Published online Jan 14, 2015. doi: 10.3748/wjg.v21.i2.432
Peer-review started: July 27, 2014
First decision: August 15, 2014
Revised: September 4, 2014
Accepted: October 21, 2014
Article in press: October 21, 2014
Published online: January 14, 2015
Foregut cystic developmental malformation (FCDM) is a very rare lesion of the alimentary tract, especially in the stomach. We discuss the concepts of gastric duplication cyst, bronchogenic cysts, and FCDM. Nomenclature has been inconsistent and confusing, but, by some definitions, gastric duplication cysts involve gastric mucosa and submucosal glands, bronchogenic cysts involve respiratory mucosa with underlying cartilage and glands, and FCDM lacks gastric mucosa or underlying glands or cartilage but has pseudostratified ciliated columnar epithelium (PCCE). We searched our departmental case files from the past 15 years and identified 12 cases of FCDM in the alimentary tract. We summarize the features of these 12 cases including a report in detail on a 52-year-old man with a submucosal cyst lined with simple PCCE and irregular and stratified circular muscle layers that merged with gastric smooth muscle bundles near the lesser curvature of the gastric cardia. A literature review of cases with this histology yielded 25 cases. We propose the term gastric-FCDM for such cases. Our own series of 12 cases confirms that preoperative recognition of the entity is infrequent and problematic. The rarity of this developmental disorder, as well as a lack of understanding of its embryologic origins, may contribute to missing the diagnosis. Not appreciating the diagnosis preoperatively can lead to an inappropriate surgical approach. In contrast, presurgical recognition of the entity will contribute to a good outcome and reduced risk of complications.
Core tip: Gastric foregut cystic developmental malformation is a rare lesion that has been reported intermittently in recent decades. Its classification was inconsistent. It has often been misdiagnosed preoperatively. By missing the nature of the diagnosis, the surgical management was quite different. Through a review of the case series and literature concerning their clinical and radiologic features, and recognition of its embryologic and histological origin, we found that it is not an irregular disease and is an easily missed diagnosis. It can be cured by rational surgery, contributing to a good outcome and reduced risk of complications.
- Citation: Geng YH, Wang CX, Li JT, Chen QY, Li XZ, Pan H. Gastric foregut cystic developmental malformation: Case series and literature review. World J Gastroenterol 2015; 21(2): 432-438
- URL: https://www.wjgnet.com/1007-9327/full/v21/i2/432.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i2.432
Gastric foregut cystic developmental malformation (G-FCDM) is a rare lesion and is composed of an intramural cyst in the stomach with a lining of pseudostratified ciliated columnar epithelium (PCCE). Cysts of this nature have been reported for several decades and were given various names including duplication cyst of the stomach with ciliated lining[1-4], bronchogenic cyst of the stomach[5-12], and foregut duplication cyst of the stomach[13-21]. Preoperatively, a misdiagnosis as gastrointestinal stromal tumor (GIST) and leiomyoma was not unusual[2,8,9,11,12,15]. With the aforementioned shared histopathologic characteristics and clinicoradiologic features that mimic GIST, are cysts with PCCE truly a form of gastric duplication cyst[4]? Recent reanalysis has led to the conclusion that a cystic developmental malformation of the primitive foregut vestiges may be a reasonable embryologic explanation for the entity[14,22,23]. In this paper, we review the features of the aforementioned gastric cysts and review those that only have PCCE, along with a series of secondary changes arising in the developmental process of the cyst, which could help with choosing the appropriate surgical procedure[24].
