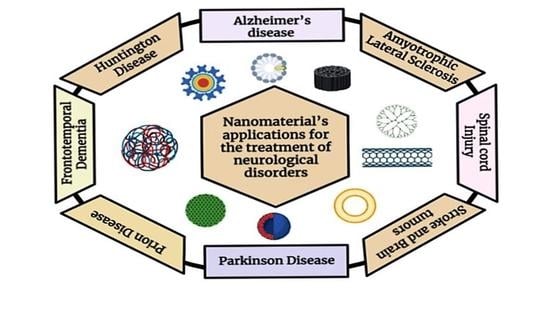
Applications of Various Types of Nanomaterials for the Treatment of Neurological Disorders
Abstract
:1. Introduction
2. Types of Nanomaterials Used for the Treatment of Neurological Disorders
2.1. Quantum Dots
2.2. Metallic Nanoparticles
2.3. Dendrimers
2.4. Carbon Nanotubes
2.5. Polymeric Nanoparticles
2.6. Liposomes
2.7. Micelles
3. Nanomaterials for the Treatment of Neurodegenerative Diseases
3.1. Alzheimer’s Disease (AD)

3.2. Parkinson Disease
3.3. Huntington Disease
3.4. Amyotrophic Lateral Sclerosis (ALS)
3.5. Frontotemporal Dementia
3.6. Prion Disease
3.7. Spinal Cord Injury
3.8. Stroke
3.9. Brain Tumors
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Re, F.; Gregori, M.; Masserini, M. Nanotechnology for neurodegenerative disorders. Maturitas 2012, 73, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Gitler, A.D.; Dhillon, P.; Shorter, J. Neurodegenerative Disease: Models, Mechanisms, and a New Hope; The Company of Biologists Ltd.: Cambridge, UK, 2017; Volume 10, pp. 499–502. [Google Scholar]
- WHO. The Top 10 Causes of Death-WHO|World Health Organization; WHO: Geneva, Switzerland, 2020; Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 12 January 2022).
- Ramos-Cabrer, P.; Agulla, J.; Argibay, B.; Pérez-Mato, M.; Castillo, J. Serial MRI study of the enhanced therapeutic effects of liposome-encapsulated citicoline in cerebral ischemia. Int. J. Pharm. 2011, 405, 228–233. [Google Scholar] [CrossRef] [PubMed]
- El-aziz, E.A.E.-d.A.; Elgayar, S.F.; Mady, F.M.; Abourehab, M.A.; Hasan, O.A.; Reda, L.M.; Alaaeldin, E. The Potential of Optimized Liposomes in Enhancement of Cytotoxicity and Apoptosis of Encapsulated Egyptian Propolis on Hep-2 Cell Line. Pharmaceutics 2021, 13, 2184. [Google Scholar] [CrossRef]
- Abbott, N.J.; Patabendige, A.A.; Dolman, D.E.; Yusof, S.R.; Begley, D.J. Structure and function of the blood–brain barrier. Neurobiol. Dis. 2010, 37, 13–25. [Google Scholar] [CrossRef] [PubMed]
- Tosi, G.; Costantino, L.; Ruozi, B.; Forni, F.; Vandelli, M.A. Polymeric nanoparticles for the drug delivery to the central nervous system. Expert Opin. Drug Deliv. 2008, 5, 155–174. [Google Scholar] [CrossRef]
- Cano, A.; Sánchez-López, E.; Ettcheto, M.; López-Machado, A.; Espina, M.; Souto, E.B.; Galindo, R.; Camins, A.; García, M.L.; Turowski, P. Current advances in the development of novel polymeric nanoparticles for the treatment of neurodegenerative diseases. Nanomedicine 2020, 15, 1239–1261. [Google Scholar] [CrossRef]
- Zhang, W.; Sigdel, G.; Mintz, K.J.; Seven, E.S.; Zhou, Y.; Wang, C.; Leblanc, R.M. Carbon dots: A future Blood–Brain Barrier penetrating nanomedicine and drug nanocarrier. Int. J. Nanomed. 2021, 16, 5003. [Google Scholar] [CrossRef]
- Ashrafizadeh, M.; Mohammadinejad, R.; Kailasa, S.K.; Ahmadi, Z.; Afshar, E.G.; Pardakhty, A. Carbon dots as versatile nanoarchitectures for the treatment of neurological disorders and their theranostic applications: A review. Adv. Colloid Interface Sci. 2020, 278, 102123. [Google Scholar] [CrossRef]
- Sim, T.M.; Tarini, D.; Dheen, S.T.; Bay, B.H.; Srinivasan, D.K. Nanoparticle-based technology approaches to the management of neurological disorders. Int. J. Mol. Sci. 2020, 21, 6070. [Google Scholar] [CrossRef]
- Huang, M.; Gu, X.; Gao, X. Nanotherapeutic strategies for the treatment of neurodegenerative diseases. In Brain Targeted Drug Delivery System; Elsevier: Amsterdam, The Netherlands, 2019; pp. 321–356. [Google Scholar]
- Ilyas, M.; Waris, A.; Khan, A.U.; Zamel, D.; Yar, L.; Baset, A.; Muhaymin, A.; Khan, S.; Ali, A.; Ahmad, A. Biological synthesis of titanium dioxide nanoparticles from plants and microorganisms and their potential biomedical applications. Inorg. Chem. Commun. 2021, 133, 108968. [Google Scholar] [CrossRef]
- Hussain, Z.; Thu, H.E.; Elsayed, I.; Abourehab, M.A.; Khan, S.; Sohail, M.; Sarfraz, R.M.; Farooq, M.A. Nano-scaled materials may induce severe neurotoxicity upon chronic exposure to brain tissues: A critical appraisal and recent updates on predisposing factors, underlying mechanism, and future prospects. J. Control. Release 2020, 328, 873–894. [Google Scholar] [CrossRef] [PubMed]
- Gregori, M.; Masserini, M.; Mancini, S. Nanomedicine for the treatment of Alzheimer’s disease. Nanomedicine 2015, 10, 1203–1218. [Google Scholar] [CrossRef]
- Villalva, M.D.; Agarwal, V.; Ulanova, M.; Sachdev, P.S.; Braidy, N. Quantum dots as a theranostic approach in Alzheimer’s disease: A systematic review. Nanomedicine 2021, 16, 1595–1611. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, S.; Shende, P. Cyclodextrins-modified metallic nanoparticles for effective cancer therapy. J. Control. Release 2021, 339, 41–50. [Google Scholar] [CrossRef]
- Modi, G.; Pillay, V.; Choonara, Y.E. Advances in the treatment of neurodegenerative disorders employing nanotechnology. Ann. N. Y. Acad. Sci. 2010, 1184, 154–172. [Google Scholar] [CrossRef] [PubMed]
- Hussain, Z.; Rahim, M.A.; Jan, N.; Shah, H.; Rawas-Qalaji, M.; Khan, S.; Sohail, M.; Thu, H.E.; Ramli, N.A.; Sarfraz, R.M. Cell membrane cloaked nanomedicines for bio-imaging and immunotherapy of cancer: Improved pharmacokinetics, cell internalization and anticancer efficacy. J. Control. Release 2021, 335, 130–157. [Google Scholar] [CrossRef]
- Wu, T.; Zhang, T.; Chen, Y.; Tang, M. Research advances on potential neurotoxicity of quantum dots. J. Appl. Toxicol. 2016, 36, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Utkin, Y.N. Brain and quantum dots: Benefits of nanotechnology for healthy and diseased brain. Cent. Nerv. Syst. Agents Med. Chem. (Former. Curr. Med. Chem.-Cent. Nerv. Syst. Agents) 2018, 18, 193–205. [Google Scholar] [CrossRef]
- Aswathy, R.G.; Yoshida, Y.; Maekawa, T.; Kumar, D.S. Near-infrared quantum dots for deep tissue imaging. Anal. Bioanal. Chem. 2010, 397, 1417–1435. [Google Scholar] [CrossRef]
