Figure 4). Subsequently, the residual choledocholithiasis was cleared by a choledochoscopic procedure, and the injury of the common bile duct was repaired by longitudinal, slivered, pedunculated liver round ligament with the serous face towards the bile duct, and T-tube drainage from the middle of the liver round ligament (Figure 5). Two weeks later, T-tube visualization was performed and the contrast agent was introduced smoothly into the duodenum with no extravasation or bile duct stenosis (Figure 6). Six months later, endoscopy was performed through the T-tube fistula, with good repair of the bile duct wall. Eight months later, MRCP confirmed the absence of bile duct stenosis.
Fibrin glue is a biodegradable, absorbable biological agent, which is widely used in surgery to reduce leakage and bleeding from the wound, promote wound healing, and prevent adhesion. Capillary and fibroblast proliferation appears around the periphery and inside the wound within 3 d, the fibrin polymer disappears after 7 d and the wound is considered to be fully healed[12]. The current example showed fibrin glue had not been absorbed in the body for 3 years, and the ranked reactions of organization to fibrin glue may have affected its absorption. This phenomenon is a rare complication, similar to titanium clip and surgical suture migration into the common bile duct following open or laparoscopic cholecystectomy, and the migration time ranges from 10 d to 10 years[13,14]. The solid fibrin glue can be extruded from the bile duct, which ultimately causes bile duct defects and stricture, during endoscopic stone extraction. The etiology of this complication may be linked to a chronic rejection reaction of the body to fibrin glue, application of a large dose or improper use, such as local injection.
Preoperative abdominal ultrasound, CT and MRCP revealed multiple stones in the common bile duct, with no evidence of cholangiocarcinoma. However, the common bile duct felt rigid and not all the stones could be removed by ERCP, which revealed possible cholangiocarcinoma. Histopathology of tissue removed by ERCP confirmed calcified biliary mucosa. Therefore, intraoperative histopathological examination is particularly important. The tissue patch of omentum majus, omentum minus, gallbladder wall, and ligamentum teres hepatis can be used to repair bile duct defects[15,16]. The pedicle patch, formed by the longitudinal, slivered, pedunculated liver round ligament, was used to repair the bile duct defect, with the serous face towards the bile duct. There was no abdominal infection, tissue necrosis or other serious complications. Cholangiography and biliary endoscopy showed good repair without iatrogenic bile duct stricture. However, there is some controversy surrounding the postoperative use of T-tubes. Some researchers believe that the T-tube can be removed if angiography shows absence of biliary bile duct stenosis at 3 mo after extrahepatic bile duct injury with the liver round ligament[16,17]. A support tube should be placed, < 12 mo, to reduce the incidence of postoperative biliary strictures[18].
We should strictly control the use of fibrin glue in surgery, and large doses of fibrin glue for bleeding and bile duct bile leakage should be prohibited. There is no scientific proof that topical haemostatic agents really reduce resection surface related complications[19]. Bile duct injury may be avoided by incomplete absorption and discharge reactions of the fibrin glue. The effect of using liver round ligament to repair extrahepatic bile duct is satisfactory, which is worthy of promotion for clinical use, but the time of placement time of the support tube needs verified in further animal experiments.
A 65-year-old man presented with common bile duct injury caused by fibrin glue.
The patient was initially admitted for icteric skin and sclera caused by common bile duct stones.
The differential diagnosis was cholangiocarcinoma.
Routine blood tests showed: total bilirubin 107.9 μmol/L, conjugated bilirubin 40.2 μmol/L, unconjugated hyperbilirubinemia 37.6 μmol/L, alanine aminotransferase 154 U/L, aspartate aminotransferase 69 U/L, alkaline phosphatase 284 U/L, and γ-glutamyl transferase 616 U/L.
Preoperative ultrasound, computed tomography and magnetic resonance cholangiopancreatography indicated multiple stones in the extrahepatic bile duct and common bile duct, dilated intrahepatic bile duct, and cholecystectomy change.
Pathological analysis confirmed calcified biliary mucosa.
Open surgery was performed to clear the stones by a choledochoscopic procedure and the injury of the common bile duct was repaired by liver round ligament.
The use of fibrin glue should strictly be controlled in surgery, and large doses of fibrin glue for bleeding and bile duct bile leakage should be carefully monitored.
This is an important complication caused by fibrin glue and this case report may be interest to the readers of this journal.
