Published online Nov 7, 2008. doi: 10.3748/wjg.14.6418
Revised: September 16, 2008
Accepted: September 23, 2008
Published online: November 7, 2008
Polysplenia syndrome, defined as the presence of multiple spleens of almost equal volume, is a rare condition involving congenital anomalies in multiple organ systems. We report this anomaly in a 41-year-old female who underwent a left lateral sectionectomy due to recurrent cholangitis and impacted left lateral duct stones. Polysplenia syndrome with preduodenal vein was diagnosed preoperatively by computed tomography (CT) and surgery was done safely. Although the polysplenia syndrome with preduodenal portal vein (PDPV) in adult is rarely encountered, surgeons need to understand the course of the portal vein and exercise caution in approaching the biliary tract.
- Citation: Seo HI, Jeon TY, Sim MS, Kim S. Polysplenia syndrome with preduodenal portal vein detected in adults. World J Gastroenterol 2008; 14(41): 6418-6420
- URL: https://www.wjgnet.com/1007-9327/full/v14/i41/6418.htm
- DOI: https://dx.doi.org/10.3748/wjg.14.6418
Polysplenia syndrome is a rare disease that occurs in patients with two or more spleens of identical sizes and various organ anomalies[1]. Reports indicate that most patients with polysplenia syndrome die before 5 years of age because the disease is often associated with congenital anomalies, such as cardiovascular anomalies[2]. Severe cardiovascular anomalies include interruption of the suprarenal inferior vena cava, atrioventricular septal defects, ipsilateral pulmonary venous drainage, ventricular outflow tract obstruction, dextrocardia and abnormal great vessel relationships[3]. Some patients with polysplenia syndrome have a normal heart or only minor cardiac defects, are often diagnosed incidentally in patients being treated for other disease[4]. However, they may harbor anomalies in abdominal organs or the gastrointestinal tract, one example of which is a preduodenal portal vein (PDPV)[5]. A PDPV can be diagnosed early as duodenal obstruction in infants, but is often found incidentally or during surgery when there are no symptoms[6].
One of the ways to prevent injuries to the hepatic portal system during surgery is to diagnosis polyspenia syndrome accompanied by a PDPV prior to surgery. We treated a patient with polysplenia syndrome, which was diagnosed during a left lateral sectionectomy to treat intrahepatic duct stones, and we report our findings along with related studies.
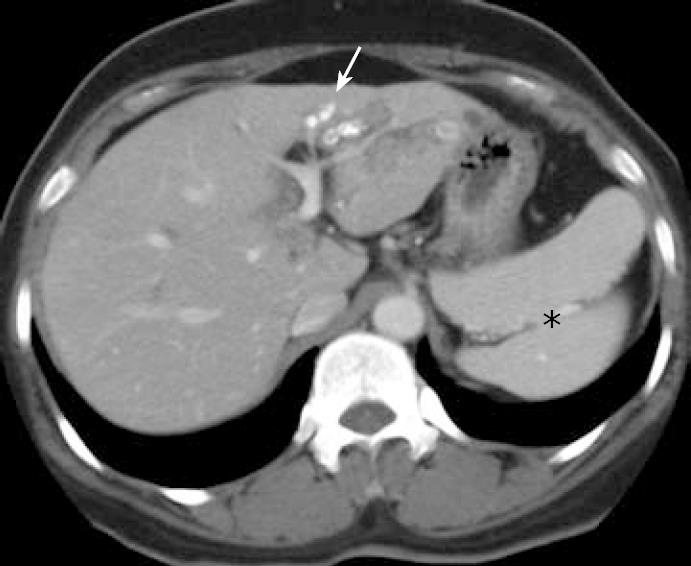
A 41-year-old female presented for evaluation of right upper quadrant pain of 1 mo duration. At a local hospital, she was noted to have polysplenia and left lateral intrahepatic duct stones without intrahepatic duct dilatation of segment 4. She was referred to our institution for further evaluation and treatment. The physical examination revealed no abnormalities. An abdominal computed tomography (CT) showed intrahepatic duct stones with polysplenia and the portal vein was located anteriorly to the duodenum (Figure 1). Laboratory findings revealed elevated levels of aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase and lactate dehydrogenase. Echocardiography and chest radiography were normal. The diagnosis of intraheptic duct stones with polyspenia syndrome was established.