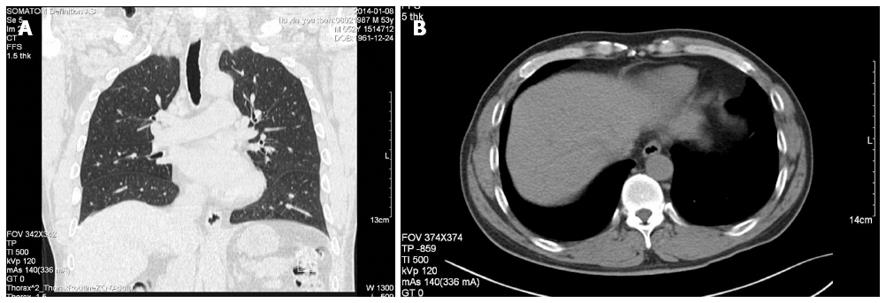
One month prior to admission, a 52-year-old man had epigastric discomfort and noted a mass. As he did not have chills, fever, nausea, vomiting, or diarrhea, he did not attach importance to it initially. However, his symptoms persisted, prompting him to seek medical attention. Endoscopy of the upper gastrointestinal tract revealed a gastric submucosal eminence at the subphrenic gastroesophageal junction. Pathologic diagnosis was chronic nonatrophic gastritis. Abdominal frontal and transversal computed tomography (CT) showed a well-circumscribed, homogeneous, non-enhancing, low-density, submucosal cystic mass measuring 3.0 cm × 4.2 cm on the lesser curvature of the stomach near the cardia, with a CT number of 17 Hu (Figure 1). Preliminary suspicion was of a GIST with cystic change. On physical examination, he was in good condition and laboratory studies were within the normal range. He had an exploratory laparotomy under general anesthesia. Intraoperatively, the liver, peritoneum, and pelvis were free of metastatic disease, and no ascites was detected. A soft 4.0 cm × 3.0 cm mass was noted at the lesser curvature, near the cardia. He underwent proximal gastrectomy with lymph node dissection. The postoperative course was uneventful and there was no recurrence after 5 mo.
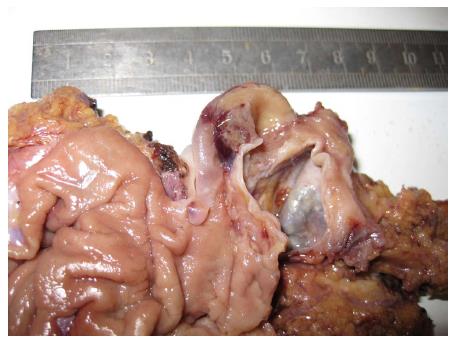
Gross examination of the proximal stomach showed that the cystic lesion was embedded in the gastric muscular layer and intimately associated with the submucosal lesser curvature near the cardia. It was located towards the esophageal margin of the proximal gastrectomy specimen (Figure 2). Thick, pale-yellow liquid was present within the cyst. The cyst did not communicate with the gastric lumen and measured 6.5 cm × 5 cm × 5 cm with a wall thickness that ranged from 0.1 to 0.3 cm.
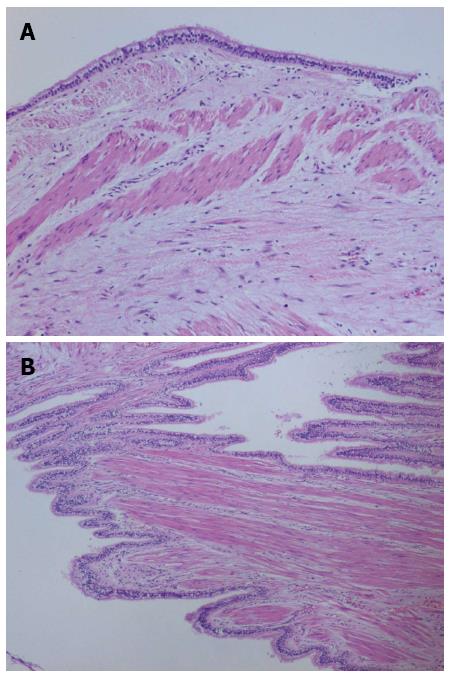
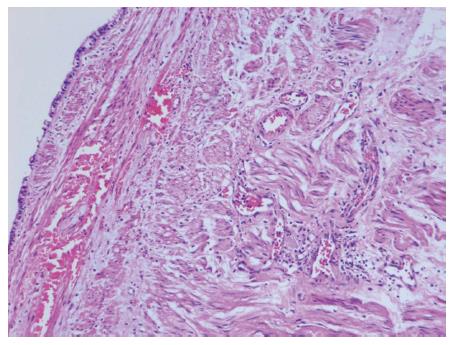
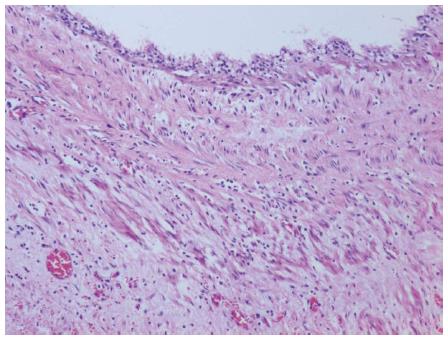
The cyst wall was lined by a simple columnar epithelium and had a criss-crossing and stratified circular muscle layer (Figure 3A), and part of the cystic wall was lined with irregular longitudinal muscle bundles (Figure 3B). This circular muscle was stratified and merged with the muscular wall of the stomach at the attachment site, and the myenteric plexus was seen (Figure 4). Cartilaginous tissue, seromucinous glands, gastric epithelium and submucosal glands were not identified. Squamous metaplasia of the PCCE was detected (Figure 5). Cholesterol crystals and a histocytic response were present. All the dissected systematic lymph nodes were negative.