- Liu, J.; Erogbogbo, F.; Yong, K.-T.; Ye, L.; Liu, J.; Hu, R.; Chen, H.; Hu, Y.; Yang, Y.; Yang, J. Assessing clinical prospects of silicon quantum dots: Studies in mice and monkeys. ACS Nano 2013, 7, 7303–7310. [Google Scholar] [CrossRef]
- Shang, W.; Zhang, X.; Zhang, M.; Fan, Z.; Sun, Y.; Han, M.; Fan, L. The uptake mechanism and biocompatibility of graphene quantum dots with human neural stem cells. Nanoscale 2014, 6, 5799–5806. [Google Scholar] [CrossRef]
- Ren, C.; Hu, X.; Zhou, Q. Graphene oxide quantum dots reduce oxidative stress and inhibit neurotoxicity in vitro and in vivo through catalase-like activity and metabolic regulation. Adv. Sci. 2018, 5, 1700595. [Google Scholar] [CrossRef] [PubMed]
- Tian, X.; Fan, T.; Zhao, W.; Abbas, G.; Han, B.; Zhang, K.; Li, N.; Liu, N.; Liang, W.; Huang, H. Recent advances in the development of nanomedicines for the treatment of ischemic stroke. Bioact. Mater. 2021, 6, 2854–2869. [Google Scholar] [CrossRef]
- Xu, G.; Mahajan, S.; Roy, I.; Yong, K.-T. Theranostic quantum dots for crossing blood–brain barrier in vitro and providing therapy of HIV-associated encephalopathy. Front. Pharmacol. 2013, 4, 140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walters, R.; Medintz, I.L.; Delehanty, J.B.; Stewart, M.H.; Susumu, K.; Huston, A.L.; Dawson, P.E.; Dawson, G. The role of negative charge in the delivery of quantum dots to neurons. Asn Neuro 2015, 7, 1759091415592389. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kang, I.; Yoo, J.M.; Kim, D.; Kim, J.; Cho, M.K.; Lee, S.-E.; Kim, D.J.; Lee, B.-C.; Lee, J.Y.; Kim, J.-J. Graphene quantum dots alleviate impaired functions in Niemann-pick disease type C in vivo. Nano Lett. 2021, 21, 2339–2346. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Wang, Y.; Lin, F.; Liu, Y.; Gu, R.; Liu, W.; Xiao, C. Selenium-doped carbon quantum dots efficiently ameliorate secondary spinal cord injury via scavenging reactive oxygen species. Int. J. Nanomed. 2020, 15, 10113. [Google Scholar] [CrossRef] [PubMed]
- Dong, J.; Tao, L.; Abourehab, M.A.; Hussain, Z. Design and development of novel hyaluronate-modified nanoparticles for combo-delivery of curcumin and alendronate: Fabrication, characterization, and cellular and molecular evidences of enhanced bone regeneration. Int. J. Biol. Macromol. 2018, 116, 1268–1281. [Google Scholar] [CrossRef]
- Sintov, A.; Velasco-Aguirre, C.; Gallardo-Toledo, E.; Araya, E.; Kogan, M. Metal nanoparticles as targeted carriers circumventing the blood–brain barrier. Int. Rev. Neurobiol. 2016, 130, 199–227. [Google Scholar]
- Waris, A.; Din, M.; Ali, A.; Afridi, S.; Baset, A.; Khan, A.U.; Ali, M. Green fabrication of Co and Co3O4 nanoparticles and their biomedical applications: A review. Open Life Sci. 2021, 16, 14–30. [Google Scholar] [CrossRef] [PubMed]
- Waris, A.; Din, M.; Ali, A.; Ali, M.; Afridi, S.; Baset, A.; Khan, A.U. A comprehensive review of green synthesis of copper oxide nanoparticles and their diverse biomedical applications. Inorgan. Chem. Commun. 2021, 123, 1387–7003. [Google Scholar] [CrossRef]
- Dawoud, M.; Abourehab, M.A.; Abdou, R. Monoolein cubic nanoparticles as novel carriers for docetaxel. J. Drug Deliv. Sci. Technol. 2020, 56, 101501. [Google Scholar] [CrossRef]
- Mody, V.V.; Siwale, R.; Singh, A.; Mody, H.R. Introduction to metallic nanoparticles. J. Pharm. Bioallied Sci. 2010, 2, 282. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.; Chen, A.; Zhang, Y.; Wang, J.; Shao, L.; Wei, L. Central nervous system toxicity of metallic nanoparticles. Int. J. Nanomed. 2015, 10, 4321. [Google Scholar]
- Sriramoju, B.; Kanwar, R.K.; Kanwar, J.R. Nanomedicine based nanoparticles for neurological disorders. Curr. Med. Chem. 2014, 21, 4154–4168. [Google Scholar] [CrossRef]
- Ayaz, M.; Ovais, M.; Ahmad, I.; Sadiq, A.; Khalil, A.T.; Ullah, F. Biosynthesized metal nanoparticles as potential Alzheimer’s disease therapeutics. In Metal Nanoparticles for Drug Delivery and Diagnostic Applications; Elsevier: Amsterdam, The Netherlands, 2020; pp. 31–42. [Google Scholar]
- Waris, A.; Ali, M.; Khan, A.U.; Ali, A.; Baset, A. Role of nanotechnology in diagnosing and treating COVID-19 during the pandemic. Int. J. Clin. Virol. 2020, 4, 65–70. [Google Scholar]
- Shan, D.; Ma, C.; Yang, J. Enabling biodegradable functional biomaterials for the management of neurological disorders. Adv. Drug Deliv. Rev. 2019, 148, 219–238. [Google Scholar] [CrossRef]
- Muheem, A.; Jahangir, M.A.; Jaiswal, C.P.; Jafar, M.; Ahmad, M.Z.; Ahmad, J.; Warsi, M.H. Recent patents, regulatory issues, and toxicity of nanoparticles in neuronal disorders. Curr. Drug Metab. 2021, 22, 263–279. [Google Scholar] [CrossRef]
- Fischer, M.; Vögtle, F. Dendrimers: From design to application—A progress report. Angew. Chem. Int. Ed. 1999, 38, 884–905. [Google Scholar] [CrossRef]
- Boas, U.; Heegaard, P.M. Dendrimers in drug research. Chem. Soc. Rev. 2004, 33, 43–63. [Google Scholar] [CrossRef]
- Kannan, R.; Nance, E.; Kannan, S.; Tomalia, D.A. Emerging concepts in dendrimer-based nanomedicine: From design principles to clinical applications. J. Intern. Med. 2014, 276, 579–617. [Google Scholar] [CrossRef] [PubMed]
- Vögtle, F.; Gestermann, S.; Hesse, R.; Schwierz, H.; Windisch, B. Functional dendrimers. Prog. Polym. Sci. 2000, 25, 987–1041. [Google Scholar] [CrossRef]
- Svenson, S.; Tomalia, D.A. Dendrimers in biomedical applications—Reflections on the field. Adv. Drug Deliv. Rev. 2012, 64, 102–115. [Google Scholar] [CrossRef]
- Beg, S.; Samad, A.; Alam, M.I.; Nazish, I. Dendrimers as novel systems for delivery of neuropharmaceuticals to the brain. CNS Neurol. Disord.-Drug Targets (Former. Curr. Drug Targets-CNS Neurol. Disord.) 2011, 10, 576–588. [Google Scholar]
- Serramía, M.J.; Álvarez, S.; Fuentes-Paniagua, E.; Clemente, M.I.; Sánchez-Nieves, J.; Gómez, R.; de la Mata, J.; Muñoz-Fernández, M.Á. In vivo delivery of siRNA to the brain by carbosilane dendrimer. J. Control. Release 2015, 200, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Porterfield, J.E.; Smith, E.; Sharma, R.; Kannan, S.; Kannan, R.M. Effect of mannose targeting of hydroxyl PAMAM dendrimers on cellular and organ biodistribution in a neonatal brain injury model. J. Control. Release 2018, 283, 175–189. [Google Scholar] [CrossRef] [PubMed]