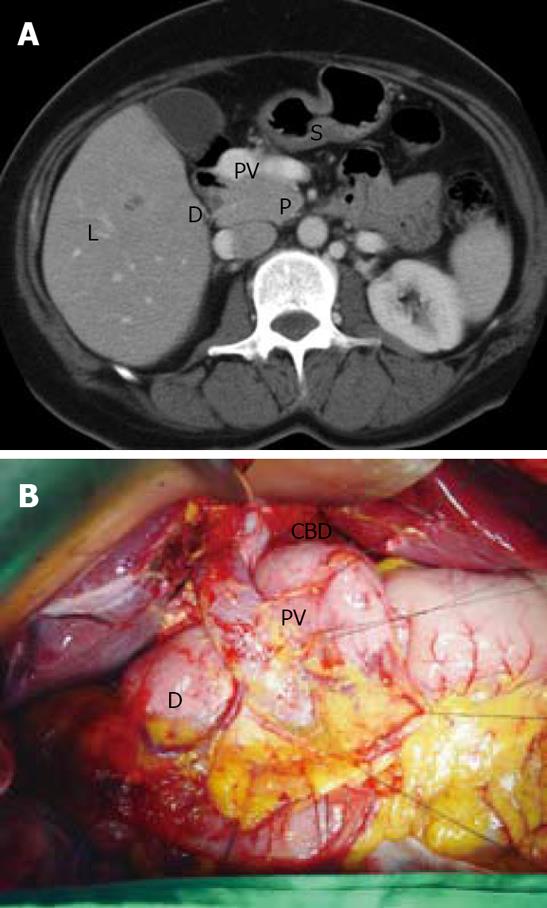
The surgical procedure for intrahepatic duct stones began with a thorough exploration of the abdomen. The portal vein was detected in front of the first part of the duodenum. The portal vein passed upward, right to the common bile duct, and bifurcated into the left and right portal branches in the porta hepatis (Figure 2). Both the common bile duct and the right hepatic artery were identified to the left of the portal vein. The left hepatic artery originated from the left gastric artery. The presence of two spleens was confirmed on the left side of the upper abdomen, along with the greater curvature of the stomach. A nasogastric tube passed through duodenum without any difficulty. We could not locate the stenotic duodenal region posterior to the portal vein. The shape of the liver and pancreas were normal; the small bowel and colon were normally positioned.
A left lateral sectionectomy with a cholecystectomy was performed safely. An intraoperative choledochoscopy through the segment 3 bile duct was done for removal of the right intrahepatic duct stone, and we confirmed no residual stones existed in the bile duct based on T-tube cholangiography (Figure 3). The postoperative course was uneventful, and the patient was discharged 12 d postoperatively.
As the name of the condition implies, polysplenia syndrome refers to patients with two or more spleens. Studies also include descriptions of cases that involve a number of very small spleens, a multilobular spleen with tiny accessory spleen, and an undivided spleen[2,7].
The spleen develops during the 5th embryonic week from the splenic primordia, originating from the dorsal mesogastrium. The initial splenic primordia are then created as incisures on the left side of the dorsal mesogastrium. When the incisures fail to fuse, they create two or more spleens[8]. The blood flow of an embryo makes a transition from symmetric to asymmetric around the 25th d to determine the visceral sidedness, and it has been suggested that this is when cono-truncal anomalies and anomalies of atrioventricular canal occur[9]. At the same time, PDPV also develop. Venous blood is drained from the primitive gut, consisting of two vitelline veins of the yolk sac. The veins implement communication in the liver (cranial communication), behind (middle communication) and in front of (caudal communication) the duodenum. When the caudal and cranial communications are lost during the 9-mm embryo stage, the S-shape portal vein is created. It is believed that the PDPV anomaly is developed during this stage if cranial and middle communications are lost[10].
Although the exact cause of polysplenia is unknown, studies have suggested that it is caused by various factors including embryogenic, genetic, and teratogenic components[11]. Since splenic anomalies (splenic agenesis, hypogenesis and polysplenia) are often accompanied by anomalies in the cardiovascular tract and other abdominal organs, it can be inferred that the spleen plays a significant role during the early embryonic stage[12].
Reports indicate that polysplenia syndrome occurs in both genders with an identical frequency[5]. Known cardiovascular anomalies include absence or hypoplasia of the suprarenal inferior vena cava (with or without azygos or hemiazygos continuation), levoisomerism of the right bronchial tree, dextrocardia, ventricular septal defects, and the absence of the coronary sinuses, most patients die before 5 years of age due to the accompanying cardiovascular anomalies. Patients without cardiac anomalies may reach adulthood, accounting for 10%-15% of cases of polysplenia. Since most adult patients do not exhibit any symptoms, polysplenia syndrome is often diagnosed incidentally during other procedures[5]. Even adult patients can have anomalies in abdominal organs including visceral heterotaxia with a right-sided stomach, a left-sided or large midline liver, right-sided spleen, malrotation of the intestine, a short pancreas, and anomalies of the inferior vena cava. Cases with only PDPV, as with our patient, are recognized as very minor anomalous cases. Even though intestinal obstruction is often displayed in such cases, there were no anomalies of the digestion system for our patient. First described by Knight HO in 1921, PDPV is a congenital anomaly that involves the portal vein passing in front of the duodenum[13]. A PDPV can be associated with duodenal atresia, stenosis, web, annular pancreas and malrotation, and surgery may be required for treatment[14]. However, since the portal vein is a thin-walled, low-pressure vessel, it is highly unlikely that PDPV alone can cause duodenal obstruction. Patients can survive to reach adulthood without any symptoms, and the anomaly is often found during examinations or surgeries to treat other diseases.