G-FCDM may represent a congenital anomaly with late differentiation rather than imperfect involution of embryonic vestiges, but the undifferentiated foregut vestiges undergo transition and differentiate during the embryonic period[20]. One model postulates that the primitive lung bud derives from the respiratory laryngotracheal tube of the ventral foregut but is incompletely separated from the dorsal foregut in week seven of fetal development[24]. Several hypotheses to explain the dissociated foregut malformations suggest that they probably arise from pinching off and form the budding remnants[25], migration of the aberrant rest, supernumerary lung buds, and incomplete involution of the connecting stalk or fistula that connects with the digestive or respiratory tract[26-28].
Some authors would classify our described case as gastric bronchogenic cyst. Bronchogenic cysts are thought to be in the spectrum of foregut cystic malformations. Traditional embryology theory postulates that the basic difference between the two entities is the timing of budding. Foregut cysts are derived from pinching off at the time of bronchiolar differentiation, which is later than that of bronchogenic cysts; hence, the presence of cartilage and glandular tissue in the wall of the bronchogenic cyst[29]. Histologically, the foregut cysts are lined with PCCE, subepithelial connective tissue followed by a smooth muscle layer and an outer fibrous layer[29,30], but bronchogenic cysts additionally contain cartilage and glandular tissues in the cyst wall[16,23].
Gastrointestinal duplication cysts are rare congenital malformations that may occur anywhere from the mouth to the anus[31-33]. Cunningham et al[19] have suggested that the term gastric duplication implies the presence of gastric epithelium. Ladd and Grossa[34], later supported by Parker et al[35], have proposed more detailed criteria: close proximity to the gastrointestinal tract; a lining that resembles some part of the gastrointestinal tract; and a smooth muscle layer that shares the muscle wall with the gut, or is intermingled with the muscular layer of the bowel. Abiding by these criteria, cysts lined with PCCE do not qualify as gastrointestinal duplication cysts, including our 12 cases, because they lack archenteric epithelium. Similarly, in our cases, neither cartilaginous tissue nor seromucinous glands were present, so they do not qualify as bronchogenic cysts. In the literature, most reported cysts lined with PCCE are often described as foregut duplication cysts of the stomach[19].
Our literature search gathered 24 reports including 25 cases listed in Table 1[1-22,36]. From the literature review, gastric foregut cyst lined simply by PCCE is a delayed-onset disease (14 women and 11 men from 25 to 76 years-old). Our own series of patients in Table 2 also consisted of adults (age: 32-83 years) and had an equal sex distribution (6 women and 6 men). Most of the previously reported lesions involved the lesser curvature of the stomach and were near the gastroesophageal junction or cardia (12/24; 50%). Our series had a slight predominance of esophageal lesions (5/12; 42%), which was consistent with the literature reports of lesions above the diaphragm involving the esophagus[2,16]. Whether the predilection site of esophagus is related with the closest adjacency between the ventral embryo vestiges and dorsal tubes remains unknown. It is usually asymptomatic and occasionally found as a gastric wall mass on physical examination. Some patients present with epigastric pain. Patients with an older age or with a longer clinical history of symptoms tend to present with a larger mass and are more likely to have epigastric discomfort, gastric ulcer, gastroesophageal reflux, or occasionally canceration[37,38]. Some of these signs and symptoms are presumably related to the effect of the mass on adjacent structures[20]. Morphologically, the lined epithelium with focal squamous metaplasia were also sporadically reported[4,22]. As a result of the cyst location within the gastric muscular layer and a lack of communication with the gastric lumen, many such lesions are preoperatively misdiagnosed as intramural GIST and leiomyoma, which present with different imaging findings, although they probably share similar clinical representation. It has been proposed that all foregut developmental anomalies, including gastric duplication cyst with PCCE lining and bronchogenic cyst without cartilage and glandular tissue, should be grouped under the heading of foregut cystic malformations because they all share a common origin from the foregut and differ from each other in migration, location, and degree of differentiation[23,27,28,39]. Gastric cysts with PCCE are not true duplication cysts of the foregut, but the cystic development of foregut embryologic vestiges. Therefore, we suggest designating this as G-FCDM. With regard to the predominant location of G-FCDM at the lesser curvature of the stomach, it remains to be established whether this is due to migration of the embryo vestiges or some other reason.
