Published online Apr 28, 2015. doi: 10.3748/wjg.v21.i16.5023
Peer-review started: October 21, 2014
First decision: November 14, 2014
Revised: December 9, 2014
Accepted: February 12, 2015
Article in press: February 13, 2015
Published online: April 28, 2015
AIM: To evaluate the efficacy of adding irsogladine maleate (IM) to proton-pump inhibitor (PPI) therapy in non-erosive reflux disease (NERD) treatment.
METHODS: One hundred patients with NERD were recruited and randomized to receive rabeprazole plus IM (group I) or rabeprazole plus placebo (group P). The efficacy of the treatment was assessed using the Frequency Scale for the Symptoms of Gastroesophageal Reflux Disease (FSSG) and the short form (SF)-36 quality of life questionnaires after four weeks of treatment. We also assessed whether patients with NERD with minimal changes (grade M) had different responses to the therapies compared with patients who did not have minimal changes (grade N).
RESULTS: Group I and group P showed significant improvements in their FSSG scores after the treatment (from 17.9 ± 7.9 to 9.0 ± 7.6, and from 17.7 ± 7.3 to 11.2 ± 7.9, respectively, P = 0.0001), but there was no statistically significant difference between the FSSG scores in group I and those in group P. Subgroup analysis showed that significant improvements in the FSSG scores occurred in the patients in group I who had NERD grade N (modified Los Angeles classification) (7.8 ± 7.4 vs 12.5 ± 9.8, P = 0.041). The SF-36 scores for patients with NERD grade N who had received IM and rabeprazole were significantly improved in relation to their vitality and mental health scores.
CONCLUSION: The addition of IM to rabeprazole significantly improves gastroesophageal reflux disease symptoms and the quality of the lives of patients with NERD grade N.
Core tip: Proton pump inhibitor (PPI) therapy is considered the mainstay for the treatment of non-erosive reflux disease (NERD). However, it is less effective in NERD than it is in reflux esophagitis. This study evaluated the efficacy of adding irsogladine maleate (IM) to PPI therapy in the treatment of NERD. Adding IM to rabeprazole improved both the gastroesophageal reflux disease symptoms and the quality of the lives of patients with NERD showing no endoscopic abnormalities, a categorization that was based on the modified Los Angeles classification.
- Citation: Suzuki T, Matsushima M, Masui A, Tsuda S, Imai J, Nakamura J, Tsukune Y, Uchida T, Yuhara H, Igarashi M, Koike J, Mine T. Irsogladine maleate and rabeprazole in non-erosive reflux disease: A double-blind, placebo-controlled study. World J Gastroenterol 2015; 21(16): 5023-5031
- URL: https://www.wjgnet.com/1007-9327/full/v21/i16/5023.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i16.5023
Gastroesophageal reflux disease (GERD) is a chronic disorder characterized by unpleasant reflux symptoms that include heartburn, sore throat, belching, nausea, voice changes, chest pain, cough, and acid regurgitation[1]. GERD includes both reflux esophagitis (RE) and non-erosive reflux disease (NERD). According to the Montreal consensus conference[2], RE is characterized by mucosal damage within the esophagus that can be visualized during endoscopy, whereas mucosal breaks are not seen in NERD. Endoscopic examinations indicate that about two-thirds of patients with GERD symptoms have no erosive changes[3]. The detailed endoscopic findings from patients with NERD can be divided into two groups that can be defined using a modification of the Los Angeles classification, with one group showing no endoscopic abnormalities (grade N), and the other group showing minimal endoscopic changes, for example, whitish or reddish edematous changes (grade M)[4]. However, little is known about clinical utility of endoscopic classification in NERD.
Most GERD patients are treated with proton pump inhibitors (PPI) to control their symptoms. Reports have suggested that compared with patients with RE, those with NERD had lower response rates to acid suppression therapy, and about half of the patients with NERD did not show adequate improvements in their reflux symptoms when a standard dose of PPI was administered[3,5]. Nevertheless, the initial management of NERD is the same as that of RE, and it comprises PPI mono-therapy.