- Yellepeddi, V.K.; Mohammadpour, R.; Kambhampati, S.P.; Sayre, C.; Mishra, M.K.; Kannan, R.M.; Ghandehari, H. Pediatric oral formulation of dendrimer-N-acetyl-l-cysteine conjugates for the treatment of neuroinflammation. Int. J. Pharm. 2018, 545, 113–116. [Google Scholar] [CrossRef]
- Sharma, R.; Kim, S.-Y.; Sharma, A.; Zhang, Z.; Kambhampati, S.P.; Kannan, S.; Kannan, R.M. Activated microglia targeting dendrimer–minocycline conjugate as therapeutics for neuroinflammation. Bioconjug. Chem. 2017, 28, 2874–2886. [Google Scholar] [CrossRef]
- Nance, E.; Zhang, F.; Mishra, M.K.; Zhang, Z.; Kambhampati, S.P.; Kannan, R.M.; Kannan, S. Nanoscale effects in dendrimer-mediated targeting of neuroinflammation. Biomaterials 2016, 101, 96–107. [Google Scholar] [CrossRef] [Green Version]
- Leiro, V.; Duque Santos, S.; Lopes, C.D.; Paula Pêgo, A. Dendrimers as powerful building blocks in central nervous system disease: Headed for successful nanomedicine. Adv. Funct. Mater. 2018, 28, 1700313. [Google Scholar] [CrossRef] [Green Version]
- Mignani, S.; Bryszewska, M.; Zablocka, M.; Klajnert-Maculewicz, B.; Cladera, J.; Shcharbin, D.; Majoral, J.-P. Can dendrimer based nanoparticles fight neurodegenerative diseases? Current situation versus other established approaches. Prog. Polym. Sci. 2017, 64, 23–51. [Google Scholar] [CrossRef]
- Xiang, C.; Zhang, Y.; Guo, W.; Liang, X.-J. Biomimetic carbon nanotubes for neurological disease therapeutics as inherent medication. Acta Pharm. Sin. B 2020, 10, 239–248. [Google Scholar] [CrossRef] [PubMed]
- Mbayachi, V.B.; Ndayiragije, E.; Sammani, T.; Taj, S.; Mbuta, E.R. Graphene synthesis, characterization and its applications: A review. Results Chem. 2021, 3, 100163. [Google Scholar] [CrossRef]
- Komane, P.P.; Choonara, Y.E.; du Toit, L.C.; Kumar, P.; Kondiah, P.P.; Modi, G.; Pillay, V. Diagnosis and treatment of neurological and ischemic disorders employing carbon nanotube technology. J. Nanomater. 2016, 2016, 9417874. [Google Scholar] [CrossRef] [Green Version]
- Nunes, A.; Al-Jamal, K.; Nakajima, T.; Hariz, M.; Kostarelos, K. Application of carbon nanotubes in neurology: Clinical perspectives and toxicological risks. Arch. Toxicol. 2012, 86, 1009–1020. [Google Scholar] [CrossRef]
- Belyanskaya, L.; Weigel, S.; Hirsch, C.; Tobler, U.; Krug, H.F.; Wick, P. Effects of carbon nanotubes on primary neurons and glial cells. Neurotoxicology 2009, 30, 702–711. [Google Scholar] [CrossRef]
- Fabbro, A.; Prato, M.; Ballerini, L. Carbon nanotubes in neuroregeneration and repair. Adv. Drug Deliv. Rev. 2013, 65, 2034–2044. [Google Scholar] [CrossRef]
- Jain, S.; Singh, S.R.; Pillai, S. Toxicity issues related to biomedical applications of carbon nanotubes. J. Nanomed. Nanotechol. 2012, 3, 2. [Google Scholar] [CrossRef]
- Gustavsson, P.; Hedmer, M.; Rissler, J. Carbon Nanotubes-Exposure, Toxicology and Protective Measures in the Work Environment; The Swedish Work Environment Authority: Arbetsmiljöverket, Sweden, 2011.
- Hussain, Z.; Pandey, M.; Thu, H.E.; Kaur, T.; Jia, G.W.; Ying, P.C.; Xian, T.M.; Abourehab, M.A. Hyaluronic acid functionalization improves dermal targeting of polymeric nanoparticles for management of burn wounds: In vitro, ex vivo and in vivo evaluations. Biomed. Pharmacother. 2022, 150, 112992. [Google Scholar] [CrossRef]
- Tiwari, S.B.; Amiji, M.M. A review of nanocarrier-based CNS delivery systems. Curr. Drug Deliv. 2006, 3, 219–232. [Google Scholar] [CrossRef]
- Pardridge, W.M. Blood-brain barrier drug targeting: The future of brain drug development. Mol. Interv. 2003, 3, 90. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Garcia, E.; Andrieux, K.; Gil, S.; Couvreur, P. Colloidal carriers and blood–brain barrier (BBB) translocation: A way to deliver drugs to the brain? Int. J. Pharm. 2005, 298, 274–292. [Google Scholar] [CrossRef]
- Palmer, A.M. The role of the blood brain barrier in neurodegenerative disorders and their treatment. J. Alzheimer’s Dis. 2011, 24, 643–656. [Google Scholar] [CrossRef]
- Nagpal, K.; Singh, S.K.; Mishra, D.N. Chitosan nanoparticles: A promising system in novel drug delivery. Chem. Pharm. Bull. 2010, 58, 1423–1430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhaskar, S.; Tian, F.; Stoeger, T.; Kreyling, W.; de la Fuente, J.M.; Grazú, V.; Borm, P.; Estrada, G.; Ntziachristos, V.; Razansky, D. Multifunctional Nanocarriers for diagnostics, drug delivery and targeted treatment across blood-brain barrier: Perspectives on tracking and neuroimaging. Part. Fibre Toxicol. 2010, 7, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, L.-S.; Chuang, M.-C.; Ho, J.-a.A. Nanotheranostics—A review of recent publications. Int. J. Nanomed. 2012, 7, 4679. [Google Scholar]
- Shim, M.S.; Kwon, Y.J. Stimuli-responsive polymers and nanomaterials for gene delivery and imaging applications. Adv. Drug Deliv. Rev. 2012, 64, 1046–1059. [Google Scholar] [CrossRef]
- Fontes, M.A.P.; Vaz, G.C.; Cardoso, T.Z.D.; de Oliveira, M.F.; Campagnole-Santos, M.J.; Dos Santos, R.A.S.; Sharma, N.M.; Patel, K.P.; Frézard, F. GABA-containing liposomes: Neuroscience applications and translational perspectives for targeting neurological diseases. Nanomed. Nanotechnol. Biol. Med. 2018, 14, 781–788. [Google Scholar] [CrossRef]
- Frézard, F.; dos Santos, R.A.; Fontes, M.A. Liposome-encapsulated neuropeptides for site-specific microinjection. In Neuropeptides; Springer: Berlin/Heidelberg, Germany, 2011; pp. 343–355. [Google Scholar]
- Ulrich, A.S. Biophysical aspects of using liposomes as delivery vehicles. Biosci. Rep. 2002, 22, 129–150. [Google Scholar] [CrossRef]
- Spuch, C.; Navarro, C. Liposomes for targeted delivery of active agents against neurodegenerative diseases (Alzheimer’s disease and Parkinson’s disease). J. Drug Deliv. 2011, 2011, 469679. [Google Scholar] [CrossRef] [Green Version]