| No. | Sex | Age (yr) | Complaints | Location | Size (cm) | Ref. |
| 1 | M | 56 | No | NGEJ, AW | 5 × 3 × 3 | Napolitano et al[13], 2013 |
| 2 | F | 34 | EP, GR | NGEJ, GC | 4.5 × 3.2 | Montemurro et al[1], 2011 |
| 3 | M | 29 | AP | Fundus GC | 8.5 × 5.5 × 4.8 | Khoury et al[14], 2011 |
| F | 26 | EP | Middle body LC | 5 × 2.2 × 2 | ||
| 4 | M | 76 | No | NGEJ, LC | 4 × 4 | Jiang et al[2], 2011 |
| 5 | M | 42 | Left lumbar pain | AGIJ, LC | 4.5 × 5.2 | Mardi et al[15], 2010 |
| 6 | F | 25 | EP | Gastric fundus | 3 × 2.5 × 2 | Jiang et al[5], 2010 |
| 7 | F | 60 | No | Cardia, LC | 3 | Sato et al[6], 2008 |
| 8 | F | 72 | No | Middle body, LC | 2 × 1.5 | Murakami et al[16], 2008 |
| 9 | M | 37 | EP | NGEJ, LC | 4 × 4 | Wakabayashi et al[7], 2007 |
| 10 | M | 40 | ED | NGEJ, LC | 6 × 5 | Hall et al[17], 2007 |
| 11 | F | 46 | Vomiting | PW of fundus; | 8 × 5.5 | Theodosopoulos et al[18], 2007 |
| Gastrosplenic ligament | 3 × 3 | |||||
| 12 | F | 38 | No | Cardia, LC | 7 × 5 | Lee et al[8], 2006 |
| 13 | F | 63 | Fever, AP | PW of fundus | 10 × 7.6 | Cunningham et al[19], 2006 |
| 14 | F | 39 | No | Fundus | 4 × 2.5 × 1 | Melo et al[9], 2005 |
| 15 | M | 26 | EP | NA | NA | Rubio et al[10], 2005 |
| 16 | F | 62 | No | NGEJ, LC | 3.5 × 2.5 × 1.5 | Song et al[11], 2005 |
| 17 | F | 59 | No | PW of stomach, LC | 7 × 5 | Hedayati et al[12], 2003 |
| 18 | M | 35 | EP | NGEJ, LC | 7 × 6 × 5 | Kim et al[20], 2000 |
| 19 | M | 34 | No | GC | large | Ikehata et al[3], 2000 |
| 20 | M | 25 | No | PW of fundus | 6.5 × 5 × 5 | Takahara et al[4], 1996 |
| 21 | F | 35 | EP, nausea | PW | 5.5 × 2.5 × 2 | Laraja et al[21], 1995 |
| 22 | F | 61 | Heart failure | Cardia, intramural | 2 × 1.5 | Shireman[36], 1987 |
| 23 | F | 46 | No | NGEJ, GC | 6 × 8 | Gensler et al[22], 1966 |
| 24 | M | 52 | ED | LC, NGEJ | 6.5 × 5 | Present case |
| No. | Sex | Age (yr) | Complaints | Location | Size (cm) | Surgical option |
| 1 | F | 35 | CT | Esophagus | 2.5 × 1.5 × 1 | CE |
| 2 | M | 51 | ED | Lower esophagus | 3 × 2 | CE |
| 3 | F | 44 | No | PT, lesser omental sac | 8 × 3 × 2 | CE |
| 4 | M | 76 | No | NGEJ, LC | 4 × 4 | Total gastrectomy with SLND |
| 5 | F | 54 | ED | Lower esophagus | 4 × 2.5 × 2 | CE |
| 6 | M | 40 | NA | Biliary tract | 3 × 2.5 | CE |
| 7 | F | 42 | CT | Esophagus | 4 × 2.5 × 1 | CE |
| 8 | F | 32 | No | PT, gastrosplenic ligament | 5 × 4 × 3 | CE |
| 9 | M | 41 | No | PW, LC | 3.5 × 2.5 × 0.8 | CE |
| 10 | F | 42 | NA | Esophagus | 2.5 × 1.8 | CE |
| 11 | M | 83 | NA | Distal ileum | 6.7 × 5 × 4.1 | CE |
| Present | M | 52 | ED | LC, NGEJ | 6.5 × 5 | Proximal partial gastrectomy with SLND |
In symptomatic and occasionally discovered G-FCDM, CT can detect the presence of the abdominal mass, but it frequently fails to recognize its cystic nature due to the thick cyst wall[8]. Despite the fact that GIST is clinically more common than G-FCDM, it does not often show necrosis and cystic change. In the imaging study, cystic changes in GIST tend to be focal with irregular internal surfaces rather than smooth as in congenital cysts, and usually do not involve the whole tumor. Moreover, the