However, recent studies revealed that these endoscopy-negative patients with reflux symptoms include different pathophysiological mechanisms. On the basis of esophageal 24-h multichannel intraluminal impedance combined with pH measurements, NERD patients can be classified into three groups, as follows: (1) patients with abnormal distal esophageal acid exposure; (2) patients with normal distal esophageal acid exposure and positive symptom associations for either acid and/or non-acid reflux (hypersensitive esophagus); and (3) patients with normal distal esophageal acid exposure and negative symptom associations (functional heartburn)[6,7]. Furthermore, a meta-analysis emphasized that well-defined NERD patients, including those in the aforementioned groups (1) and (2), have responses to PPI therapy that are similar to those seen in patients with RE, and that patients with functional heartburn do not respond to PPI therapy[8]. However, NERD that is diagnosed on the basis of endoscopic findings alone cannot exclude some patients who have functional heartburn.
Although the pathophysiology of NERD remains unclear, electron microscopy and light microscopy have revealed esophageal mucosal dilated intercellular spaces (DIS) in patients with NERD. Exposure to excessive amounts of acid could cause the development of DIS, which correlates well with the symptom of heartburn, and DIS could be useful markers for the breaks in the epithelial barrier that reflect an increase in paracellular permeability[9,10].
Irsogladine maleate (IM) activates gap junctional intercellular communication, and it has been widely used as an anti-ulcer treatment in Japan, Korea, and China; however, little is known about its effects on patients with NERD. This study aimed to evaluate the efficacy of adding IM to PPI therapy in the treatment of patients with NERD in a prospective, randomized, double-blind, placebo-controlled trial.
Patients who presented to Tokai University Hospital from August 2008 to July 2012 with persistent GERD symptoms were enrolled to participate in the study if they did not have mucosal breaks in their esophagi, and if they had Frequency Scale for the Symptoms of GERD (FSSG) scores of ≥ 8. The FSSG is used to diagnose GERD and to determine the efficacy of GERD treatment. The FSSG questionnaire consists of seven questions that relate to reflux (questions 1, 4, 6, 7, 9, 10, 12) and five questions that relate to acid-related dysmotility symptoms (questions 2, 3, 5, 8, 11) that were generated by Kusano et al[11], and it was used in several clinical studies of GERD[11-13].
Patients were excluded from the study if they were younger than 20 years, were allergic to rabeprazole or IM, had any level of esophagitis determined by gastrointestinal endoscopy, were pregnant, were taking atazanavir sulfate, or anti-coagulant, anti-platelet, or pro-kinetic agents, had a history of gastrointestinal malignancy, peptic ulcers, or gastrointestinal tract surgery, or if they had used any PPI therapy within four weeks of enrolling in the study.
After providing written informed consent, the patients were asked to complete a short form (SF)-36 quality of life (QOL) questionnaire. They were randomized by an independent investigator who used a random number generated by a computer to assign the patients to one of two groups, as follows: those who were to receive rabeprazole and IM (group I) and those who were to receive rabeprazole and placebo (group P). At the end of the four-week study period, the patients were asked to complete post-treatment FSSG and SF-36 QOL questionnaires. The FSSG results were considered in terms of the total score and each symptom score. Patients were asked whether they had experienced any adverse events at the end of the study.
The primary endpoint of this study was an improvement in the FSSG score, and determining whether patients with NERD with minimal changes (grade M) had different response to the therapies compared with those without minimal changes (grade N). The study’s secondary endpoints included the SF-36 scores and the occurrence of side effects. The university’s ethics committee approved the study protocol. This study was performed in accordance with the principles laid down in the Declaration of Helsinki. The study was registered in the UMIN Clinical Trials Registry (Registry ID Number: UMIN000015731).
The sample size was estimated based on the statistical analysis of the improvements in the FSSG scores in each group. Previous data have shown that about half of the patients with NERD have adequate improvements in their reflux symptoms when they are treated with a standard PPI dose. In this study, the predicted improvements in the FSSG scores were estimated to be 75% in group I and 50% in group P. As a result, 45 patients were required in each group to detect a significant difference between the groups with an α value of 0.05 and a power (1-β) of 0.8.
We compared the two groups in relation to the proportions of the sexes, smoking habits, the presence of hiatal hernias, alcohol consumption, and the endoscopic grades using the χ2 test. Continuous variables are presented as the means ± SD. Differences in the continuous variables, including age, the FSSG scores, and the body mass indices, were analyzed using the Mann-Whitney U-test. A P value of < 0.05 was considered statistically significant. The SF-36 QOL questionnaire scores were evaluated using the Wilcoxon signed-rank test.