P- Reviewer: Athanasopoulos PG, Harada R, Piccinni G, Sharma M, Sun LM S- Editor: Gou SX L- Editor: O’Neill M E- Editor: Zhang DN
| 1. | Chan MS, Teoh AY, Chan KW, Tang YC, Ng EK, Leong HT. Randomized double-blinded prospective trial of fibrin sealant spray versus mechanical stapling in laparoscopic total extraperitoneal hernioplasty. Ann Surg. 2014;259:432-437. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | Evaristo-Méndez G, Sánchez-Hernández AT, Melo-Velázquez A, Ventura-Sauceda FA, Sepúlveda-Castro RR. [Sigmoido-buttock fistula by diverticulitis: report of a rare complication]. Cir Cir. 2013;81:158-162. [PubMed] [Cited in This Article: ] |
| 3. | Hiura Y, Takiguchi S, Yamamoto K, Kurokawa Y, Yamasaki M, Nakajima K, Miyata H, Fujiwara Y, Mori M, Doki Y. Use of fibrin glue sealant with polyglycolic acid sheets to prevent pancreatic fistula formation after laparoscopic-assisted gastrectomy. Surg Today. 2013;43:527-533. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Cagatay HH, Gokce G, Ekinci M, Koban Y, Daraman O, Ceylan E. Long-term comparison of fibrin tissue glue and vicryl suture in conjunctival autografting for pterygium surgery. Postgrad Med. 2014;126:97-103. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Ussat S, Lodes U, Wex C, Rapp L, Schulz HU, Meyer F. [Successful closure of a postoperative esophagobronchial fistula following esophageal resection using fibrin glue]. Dtsch Med Wochenschr. 2013;138:1406-1409. [PubMed] [Cited in This Article: ] |
| 6. | Fussey JM, Luesley DM, Sterne GD. Vaginoplasty: a modern approach: a report of 2 cases. J Reprod Med. 2013;58:441-444. [PubMed] [Cited in This Article: ] |
| 7. | Rousou JA. Use of fibrin sealants in cardiovascular surgery: a systematic review. J Card Surg. 2013;28:238-247. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Rafijah G, Bowen AJ, Dolores C, Vitali R, Mozaffar T, Gupta R. The effects of adjuvant fibrin sealant on the surgical repair of segmental nerve defects in an animal model. J Hand Surg Am. 2013;38:847-855. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Martinez-de-la-Casa JM, Rayward O, Saenz-Frances F, Mendez C, Bueso ES, Garcia-Feijoo J. Use of a fibrin adhesive for conjunctival closure in trabeculectomy. Acta Ophthalmol. 2013;91:425-428. [PubMed] [Cited in This Article: ] |
| 10. | Sanjay P, Watt DG, Wigmore SJ. Systematic review and meta-analysis of haemostatic and biliostatic efficacy of fibrin sealants in elective liver surgery. J Gastrointest Surg. 2013;17:829-836. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Ding H, Yuan JQ, Zhou JH, Zheng XY, Ye P, Mao C, Chen Q. Systematic review and meta-analysis of application of fibrin sealant after liver resection. Curr Med Res Opin. 2013;29:387-394. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Maralcan G, Başkonuş I, Aybasti N, Gökalp A. The use of fibrin glue in the treatment of fistula-in-ano: a prospective study. Surg Today. 2006;36:166-170. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 39] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Kim KH, Jang BI, Kim TN. A common bile duct stone formed by suture material after open cholecystectomy. Korean J Intern Med. 2007;22:279-282. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Dolay K, Alis H, Soylu A, Altaca G, Aygun E. Migrated endoclip and stone formation after cholecystectomy: a new danger of acute pancreatitis. World J Gastroenterol. 2007;13:6446-6448. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 19] [Cited by in F6Publishing: 21] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 15. | Liang B, Huang XQ, Wang J, Xia HT, Liu B, Xiang X, Dong JH, Huang ZQ. Choledochoplasty for major bile duct diedct in Mirizzi syndrome. Zhonghua Gandan Waike Zazhi. 2012;18:743-746. [Cited in This Article: ] |
| 16. | Yang YC, Kang X, Yang SH, Feng TX. Repair of defect/necrosis of bile duct wall by anto-tissue patches. Zhonghua Gandan Waike Zazhi. 2007;13:233-234. [Cited in This Article: ] |
| 17. | Wu JS, Peng C, Yin XM, Cheng W. The use of liver round ligament in the hepatobiliary surgery. Gandanyi Waike Zazhi. 2008;20:371-372. [Cited in This Article: ] |
| 18. | Wan ZS, Xiong D, Liu R. The use of liver round ligament in extrahepatic bile ducts deletion. Xiandai Zhongxiyi Jiehe Zazhi. 2014;23:728-729. [Cited in This Article: ] |
| 19. | Boonstra EA, Molenaar IQ, Porte RJ, de Boer MT. Topical haemostatic agents in liver surgery: do we need them? HPB (Oxford). 2009;11:306-310. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |