Association between Different Types of Plant-Based Diets and Risk of Dyslipidemia: A Prospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Cohort
2.2. Assessment of Plant-Based Diet Index Score
2.3. Measurements
2.4. Ascertainment of Dyslipidemia
2.5. Assessment of Covariates
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jellinger, P.S.; Handelsman, Y.; Rosenblit, P.D.; Bloomgarden, Z.T.; Fonseca, V.A.; Garber, A.J.; Grunberger, G.; Guerin, C.K.; Bell, D.S.H.; Mechanick, J.I.; et al. American Association of Clinical Endogcrinologists and American College of Endocrinology Guidelines for Mangeament of Dyslipidemia and Prevention of Cardiovascular Disease. Endocr. Pract. 2017, 23, 1–87. [Google Scholar]
- Lin, C.-F.; Chang, Y.-H.; Chien, S.-C.; Lin, Y.-H.; Yeh, H.-Y. Epidemiology of dyslipidemia in the Asia Pacific region. Int. J. Gerontol. 2018, 12, 2–6. [Google Scholar] [CrossRef]
- Satija, A.; Hu, F.B. Plant-based diets and cardiovascular health. Trends Cardiovasc. Med. 2018, 28, 437–441. [Google Scholar] [CrossRef]
- Ferdowsian, H.R.; Barnard, N.D. Effects of plant-based diets on plasma lipids. Am. J. Cardiol. 2009, 104, 947–956. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Zheng, J.; Yang, B.; Jiang, J.; Fu, Y.; Li, D. Effects of Vegetarian Diets on Blood Lipids: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Am. Heart Assoc. 2015, 4, e002408. [Google Scholar] [CrossRef] [Green Version]
- Yokoyama, Y.; Nishimura, K.; Barnard, N.D.; Takegami, M.; Watanabe, M.; Sekikawa, A.; Okamura, T.; Miyamoto, Y. Vegetarian diets and blood pressure: A meta-analysis. JAMA Intern. Med. 2014, 174, 577–587. [Google Scholar] [CrossRef]
- Zhang, Z.; Wang, J.; Chen, S.; Wei, Z.; Li, Z.; Zhao, S.; Lu, W. Comparison of vegetarian diets and omnivorous diets on plasma level of HDL-c: A meta-analysis. PLoS ONE 2014, 9, e92609. [Google Scholar] [CrossRef]
- Picasso, M.C.; Lo-Tayraco, J.A.; Ramos-Villanueva, J.M.; Pasupuleti, V.; Hernandez, A.V. Effect of vegetarian diets on the presentation of metabolic syndrome or its components: A systematic review and meta-analysis. Clin. Nutr. 2019, 38, 1117–1132. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.; Rebholz, C.M.; Garcia-Larsen, V.; Steffen, L.M.; Coresh, J.; Caulfield, L.E. Operational Differences in Plant-Based Diet Indices Affect the Ability to Detect Associations with Incident Hypertension in Middle-Aged US Adults. J. Nutr. 2020, 150, 842–850. [Google Scholar] [CrossRef]
- Satija, A.; Bhupathiraju, S.N.; Rimm, E.B.; Spiegelman, D.; Chiuve, S.E.; Borgi, L.; Willett, W.C.; Manson, J.E.; Sun, Q.; Hu, F.B. Plant-Based Dietary Patterns and Incidence of Type 2 Diabetes in US Men and Women: Results from Three Prospective Cohort Studies. PLoS Med. 2016, 13, e1002039. [Google Scholar] [CrossRef] [Green Version]
- Satija, A.; Bhupathiraju, S.N.; Spiegelman, D.; Chiuve, S.E.; Manson, J.E.; Willett, W.; Rexrode, K.M.; Rimm, E.B.; Hu, F.B. Healthful and Unhealthful Plant-Based Diets and the Risk of Coronary Heart Disease in U.S. Adults. J. Am. Coll. Cardiol. 2017, 70, 411–422. [Google Scholar] [CrossRef]
- Satija, A.; Malik, V.; Rimm, E.B.; Sacks, F.; Willett, W.; Hu, F.B. Changes in intake of plant-based diets and weight change: Results from 3 prospective cohort studies. Am. J. Clin. Nutr. 2019, 110, 574–582. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.; Caulfield, L.E.; Garcia-Larsen, V.; Steffen, L.M.; Grams, M.E.; Coresh, J.; Rebholz, C.M. Plant-Based Diets and Incident CKD and Kidney Function. Clin. J. Am. Soc. Nephrol. 2019, 14, 682–691. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Micha, R.; Khatibzadeh, S.; Shi, P.; Andrews, K.G.; Engell, R.E.; Mozaffarian, D. Global, regional and national consumption of major food groups in 1990 and 2010: A systematic analysis including 266 country-specific nutrition surveys worldwide. BMJ Open 2015, 5, e008705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, S.Y.; Murphy, S.P.; Wilkens, L.R.; Yamamoto, J.F.; Sharma, S.; Hankin, J.H.; Henderson, B.E.; Kolonel, L.N. Dietary patterns using the Food Guide Pyramid groups are associated with sociodemographic and lifestyle factors: The multiethnic cohort study. J. Nutr. 2005, 135, 843–849. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, Y.; Han, B.G. Cohort Profile: The Korean Genome and Epidemiology Study (KoGES) Consortium. Int. J. Epidemiol. 2017, 46, e20. [Google Scholar] [CrossRef]
- Ahn, Y.; Kwon, E.; Shim, J.; Park, M.; Joo, Y.; Kimm, K.; Park, C.; Kim, D. Validation and reproducibility of food frequency questionnaire for Korean genome epidemiologic study. Eur. J. Clin. Nutr. 2007, 61, 1435–1441. [Google Scholar] [CrossRef] [PubMed]
- Hu, F.B.; Stampfer, M.J.; Rimm, E.; Ascherio, A.; Rosner, B.A.; Spiegelman, D.; Willett, W.C. Dietary fat and coronary heart disease: A comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am. J. Epidemiol. 1999, 149, 531–540. [Google Scholar] [CrossRef] [Green Version]
- Lim, M.; Kim, J. Association between fruit and vegetable consumption and risk of metabolic syndrome determined using the Korean Genome and Epidemiology Study (KoGES). Eur. J. Nutr. 2019, 59, 1–12. [Google Scholar] [CrossRef]
- The Korean Nutrition Society. Food composition table. In Recommended Dietary Allowances for Koreans, 7th ed.; The Joongangcopy: Seoul, Korea, 2000. [Google Scholar]
- Kang, Y.J.; Wang, H.W.; Cheon, S.Y.; Lee, H.J.; Hwang, K.M.; Yoon, H.S. Associations of obesity and dyslipidemia with intake of sodium, fat, and sugar among Koreans: A qualitative systematic review. Clin. Nutr Res. 2016, 5, 290–304. [Google Scholar] [CrossRef]
- Kim, D.; Kim, J. Dairy consumption is associated with a lower incidence of the metabolic syndrome in middle-aged and older Korean adults: The Korean Genome and Epidemiology Study (KoGES). Br. J. Nutr. 2017, 117, 148–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.J.; Yang, J.H.; Kim, J.; Cho, L.Y.; Park, B.; Ma, S.H.; Song, S.H.; Min, W.K.; Kim, S.S.; Park, M.S.; et al. Reliability of quadruplicated serological parameters in the korean genome and epidemiology study. Epidemiol. Health 2011, 33, e2011004. [Google Scholar] [CrossRef] [PubMed]