- Zheng, C. Gradient copolymer micelles: An introduction to structures as well as structural transitions. Soft Matter 2019, 15, 5357–5370. [Google Scholar] [CrossRef] [PubMed]
- Abourehab, M.A.; Ahmed, O.A.; Balata, G.F.; Almalki, W.H. Self-assembled biodegradable polymeric micelles to improve dapoxetine delivery across the blood-brain barrier. Int. J. Nanomed. 2018, 13, 3679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Croy, S.; Kwon, G. Polymeric micelles for drug delivery. Curr. Pharm. Des. 2006, 12, 4669–4684. [Google Scholar] [CrossRef] [PubMed]
- Cosgrove, K.P.; Mazure, C.M.; Staley, J.K. Evolving knowledge of sex differences in brain structure, function, and chemistry. Biol. Psychiatry 2007, 62, 847–855. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monteiro, A.F.M.; Viana, J.D.O.; Nayarisseri, A.; Zondegoumba, E.N.; Mendonça Junior, F.J.B.; Scotti, M.T.; Scotti, L. Computational studies applied to flavonoids against alzheimer’s and parkinson’s diseases. Oxidative Med. Cell. Longev. 2018, 2018, 7912765. [Google Scholar] [CrossRef]
- Islam, A.; Saif Khandker, S.; Alam, F.; Khalil, I.; Amjad Kamal, M.; Hua Gan, S. Alzheimer’s disease and natural products: Future regimens emerging from nature. Curr. Top. Med. Chem. 2017, 17, 1408–1428. [Google Scholar] [CrossRef]
- Patel, M.M.; Patel, B.M. Crossing the blood–brain barrier: Recent advances in drug delivery to the brain. CNS Drugs 2017, 31, 109–133. [Google Scholar] [CrossRef]
- Xu, W.; Ling, P.; Zhang, T. Polymeric micelles, a promising drug delivery system to enhance bioavailability of poorly water-soluble drugs. J. Drug Deliv. 2013, 2013, 340315. [Google Scholar] [CrossRef]
- Kumari, S.; Ahsan, S.M.; Kumar, J.M.; Kondapi, A.K.; Rao, N.M. Overcoming blood brain barrier with a dual purpose Temozolomide loaded Lactoferrin nanoparticles for combating glioma (SERP-17-12433). Sci. Rep. 2017, 7, 6602. [Google Scholar] [CrossRef] [Green Version]
- Kumar, A.; Singh, A. A review on Alzheimer’s disease pathophysiology and its management: An update. Pharmacol. Rep. 2015, 67, 195–203. [Google Scholar] [CrossRef]
- Furtado, D.; Björnmalm, M.; Ayton, S.; Bush, A.I.; Kempe, K.; Caruso, F. Overcoming the blood–brain barrier: The role of nanomaterials in treating neurological diseases. Adv. Mater. 2018, 30, 1801362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, A.; Tyson, J.; Patel, S.; Patel, M.; Katakam, S.; Mao, X.; He, W. Emerging Nanotechnology for Treatment of Alzheimer’s and Parkinson’s Disease. Front. Bioeng. Biotechnol. 2021, 9, 672594. [Google Scholar] [CrossRef] [PubMed]
- Sood, S.; Jain, K.; Gowthamarajan, K. Intranasal therapeutic strategies for management of Alzheimer’s disease. J. Drug Target. 2014, 22, 279–294. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, M.; Alam, M.R.; Haider, M.K.; Malik, M.; Kim, D.-K. Alzheimer’s Disease: An Overview of Major Hypotheses and Therapeutic Options in Nanotechnology. Nanomaterials 2021, 11, 59. [Google Scholar] [CrossRef]
- Chen, M.; Du, Z.-Y.; Zheng, X.; Li, D.-L.; Zhou, R.-P.; Zhang, K. Use of curcumin in diagnosis, prevention, and treatment of Alzheimer’s disease. Neural Regen. Res. 2018, 13, 742. [Google Scholar]
- Shabbir, U.; Rubab, M.; Tyagi, A.; Oh, D.-H. Curcumin and its derivatives as theranostic agents in Alzheimer’s disease: The implication of nanotechnology. Int. J. Mol. Sci. 2021, 22, 196. [Google Scholar] [CrossRef]
- Dimov, N.; Kastner, E.; Hussain, M.; Perrie, Y.; Szita, N. Formation and purification of tailored liposomes for drug delivery using a module-based micro continuous-flow system. Sci. Rep. 2017, 7, 12045. [Google Scholar] [CrossRef] [Green Version]
- Bilal, M.; Barani, M.; Sabir, F.; Rahdar, A.; Kyzas, G.Z. Nanomaterials for the treatment and diagnosis of Alzheimer’s disease: An overview. NanoImpact 2020, 20, 100251. [Google Scholar] [CrossRef]
- De Campos, A.M.; Sanchez, A.; Alonso, M.a.J. Chitosan nanoparticles: A new vehicle for the improvement of the delivery of drugs to the ocular surface. Application to cyclosporin A. Int. J. Pharm. 2001, 224, 159–168. [Google Scholar] [CrossRef]
- Fox, L.J.; Richardson, R.M.; Briscoe, W.H. PAMAM dendrimer-cell membrane interactions. Adv. Colloid Interface Sci. 2018, 257, 1–18. [Google Scholar] [CrossRef]
- Song, S.; Wu, J.; Cheng, Y.; Ma, L.; Liu, T.; Liu, J.; Liu, J.; Sotor, J.; Luan, P. Emerging two-dimensional materials-enabled diagnosis and treatments of Alzheimer’s disease: Status and future challenges. Appl. Mater. Today 2021, 23, 101028. [Google Scholar] [CrossRef]
- Park, H.-Y.; Seok, H.-Y.; Park, B.-K.; Kim, S.-H.; Goh, C.-H.; Lee, B.-h.; Lee, C.-H.; Moon, Y.-H. Overexpression of Arabidopsis ZEP enhances tolerance to osmotic stress. Biochem. Biophys. Res. Commun. 2008, 375, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Faiyaz, M.; Ganayee, M.A.; Akhtar, S.; Krishnan, S.; Flora, B.; Dogra, D.; Jha, N.K.; Chellappan, D.K.; Negi, P.; Dua, K. Nanomaterials in Alzheimer’s disease treatment: A comprehensive review. Front. Biosci. (Landmark Ed.) 2021, 26, 851–865. [Google Scholar] [PubMed]
- American Psychiatric Association, A. Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association: Washington, DC, USA, 1980; Volume 3. [Google Scholar]
- Colvert, E.; Tick, B.; McEwen, F.; Stewart, C.; Curran, S.R.; Woodhouse, E.; Gillan, N.; Hallett, V.; Lietz, S.; Garnett, T. Heritability of autism spectrum disorder in a UK population-based twin sample. JAMA Psychiatry 2015, 72, 415–423. [Google Scholar] [CrossRef]
- Hua, X.; Thompson, P.M.; Leow, A.D.; Madsen, S.K.; Caplan, R.; Alger, J.R.; O’Neill, J.; Joshi, K.; Smalley, S.L.; Toga, A.W. Brain growth rate abnormalities visualized in adolescents with autism. Hum. Brain Mapp. 2013, 34, 425–436. [Google Scholar] [CrossRef] [Green Version]
- Moni, M.; Rahman, M.; Begum, M.; Uddin, M.; Ashraf, G.M. Deciphering the Role of Nanoparticle-Based Treatment for Parkinson’s Disease. Curr. Drug Metab. 2021, 22, 550–560. [Google Scholar] [CrossRef]
- Adhikary, R.R.; Sandbhor, P.; Banerjee, R. Nanotechnology platforms in Parkinson’s Disease. ADMET DMPK 2015, 3, 155–181. [Google Scholar] [CrossRef] [Green Version]
- Pardridge, W.M. Molecular Trojan horses for blood–brain barrier drug delivery. Curr. Opin. Pharmacol. 2006, 6, 494–500. [Google Scholar] [CrossRef]
- Pardeshi, C.V.; Belgamwar, V.S.; Surana, S.J. Nanotechnology-Mediated Nose-to-Brain Drug Delivery for Neurodegenerative Disorders. In Nanobiotechnology in Neurodegenerative Diseases; Springer: Berlin/Heidelberg, Germany, 2019; pp. 163–175. [Google Scholar]
- Hu, K.; Shi, Y.; Jiang, W.; Han, J.; Huang, S.; Jiang, X. Lactoferrin conjugated PEG-PLGA nanoparticles for brain delivery: Preparation, characterization and efficacy in Parkinson’s disease. Int. J. Pharm. 2011, 415, 273–283. [Google Scholar] [CrossRef]
- Soto, C.; Pritzkow, S. Protein misfolding, aggregation, and conformational strains in neurodegenerative diseases. Nat. Neurosci. 2018, 21, 1332–1340. [Google Scholar] [CrossRef]
- Ulmer, T.S.; Bax, A.; Cole, N.B.; Nussbaum, R.L. Structure and dynamics of micelle-bound human α-synuclein. J. Biol. Chem. 2005, 280, 9595–9603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alimohammadi, E.; Nikzad, A.; Khedri, M.; Rezaian, M.; Jahromi, A.M.; Rezaei, N.; Maleki, R. Potential treatment of Parkinson’s disease using new-generation carbon nanotubes: A biomolecular in silico study. Nanomedicine 2020, 16, 189–204. [Google Scholar] [CrossRef] [PubMed]
- Gao, G.; Chen, R.; He, M.; Li, J.; Wang, L.; Sun, T. Gold nanoclusters for Parkinson’s disease treatment. Biomaterials 2019, 194, 36–46. [Google Scholar] [CrossRef]
- Walker, F.O. Huntington’s disease. Lancet 2007, 369, 218–228. [Google Scholar] [CrossRef]
- Cong, W.; Bai, R.; Li, Y.-F.; Wang, L.; Chen, C. Selenium nanoparticles as an efficient nanomedicine for the therapy of Huntington’s disease. ACS Appl. Mater. Interfaces 2019, 11, 34725–34735. [Google Scholar] [CrossRef] [PubMed]
- Debnath, K.; Pradhan, N.; Singh, B.K.; Jana, N.R.; Jana, N.R. Poly (trehalose) nanoparticles prevent amyloid aggregation and suppress polyglutamine aggregation in a Huntington’s disease model mouse. ACS Appl. Mater. Interfaces 2017, 9, 24126–24139. [Google Scholar] [CrossRef]
- Cardoso, B.R.; Roberts, B.R.; Bush, A.I.; Hare, D.J. Selenium, selenoproteins and neurodegenerative diseases. Metallomics 2015, 7, 1213–1228. [Google Scholar] [CrossRef] [Green Version]
- An, Z.; Yan, J.; Zhang, Y.; Pei, R. Applications of nanomaterials for scavenging reactive oxygen species in the treatment of central nervous system diseases. J. Mater. Chem. B 2020, 8, 8748–8767. [Google Scholar] [CrossRef]
- Cunha, A.; Gaubert, A.; Latxague, L.; Dehay, B. PLGA-Based nanoparticles for neuroprotective drug delivery in neurodegenerative diseases. Pharmaceutics 2021, 13, 1042. [Google Scholar] [CrossRef]
- Cano, A.; Ettcheto, M.; Espina, M.; Auladell, C.; Folch, J.; Kühne, B.A.; Barenys, M.; Sánchez-López, E.; Souto, E.B.; García, M.L. Epigallocatechin-3-gallate PEGylated poly (lactic-co-glycolic) acid nanoparticles mitigate striatal pathology and motor deficits in 3-nitropropionic acid intoxicated mice. Nanomedicine 2020, 16, 19–35. [Google Scholar] [CrossRef]
- Van Es, M.A.; Hardiman, O.; Chio, A.; Al-Chalabi, A.; Pasterkamp, R.J.; Veldink, J.H.; Van den Berg, L.H. Amyotrophic lateral sclerosis. Lancet 2017, 390, 2084–2098. [Google Scholar] [CrossRef]
- Mazibuko, Z.; Choonara, Y.E.; Kumar, P.; Du Toit, L.C.; Modi, G.; Naidoo, D.; Pillay, V. A review of the potential role of nano-enabled drug delivery technologies in amyotrophic lateral sclerosis: Lessons learned from other neurodegenerative disorders. J. Pharm. Sci. 2015, 104, 1213–1229. [Google Scholar] [CrossRef] [PubMed]
- Bondì, M.L.; Craparo, E.F.; Giammona, G.; Drago, F. Brain-targeted solid lipid nanoparticles containing riluzole: Preparation, characterization and biodistribution. Nanomedicine 2010, 5, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Andaloussi, S.E.; Lakhal, S.; Mäger, I.; Wood, M.J. Exosomes for targeted siRNA delivery across biological barriers. Adv. Drug Deliv. Rev. 2013, 65, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Rayner, S.; Chung, R.; Shi, B.; Liang, X. Advances in nanotechnology-based strategies for the treatments of amyotrophic lateral sclerosis. Mater. Today Bio 2020, 6, 100055. [Google Scholar] [CrossRef]
- Alvarez-Erviti, L.; Seow, Y.; Yin, H.; Betts, C.; Lakhal, S.; Wood, M.J. Delivery of siRNA to the mouse brain by systemic injection of targeted exosomes. Nat. Biotechnol. 2011, 29, 341–345. [Google Scholar] [CrossRef]
- Haney, M.J.; Klyachko, N.L.; Zhao, Y.; Gupta, R.; Plotnikova, E.G.; He, Z.; Patel, T.; Piroyan, A.; Sokolsky, M.; Kabanov, A.V. Exosomes as drug delivery vehicles for Parkinson’s disease therapy. J. Control. Release 2015, 207, 18–30. [Google Scholar] [CrossRef] [Green Version]
- Wiley, N.J.; Madhankumar, A.; Mitchell, R.M.; Neely, E.B.; Rizk, E.; Douds, G.L.; Simmons, Z.; Connor, J.R. Lipopolysaccharide Modified Liposomes for Amyotropic Lateral Sclerosis Therapy: Efficacy in SOD1 Mouse Model. Adv. Nanoparticles 2012, 1, 44–53. [Google Scholar] [CrossRef] [Green Version]
- Shanmukhapuvvada, Y.; Vankayalapati, S. Design and development of riluzole loaded chitosan nanoparticles by emulsification crosslinking. Int. J. Pharm. Pharm. Sci 2012, 4, 244–248. [Google Scholar]
- Nguyen, T.T.; Nguyen, T.T.D.; Vo, T.K.; Nguyen, M.K.; Van Vo, T.; Van Vo, G. Nanotechnology-based drug delivery for central nervous system disorders. Biomed. Pharmacother. 2021, 143, 112117. [Google Scholar] [CrossRef]
- Novak, V.; Rogelj, B.; Župunski, V. Therapeutic potential of polyphenols in amyotrophic lateral sclerosis and frontotemporal dementia. Antioxidants 2021, 10, 1328. [Google Scholar] [CrossRef] [PubMed]