proteinaceous cyst fluid[16,40] of G-FCDM is very helpful in identifying the necrosis of GIST. G-FCDM, but not GIST, can alter their shape with changing posture when they are large enough and with low tension. Leiomyoma is similar. Endoscopic ultrasound (EUS) is helpful in identifying the intramural or extramural relation of the gastrointestinal tract[41-45]. CT[46,47], magnetic resonance imaging or ultrasonography could indicates the presence of an abdominal cystic lesion or mass incidentally, but it cannot identify the nature of the lesion[2,21,40,48,49]. EUS-guided fine-needle aspiration (EUS-FNA)[50], CT-guided needle biopsy and intraoperative frozen section diagnosis can provide histologic diagnosis of G-FCDM and guide operative plans. The presence of PCCE and absence of neoplastic cells confirm the nature of the cyst[43], but considering the complications, some people do not advise performing a biopsy to confirm the diagnosis of resectable GIST because it can lead to tumor dissemination or hemorrhage[51,52].
The management of asymptomatic cases remains controversial[41]. Watchful waiting is suggested after confirming the benign nature of these cysts by EUS-FNA, and Ponder and Collins[19] concluded that surgery is not necessary if the respiratory-type epithelial cells are diagnosed on EUS-FNA. For single symptomatic cases, the recommended management is complete cyst excision without violation of the gastric lumen[53]. Segmental or total gastrectomy is only a secondary alternative in the case of an indefinite diagnosis before operations[54]. However, if the cyst communicates with the gastric lumen that can easily induce infection, or with other serious gastric mucosal complications, such as ulceration, perforation, bleeding[55], fistula formation[38], obstruction and even malignant change, although rare, partial gastrectomy may be required[2,5,16]. From Table 2, we can see surgical treatment typically involved excision of the lesion without injury to attached organs, except the stomach. Of our three cases of G-FCDM, only one was correctly identified preoperatively and the cyst was successfully removed laparoscopically. The other two cases were incorrectly treated as GISTs, which are more common than congenital cysts, and led to unnecessary segmental gastrectomy and systematic lymph node dissection. With advances in medical technology and further understanding of G-FCDM, the advisable laparoscopic surgery for cyst removal has become more common in recent studies[16,24].
In summary, G-FCDM lined by PCCE is a rare lesion derived from foregut developmental malformation. The clinical manifestation is usually nonspecific, and it is easily misdiagnosed radiologically and clinically as a GIST or leiomyoma. EUS-FNA/CT-guided needle biopsy and frozen section diagnosis could be helpful in identifying the nature of the cyst and guide the surgical options. Although rare, better understanding of the origins of G-FCDM lined by PCCE and taking precise auxiliary examinations could help differential diagnosis from gastric wall masses, and surgically cure them without overtreatment.