- Rhee, E.-J.; Kim, H.C.; Kim, J.H.; Lee, E.Y.; Kim, B.J.; Kim, E.M.; Song, Y.; Lim, J.H.; Kim, H.J.; Choi, S. 2018 Guidelines for the management of dyslipidemia in Korea. Korean J. Intern. Med. 2019, 34, 723–771. [Google Scholar] [CrossRef] [Green Version]
- Lee, K.; Giovannucci, E.L.; Kim, J. The effect of smoking and sex on the association between long-term alcohol consumption and metabolic syndrome in middle-aged and older population. J. Epidemiol. 2020. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R., Jr.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of physical activities: An update of activity codes and MET intensities. Med. Sci. Sports Exerc. 2000, 32, S498–S504. [Google Scholar] [CrossRef] [Green Version]
- Jian, Z.H.; Chiang, Y.C.; Lung, C.C.; Ho, C.C.; Ko, P.C.; Ndi Nfor, O.; Chang, H.C.; Liaw, Y.C.; Liang, Y.C.; Liaw, Y.P. Vegetarian diet and cholesterol and TAG levels by gender. Public Health Nutr. 2015, 18, 721–726. [Google Scholar] [CrossRef] [Green Version]
- Schoenfeld, D. Partial residuals for the proportional hazards regression model. Biometrika 1982, 69, 239–241. [Google Scholar] [CrossRef]
- Yokoyama, Y.; Levin, S.M.; Barnard, N.D. Association between plant-based diets and plasma lipids: A systematic review and meta-analysis. Nutr. Rev. 2017, 75, 683–698. [Google Scholar] [CrossRef]
- Jenkins, D.J.; Wong, J.M.; Kendall, C.W.; Esfahani, A.; Ng, V.W.; Leong, T.C.; Faulkner, D.A.; Vidgen, E.; Greaves, K.A.; Paul, G.; et al. The effect of a plant-based low-carbohydrate (“Eco-Atkins”) diet on body weight and blood lipid concentrations in hyperlipidemic subjects. Arch. Intern. Med. 2009, 169, 1046–1054. [Google Scholar] [CrossRef] [Green Version]
- Hu, F.B.; Stampfer, M.J.; Manson, J.E.; Rimm, E.; Colditz, G.A.; Rosner, B.A.; Hennekens, C.H.; Willett, W.C. Dietary fat intake and the risk of coronary heart disease in women. N. Engl. J. Med. 1997, 337, 1491–1499. [Google Scholar] [CrossRef]
- Brown, L.; Rosner, B.; Willett, W.W.; Sacks, F.M. Cholesterol-lowering effects of dietary fiber: A meta-analysis. Am. J. Clin. Nutr. 1999, 69, 30–42. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, D.J.; Kendall, C.W.; Jackson, C.J.; Connelly, P.W.; Parker, T.; Faulkner, D.; Vidgen, E.; Cunnane, S.C.; Leiter, L.A.; Josse, R.G. Effects of high- and low-isoflavone soyfoods on blood lipids, oxidized LDL, homocysteine, and blood pressure in hyperlipidemic men and women. Am. J. Clin. Nutr. 2002, 76, 365–372. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Quiñones, M.; Miguel, M.; Aleixandre, A. The polyphenols, naturally occurring compounds with beneficial effects on cardiovascular disease. Nutr. Hosp. 2012, 27, 76–89. [Google Scholar]
- Hiza, H.A.; Casavale, K.O.; Guenther, P.M.; Davis, C.A. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J. Acad. Nutr. Diet. 2013, 113, 297–306. [Google Scholar] [CrossRef]