Polysplenia syndrome can be detected relatively easily with diagnostic imaging including abdominal CT and magnetic resonance imaging (MRI)[15]. In our case, polysplenia syndrome was diagnosed incidentally while examining the patient who was complaining of pain in the right upper abdomen and fever. Known causes of atrophy of the lateral segment of the liver in PDPV include selective portal vein obstruction, biliary duct obstruction, partial obstruction of the portal vein associated with distention of the hepatic bile duct, long-standing malnutrition and cachexia, or toxic and vascular influences[14]. However, in the case of our patient, it is likely that the atrophy was caused by intrahepatic duct stones. Reports indicate that most cases of PDPV in adults involve surgery for cholelithiasis, making us believe that PDPV could be a cause for cholelithiasis[14]. When surgery is required, care must be exercised, especially for procedures involving the upper abdomen. If PDPV is not detected prior to surgery, it can cause severe complications, such as hemorrhage and vascular ligation. Such accidents can be prevented by performing careful diagnostic imaging in advance, such as CT, and especially noting the possibility of PDPV in cases of polysplenia syndrome.
Peer reviewers: Li-Qin Zhao, PhD, Department of Radiology, Beijing Friendship Hospital Affiliate of Capital University of Medical Science, 95, Yongan Road, Xuanwu Distric, Beijing 100050, China; Byung Ihn Choi, Professor, Department of Radiology, Seoul National University Hospital, 28, Yeongeon-dong, Jongno-gu, Seoul 110-744, South Korea
S- Editor Li DL E- Editor Ma WH
| 1. | Griffiths JD, Marshall VC. Torsion of the spleen in the polysplenia syndrome. Aust N Z J Surg. 1984;54:571-573. [Cited in This Article: ] |
| 2. | Gayer G, Hertz M, Strauss S, Zissin R. Congenital anomalies of the spleen. Semin Ultrasound CT MR. 2006;27:358-369. [Cited in This Article: ] |
| 3. | Roguin N, Hammerman H, Korman S, Riss E. Angiography of azygos continuation of inferior vena cava in situs ambiguus with left isomerism (polysplenia syndrome). Pediatr Radiol. 1984;14:109-112. [Cited in This Article: ] |
| 4. | Gayer G, Apter S, Jonas T, Amitai M, Zissin R, Sella T, Weiss P, Hertz M. Polysplenia syndrome detected in adulthood: report of eight cases and review of the literature. Abdom Imaging. 1999;24:178-184. [Cited in This Article: ] |
| 5. | Peoples WM, Moller JH, Edwards JE. Polysplenia: a review of 146 cases. Pediatr Cardiol. 1983;4:129-137. [Cited in This Article: ] |
| 6. | Ooshima I, Maruyama T, Ootsuki K, Ozaki M. Preduodenal portal vein in the adult. J Hepatobiliary Pancreat Surg. 1998;5:455-458. [Cited in This Article: ] |
| 7. | Abut E, Akkaya L, Uysal U, Arman A, Guveli H, Bolukbas C, Kurdas OO. Selective spleen scintigraphy in the diagnosis of polysplenia syndrome. Br J Radiol. 2004;77:698-700. [Cited in This Article: ] |
| 8. | Gayer G, Zissin R, Apter S, Atar E, Portnoy O, Itzchak Y. CT findings in congenital anomalies of the spleen. Br J Radiol. 2001;74:767-772. [Cited in This Article: ] |
| 9. | Miyabara S, Sugihara H, Kamio A, Oota K, Abe H, Kato S. Atypical polysplenia only with the hepatic segment of inferior vena in a middle-aged. Acta pathol Jpn. 1984;34:111-116. [Cited in This Article: ] |
| 10. | Muneta S, Sakai S, Fukuda H, Imamura Y, Matsumoto I. Polysplenia syndrome with various visceral anomalies in an adult: embryological and clinical considerations. Intern Med. 1992;31:1026-1031. [Cited in This Article: ] |
| 11. | de la Monte SM, Hutchins GM. Sisters with polysplenia. Am J Med Genet. 1985;21:171-176. [Cited in This Article: ] |
| 12. | Nakada K, Kawaguchi F, Wakisaka M, Nakada M, Enami T, Yamate N. Digestive tract disorders associated with asplenia/polysplenia syndrome. J Pediatr Surg. 1997;32:91-94. [Cited in This Article: ] |
| 13. | Knight HO. An anomalous portal vein with its surgical dangers. Ann Surg. 1921;74:697-699. [Cited in This Article: ] |
| 14. | Ishizaki Y, Tanaka M, Okuyama T. Surgical implications of preduodenal portal vein in the adult. Case report and review of the literature. Arch Surg. 1994;129:773-775. [Cited in This Article: ] |
| 15. | Kobayashi H, Kawamoto S, Tamaki T, Konishi J, Togashi K. Polysplenia associated with semiannular pancreas. Eur Radiol. 2001;11:1639-1641. [Cited in This Article: ] |