P- Reviewer: Narattaphol C, Takayuki M, Uwe K S- Editor: Yu J L- Editor: AmEditor E- Editor: Ma S
| 1. | Montemurro S, Cartanese C, De Luca R, Zito FA, Ranieri G, Ruggieri E. Duplication cyst of the stomach with respiratory epithelium in adult: an uncommon finding. Report of case and review of literature. Ann Ital Chir. 2011;82:487-491. [PubMed] [Cited in This Article: ] |
| 2. | Jiang W, Zhang B, Fu YB, Wang JW, Gao SL, Zhang SZ, Wu YL. Gastric duplication cyst lined by pseudostratified columnar ciliated epithelium: a case report and literature review. J Zhejiang Univ Sci B. 2011;12:28-31. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Ikehata A, Sakuma T. Gastric duplication cyst with markedly elevated concentration of carbohydrate antigen 19-9. Am J Gastroenterol. 2000;95:842-843. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 4. | Takahara T, Torigoe T, Haga H, Yoshida H, Takeshima S, Sano S, Ishii Y, Furuya T, Nakamura E, Ishikawa M. Gastric duplication cyst: evaluation by endoscopic ultrasonography and magnetic resonance imaging. J Gastroenterol. 1996;31:420-424. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Jiang L, Jiang L, Cheng N, Yan L. Bronchogenic cyst of the gastric fundus in a young woman. Dig Liver Dis. 2010;42:826. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Sato M, Irisawa A, Bhutani MS, Schnadig V, Takagi T, Shibukawa G, Wakatsuki T, Imamura H, Takahashi Y, Sato A. Gastric bronchogenic cyst diagnosed by endosonographically guided fine needle aspiration biopsy. J Clin Ultrasound. 2008;36:237-239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Wakabayashi H, Okano K, Yamamoto N, Suzuki Y, Inoue H, Kadota K, Haba R. Laparoscopically resected foregut duplication cyst (bronchogenic) of the stomach. Dig Dis Sci. 2007;52:1767-1770. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Lee SH, Park DH, Park JH, Kim HS, Park SH, Kim SJ, Oh MH. Endoscopic mucosal resection of a gastric bronchogenic cyst that was mimicking a solid tumor. Endoscopy. 2006;38 Suppl 2:E12-E13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Melo N, Pitman MB, Rattner DW. Bronchogenic cyst of the gastric fundus presenting as a gastrointestinal stromal tumor. J Laparoendosc Adv Surg Tech A. 2005;15:163-165. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Rubio CA, Orrego A, Willén R. Congenital bronchogenic cyst in the gastric mucosa. J Clin Pathol. 2005;58:335. [PubMed] [Cited in This Article: ] |
| 11. | Song SY, Noh JH, Lee SJ, Son HJ. Bronchogenic cyst of the stomach masquerading as benign stromal tumor. Pathol Int. 2005;55:87-91. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Hedayati N, Cai DX, McHenry CR. Subdiaphragmatic bronchogenic cyst masquerading as an “adrenal incidentaloma”. J Gastrointest Surg. 2003;7:802-804. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 13. | Napolitano V, Pezzullo AM, Zeppa P, Schettino P, D’Armiento M, Palazzo A, Della Pietra C, Napolitano S, Conzo G. Foregut duplication of the stomach diagnosed by endoscopic ultrasound guided fine-needle aspiration cytology: case report and literature review. World J Surg Oncol. 2013;11:33. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Khoury T, Rivera L. Foregut duplication cysts: a report of two cases with emphasis on embryogenesis. World J Gastroenterol. 2011;17:130-134. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 26] [Cited by in F6Publishing: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Mardi K, Kaushal V, Gupta S. Foregut duplication cysts of stomach masquerading as leiomyoma. Indian J Pathol Microbiol. 2010;53:829-830. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Murakami S, Isozaki H, Shou T, Sakai K, Toyota H. Foregut duplication cyst of the stomach with pseudostratified columnar ciliated epithelium. Pathol Int. 2008;58:187-190. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Hall DA, Pu RT, Pang Y. Diagnosis of foregut and tailgut cysts by endosonographically guided fine-needle aspiration. Diagn Cytopathol. 2007;35:43-46. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Theodosopoulos T, Marinis A, Karapanos K, Vassilikostas G, Dafnios N, Samanides L, Carvounis E. Foregut duplication cysts of the stomach with respiratory epithelium. World J Gastroenterol. 2007;13:1279-1281. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 26] [Cited by in F6Publishing: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Cunningham SC, Hansel DE, Fishman EK, Cameron JL. Foregut duplication cyst of the stomach. J Gastrointest Surg. 2006;10:620-621. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Kim DH, Kim JS, Nam ES, Shin HS. Foregut duplication cyst of the stomach. Pathol Int. 2000;50:142-145. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 51] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Laraja RD, Rothenberg RE, Chapman J, Imran-ul-Haq MT. Foregut duplication cyst: a report of a case. Am Surg. 1995;61:840-841. [PubMed] [Cited in This Article: ] |