- Vitale, M.; Masulli, M.; Cocozza, S.; Anichini, R.; Babini, A.C.; Boemi, M.; Bonora, E.; Buzzetti, R.; Carpinteri, R.; Caselli, C.; et al. Sex differences in food choices, adherence to dietary recommendations and plasma lipid profile in type 2 diabetes—The TOSCA.IT study. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 879–885. [Google Scholar] [CrossRef] [PubMed]
- Gylling, H.; Strandberg, T.E.; Kovanen, P.T.; Simonen, P. Lowering Low-Density Lipoprotein Cholesterol Concentration with Plant Stanol Esters to Reduce the Risk of Atherosclerotic Cardiovascular Disease Events at a Population Level: A Critical Discussion. Nutrients 2020, 12, 2346. [Google Scholar] [CrossRef]
- Lee, J.; Kim, J. Egg consumption is associated with a lower risk of type 2 diabetes in middle-aged and older men. Nutr. Res. Pract. 2018, 12, 396–405. [Google Scholar] [CrossRef]
- Song, S.; Lee, J.E.; Song, W.O.; Paik, H.Y.; Song, Y. Carbohydrate intake and refined-grain consumption are associated with metabolic syndrome in the Korean adult population. J. Acad. Nutr. Diet. 2014, 114, 54–62. [Google Scholar] [CrossRef]
- Song, S.; Song, W.O.; Song, Y. Dietary carbohydrate and fat intakes are differentially associated with lipid abnormalities in Korean adults. J. Clin. Lipidol. 2017, 11, 338–347. [Google Scholar] [CrossRef]

| Q1 | Q2 | Q3 | Q4 | Q5 | ||
|---|---|---|---|---|---|---|
| Overall Plant-Based Diet Index | ||||||
| Sample size, n | 886 | 934 | 1038 | 826 | 823 | |
| Median score (range) | 44 (32–46) | 48 (47–49) | 51 (50–52) | 54 (53–55) | 58 (56–71) | |
| Female, n (%) | 488 (55.1) | 535 (57.3) | 609 (58.7) | 490 (59.3) | 519 (63.1) | |
| Age, years | 49.9 (8.6) | 50.9 (8.9) | 51.9 (9.1) | 52.4 (8.7) | 53.7 (9.1) | |
| Residential location, n (%) | ||||||
| Rural, Ansung | 400 (45.2) | 436 (46.7) | 515 (49.6) | 425 (51.5) | 482 (58.6) | |
| Urban, Ansan | 486 (54.8) | 498 (53.3) | 523 (50.4) | 401 (48.5) | 341 (41.4) | |
| Edu Education level, n (%) | ||||||
| ≤6 years | 215 (24.3) | 283 (30.3) | 333 (32.1) | 292 (35.4) | 350 (42.5) | |
| 7–12 years | 518 (58.5) | 519 (55.6) | 591 (56.9) | 446 (54.0) | 411 (49.9) | |
| >12 years | 153 (17.2) | 132 (14.1) | 114 (11.0) | 88 (10.6) | 62 (7.6) | |
| Pack-years of cigarettes, pack/year | 7.9 ± 13.9 | 8.2 ± 15.9 | 7.8 ± 15.4 | 7.8 ± 14.9 | 8.1 ± 16.1 | |
| Alcohol intake, g/day | 10.0 ± 21.0 | 9.7 ± 22.0 | 8.9 ± 19.7 | 7.4 ± 16.6 | 7.4 ± 20.8 | |
| Body Mass Index, kg/m2 | 23.9 ± 3.0 | 23.9 ± 3.0 | 24.0 ± 3.2 | 23.9 ± 3.3 | 24.3 ± 3.2 | |
| Physical activity, MET/day | 21.7 ± 14.8 | 23.2 ± 15.0 | 23.6 ± 15.2 | 25.1 ± 15.6 | 26.2 ± 15.8 | |
| Total energy intake, kcal/day | 2045 ± 696 | 1955 ± 636 | 1907 ± 597 | 1912 ± 588 | 1846 ± 589 | |
| Triglycerides, mmol/L | 1.2 ± 0.4 | 1.2 ± 0.4 | 1.2 ± 0.4 | 1.2 ± 0.4 | 1.2 ± 0.4 | |
| LDL-C, mmol/L | 3.0 ± 0.6 | 2.9 ± 0.7 | 3.0 ± 0.7 | 2.9 ± 0.7 | 2.9 ± 0.6 | |
| HDL-C, mmol/L | 1.4 ± 0.3 | 1.4 ± 0.3 | 1.4 ± 0.3 | 1.4 ± 0.3 | 1.4 ± 0.2 | |
| Total cholesterol, mmol/L | 4.9 ± 0.7 | 4.9 ± 0.7 | 4.9 ± 0.7 | 4.9 ± 0.7 | 4.9 ± 0.7 | |
| Healthy plant food, servings/day | 9.4 ± 4.7 | 10.5 ± 4.7 | 10.9 ± 5.0 | 12.1 ± 4.9 | 12.8 ± 5.1 | |
| Less healthy plant food, servings/day | 6.3 ± 2.7 | 6.7 ± 2.8 | 7.0 ± 2.9 | 7.4 ± 3.0 | 7.8 ± 3.1 | |
| Animal food, servings/day | 3.9 ± 2.7 | 3.4 ± 1.9 | 3.1 ± 1.8 | 3.0 ± 1.7 | 2.4 ± 1.5 | |
| Healthful plant-based diet index | ||||||
| Sample size, n | 890 | 959 | 788 | 982 | 888 | |
| Median score (range) | 43 (30~45) | 48 (46~49) | 51 (50~52) | 54 (53~56) | 59 (57~73) | |
| Female, n (%) | 409 (46.0) | 507 (52.9) | 457 (58.0) | 622 (63.3) | 888 (72.8) | |
| Age, years | 49.0 (8.3) | 51.2 (8.9) | 51.8 (9.0) | 52.7 (9.0) | 53.6 (9.0) | |
| Residential location, n (%) | ||||||
| Rural, Ansung | 293 (32.9) | 458 (47.8) | 426 (54.1) | 557 (56.7) | 524 (59.0) | |
| Urban, Ansan | 597 (67.1) | 501 (52.2) | 362 (45.9) | 425 (43.3) | 364 (41.0) | |
| Education level, n (%) | ||||||
| ≤6 years | 188 (21.1) | 274 (28.6) | 263 (33.4) | 371 (37.8) | 377 (42.5) | |
| 7–12 years | 543 (61.0) | 562 (58.6) | 428 (54.3) | 505 (51.4) | 447 (50.3) | |
| >12 years | 159 (17.9) | 123 (12.8) | 97 (12.3) | 106 (10.8) | 64 (7.2) | |
| Pack-years of cigarettes, pack/year | 10.2 ± 16.2 | 8.8 ± 14.9 | 8.1 ± 15.9 | 7.0 ± 13.8 | 5.7 ± 15.2 | |
| Alcohol intake, g/day | 11.6 ± 22.2 | 9.7 ± 20.7 | 8.7 ± 19.6 | 7.3 ± 17.3 | 6.6 ± 20.4 | |
| Body Mass Index, kg/m2 | 24.1 ± 3.0 | 23.8 ± 3.0 | 23.8 ± 3.1 | 24.1 ± 3.3 | 24.2 ± 3.3 | |
| Physical activity, MET/day | 21.6 ± 14.3 | 23.4 ± 15.8 | 25.0 ± 15.0 | 24.6 ± 15.6 | 25.0 ± 15.5 | |
| Total energy intake, kcal/day | 1929 ± 607 | 2007 ± 647 | 1952 ± 630 | 1888 ± 609 | 1894 ± 629 | |
| Triglycerides, mmol/L | 1.2 ± 0.4 | 1.2 ± 0.4 | 1.2 ± 0.4 | 1.2 ± 0.4 | 1.2 ± 0.4 | |
| LDL-C, mmol/L | 3.0 ± 0.6 | 3.0 ± 0.6 | 2.9 ± 0.7 | 2.9 ± 0.7 | 2.9 ± 0.7 | |
| HDL-C, mmol/L | 1.4 ± 0.2 | 1.4 ± 0.3 | 1.4 ± 0.3 | 1.4 ± 0.3 | 1.4 ± 0.3 | |
| Total cholesterol, mmol/L | 5.0 ± 0.7 | 4.9 ± 0.7 | 4.9 ± 0.7 | 4.9 ± 0.7 | 4.8 ± 0.7 | |
| Healthy plant food, servings/day | 9.2 ± 4.2 | 10.9 ± 5.4 | 11.1 ± 5.0 | 11.5 ± 4.9 | 12.6 ± 5.0 | |
| Less healthy plant food, servings/day | 8.4 ± 3.0 | 7.8 ± 2.8 | 7.2 ± 2.9 | 6.3 ± 2.5 | 5.4 ± 2.5 | |
| Animal food, servings/day | 3.8 ± 1.9 | 3.7 ± 2.1 | 3.3 ± 2.1 | 2.8 ± 1.6 | 2.3 ± 1.5 | |
| Unhealthful plant-based diet index | ||||||
| Sample size, n | 902 | 885 | 995 | 955 | 770 | |
| Median score (range) | 44 (30–46) | 49 (47–50) | 52 (51–54) | 57 (55–59) | 62 (60–75) | |
| Female, n (%) | 642 (71.2) | 535 (60.5) | 565 (56.8) | 485 (50.8) | 414 (53.8) | |
| Age, years | 48.7 (7.8) | 50.1 (8.4) | 51.8 (8.9) | 52.7 (9.2) | 55.4 (9.1) | |
| Residential location, n (%) | ||||||
| Rural, Ansung | 248 (27.5) | 339 (38.3) | 488 (49.1) | 588 (61.6) | 595 (77.3) | |
| Urban, Ansan | 654 (72.5) | 546 (61.7) | 507 (50.9) | 367 (38.4) | 175 (22.7) | |
| Education level, n (%) | ||||||
| ≤6 years | 132 (14.6) | 223 (25.2) | 331 (33.3) | 387 (40.5) | 400 (52.0) | |
| 7–12 years | 595 (66.0) | 529 (59.8) | 547 (55.0) | 483 (50.6) | 331 (43.0) | |
| >12 years | 175 (19.4) | 133 (15.0) | 117 (11.7) | 85 (8.9) | 39 (5.0) | |
| Pack-years of cigarettes, pack/year | 5.0 ± 12.6 | 7.6 ± 14.4 | 8.0 ± 15.2 | 9.7 ± 16.6 | 9.6 ± 16.8 | |
| Alcohol intake, g/day | 6.7 ± 16.3 | 8.9 ± 19.5 | 9.4 ± 21.3 | 10.2 ± 23.3 | 8.4 ± 19.3 | |
| Body Mass Index, kg/m2 | 24.1 ± 3.1 | 24.2 ± 3.2 | 24.2 ± 3.1 | 23.9 ± 3.1 | 23.8 ± 3.3 | |
| Physical activity, MET/day | 20.6 ± 12.7 | 22.9 ± 14.2 | 23.9 ± 16.1 | 25.8 ± 16.1 | 26.8 ± 16.8 | |
| Total energy intake, kcal/day | 2075 ± 583 | 2054 ± 633 | 1931 ± 648 | 1875 ± 626 | 1707 ± 556 | |
| Triglycerides, mmol/L | 1.1 ± 0.4 | 1.2 ± 0.4 | 1.2 ± 0.4 | 1.2 ± 0.4 | 1.3 ± 0.4 | |
| LDL-C, mmol/L | 2.9 ± 0.6 | 3.0 ± 0.6 | 3.0 ± 0.6 | 2.9 ± 0.7 | 2.9 ± 0.7 | |
| HDL-C, mmol/L | 1.4 ± 0.3 | 1.4 ± 0.3 | 1.4 ± 0.3 | 1.4 ± 0.3 | 1.4 ± 0.3 | |
| Total cholesterol, mmol/L | 4.9 ± 0.7 | 4.9 ± 0.7 | 4.9 ± 0.7 | 4.9 ± 0.7 | 4.8 ± 0.7 | |
| Healthy plant food, servings/day | 14.7 ± 5.0 | 12.8 ± 4.7 | 11.1 ± 4.3 | 9.3 ± 3.7 | 7.0 ± 3.5 | |
| Less healthy plant food, servings/day | 5.9 ± 2.5 | 6.6 ± 2.8 | 7.1 ± 3.0 | 7.5 ± 3.0 | 8.0 ± 3.0 | |
| Animal food, servings/day | 4.5 ± 2.1 | 3.8 ± 1.9 | 3.2 ± 1.6 | 2.5 ± 1.5 | 1.7 ± 1.2 | |
| Overall Plant-Based Diet Index | Healthful Plant-Based Diet Index | Unhealthful Plant-Based Diet Index | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | Q1 | Q2 | Q3 | Q4 | Q5 | Q1 | Q2 | Q3 | Q4 | Q5 | |
| No of participants (no of cases) | 886 (602) | 934 (635) | 1038 (668) | 826 (538) | 823 (552) | 890 (617) | 959 (639) | 788 (516) | 982 (646) | 888 (577) | 902 (560) | 885 (559) | 995 (657) | 955 (672) | 770 (547) |
| Person years | 5392 | 5798 | 7059 | 5489 | 5576 | 4628 | 6204 | 5371 | 6843 | 6268 | 6673 | 6168 | 6351 | 5894 | 4228 |
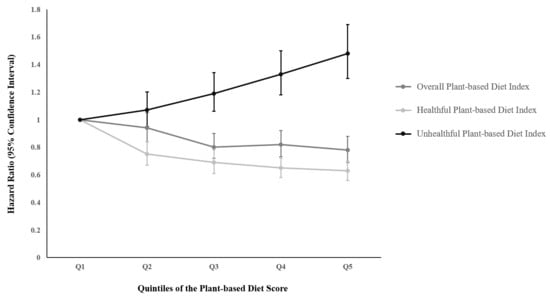
| Model 1 a | 1.00 | 0.95 (0.85–1.06) | 0.82 (0.73–0.91) | 0.83 (0.74–0.94) | 0.82 (0.73–0.93) | 1.00 | 0.75 (0.67–0.84) | 0.68 (0.61–0.77) | 0.66 (0.59–0.74) | 0.63 (0.56–0.71) | 1.00 | 1.07 (0.95–1.21) | 1.19 (1.06–1.33) | 1.30 (1.16–1.45) | 1.43 (1.27–1.62) |
| P-trend | <0.0001 | <0.0001 | <0.0001 | ||||||||||||
| Model 2 b | 1.00 | 0.94 (0.84–1.05) | 0.80 (0.72–0.90) | 0.82 (0.73–0.92) | 0.78 (0.69–0.88) | 1.00 | 0.75 (0.67–0.84) | 0.69 (0.61–0.78) | 0.65 (0.58–0.72) | 0.63 (0.56–0.70) | 1.00 | 1.07 (0.95–1.20) | 1.19 (1.06–1.34) | 1.33 (1.18–1.50) | 1.48 (1.30–1.69) |
| P-trend | <0.0001 | <0.0001 | <0.0001 | ||||||||||||
| P-interaction for sex | 0.8170 | 0.2439 | 0.1897 | ||||||||||||
| Per SD c | 0.91 (0.87–0.94) | 0.84 (0.81–0.88) | 1.16 (1.11–1.21) | ||||||||||||
| Overall Plant-Based Diet Index | Healthful Plant-Based Diet Index | Unhealthful Plant-Based Diet Index | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | Q1 | Q2 | Q3 | Q4 | Q5 | Q1 | Q2 | Q3 | Q4 | Q5 | |
| Hypertriglyceridemia | |||||||||||||||
| Men | |||||||||||||||
| No of participants (no of cases) | 608 (202) | 526 (163) | 646 (193) | 515 (135) | 508 (129) | 590 (220) | 599 (177) | 521 (143) | 577 (147) | 516 (135) | 600 (164) | 538 (162) | 611 (176) | 528 (167) | 526 (153) |