One hundred patients with NERD were randomized to one of the two groups, but three patients were excluded from the study because some of their data were missing. Consequently, 97 patients were included in the analysis. Group I comprised 49 individuals, which included 13 men, and their mean ± SD age was 51.1 ± 16.4 years. Group P comprised 48 individuals, which included 19 men, and their mean ± SD age was 51.1 ± 14.8 years. The baseline characteristics of the patients were comparable (Table 1).
| Group I (n = 49) | Group P (n = 48) | P value | |
| Age (yr), mean ± SD | 51.1 ± 16.4 | 51.1 ± 14.8 | 0.77 |
| Sex, male/female | 13/36 | 19/29 | 0.17 |
| BMI (kg/m2) | 22.4 ± 4.3 | 21.8 ± 3.1 | 0.59 |
| Height (cm) | 159 ± 7.3 | 161.5 ± 8.7 | 0.24 |
| Weight (kg), mean ± SD | 57.1 ± 12.2 | 56.7 ± 8.6 | 0.63 |
| NERD grade (N/M) | 21/28 | 20/28 | 0.91 |
| Hiatal hernia (+/-) | 11/38 | 10/38 | 0.85 |
| Drinking (+/-) | 16/33 | 20/28 | 0.36 |
| Smoking (+/-) | 2/47 | 9/39 | 0.05 |
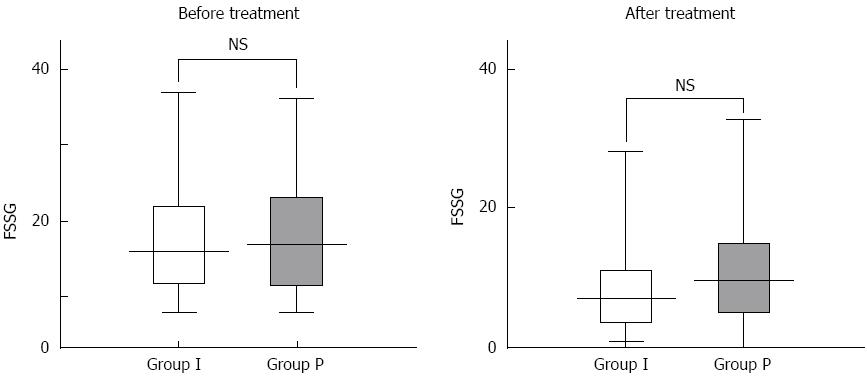
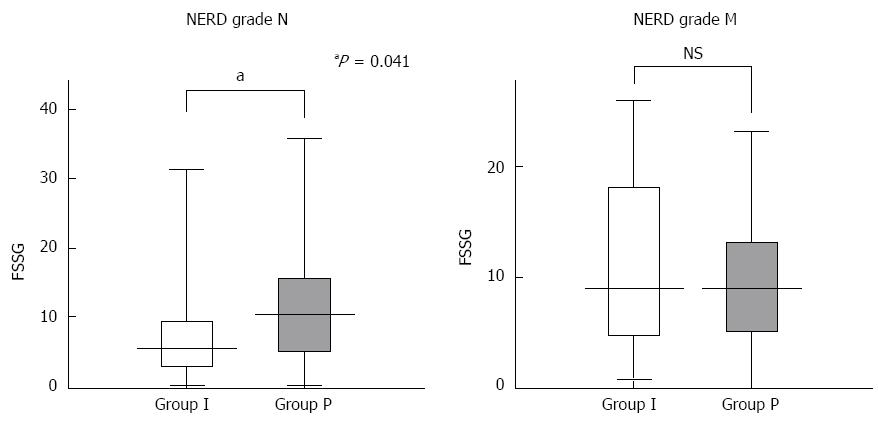
The mean ± SD pre-treatment FSSG scores for group I and group P were 17.9 ± 7.9 and 17.7 ± 7.3 years, respectively. The mean ± SD post-treatment FSSG scores for group I and group P were 9.0 ± 7.6 and 11.2 ± 7.9 years, respectively. Although significant improvements in the FSSG scores were observed within both groups after treatment (P = 0.0001), there was no statistically significant difference between the groups with respect to the FSSG scores after four weeks of treatment (P = 0.15) (Figure 1). Of the seven subscale scores for reflux, the scores for question 10 (Do you get bitter liquid coming up into your throat?) and question 12 (Do you get heartburn if you bend over?) of the FSSG were significantly lower in group I compared with group P. There were no significant differences in the five subscale scores for acid-related dysmotility symptoms between the groups (Figure 2). Next, we assessed whether patients with NERD who had minimal changes (grade M) had different responses to the therapies compared with those without minimal changes (grade N). The clinical characteristics of the patients assigned to the modified Los Angeles classification grades N and M are shown in Table 2. The data indicate that the characteristics associated with NERD grade N were a shorter stature and a lower frequency of esophageal hiatal hernias. Subgroup analysis showed that the FSSG scores for the patients with NERD grade N in group I were significantly lower than the FSSG scores for the patients with NERD grade N in group P after four weeks of treatment (7.8 ± 7.4 vs 12.5 ± 9.8, P = 0.041), but there was no statistically significant difference between the study groups in relation to the FSSG scores for patients with NERD grade M (Figure 3).
| Grade N (n = 56) | Grade M (n = 41) | P value | |
| Age (yr), mean ± SD | 49.8 ± 16.7 | 53.3 ± 13.7 | 0.32 |
| Sex, male/female | 14/42 | 18/23 | 0.05 |
| BMI (kg/m2) | 22.5 ± 4.4 | 21.5 ± 2.6 | 0.44 |
| Height (cm) | 158.6 ± 7.3 | 162.9 ± 8.3 | 0.02 |
| Weight (kg) | 56.7 ± 12.1 | 57.2 ± 8.4 | 0.50 |
| Hiatal hernia (+/-) | 7/49 | 14/27 | 0.02 |
| Drinking (+/-) | 17/39 | 18/23 | 0.10 |
| Smoking (+/-) | 7/49 | 8/23 | 0.30 |
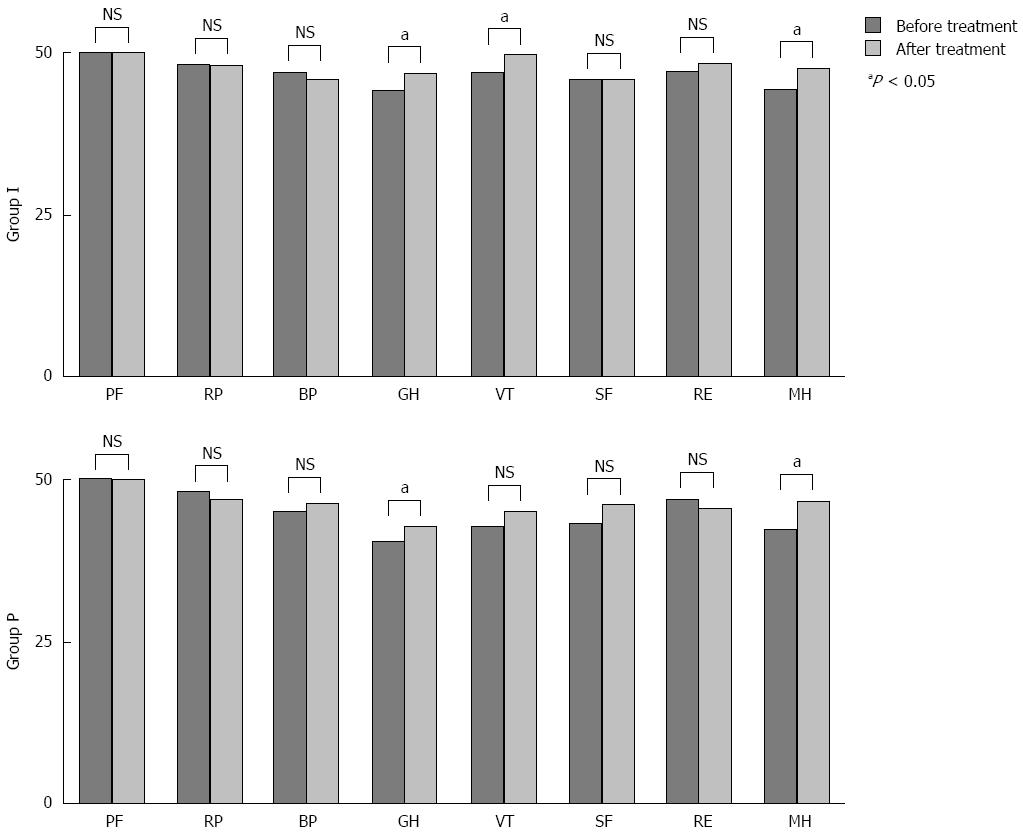
The SF-36 scores for group I significantly improved in relation to general health, vitality, and mental health after treatment, whereas the SF-36 scores for group P improved in relation to general health and mental health after treatment (Figure 4). Subgroup analysis showed that the SF-36 scores for patients with NERD grade N in group I significantly improved in relation to vitality and mental health after treatment, but there were no statistically significant differences in the SF-36 scores for patients with NERD grade M in group I after treatment (Figure 5). We did not detect any improvements in the SF-36 scores in group P after treatment, with the exception of the mental health scores for the patients with NERD grade M.
Patient compliance was determined by counting the remaining units of medication at the end of the four-week study period. All of the patients took more than 90% of the prescribed medication. No serious adverse events occurred, and none of the participants terminated the study because of adverse events.
The inhibition of acid secretion within the stomach using PPI or histamine 2 receptor blockers is the main approach for the treatment of NERD[14-17]. However, approximately half of the patients with NERD are resistant to therapy[18]. Many factors are associated with the pathogenesis of acid-suppression therapy-refractory NERD, including gas or bile acid reflux, mucosal hypersensitivity, delayed gastric emptying, and psychological disorders[18-21]. An appropriate therapeutic approach for patients with NERD has yet to be established if they fail to respond to acid suppression therapy. Therefore, determining the efficacy of therapeutic agents added to PPI therapy in patients with NERD has been anticipated for a long time. Sakata et al[12] reported that rikkunshito, which acts as a prokinetic agent and improves gastric empting and gastric accommodation, improved GERD symptoms in patients with PPI-refractory NERD. However, adding mosapride, which is another prokinetic agent, to PPI therapy did not significantly improve GERD symptoms compared with PPI therapy administered alone to patients with NERD[22]. Rebamipide, a cytoprotective anti-ulcer agent, also failed to effectively control reflux symptoms in patients with PPI-refractory NERD[23]. In the present study, we evaluated the efficacy of adding IM to rabeprazole in the treatment of patients with NERD in a prospective, randomized, double-blind, placebo-controlled trial. The impact of the therapy on the quality of the patients’ lives was evaluated as a secondary endpoint.
The results showed that using the PPI alone and in combination with IM significantly improved the FSSG scores after four weeks of treatment (P = 0.0001); however, there was no statistically significant difference between the groups. These data suggest that controlling acid secretion in the stomach is quite important for the treatment of NERD. Comparisons of the groups in relation to each FSSG score showed that the scores for two reflux-related questions significantly improved in the patients who received combination therapy compared with those who received mono-therapy, which suggests that IM may play a greater preventive role in relation to reflux compared with acid-related dysmotility symptoms. These results appear to be reasonable, given that IM could affect the epithelial cell connections or communications in the esophagus.
The Montreal consensus conference defined NERD as the presence of troublesome reflux-associated symptoms in the absence of mucosal breaks on endoscopy[2]. Recently, the endoscopic findings associated with NERD were classified into two groups, grades N and M. However, the clinical differences between the groups are not clear. In this study, the group of patients classified as having NERD grade N was characterized by shorter statures and lower frequencies of esophageal hiatal hernias. Joh et al[24] reported that NERD grade M patients tended to show a higher frequency of esophageal hiatal hernias, and they suggested that the minimal changes are most likely attributable to gastric acid reflux, which was based on their ambulatory 24-h esophageal monitoring data. Our study showed that in patients with NERD grade N, the addition of IM to PPI therapy significantly improved the FSSG scores compared with PPI mono-therapy, but this was not seen in patients with NERD grade M. These data suggest that factors that affect intercellular communication as well as reflux acid may be associated with the development of NERD grade N, whereas gastric acid reflux may play a major role in the development of NERD grade M.
IM facilitates intercellular communication through the gap junctions in the gastrointestinal tract, including the esophagus. Oyamada et al[25] demonstrated the existence of connexins 26 and 43 in human esophageal tissue. Several investigators have suggested that connexin-mediated intercellular communication could affect the formation of functional tight junctions[26-28]. A microscopic study found that esophageal mucosal DIS are present in patients with NERD, they are produced as a consequence of exposure to excess acid, and that esophageal mucosal DIS are associated with the symptom of heartburn[6]. A more recent study has shown that hypersensitive esophagus, which is associated with normal acid exposure and positive symptom associations for either acid and/or non-acid reflux, was related to DIS as well as basal cell hyperplasia and papillae elongation[29]. Taken together, these data suggest that the facilitation of gap junctional intercellular communication by IM may relieve NERD symptoms by ameliorating esophageal mucosal hypersensitivity to non-acid reflux[7,29,30]. We could easily speculate based on the current study’s results that NERD grade N includes more patients with hypersensitive esophagi than NERD grade M. Further investigations are required to elucidate the precise therapeutic mechanisms of IM.
Patients with GERD symptoms tend to have a lower QOL compared with the general population[31]. Recently, the SF-36 questionnaire has been used to screen for GERD and to assess QOL before and after treatment[32]. In the present study, the patients who received combination therapy showed significant improvements in three subscale scores, namely, general health, vitality, and mental health, whereas patients who received mono-therapy only showed improvements in two subscale scores. Subgroup analysis showed significant improvements in the vitality and mental health scores for patients with NERD grade N who received combination therapy, whereas no statistically significant improvements were observed for the patients with NERD grade M who received combination therapy. Given that the QOL data corresponded with the improvements in the GERD symptoms after the patients had been treated with IM and PPI, these results are acceptable.
Our study has some limitations that are described next. The main limitation of this study relates to the fact that NERD was diagnosed on the basis of the endoscopic findings alone. An accurate and reliable definition of NERD is needed to appropriately inform the discussion about the treatment of NERD. The second limitation relates to the study being a single-center investigation with a relatively small sample size. Hence, further trials employing larger numbers of subjects are necessary to verify our findings, and in these trials the pathological mechanisms underlying NERD should be investigated. The third limitation associated with this study relates to the controversy that surrounds the diagnostic and clinical relevance of the modified Los Angeles Classification for NERD. The fourth limitation of this study relates to the effects that IM metabolites or drug interactions among IM, rabeprazole, and other medicines might have had on the results of this study.
In conclusion, this is the first randomized controlled trial that has demonstrated that adding IM to PPI therapy improves patients’ GERD symptoms as well as the quality of their lives, particularly in NERD grade N patients. We consider that combination therapy may be an appropriate therapeutic option for patients with NERD.
Proton pump inhibitor (PPI) therapy is considered the mainstay for the treatment of non-erosive reflux disease (NERD). Some reports have suggested that compared with patients with reflux esophagitis, those with NERD have lower response rates to acid suppression therapy. However, a recent meta-analysis emphasized that well-defined NERD patients, including those with abnormal distal esophageal acid exposure and those with hypersensitive esophagi, have responses to PPI therapy that are similar to those seen in patients with RE.
Although the pathophysiology of NERD remains unclear, electron microscopy and light microscopy have demonstrated the presence of esophageal mucosal dilated intercellular spaces (DIS) in patients with NERD. Irsogladine maleate (IM) activates gap junctional intercellular communication and affects the mucosal DIS; however, little is known about the effects of IM on patients with NERD.
This double-blind, placebo-controlled study showed that adding IM to rabeprazole improved gastroesophageal reflux disease (GERD) symptoms and the quality of the lives of patients categorized as having NERD who did not have minimal changes (grade N), which was based on the modified Los Angeles classification.
This prospective, double-blind, placebo-controlled trial was designed to evaluate the efficacy of adding IM to PPI therapy in endoscopy-negative Japanese patients with reflux symptoms. The study’s main finding was that there was no statistically significant difference between group I (IM + PPI) and group P (placebo + PPI) with respect to the Frequency Scale for the Symptoms of GERD (FSSG) scores. Moreover, a subgroup analysis showed that significant improvements in the FSSG scores had occurred in the patients in group I who had NERD grade N, which was defined based on endoscopic assessments.