| 22. | Gensler S, Seidenberg B, Rifkin H, Rubinstein BM. Ciliated lined intramural cyst of the stomach: case report and suggested embryogenesis. Ann Surg. 1966;163:954-956. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 38] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Sharma S, Nezakatgoo N, Sreenivasan P, Vanatta J, Jabbour N. Foregut cystic developmental malformation: new taxonomy and classification--unifying embryopathological concepts. Indian J Pathol Microbiol. 2009;52:461-472. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Gray SW, Skandalakis JE. Embryology for Surgeons. Philadelphia: W.B. Saunders Company 1972; 217-383. [Cited in This Article: ] |
| 25. | Hall NJ, Ade-Ajayi N, Peebles D, Pierro A. Antenatally diagnosed duplication cyst of the tongue: modern imaging modalities assist perinatal management. Pediatr Surg Int. 2005;21:289-291. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Horne G, Ming-Lum C, Kirkpatrick AW, Parker RL. High-grade neuroendocrine carcinoma arising in a gastric duplication cyst: a case report with literature review. Int J Surg Pathol. 2007;15:187-191. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 34] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 27. | Kim KW, Kim WS, Cheon JE, Lee HJ, Kim CJ, Kim IO, Yeon KM. Complex bronchopulmonary foregut malformation: extralobar pulmonary sequestration associated with a duplication cyst of mixed bronchogenic and oesophageal type. Pediatr Radiol. 2001;31:265-268. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 32] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Eom DW, Kang GH, Kim JW, Ryu DS. Unusual bronchopulmonary foregut malformation associated with pericardial defect: bronchogenic cyst communicating with tubular esophageal duplication. J Korean Med Sci. 2007;22:564-567. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Chatelain D, Chailley-Heu B, Terris B, Molas G, Le Caë A, Vilgrain V, Belghiti J, Degott C, Flejou JF. The ciliated hepatic foregut cyst, an unusual bronchiolar foregut malformation: a histological, histochemical, and immunohistochemical study of 7 cases. Hum Pathol. 2000;31:241-246. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 55] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 30. | Horii T, Ohta M, Mori T, Sakai M, Hori N, Yamaguchi K, Fujino H, Oishi T, Inada Y, Nakamura K. Ciliated hepatic foregut cyst. A report of one case and a review of the literature. Hepatol Res. 2003;26:243-248. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 31. | Bower RJ, Sieber WK, Kiesewetter WB. Alimentary tract duplications in children. Ann Surg. 1978;188:669-674. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 157] [Cited by in F6Publishing: 141] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 32. | O’Donnell PL, Morrow JB, Fitzgerald TL. Adult gastric duplication cysts: a case report and review of literature. Am Surg. 2005;71:522-525. [PubMed] [Cited in This Article: ] |
| 33. | Ohbayashi Y, Miyake M, Nagahata S. Gastrointestinal cyst of the tongue: a possible duplication cyst of foregut origin. J Oral Maxillofac Surg. 1997;55:626-628; discussion 629-630. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 34. | Miller RF, Graub M, Pashuck ET. Bronchogenic cysts; anomalies resulting from maldevelopment of the primitive foregut and midgut. Am J Roentgenol Radium Ther Nucl Med. 1953;70:771-785. [PubMed] [Cited in This Article: ] |
| 35. | Parker BC, Guthrie J, France NE, Atwell JD. Gastric duplications in infancy. J Pediatr Surg. 1972;7:294-298. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 36. | Shireman PK. Intramural cyst of the stomach. Hum Pathol. 1987;18:857-858. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 37. | Kuraoka K, Nakayama H, Kagawa T, Ichikawa T, Yasui W. Adenocarcinoma arising from a gastric duplication cyst with invasion to the stomach: a case report with literature review. J Clin Pathol. 2004;57:428-431. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 97] [Cited by in F6Publishing: 102] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 38. | Whiddon DR, Olutoye OO, Broderick TJ, Mills AS, Turner MA, Zfass AM, Sugerman HJ. Recurrent acute pancreatitis caused by a gastric duplication communicating with an aberrant pancreas. Am Surg. 1999;65:121-124. [PubMed] [Cited in This Article: ] |