| Model a | 1.00 | 0.93 (0.76–1.14) | 0.90 (0.74–1.09) | 0.81 (0.65–1.01) | 0.75 (0.60–0.94) | 1.00 | 0.69 (0.56–0.84) | 0.62 (0.50–0.76) | 0.58 (0.47–0.71) | 0.61 (0.49–0.76) | 1.00 | 1.24 (0.99–1.54) | 1.17 (0.94–1.46) | 1.44 (1.14–1.80) | 1.33 (1.04–1.69) |
| P-trend | 0.0056 | <0.0001 | 0.0092 | ||||||||||||
| Women | |||||||||||||||
| No of participants (no of cases) | 703 (171) | 733 (167) | 833 (207) | 638 (157) | 663 (180) | 704 (190) | 736 (178) | 651 (154) | 771 (181) | 708 (179) | 772 (159) | 686 (153) | 756 (188) | 605 (162) | 748 (220) |
| Model | 1.00 | 0.88 (0.71–1.08) | 0.91 (0.74–1.11) | 0.90 (0.72–1.12) | 0.92 (0.74–1.14) | 1.00 | 0.81 (0.66–0.99) | 0.76 (0.62–0.95) | 0.69 (0.56–0.85) | 0.76 (0.62–0.93) | 1.00 | 1.14 (0.91–1.42) | 1.28 (1.03–1.60) | 1.34 (1.07–1.69) | 1.60 (1.27–2.01) |
| P-trend | 0.6063 | 0.0037 | <0.0001 | ||||||||||||
| Hypercholesterolemia | |||||||||||||||
| Men | |||||||||||||||
| No of participants (no of cases) | 686 (111) | 653 (78) | 736 (77) | 621 (80) | 626 (64) | 666 (105) | 740 (92) | 815 (75) | 669 (77) | 632 (61) | 716 (90) | 629 (75) | 723 (94) | 630 (73) | 624 (78) |
| Model | 1.00 | 0.73 (0.55–0.98) | 0.63 (0.47–0.84) | 0.82 (0.61–1.09) | 0.67 (0.49–0.91) | 1.00 | 0.75 (0.56–0.99) | 0.74 (0.55–1.00) | 0.68 (0.50–0.91) | 0.58 (0.42–0.80) | 1.00 | 1.05 (0.77–1.43) | 1.27 (0.95–1.71) | 1.30 (0.94–1.79) | 1.62 (1.15–2.27) |
| P-trend | 0.0319 | 0.0011 | 0.0036 | ||||||||||||
| Women | |||||||||||||||
| No of participants (no of cases) | 516 (130) | 552 (145) | 604 (116) | 487 (106) | 482 (95) | 505 (136) | 561 (132) | 496 (115) | 578 (121) | 501 (88) | 571 (128) | 499 (120) | 578 (130) | 452 (108) | 541 (106) |
| Model | 1.00 | 1.01 (0.80–1.28) | 0.71 (0.55–0.91) | 0.81 (0.63–1.05) | 0.71 (0.54–0.93) | 1.00 | 0.79 (0.62–1.00) | 0.82 (0.64–1.05) | 0.66 (0.52–0.85) | 0.54 (0.41–0.71) | 1.00 | 1.25 (0.97–1.60) | 1.20 (0.94–1.55) | 1.36 (1.04–1.78) | 1.28 (0.96–1.71) |
| P-trend | 0.0028 | <0.0001 | 0.0582 | ||||||||||||
| Low HDL-C | |||||||||||||||
| Men | |||||||||||||||
| No of participants (no of cases) | 552 (303) | 528 (276) | 626 (336) | 482 (251) | 493 (277) | 553 (316) | 560 (298) | 501 (263) | 567 (279) | 500 (287) | 562 (280) | 525 (275) | 591 (305) | 484 (277) | 519 (306) |
| Model | 1.00 | 0.93 (0.79–1.09) | 0.90 (0.77–1.05) | 0.85 (0.72–1.01) | 0.86 (0.72–1.01) | 1.00 | 0.74 (0.63–0.87) | 0.67 (0.57–0.80) | 0.57 (0.48–0.67) | 0.70 (0.59–0.82) | 1.00 | 1.09 (0.92–1.29) | 1.09 (0.92–1.29) | 1.24 (1.04–1.48) | 1.32 (1.10–1.59) |
| P-trend | 0.0365 | <0.0001 | 0.0014 | ||||||||||||
| Women | |||||||||||||||
| No of participants (no of cases) | 669 (303) | 719 (332) | 810 (359) | 594 (280) | 637 (282) | 676 (305) | 705 (322) | 613 (282) | 737 (324) | 698 (323) | 710 (249) | 646 (257) | 749 (340) | 611 (344) | 713 (376) |
| Model | 1.00 | 0.95 (0.81–1.10) | 0.84 (0.72–0.98) | 0.87 (0.74–1.03) | 0.76 (0.64–0.89) | 1.00 | 0.88 (0.75–1.03) | 0.80 (0.68–0.95) | 0.71 (0.60–0.83) | 0.73 (0.62–0.86) | 1.00 | 1.18 (0.99–1.40) | 1.37 (1.15–1.62) | 1.68 (1.41–2.00) | 1.72 (1.44–2.05) |