- Tripodo, G.; Chlapanidas, T.; Perteghella, S.; Vigani, B.; Mandracchia, D.; Trapani, A.; Galuzzi, M.; Tosca, M.C.; Antonioli, B.; Gaetani, P. Mesenchymal stromal cells loading curcumin-INVITE-micelles: A drug delivery system for neurodegenerative diseases. Colloids Surf. B Biointerfaces 2015, 125, 300–308. [Google Scholar] [CrossRef] [PubMed]
- Mead, S. Prion disease genetics. Eur. J. Hum. Genet. 2006, 14, 273–281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skinner, P.J.; Kim, H.O.; Bryant, D.; Kinzel, N.J.; Reilly, C.; Priola, S.A.; Ward, A.E.; Goodman, P.A.; Olson, K.; Seelig, D.M. Treatment of prion disease with heterologous prion proteins. PLoS ONE 2015, 10, e0131993. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nirale, P.; Paul, A.; Yadav, K.S. Nanoemulsions for targeting the neurodegenerative diseases: Alzheimer’s, Parkinson’s and Prion’s. Life Sci. 2020, 245, 117394. [Google Scholar] [CrossRef]
- Chountoulesi, M.; Demetzos, C. Promising nanotechnology approaches in treatment of autoimmune diseases of central nervous system. Brain Sci. 2020, 10, 338. [Google Scholar] [CrossRef]
- Maresca, M.; Derghal, A.; Carravagna, C.; Dudin, S.; Fantini, J. Controlled aggregation of adenine by sugars: Physicochemical studies, molecular modelling simulations of sugar–aromatic CH–π stacking interactions, and biological significance. Phys. Chem. Chem. Phys. 2008, 10, 2792–2800. [Google Scholar] [CrossRef]
- El Moustaine, D.; Perrier, V.; Smeller, L.; Lange, R.; Torrent, J. Full-length prion protein aggregates to amyloid fibrils and spherical particles by distinct pathways. FEBS J. 2008, 275, 2021–2031. [Google Scholar] [CrossRef]
- Wei, G.; Su, Z.; Reynolds, N.P.; Arosio, P.; Hamley, I.W.; Gazit, E.; Mezzenga, R. Self-assembling peptide and protein amyloids: From structure to tailored function in nanotechnology. Chem. Soc. Rev. 2017, 46, 4661–4708. [Google Scholar] [CrossRef]
- Li, J.; Cai, S.; Zeng, C.; Chen, L.; Zhao, C.; Huang, Y.; Cai, W. Urinary exosomal vitronectin predicts vesicoureteral reflux in patients with neurogenic bladders and spinal cord injuries. Exp. Ther. Med. 2022, 23, 65. [Google Scholar] [CrossRef]
- Chen, Y.; Tang, Y.; Vogel, L.; DeVivo, M. Causes of spinal cord injury. Top. Spinal Cord Inj. Rehabil. 2013, 19, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zimmermann, R.; Vieira Alves, Y.; Sperling, L.E.; Pranke, P. Nanotechnology for the treatment of spinal cord injury. Tissue Eng. Part B Rev. 2021, 27, 353–365. [Google Scholar] [CrossRef] [PubMed]
- Schaal, S.M.; Garg, M.S.; Ghosh, M.; Lovera, L.; Lopez, M.; Patel, M.; Louro, J.; Patel, S.; Tuesta, L.; Chan, W.-M. The therapeutic profile of rolipram, PDE target and mechanism of action as a neuroprotectant following spinal cord injury. PLoS ONE 2012, 7, e43634. [Google Scholar] [CrossRef] [PubMed]
- Macks, C.; Gwak, S.-J.; Lynn, M.; Lee, J.S. Rolipram-loaded polymeric micelle nanoparticle reduces secondary injury after rat compression spinal cord injury. J. Neurotrauma 2018, 35, 582–592. [Google Scholar] [CrossRef] [PubMed]
- Tyler, J.Y.; Xu, X.-M.; Cheng, J.-X. Nanomedicine for treating spinal cord injury. Nanoscale 2013, 5, 8821–8836. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, T.I.; Hemalatha, S.; Waseem, M. Promising role of nano-encapsulated drugs for spinal cord injury. Mol. Neurobiol. 2020, 57, 1978–1985. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.; Shi, R.; Borgens, R.B. Chitosan produces potent neuroprotection and physiological recovery following traumatic spinal cord injury. J. Exp. Biol. 2010, 213, 1513–1520. [Google Scholar] [CrossRef]
- Brent, J. Current management of ethylene glycol poisoning. Drugs 2001, 61, 979–988. [Google Scholar] [CrossRef]
- Kreuter, J.; Alyautdin, R.N.; Kharkevich, D.A.; Ivanov, A.A. Passage of peptides through the blood-brain barrier with colloidal polymer particles (nanoparticles). Brain Res. 1995, 674, 171–174. [Google Scholar] [CrossRef]
- Alyaudtin, R.N.; Reichel, A.; Löbenberg, R.; Ramge, P.; Kreuter, J.; Begley, D.J. Interaction of poly (butylcyanoacrylate) nanoparticles with the blood-brain barrier in vivo and in vitro. J. Drug Target. 2001, 9, 209–221. [Google Scholar] [CrossRef]
- Ramge, P.; Unger, R.E.; Oltrogge, J.B.; Zenker, D.; Begley, D.; Kreuter, J.; Von Briesen, H. Polysorbate-80 coating enhances uptake of polybutylcyanoacrylate (PBCA)-nanoparticles by human and bovine primary brain capillary endothelial cells. Eur. J. Neurosci. 2000, 12, 1931–1940. [Google Scholar] [CrossRef] [PubMed]
- Amar, S.K.; Anand, U.; Verma, A. Cerebrovascular Imaging in a Rodent Stroke Model. Models Tech. Stroke Biol. 2021, 1, 97–105. [Google Scholar]
- Assunção-Silva, R.; Gomes, E.; Silva, N.; Salgado, A. Nanoengineered biomaterials for spinal cord regeneration. In Nanoengineered Biomaterials for Regenerative Medicine; Elsevier: Amsterdam, The Netherlands, 2019; pp. 167–185. [Google Scholar]
- Astrup, J.; Siesjö, B.K.; Symon, L. Thresholds in cerebral ischemia-the ischemic penumbra. Stroke 1981, 12, 723–725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cook, D.J.; Teves, L.; Tymianski, M. Treatment of stroke with a PSD-95 inhibitor in the gyrencephalic primate brain. Nature 2012, 483, 213–217. [Google Scholar] [CrossRef]
- Sacchetti, M.L. Is it time to definitely abandon neuroprotection in acute ischemic stroke? Am. Heart Assoc. 2008, 39, 1659–1660. [Google Scholar] [CrossRef] [Green Version]
- Kubinová, Š.; Syková, E. Nanotechnology for treatment of stroke and spinal cord injury. Nanomedicine 2010, 5, 99–108. [Google Scholar] [CrossRef]
- Sarmah, D.; Banerjee, M.; Datta, A.; Kalia, K.; Dhar, S.; Yavagal, D.R.; Bhattacharya, P. Nanotechnology in the diagnosis and treatment of stroke. Drug Discov. Today 2021, 26, 585–592. [Google Scholar] [CrossRef]
- Mohan, A.; Narayanan, S.; Balasubramanian, G.; Sethuraman, S.; Krishnan, U.M. Dual drug loaded nanoliposomal chemotherapy: A promising strategy for treatment of head and neck squamous cell carcinoma. Eur. J. Pharm. Biopharm. 2016, 99, 73–83. [Google Scholar] [CrossRef]