| 39. | Matsubayashi J, Ishida T, Ozawa T, Aoki T, Koyanagi Y, Mukai K. Subphrenic bronchopulmonary foregut malformation with pulmonary-sequestration-like features. Pathol Int. 2003;53:313-316. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 40. | Johnston J, Wheatley GH, El Sayed HF, Marsh WB, Ellison EC, Bloomston M. Gastric duplication cysts expressing carcinoembryonic antigen mimicking cystic pancreatic neoplasms in two adults. Am Surg. 2008;74:91-94. [PubMed] [Cited in This Article: ] |
| 41. | Eloubeidi MA, Cohn M, Cerfolio RJ, Chhieng DC, Jhala N, Jhala D, Eltoum IA. Endoscopic ultrasound-guided fine-needle aspiration in the diagnosis of foregut duplication cysts: the value of demonstrating detached ciliary tufts in cyst fluid. Cancer. 2004;102:253-258. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 55] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 42. | Wang B, Hunter WJ, Bin-Sagheer S, Bewtra C. Rare potential pitfall in endoscopic ultrasound-guided fine needle aspiration biopsy in gastric duplication cyst: a case report. Acta Cytol. 2009;53:219-222. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 43. | Fazel A, Moezardalan K, Varadarajulu S, Draganov P, Eloubeidi MA. The utility and the safety of EUS-guided FNA in the evaluation of duplication cysts. Gastrointest Endosc. 2005;62:575-580. [PubMed] [Cited in This Article: ] |
| 44. | Sakamoto H, Kitano M, Matsui S, Kamata K, Komaki T, Imai H, Dote K, Kudo M. Estimation of malignant potential of GI stromal tumors by contrast-enhanced harmonic EUS (with videos). Gastrointest Endosc. 2011;73:227-237. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 80] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 45. | Xia Y, Kitano M, Kudo M, Imai H, Kamata K, Sakamoto H, Komaki T. Characterization of intra-abdominal lesions of undetermined origin by contrast-enhanced harmonic EUS (with videos). Gastrointest Endosc. 2010;72:637-642. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 46. | Kuhlman JE, Fishman EK, Wang KP, Siegelman SS. Esophageal duplication cyst: CT and transesophageal needle aspiration. AJR Am J Roentgenol. 1985;145:531-532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 47] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 47. | Adam A, MacSweeney JE, Whyte MK, Smith PL, Ind PW. CT-guided extrapleural drainage of bronchogenic cyst. J Comput Assist Tomogr. 1989;13:1065-1068. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 48. | Hirooka Y, Itoh A, Kawashima H, Ohno E, Itoh Y, Nakamura Y, Hiramatsu T, Sugimoto H, Sumi H, Hayashi D. Contrast-enhanced endoscopic ultrasonography in digestive diseases. J Gastroenterol. 2012;47:1063-1072. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 49. | Giovannini M. The place of endoscopic ultrasound in bilio-pancreatic pathology. Gastroenterol Clin Biol. 2010;34:436-445. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 50. | Bhatia V, Garg PK, Gupta SD, Dash NR, Saluja SS, Madan K. Demonstration of peristalsis in gastric duplication cyst by EUS: implications for diagnosis and symptomatology (with videos). Gastrointest Endosc. 2008;68:183-185. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 51. | Chaudhry UI, DeMatteo RP. Management of resectable gastrointestinal stromal tumor. Hematol Oncol Clin North Am. 2009;23:79-96, viii. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 52. | Ryan AG, Zamvar V, Roberts SA. Iatrogenic candidal infection of a mediastinal foregut cyst following endoscopic ultrasound-guided fine-needle aspiration. Endoscopy. 2002;34:838-839. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 47] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 53. | Faigel DO, Burke A, Ginsberg GG, Stotland BR, Kadish SL, Kochman ML. The role of endoscopic ultrasound in the evaluation and management of foregut duplications. Gastrointest Endosc. 1997;45:99-103. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 48] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 54. | Holcomb GW, Gheissari A, O’Neill JA, Shorter NA, Bishop HC. Surgical management of alimentary tract duplications. Ann Surg. 1989;209:167-174. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 218] [Cited by in F6Publishing: 243] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 55. | Klimopoulos S, Gialvalis D, Marougas M, Zotos D, Orfanos N, Roussakis A, Argyriou P, Pantelidaki C. Unusual case of massive hemorrhage of a gastric duplication cyst in a very advanced age. Langenbecks Arch Surg. 2009;394:745-747. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |