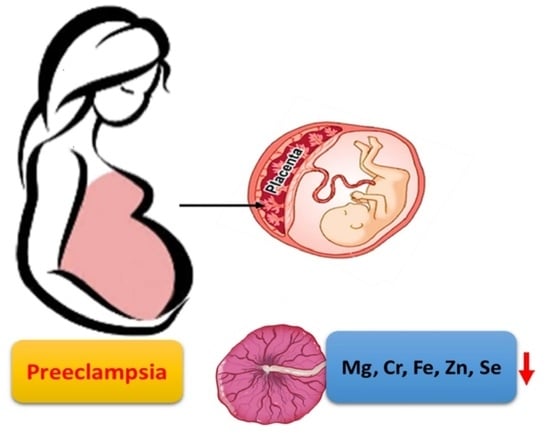
Reduction in Placental Metal and Metalloid in Preeclampsia: A Case–Control Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Study Participants
2.2. Assay of Metal and Metalloid in Placenta
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Study Participants
3.2. Metal and Metalloid in Placenta
3.3. Placental Metals and Metalloids and Preeclampsia Risk
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bartal, M.F.; Sibai, B.M. Eclampsia in the 21st century. Am. J. Obstet. Gynecol. 2022, 226, S1237–S1253. [Google Scholar] [CrossRef]
- Erez, O.; Romero, R.; Jung, E.; Chaemsaithong, P.; Bosco, M.; Suksai, M.; Gallo, D.M.; Gotsch, F. Preeclampsia and eclampsia: The conceptual evolution of a syndrome. Am. J. Obstet. Gynecol. 2022, 226, S786–S803. [Google Scholar] [CrossRef]
- Powe, C.E.; Levine, R.J.; Karumanchi, S.A. Preeclampsia, a Disease of the Maternal Endothelium The Role of Antiangiogenic Factors and Implications for Later Cardiovascular Disease. Circulation 2011, 123, 2856–2869. [Google Scholar] [CrossRef]
- Garovic, V.D.; Dechend, R.; Easterling, T.; Karumanchi, A.; Baird, S.M.; Magee, L.A.; Rana, S.; Vermunt, J.V.; August, P.; Chair, V.; et al. Hypertension in Pregnancy: Diagnosis, Blood Pressure Goals, and Pharmacotherapy: A Scientific Statement from the American Heart Association. Hypertension 2022, 79, E21–E41. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.A.; Magee, L.A.; Kenny, L.C.; Karumanchi, S.A.; McCarthy, F.P.; Saito, S.; Hall, D.R.; Warren, C.E.; Adoyi, G.; Ishaku, S.; et al. Hypertensive Disorders of Pregnancy ISSHP Classification, Diagnosis, and Management Recommendations for International Practice. Hypertension 2018, 72, 24–43. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.G.; Zhang, M.Y.; Guallar, E.; Wang, G.Y.; Hong, X.M.; Wang, X.B.; Mueller, N.T. Trace Minerals, Heavy Metals, and Preeclampsia: Findings from the Boston Birth Cohort. J. Am. Heart Assoc. 2019, 8, e012436. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, K.K.; Han, T.B.; Zhang, P.; Chen, X.; Wu, W.W.; Feng, Y.L.; Yang, H.L.; Li, M.; Xie, B.J.; et al. Exposure to multiple metals and prevalence for preeclampsia in Taiyuan, China. Environ. Int. 2020, 145, 106098. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, J.; Liao, J.; Hu, C.; Cao, Z.; Xia, W.; Xu, S.; Li, Y. Impacts of Ambient Fine Particulate Matter on Blood Pressure Pattern and Hypertensive Disorders of Pregnancy Evidence from the Wuhan Cohort Study. Hypertension 2021, 77, 1133–1140. [Google Scholar] [CrossRef]
- Borghese, M.M.; Fisher, M.; Ashley-Martin, J.; Fraser, W.D.; Trottier, H.; Lanphear, B.; Johnson, M.; Helewa, M.; Foster, W.; Walker, M.; et al. Individual, Independent, and Joint Associations of Toxic Metals and Manganese on Hypertensive Disorders of Pregnancy: Results from the MIREC Canadian Pregnancy Cohort. Environ. Health Perspect. 2023, 131, 47014. [Google Scholar] [CrossRef] [PubMed]