- Kaviarasi, S.; Yuba, E.; Harada, A.; Krishnan, U.M. Emerging paradigms in nanotechnology for imaging and treatment of cerebral ischemia. J. Control. Release 2019, 300, 22–45. [Google Scholar] [CrossRef]
- Yan, X.; Scherphof, G.L.; Kamps, J.A. Liposome opsonization. J. Liposome Res. 2005, 15, 109–139. [Google Scholar] [CrossRef]
- Kang, X.; Chen, H.; Li, S.; Jie, L.; Hu, J.; Wang, X.; Qi, J.; Ying, X.; Du, Y. Magnesium lithospermate B loaded PEGylated solid lipid nanoparticles for improved oral bioavailability. Colloids Surf. B Biointerfaces 2018, 161, 597–605. [Google Scholar] [CrossRef] [PubMed]
- Zarhri, Z.; Houmad, M.; Ziat, Y.; El Rhazouani, O.; Slassi, A.; Benyoussef, A.; El Kenz, A. Ab-initio study of magnetism behavior in TiO2 semiconductor with structural defects. J. Magn. Magn. Mater. 2016, 406, 212–216. [Google Scholar] [CrossRef]
- Sarmah, D.; Saraf, J.; Kaur, H.; Pravalika, K.; Tekade, R.K.; Borah, A.; Kalia, K.; Dave, K.R.; Bhattacharya, P. Stroke management: An emerging role of nanotechnology. Micromachines 2017, 8, 262. [Google Scholar] [CrossRef] [Green Version]
- Li, C.; Sun, T.; Jiang, C. Recent advances in nanomedicines for the treatment of ischemic stroke. Acta Pharm. Sin. B 2021, 11, 1767–1788. [Google Scholar] [CrossRef]
- Naccarato, M.; Grandi, F.C.; Dennis, M.; Sandercock, P.A. Physical methods for preventing deep vein thrombosis in stroke. Cochrane Database Syst. Rev. 2010, 8, CD001922. [Google Scholar] [CrossRef]
- Li, H.; Yang, Z.; Tang, Q.; Shi, Z.; Mao, Y. Embolic Stroke Model with Magnetic Nanoparticles. ACS Appl. Mater. Interfaces 2021, 13, 43993–44001. [Google Scholar] [CrossRef] [PubMed]
- Su, M.; Dai, Q.; Chen, C.; Zeng, Y.; Chu, C.; Liu, G. Nano-medicine for thrombosis: A precise diagnosis and treatment strategy. Nano-Micro Lett. 2020, 12, 96. [Google Scholar] [CrossRef] [Green Version]
- Sampetrean, O.; Saya, H. Modeling phenotypes of malignant gliomas. Cancer Sci. 2018, 109, 6–14. [Google Scholar] [CrossRef] [Green Version]
- Wilson, B.; Samanta, M.K.; Santhi, K.; Kumar, K.P.S.; Paramakrishnan, N.; Suresh, B. Poly(n-butylcyanoacrylate) nanoparticles coated with polysorbate 80 for the targeted delivery of rivastigmine into the brain to treat Alzheimer’s disease. Brain Res. 2008, 1200, 159–168. [Google Scholar] [CrossRef]
- Kaushik, A.C.; Bharadwaj, S.; Kumar, S.; Wei, D.-Q. Nano-particle mediated inhibition of Parkinson’s disease using computational biology approach. Sci. Rep. 2018, 8, 9169. [Google Scholar] [CrossRef] [Green Version]
- Cui, Z.; Lockman, P.R.; Atwood, C.S.; Hsu, C.-H.; Gupte, A.; Allen, D.D.; Mumper, R.J. Novel D-penicillamine carrying nanoparticles for metal chelation therapy in Alzheimer’s and other CNS diseases. Eur. J. Pharm. Biopharm. 2005, 59, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Kogan, M.J.; Bastus, N.G.; Amigo, R.; Grillo-Bosch, D.; Araya, E.; Turiel, A.; Labarta, A.; Giralt, E.; Puntes, V.F. Nanoparticle-mediated local and remote manipulation of protein aggregation. Nano Lett. 2006, 6, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Gilert, A.; Machluf, M. Nano to micro delivery systems: Targeting angiogenesis in brain tumors. J. Angiogenesis Res. 2010, 2, 20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jagaran, K.; Singh, M. Nanomedicine for Neurodegenerative Disorders: Focus on Alzheimer’s and Parkinson’s Diseases. Int. J. Mol. Sci. 2021, 22, 9082. [Google Scholar] [CrossRef]
- Gambaryan, P.; Kondrasheva, I.; Severin, E.; Guseva, A.; Kamensky, A. Increasing the Efficiency of Parkinson’s Disease Treatment Using a poly (lactic-co-glycolic acid)(PLGA) Based L-DOPA Delivery System. Exp. Neurobiol. 2014, 23, 246. [Google Scholar] [CrossRef] [Green Version]
- Huang, R.; Boltze, J.; Li, S. Strategies for improved intra-arterial treatments targeting brain tumors: A systematic review. Front. Oncol. 2020, 10, 1443. [Google Scholar] [CrossRef]
- Beccaria, K.; Canney, M.; Bouchoux, G.; Puget, S.; Grill, J.; Carpentier, A. Blood-brain barrier disruption with low-intensity pulsed ultrasound for the treatment of pediatric brain tumors: A review and perspectives. Neurosurg. Focus 2020, 48, E10. [Google Scholar] [CrossRef] [Green Version]
- Reese, T.; Karnovsky, M.J. Fine structural localization of a blood-brain barrier to exogenous peroxidase. J. Cell Biol. 1967, 34, 207–217. [Google Scholar] [CrossRef] [Green Version]
- Chen, E.M.; Quijano, A.R.; Seo, Y.-E.; Jackson, C.; Josowitz, A.D.; Noorbakhsh, S.; Merlettini, A.; Sundaram, R.K.; Focarete, M.L.; Jiang, Z. Biodegradable PEG-poly (ω-pentadecalactone-co-p-dioxanone) nanoparticles for enhanced and sustained drug delivery to treat brain tumors. Biomaterials 2018, 178, 193–203. [Google Scholar] [CrossRef]
- Kozielski, K.L.; Ruiz-Valls, A.; Tzeng, S.Y.; Guerrero-Cázares, H.; Rui, Y.; Li, Y.; Vaughan, H.J.; Gionet-Gonzales, M.; Vantucci, C.; Kim, J. Cancer-selective nanoparticles for combinatorial siRNA delivery to primary human GBM in vitro and in vivo. Biomaterials 2019, 209, 79–87. [Google Scholar] [CrossRef]
- Caruso, G.; Marino, D.; Caffo, M. Nanoparticles and CNS delivery of therapeutic agents in the treatment of primary brain tumors. J. Anal. Oncol. 2014, 3, 105–112. [Google Scholar]
- Sun, X.; Liu, Z.; Welsher, K.; Robinson, J.T.; Goodwin, A.; Zaric, S.; Dai, H. Nano-graphene oxide for cellular imaging and drug delivery. Nano Res. 2008, 1, 203–212. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rehman, F.U. Impact of bioinspired nanotechnology on brain diseases amelioration. Biomed. Lett. 2020, 6, 17–22. [Google Scholar]
- Mukhtar, M.; Bilal, M.; Rahdar, A.; Barani, M.; Arshad, R.; Behl, T.; Brisc, C.; Banica, F.; Bungau, S. Nanomaterials for diagnosis and treatment of brain cancer: Recent updates. Chemosensors 2020, 8, 117. [Google Scholar] [CrossRef]
- Brynskikh, A.M.; Zhao, Y.; Mosley, R.L.; Li, S.; Boska, M.D.; Klyachko, N.L.; Kabanov, A.V.; Gendelman, H.E.; Batrakova, E.V. Macrophage delivery of therapeutic nanozymes in a murine model of Parkinson’s disease. Nanomedicine 2010, 5, 379–396. [Google Scholar] [CrossRef] [Green Version]