P- Reviewer: George J, Higuchi K, Savarino E, Xie HG S- Editor: Yu J L- Editor: O’Neill M E- Editor: Wang CH
| 1. | Moayyedi P, Talley NJ. Gastro-oesophageal reflux disease. Lancet. 2006;367:2086-2100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 279] [Cited by in F6Publishing: 239] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 2. | Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900-120; quiz 1943. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2368] [Cited by in F6Publishing: 2220] [Article Influence: 123.3] [Reference Citation Analysis (2)] |
| 3. | Armstrong D. A critical assessment of the current status of non-erosive reflux disease. Digestion. 2008;78 Suppl 1:46-54. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Hongo M. Minimal changes in reflux esophagitis: red ones and white ones. J Gastroenterol. 2006;41:95-99. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 83] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Fass R, Shapiro M, Dekel R, Sewell J. Systematic review: proton-pump inhibitor failure in gastro-oesophageal reflux disease--where next? Aliment Pharmacol Ther. 2005;22:79-94. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 288] [Cited by in F6Publishing: 241] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 6. | Savarino E, Zentilin P, Savarino V. NERD: an umbrella term including heterogeneous subpopulations. Nat Rev Gastroenterol Hepatol. 2013;10:371-380. [PubMed] [Cited in This Article: ] |
| 7. | Savarino E, Zentilin P, Tutuian R, Pohl D, Gemignani L, Malesci A, Savarino V. Impedance-pH reflux patterns can differentiate non-erosive reflux disease from functional heartburn patients. J Gastroenterol. 2012;47:159-168. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 81] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 8. | Weijenborg PW, Cremonini F, Smout AJ, Bredenoord AJ. PPI therapy is equally effective in well-defined non-erosive reflux disease and in reflux esophagitis: a meta-analysis. Neurogastroenterol Motil. 2012;24:747-57, e350. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 94] [Cited by in F6Publishing: 99] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 9. | Pandolfino JE, Kahrilas PJ. Prolonged pH monitoring: Bravo capsule. Gastrointest Endosc Clin N Am. 2005;15:307-318. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Orlando LA, Orlando RC. Dilated intercellular spaces as a marker of GERD. Curr Gastroenterol Rep. 2009;11:190-194. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Kusano M, Shimoyama Y, Sugimoto S, Kawamura O, Maeda M, Minashi K, Kuribayashi S, Higuchi T, Zai H, Ino K. Development and evaluation of FSSG: frequency scale for the symptoms of GERD. J Gastroenterol. 2004;39:888-891. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 302] [Cited by in F6Publishing: 326] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 12. | Sakata Y, Tominaga K, Kato M, Takeda H, Shimoyama Y, Takeuchi T, Iwakiri R, Furuta K, Sakurai K, Odaka T. Clinical characteristics of elderly patients with proton pump inhibitor-refractory non-erosive reflux disease from the G-PRIDE study who responded to rikkunshito. BMC Gastroenterol. 2014;14:116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Tominaga K, Iwakiri R, Fujimoto K, Fujiwara Y, Tanaka M, Shimoyama Y, Umegaki E, Higuchi K, Kusano M, Arakawa T. Rikkunshito improves symptoms in PPI-refractory GERD patients: a prospective, randomized, multicenter trial in Japan. J Gastroenterol. 2012;47:284-292. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 14. | Talley NJ, Lauritsen K, Tunturi-Hihnala H, Lind T, Moum B, Bang C, Schulz T, Omland TM, Delle M, Junghard O. Esomeprazole 20 mg maintains symptom control in endoscopy-negative gastro-oesophageal reflux disease: a controlled trial of ‘on-demand’ therapy for 6 months. Aliment Pharmacol Ther. 2001;15:347-354. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 139] [Cited by in F6Publishing: 140] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 15. | Talley NJ, Venables TL, Green JR, Armstrong D, O’Kane KP, Giaffer M, Bardhan KD, Carlsson RG, Chen S, Hasselgren GS. Esomeprazole 40 mg and 20 mg is efficacious in the long-term management of patients with endoscopy-negative gastro-oesophageal reflux disease: a placebo-controlled trial of on-demand therapy for 6 months. Eur J Gastroenterol Hepatol. 2002;14:857-863. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 83] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 16. | Bytzer P, Blum A, De Herdt D, Dubois D. Six-month trial of on-demand rabeprazole 10 mg maintains symptom relief in patients with non-erosive reflux disease. Aliment Pharmacol Ther. 2004;20:181-188. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 65] [Cited by in F6Publishing: 47] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Kobeissy AA, Hashash JG, Jamali FR, Skoury AM, Haddad R, El-Samad S, Ladki R, Aswad R, Soweid AM. A randomized open-label trial of on-demand rabeprazole vs ranitidine for patients with non-erosive reflux disease. World J Gastroenterol. 2012;18:2390-2395. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Tominaga K, Kato M, Takeda H, Shimoyama Y, Umegaki E, Iwakiri R, Furuta K, Sakurai K, Odaka T, Kusunoki H. A randomized, placebo-controlled, double-blind clinical trial of rikkunshito for patients with non-erosive reflux disease refractory to proton-pump inhibitor: the G-PRIDE study. J Gastroenterol. 2014;49:1392-1405. [PubMed] [Cited in This Article: ] |
| 19. | Rodriguez-Stanley S, Robinson M, Earnest DL, Greenwood-Van Meerveld B, Miner PB. Esophageal hypersensitivity may be a major cause of heartburn. Am J Gastroenterol. 1999;94:628-631. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 86] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 20. | Nagahara A, Miwa H, Minoo T, Hojo M, Kawabe M, Osada T, Kurosawa A, Asaoka D, Terai T, Ohkusa T. Increased esophageal sensitivity to acid and saline in patients with nonerosive gastro-esophageal reflux disease. J Clin Gastroenterol. 2006;40:891-895. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 21. | Wiklund I, Carlsson R, Carlsson J, Glise H. Psychological factors as a predictor of treatment response in patients with heartburn: a pooled analysis of clinical trials. Scand J Gastroenterol. 2006;41:288-293. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 29] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Miwa H, Inoue K, Ashida K, Kogawa T, Nagahara A, Yoshida S, Tano N, Yamazaki Y, Wada T, Asaoka D. Randomised clinical trial: efficacy of the addition of a prokinetic, mosapride citrate, to omeprazole in the treatment of patients with non-erosive reflux disease - a double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2011;33:323-332. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 23. | Adachi K, Furuta K, Miwa H, Oshima T, Miki M, Komazawa Y, Iwakiri K, Furuta T, Koike T, Shimatani T. A study on the efficacy of rebamipide for patients with proton pump inhibitor-refractory non-erosive reflux disease. Dig Dis Sci. 2012;57:1609-1617. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Joh T, Miwa H, Higuchi K, Shimatani T, Manabe N, Adachi K, Wada T, Sasaki M, Fujiwara Y, Hongo M. Validity of endoscopic classification of nonerosive reflux disease. J Gastroenterol. 2007;42:444-449. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 25. | Oyamada Y, Oyamada M, Fusco A, Yamasaki H. Aberrant expression, function and localization of connexins in human esophageal carcinoma cell lines with different degrees of tumorigenicity. J Cancer Res Clin Oncol. 1994;120:445-453. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Morita H, Katsuno T, Hoshimoto A, Hirano N, Saito Y, Suzuki Y. Connexin 26-mediated gap junctional intercellular communication suppresses paracellular permeability of human intestinal epithelial cell monolayers. Exp Cell Res. 2004;298:1-8. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 41] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 27. | Kojima T, Spray DC, Kokai Y, Chiba H, Mochizuki Y, Sawada N. Cx32 formation and/or Cx32-mediated intercellular communication induces expression and function of tight junctions in hepatocytic cell line. Exp Cell Res. 2002;276:40-51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 61] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Isomura Y, Yamaji Y, Yamada A, Watanabe Y, Suzuki H, Kobayashi Y, Yoshida S, Watabe H, Hirata Y, Yoshida H. Irsogladine improves small-intestinal injuries in regular users of nonsteroidal anti-inflammatory drugs. Gastrointest Endosc. 2014;80:118-125. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Savarino E, Zentilin P, Mastracci L, Dulbecco P, Marabotto E, Gemignani L, Bruzzone L, de Bortoli N, Frigo AC, Fiocca R. Microscopic esophagitis distinguishes patients with non-erosive reflux disease from those with functional heartburn. J Gastroenterol. 2013;48:473-482. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 127] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 30. | Savarino E, Zentilin P, Tutuian R, Pohl D, Casa DD, Frazzoni M, Cestari R, Savarino V. The role of nonacid reflux in NERD: lessons learned from impedance-pH monitoring in 150 patients off therapy. Am J Gastroenterol. 2008;103:2685-2693. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 178] [Cited by in F6Publishing: 164] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 31. | Kulig M, Leodolter A, Vieth M, Schulte E, Jaspersen D, Labenz J, Lind T, Meyer-Sabellek W, Malfertheiner P, Stolte M. Quality of life in relation to symptoms in patients with gastro-oesophageal reflux disease-- an analysis based on the ProGERD initiative. Aliment Pharmacol Ther. 2003;18:767-776. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 172] [Cited by in F6Publishing: 167] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 32. | Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473-483. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23352] [Cited by in F6Publishing: 22698] [Article Influence: 709.3] [Reference Citation Analysis (0)] |