- Zoroddu, M.A.; Aaseth, J.; Crisponi, G.; Medici, S.; Peana, M.; Nurchi, V.M. The essential metals for humans: A brief overview. J. Inorg. Biochem. 2019, 195, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Kovacs, C.S. Maternal Mineral and Bone Metabolism during Pregnancy, Lactation, and Post-Weaning Recovery. Physiol. Rev. 2016, 96, 449–547. [Google Scholar] [CrossRef]
- Farias, P.M.; Marcelino, G.; Santana, L.F.; de Almeida, E.B.; Guimaraes, R.D.A.; Pott, A.; Hiane, P.A.; Freitas, K.D. Minerals in Pregnancy and Their Impact on Child Growth and Development. Molecules 2020, 25, 5630. [Google Scholar] [CrossRef]
- Cormick, G.; Belizan, J.M. Calcium Intake and Health. Nutrients 2019, 11, 1606. [Google Scholar] [CrossRef]
- De Baaij, J.H.F.; Hoenderop, J.G.J.; Bindels, R.J.M. Magnesium in Man: Implications for Health and Disease. Physiol. Rev. 2015, 95, 1–46. [Google Scholar] [CrossRef]
- Rylander, R. Magnesium in pregnancy blood pressure and pre-eclampsia—A review. Pregnancy Hypertens. Int. J. Womens Cardiovasc. Health 2014, 4, 146–149. [Google Scholar] [CrossRef]
- Scott, G.; Gillon, T.E.; Pels, A.; von Dadelszen, P.; Magee, L.A. Guidelines-similarities and dissimilarities: A systematic review of international clinical practice guidelines for pregnancy hypertension. Am. J. Obstet. Gynecol. 2022, 226, S1222–S1236. [Google Scholar] [CrossRef]
- Dangelo, E.K.G.; Singer, H.A.; Rembold, C.M. Magnesium Relaxes Arterial Smooth-Muscle by Decreasing Intracellular Ca2+ without Changing Intracellular Mg2+. J. Clin. Investig. 1992, 89, 1988–1994. [Google Scholar] [CrossRef]
- Duley, L.; Gülmezoglu, A.M.; Henderson-Smart, D.J.; Chou, D. Magnesium sulphate and other anticonvulsants for women with pre-eclampsia. Cochrane Database Syst. Rev. 2010, 2010, CD000025. [Google Scholar] [CrossRef] [PubMed]
- Hofmeyr, G.J.; Lawrie, T.A.; Atallah, A.N.; Duley, L.; Torloni, M.R. Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst. Rev. 2018, 10, CD001059. [Google Scholar] [CrossRef] [PubMed]
- Georgieff, M.K. Iron deficiency in pregnancy. Am. J. Obstet. Gynecol. 2020, 223, 516–524. [Google Scholar] [CrossRef] [PubMed]
- Pi, X.; Wei, Y.H.; Li, Z.W.; Jin, L.; Liu, J.F.; Zhang, Y.L.; Wang, L.L.; Ren, A.G. Higher concentration of selenium in placental tissues is associated with reduced risk for orofacial clefts. Clin. Nutr. 2019, 38, 2442–2448. [Google Scholar] [CrossRef] [PubMed]
- Majali-Martinez, A.; Hiden, U.; Ghaffari-Tabrizi-Wizsy, N.; Lang, U.; Desoye, G.; Dieber-Rotheneder, M. Placental membrane-type metalloproteinases (MT-MMPs): Key players in pregnancy. Cell Adhes. Migr. 2016, 10, 136–146. [Google Scholar] [CrossRef] [PubMed]
- Mistry, H.D.; Wilson, V.; Ramsay, M.M.; Symonds, M.E.; Pipkin, F.B. Reduced Selenium Concentrations and Glutathione Peroxidase Activity in Preeclamptic Pregnancies. Hypertension 2008, 52, 881–888. [Google Scholar] [CrossRef] [PubMed]
- Hogan, C.; Perkins, A.V. Selenoproteins in the Human Placenta: How Essential Is Selenium to a Healthy Start to Life? Nutrients 2022, 14, 628. [Google Scholar] [CrossRef] [PubMed]
- Sarwar, M.S.; Ahmed, S.; Ullah, M.S.; Kabir, H.; Rahman, G.K.M.M.; Hasnat, A.; Islam, M.S. Comparative Study of Serum Zinc, Copper, Manganese, and Iron in Preeclamptic Pregnant Women. Biol. Trace Elem. Res. 2013, 154, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Heimann, Y.; Schmidt, A.; Morales, D.; Markert, U. Analysis of Extracellular Vesicle Release and Composition after Treatment of Trophoblastic Cell Lines with Heavy Metals. Placenta 2017, 57, 297. [Google Scholar] [CrossRef]
- Kahn, L.G.; Trasande, L. Environmental Toxicant Exposure and Hypertensive Disorders of Pregnancy: Recent Findings. Curr. Hypertens. Rep. 2018, 20, 87. [Google Scholar] [CrossRef]
- Solenkova, N.V.; Newman, J.D.; Berger, J.S.; Thurston, G.; Hochman, J.S.; Lamas, G.A. Metal pollutants and cardiovascular disease: Mechanisms and consequences of exposure. Am. Heart J. 2014, 168, 812–822. [Google Scholar] [CrossRef]
- Gajewska, K.; Blazewicz, A.; Laskowska, M.; Nizinski, P.; Dymara-Konopka, W.; Komsta, L. Chemical elements and preeclampsia—An overview of current problems, challenges and significance of recent research. J. Trace Elem. Med. Biol. 2020, 59, 126468. [Google Scholar] [CrossRef]
- Gil, F.; Hernandez, A.F. Toxicological importance of human biomonitoring of metallic and metalloid elements in different biological samples. Food Chem. Toxicol. 2015, 80, 287–297. [Google Scholar] [CrossRef] [PubMed]
- Young, B.C.; Levine, R.J.; Karumanchi, S.A. Pathogenesis of Preeclampsia. Annu. Rev. Pathol. Mech. 2010, 5, 173–192. [Google Scholar] [CrossRef]
- Pan, X.F.; Wang, L.M.; Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocromol. 2021, 9, 373–392. [Google Scholar] [CrossRef] [PubMed]
- Bobb, J.F.; Valeri, L.; Claus Henn, B.; Christiani, D.C.; Wright, R.O.; Mazumdar, M.; Godleski, J.J.; Coull, B.A. Bayesian kernel machine regression for estimating the health effects of multi-pollutant mixtures. Biostatistics 2015, 16, 493–508. [Google Scholar] [CrossRef]
- Bobb, J.F.; Henn, B.C.; Valeri, L.; Coull, B.A. Statistical software for analyzing the health effects of multiple concurrent exposures via Bayesian kernel machine regression. Environ. Health 2018, 17, 67. [Google Scholar] [CrossRef]
- Staff, A.C.; Fjeldstad, H.E.; Fosheim, I.K.; Moe, K.; Turowski, G.; Johnsen, G.M.; Alnaes-Katjavivi, P.; Sugulle, M. Failure of physiological transformation and spiral artery atherosis: Their roles in preeclampsia. Am. J. Obs. Gynecol. 2022, 226, S895–S906. [Google Scholar] [CrossRef] [PubMed]
- Melchiorre, K.; Giorgione, V.; Thilaganathan, B. The placenta and preeclampsia: Villain or victim? Am. J. Obs. Gynecol. 2022, 226, S954–S962. [Google Scholar] [CrossRef]
- Qu, H.M.; Khalil, R.A. Role of ADAM and ADAMTS disintegrin and metalloproteinases in normal pregnancy and preeclampsia. Biochem. Pharmacol. 2022, 206, 115266. [Google Scholar] [CrossRef]
- Delaney, K.M.; Guillet, R.; Pressman, E.K.; Caulfield, L.E.; Zavaleta, N.; Abrams, S.A.; O’Brien, K.O. Iron absorption during pregnancy is underestimated when iron utilization by the placenta and fetus is ignored. Am. J. Clin. Nutr. 2020, 112, 576–585. [Google Scholar] [CrossRef] [PubMed]
- Desoye, G.; Gauster, M.; Wadsack, C. Placental transport in pregnancy pathologies. Am. J. Clin. Nutr. 2011, 94, 1896S–1902S. [Google Scholar] [CrossRef]
- Chen, Y.; Ou, Q.X.; Chen, Y.; Zhu, Q.L.; Tan, M.H.; Zhang, M.M.; Wu, S.Z.; Xu, H.Y. Association between trace elements and preeclampsia: A retrospective cohort study. J. Trace Elem. Med. Biol. 2022, 72, 126971. [Google Scholar] [CrossRef]
- Bommarito, P.A.; Kim, S.S.; Meeker, J.D.; Fry, R.C.; Cantonwine, D.E.; McElrath, T.F.; Ferguson, K.K. Urinary trace metals, maternal circulating angiogenic biomarkers, and preeclampsia: A single-contaminant and mixture-based approach. Environ. Health 2019, 18, 63. [Google Scholar] [CrossRef]
- Hamdan, H.Z.; Hamdan, S.Z.; Adam, I. Association of Selenium Levels with Preeclampsia: A Systematic Review and Meta-analysis. Biol. Trace Elem. Res. 2023, 201, 2105–2122. [Google Scholar] [CrossRef]
- Stojsavljevic, A.; Rovcanin, M.; Rovcanin, B.; Mikovic, Z.; Jeremic, A.; Perovic, M.; Manojlovic, D. Human biomonitoring of essential, nonessential, rare earth, and noble elements in placental tissues. Chemosphere 2021, 285, 131518. [Google Scholar] [CrossRef]
- Banu, S.K.; Stanley, J.A.; Taylor, R.J.; Sivakumar, K.K.; Arosh, J.A.; Zeng, L.X.; Pennathur, S.; Padmanabhan, V. Sexually Dimorphic Impact of Chromium Accumulation on Human Placental Oxidative Stress and Apoptosis. Toxicol. Sci. 2018, 161, 375–387. [Google Scholar] [CrossRef] [PubMed]
- Lapehn, S.; Paquette, A.G. The Placental Epigenome as a Molecular Link between Prenatal Exposures and Fetal Health Outcomes through the DOHaD Hypothesis. Curr. Environ. Health Rep. 2022, 9, 490–501. [Google Scholar] [CrossRef] [PubMed]
- Haugen, A.C.; Schug, T.T.; Collman, G.; Heindel, J.J. Evolution of DOHaD: The impact of environmental health sciences. J. Dev. Orig. Health Dis. 2015, 6, 55–64. [Google Scholar] [CrossRef] [PubMed]



| Healthy Controls (n = 113) | Preeclampsia (n = 63) | p-Value | |