- Mukherjee, A.; Madamsetty, V.S.; Paul, M.K.; Mukherjee, S. Recent advancements of nanomedicine towards antiangiogenic therapy in cancer. Int. J. Mol. Sci. 2020, 21, 455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siddiqi, K.S.; Husen, A.; Sohrab, S.S.; Yassin, M.O. Recent status of nanomaterial fabrication and their potential applications in neurological disease management. Nanoscale Res. Lett. 2018, 13, 231. [Google Scholar] [CrossRef]
- De Mendoza, A.E.-H.; Préat, V.; Mollinedo, F.; Blanco-Prieto, M.J. In vitro and in vivo efficacy of edelfosine-loaded lipid nanoparticles against glioma. J. Control. Release 2011, 156, 421–426. [Google Scholar] [CrossRef] [Green Version]
- Caruso, G.; Raudino, G.; Caffo, M. Patented nanomedicines for the treatment of brain tumors. Pharm. Pat. Anal. 2013, 2, 745–754. [Google Scholar] [CrossRef] [Green Version]
- Discher, B.M.; Won, Y.-Y.; Ege, D.S.; Lee, J.C.; Bates, F.S.; Discher, D.E.; Hammer, D.A. Polymersomes: Tough vesicles made from diblock copolymers. Science 1999, 284, 1143–1146. [Google Scholar] [CrossRef] [Green Version]
- Shevtsov, M.; Multhoff, G. Recent developments of magnetic nanoparticles for theranostics of brain tumor. Curr. Drug Metab. 2016, 17, 737–744. [Google Scholar] [CrossRef] [PubMed]
- DeCoteau, W.; Heckman, K.L.; Estevez, A.Y.; Reed, K.J.; Costanzo, W.; Sandford, D.; Studlack, P.; Clauss, J.; Nichols, E.; Lipps, J. Cerium oxide nanoparticles with antioxidant properties ameliorate strength and prolong life in mouse model of amyotrophic lateral sclerosis. Nanomed. Nanotechnol. Biol. Med. 2016, 12, 2311–2320. [Google Scholar] [CrossRef] [PubMed]
- Asil, S.M.; Ahlawat, J.; Barroso, G.G.; Narayan, M. Nanomaterial based drug delivery systems for the treatment of neurodegenerative diseases. Biomater. Sci. 2020, 8, 4109–4128. [Google Scholar] [CrossRef] [PubMed]
- Feigin, V.L.; Nichols, E.; Alam, T.; Bannick, M.S.; Beghi, E.; Blake, N.; Culpepper, W.J.; Dorsey, E.R.; Elbaz, A.; Ellenbogen, R.G. Global, regional, and national burden of neurological disorders, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 459–480. [Google Scholar] [CrossRef] [Green Version]







| Nanomaterials/Nanoparticles Used | Drug Name | Diseases | Year of Approval | Route | References |
|---|---|---|---|---|---|
| PEG-PLGA | Riluzole | Amyotrophic lateral sclerosis (ALS) | 1995 | Orally | [123] |
| Poly(n-butylcyanoacrylate) | Rivastigmine | Alzheimer’s disease | 2000 | Intravenous | [168] |
| CeO2 NP | L-DOPA | Parkinson disease | 2003 | Intranasal | [169] |
| (MPB-PE) and (PDP-PE) couples | D-Penicillamine | Alzheimer’s disease | 2005 | Nasal delivery | [170] |
| Gold Nanocrystals | Molecular surgery | Alzheimer’s disease | 2006 | [171] | |
| Inorganic and metallic nanoparticles | Nanotherm®(MagForce) | Glioblastoma multiform | 2010 | Intravenous injection | [128] |
| Intracerebral Biodegradable gel matrices/Polymer nanoparticles | Temozolomide | - | 2010 | Orally | [172] |
| Liposomes/Microcapsules | lomustine | Brain Tumor | 2010 | Orally | [172] |
| CED/Intracerebral/Intraarterial/Liposomes | Carboplatin | Brain Tumor | 2010 | Intravenous | [172] |
| Polymer NP | Copaxone®/Glatopa (Teva) | Multiple Sclerosis | 2018 | Subcutaneousinjection | [128] |
| Liposomes and polymers | Riluzole | Amyotrophic lateral sclerosis (ALS) | 2019 | Intravenous | [123] |
| Gold nanocrystals | CNM-Au8 | Multiple sclerosis | 2021 | Orally | [173] |
| PLGA | L-DOPA | Parkinson disease | - | Intranasal | [174] |
| Cerium oxide | Photothermal therapy | Stroke | 2021 | - | [26] |
| Thermotherapy and magnetic iron-oxide NPs + reduced dose radiotherapy | Nano-thermotherapy | Glioblastoma multiforme | Phase II clinical trials | Intrathecal | [128] |
| NPS | Mechanism of Action | Disease | Animal Model Used | References |
|---|---|---|---|---|
| Polymeric NPs | Transport vectors/penetrate the cell membrane through endocytosis | Stroke | NA | [184] |
| Micelles | Intravenous delivery/efficient drug delivery | PD | Mouse model | [184] |
| Graphene NPs | Destroy cancer cells | Brain tumors | Chicken embryonic angiogenesis assay | [185] |
| Gold NPs | Improved selectivity to brain | AD | Mice | [186] |
| Carbon NPs | Platelets aggregation/stem cell therapy | Stroke | Rat | [183,187] |
| Silver NPs | Efficient drug delivery | Brain tumors | - | [188] |
| Zinc oxide | Efficient drug delivery | Brain tumors | Mature Rats | [188] |
| dendrimers | Efficient drug delivery | Brain tumors | Mice | [188] |
| Lipid NPs | Accumulation of edelfosine | Brain tumors | Xenograft mouse model of glioma | [189] |
| Theranostic NPs | Improved pharmacokinetics | Brain tumors | - | [190] |
| Cerum oxide | therapeutic effect by acting as redox active agents | ALS | Male and female mice | [191] |
| Magnetic NPs | Regulate the metal homeostasis in the brain, carry a large dose of drug to achieve high local concentration and avoid toxicity, target and detect amyloid plaques in AD | AD/HD/Frontotemporal Dementia | - | [192] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Waris, A.; Ali, A.; Khan, A.U.; Asim, M.; Zamel, D.; Fatima, K.; Raziq, A.; Khan, M.A.; Akbar, N.; Baset, A.; et al. Applications of Various Types of Nanomaterials for the Treatment of Neurological Disorders. Nanomaterials 2022, 12, 2140. https://doi.org/10.3390/nano12132140
Waris A, Ali A, Khan AU, Asim M, Zamel D, Fatima K, Raziq A, Khan MA, Akbar N, Baset A, et al. Applications of Various Types of Nanomaterials for the Treatment of Neurological Disorders. Nanomaterials. 2022; 12(13):2140. https://doi.org/10.3390/nano12132140
Chicago/Turabian StyleWaris, Abdul, Asmat Ali, Atta Ullah Khan, Muhammad Asim, Doaa Zamel, Kinza Fatima, Abdur Raziq, Muhammad Ajmal Khan, Nazia Akbar, Abdul Baset, and et al. 2022. "Applications of Various Types of Nanomaterials for the Treatment of Neurological Disorders" Nanomaterials 12, no. 13: 2140. https://doi.org/10.3390/nano12132140