| P-trend | 0.0006 | <0.0001 | <0.0001 | ||||||||||||
| High LDL-C | |||||||||||||||
| Men | |||||||||||||||
| No of participants (no of cases) | 698 (126) | 674 (86) | 757 (100) | 647 (97) | 644 (68) | 696 (134) | 732 (111) | 638 (84) | 703 (87) | 651 (61) | 737 (105) | 649 (101) | 751 (95) | 636 (83) | 647 (93) |
| Model | 1.00 | 0.70 (0.53–0.92) | 0.69 (0.53–0.89) | 0.84 (0.64–1.10) | 0.58 (0.43–0.78) | 1.00 | 0.75 (0.58–0.97) | 0.63 (0.48–0.83) | 0.57 (0.43–0.74) | 0.43 (0.32–0.59) | 1.00 | 1.20 (0.91–1.58) | 1.10 (0.83–1.46) | 1.29 (0.95–1.74) | 1.69 (1.24–2.32) |
| P-trend | 0.0059 | <0.0001 | 0.0034 | ||||||||||||
| Women | |||||||||||||||
| No of participants (no of cases) | 755 (224) | 771 (198) | 858 (220) | 649 (169) | 723 (186) | 722 (221) | 798 (235) | 665 (168) | 814 (194) | 757 (179) | 791 (205) | 724 (217) | 826 (221) | 642 (168) | 773 (186) |
| Model | 1.00 | 0.81 (0.67–0.99) | 0.78 (0.65–0.94) | 0.81 (0.66–0.99) | 0.79 (0.65–0.97) | 1.00 | 0.88 (0.73–1.06) | 0.76 (0.62–0.93) | 0.67 (0.55–0.81) | 0.66 (0.54–0.81) | 1.00 | 1.30 (1.07–1.57) | 1.21 (1.00–1.47) | 1.26 (1.01–1.56) | 1.28 (1.02–1.59) |
| P-trend | 0.0360 | <0.0001 | 0.0656 | ||||||||||||
| High total cholesterol/HDL-C | |||||||||||||||
| Men | |||||||||||||||
| No of participants (no of cases) | 514 (213) | 534 (189) | 627 (243) | 530 (196) | 517 (198) | 513 (246) | 574 (218) | 547 (168) | 578 (214) | 510 (193) | 510 (186) | 546 (202) | 508 (197) | 600 (245) | 558 (209) |
| Model | 1.00 | 0.84 (0.69–1.02) | 0.94 (0.78–1.13) | 0.88 (0.72–1.07) | 1.01 (0.83–1.23) | 1.00 | 0.69 (0.58–0.83) | 0.53 (0.43–0.64) | 0.60 (0.50–0.73) | 0.65 (0.54–0.79) | 1.00 | 1.02 (0.84–1.25) | 1.18 (0.96–1.45) | 1.32 (1.08–1.61) | 1.26 (1.01–1.56) |
| P-trend | 0.8018 | <0.0001 | 0.0035 | ||||||||||||
| Women | |||||||||||||||
| No of participants (no of cases) | 675 (228) | 714 (255) | 787 (291) | 617 (274) | 633 (283) | 668 (236) | 720 (283) | 620 (251) | 718 (264) | 700 (297) | 612 (196) | 603 (185) | 727 (275) | 749 (322) | 735 (353) |
| Model | 1.00 | 1.02 (0.85–1.22) | 1.02 (0.86–1.22) | 1.30 (1.09–1.55) | 1.21 (1.01–1.45) | 1.00 | 1.09 (0.91–1.29) | 1.05 (0.88–1.26) | 0.87 (0.73–1.04) | 1.01 (0.85–1.20) | 1.00 | 1.02 (0.84–1.25) | 1.33 (1.10–1.61) | 1.60 (1.32–1.93) | 2.12 (1.74–2.58) |
| P-trend | 0.0020 | 0.2770 | <0.0001 | ||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K.; Kim, H.; Rebholz, C.M.; Kim, J. Association between Different Types of Plant-Based Diets and Risk of Dyslipidemia: A Prospective Cohort Study. Nutrients 2021, 13, 220. https://doi.org/10.3390/nu13010220
Lee K, Kim H, Rebholz CM, Kim J. Association between Different Types of Plant-Based Diets and Risk of Dyslipidemia: A Prospective Cohort Study. Nutrients. 2021; 13(1):220. https://doi.org/10.3390/nu13010220
Chicago/Turabian StyleLee, Kyueun, Hyunju Kim, Casey M. Rebholz, and Jihye Kim. 2021. "Association between Different Types of Plant-Based Diets and Risk of Dyslipidemia: A Prospective Cohort Study" Nutrients 13, no. 1: 220. https://doi.org/10.3390/nu13010220