|---|---|---|---|
| Maternal age, mean ± SD | 30.5 ± 3.5 | 31.7 ± 4.4 | 0.061 |
| n (%) | |||
| 20–24 y | 5 (4.4%) | 2 (3.2) | 0.218 |
| 25–29 y | 47 (41.6) | 24 (38.1) | |
| 30–34 y | 49 (43.4) | 23 (36.5) | |
| ≥35 y | 12 (10.6) | 14 (22.2) | |
| Prepregnancy BMI Category 1, n (%) | 0.01 | ||
| <18.5 | 22 (19.5) | 7 (11.1) | |
| 18.5–23.9 | 77 (68.1) | 37 (58.7) | |
| ≥24 | 14 (12.4) | 19 (30.2) | |
| Educational level, n (%) | 0.949 | ||
| High school and lower | 40 (35.4) | 22 (34.9) | |
| College and higher | 73 (64.6) | 41 (65.1) | |
| Gravidity, n (%) | 0.438 | ||
| 1 | 60 (53.1) | 31 (49.2) | |
| ≥2 | 53 (46.9) | 32 (50.8) | |
| Parity, n (%) | 0.939 | ||
| Nulliparous | 92 (81.4) | 51 (80.9) | |
| Multiparous | 21 (18.6) | 12 (19.1) | |
| Mode of delivery, n (%) | 0.152 | ||
| Vaginal birth | 91 (80.5) | 56 (88.9) | |
| Cesarean section | 22 (19.5) | 7 (11.1) | |
| Fetal Growth Restriction, n (%) | <0.001 | ||
| YES | 0 | 14 (22.2) | |
| NO | 113 (100) | 49 (77.8) | |
| Gestational Diabetes Mellitus, n (%) | <0.001 | ||
| YES | 0 | 13 (20.6) | |
| NO | 113 (100) | 50 (79.4) | |
| Child Characteristics | |||
| Boy, n (%) | 44(38.9) | 24(38.1) | 0.912 |
| Gestational age, mean± SD, wk | 39.2 ± 0.9 | 36.0 ± 3.0 | <0.001 |
| Preterm birth, n (%) | 0 | 30 (47.6) | <0.001 |
| Birth weight category, n (%) | <0.001 | ||
| <2500 g | 0 | 28 (44.4) | |
| 2500–3999 g | 106 (93.8) | 32 (50.8) | |
| ≥4000 g | 7 (6.2) | 3 (4.8) |
| Healthy Controls (n = 113) | Preeclampsia (n = 63) | p-Value | |
|---|---|---|---|
| Mg | 1809.58 (1500.01, 2340.72) | 1457.59 (1163.36,1833.15) | <0.001 |
| Ca | 3341.57 (2208.47, 6907.35) | 2355.98 (1249.65,3142.29) | <0.001 |
| Cr | 18.65 (10.65, 22.65) | 9.47 (7.25,15.02) | <0.001 |
| Mn | 2.51 (1.7, 3.09) | 1.89 (1.25,2.51) | <0.001 |
| Fe | 1554.66 (1239.73, 1960.29) | 966.88 (827.89,1377.96) | <0.001 |
| Co | 4.83 (0.13, 6.98) | 4.26 (2.49,6.18) | 0.376 |
| Cu | 13.69 (11.29, 17.04) | 11.33 (9.86,13.51) | <0.001 |
| Zn | 165.31 (141.18, 199.22) | 118.1 (97.75,139.53) | <0.001 |
| Se | 3.21 (2.56, 4.15) | 2.46 (2.08,2.84) | <0.001 |
| Cd | 0.24 (0.17,0.36) | 0.21 (0.15,2.35) | 0.397 |
| As | 0.34 (0.29,0.39) | 0.24 (0.19,0.28) | <0.001 |
| Preeclampsia without FGR * n = 49 | Preeclampsia with FGR * n = 14 | p-Value | |
|---|---|---|---|
| Mg | 1496.13 (1199.6, 1897.06) | 1278.40 (923.33, 1703.87) | 0.079 |
| Ca | 2419.17 (1399.99, 3369.36) | 1648.74 (762.83, 2363.44) | 0.055 |
| Cr | 9.59 (7.51, 16.37) | 8.42 (6.74, 11.79) | 0.209 |
| Mn | 1.95 (1.35, 2.51) | 1.82 (1.15, 2.43) | 0.608 |
| Fe | 1055.93 (883.22, 1435.87) | 806.10 (647.66, 894.21) | <0.001 |
| Co | 4.26 (2.28, 6.69) | 4.21 (3.11, 5.71) | 0.869 |
| Cu | 11.37 (10, 13.3) | 10.77 (8.42, 13.54) | 0.418 |
| Zn | 118.39 (98.69, 142.76) | 109.96 (76.45, 128.68) | 0.150 |
| Se | 2.47 (2.18, 2.84) | 2.25 (1.59, 2.74) | 0.203 |
| Cd | 0.22 (0.15, 2.35) | 0.20 (0.17, 1.38) | 0.647 |
| As | 0.23 (0.19, 0.29) | 0.25 (0.19, 0.28) | 0.504 |
| Term Preeclampsia n = 33 | Preterm Preeclampsia * n = 20 | Extremely Preterm Preeclampsia * n = 10 | p-Value | |
|---|---|---|---|---|
| Mg | 1437.01 (1166.51, 1757.01) | 1645.19 (1160.97, 1846.6) | 1472.48 (1226.08, 1820.85) | 0.928 |
| Ca | 2457.94 (1687.26, 3598.42) | 2006.48 (762.83, 2692.06) | 2335.17 (883.41, 2990.36) | 0.159 |
| Cr | 8.66 (7.22, 13.45) | 9.41 (7.32, 17.79) | 12.6 (8.46, 19.08) | 0.399 |
| Mn | 1.89 (1.16, 2.31) | 1.91 (1.2, 2.69) | 2.36 (1.86, 2.69) | 0.342 |
| Fe | 1064.32 (894.21, 1453.42) | 923.98 (789.85, 1130.09) | 826.86 (706.09, 1006.56) | 0.032 |
| Co | 4.44 (2.28, 6.69) | 3.44 (1.39, 5.26) | 5.12 (2.93, 5.76) | 0.388 |
| Cu | 10.82 (9.53, 13.51) | 11.48 (10.3, 13.53) | 10.15 (9.88, 12.74) | 0.699 |
| Zn | 115.98 (92.23, 136.54) | 126.45 (98.94, 163.39) | 123.07 (106.05, 138.17) | 0.350 |
| Se | 2.46 (2.08, 2.89) | 2.45 (2.13, 2.82) | 2.48 (1.9, 2.74) | 0.895 |
| Cd | 0.20 (0.14, 6.94) | 0.21 (0.19, 0.95) | 0.27 (0.17, 0.28) | 0.839 |
| As | 0.22 (0.19, 0.27) | 0.26 (0.2, 0.3) | 0.28 (0.26, 0.31) | 0.075 |
| Model 1 * | Model 2 † | |||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value | |||
| Mg | 0.99 | (0.99, 1.00) | <0.001 | 0.99 | (0.99, 1.00) | <0.001 |
| Ca | 0.94 | (0.90, 0.98) | 0.006 | 0.99 | (0.96,1.03) | 0.760 |
| Cr | 0.95 | (0.93, 0.97) | <0.001 | 0.90 | (0.85, 0.95) | <0.001 |
| Mn | 0.75 | (0.66, 0.86) | <0.001 | 0.83 | (0.59,1.17) | 0.278 |
| Fe | 0.99 | (0.99, 1.00) | <0.001 | 0.99 | (0.99, 1.00) | <0.001 |
| Co | 0.93 | (0.87, 0.98) | 0.013 | 0.99 | (0.88, 1.11) | 0.821 |
| Cu | 0.95 | (0.93, 0.97) | <0.001 | 0.92 | (0.84, 1.01) | 0.088 |
| Zn | 0.99 | (0.99, 1.00) | <0.001 | 0.98 | (0.97, 0.99) | <0.001 |
| Se | 0.78 | (0.70, 0.86) | <0.001 | 0.50 | (0.33, 0.77) | 0.002 |
| Cd | 0.98 | (0.89, 1.08) | 0.661 | 1.08 | (0.95, 1.23) | 0.222 |
| As | 0.26 | (0.10, 0.68) | 0.006 | 0.66 | (0.31, 1.40) | 0.276 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hao, Y.; Yu, W.; Wu, J.; Yue, Y.; Wu, Y.; Huang, H.; Wu, W. Reduction in Placental Metal and Metalloid in Preeclampsia: A Case–Control Study. Nutrients 2024, 16, 769. https://doi.org/10.3390/nu16060769
Hao Y, Yu W, Wu J, Yue Y, Wu Y, Huang H, Wu W. Reduction in Placental Metal and Metalloid in Preeclampsia: A Case–Control Study. Nutrients. 2024; 16(6):769. https://doi.org/10.3390/nu16060769
Chicago/Turabian StyleHao, Yanhui, Wen Yu, Jiaying Wu, Yingyu Yue, Yanting Wu, Hefeng Huang, and Weibin Wu. 2024. "Reduction in Placental Metal and Metalloid in Preeclampsia: A Case–Control Study" Nutrients 16, no. 6: 769. https://doi.org/10.3390/nu16060769