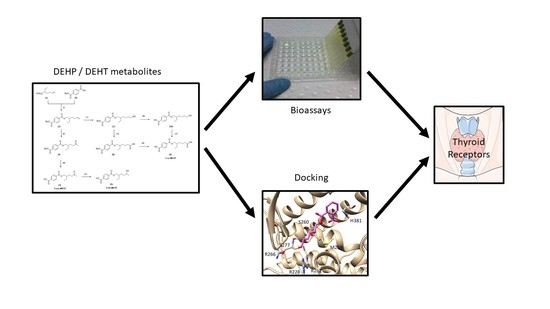
Comparative Effects of Di-(2-ethylhexyl)phthalate and Di-(2-ethylhexyl)terephthalate Metabolites on Thyroid Receptors: In Vitro and In Silico Studies
Abstract
:1. Introduction
2. Results
2.1. Access to the Secondary Metabolites 5-OH-MEHT, 5-oxo-MEHT and 5-cx-MEHT
2.2. Impact on Thyroid-Dependent Cell Growth
2.3. Docking
3. Discussion
3.1. Impact on Thyroid Hormones
3.2. Docking
3.3. In Vitro Data versus Biomonitoring Values
4. Materials and Methods
4.1. Metabolites of DEHP and DEHT
4.2. Preparation of Samples
4.3. T-Screen Assay
4.3.1. Cell Culture and Treatment
4.3.2. Cytotoxicity/Viability/Proliferation
4.3.3. Data Analysis
4.3.4. Statistical Analysis
4.4. Docking
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Supplementary Data—Synthesis of DEHP and DEHT Metabolites

Appendix B. Supplementary Data—Effects of Reference Positive Controls in the T-Screen Assay

References
- SCENIHR. Scientific Committee on Emerging and Newly-Identified Health Risks. Opinion on the Safety of Medical Devices Containing DEHP-Plasticized PVC or Other Plasticizers on Neonates and Other Groups Possibly at Risk. 2016. Available online: https://ec.europa/health/scientific_committees/emerging/docs/scenihr_o_047.pdf (accessed on 15 October 2020).
- Bernard, L.; Cueff, R.; Breysse, C.; Décaudin, B.; Sautou, V.; Armed Study Group. Migrability of PVC plasticizers from medical devices into a simulant of infused solutions. Int. J. Pharm. 2015, 485, 341–347. [Google Scholar] [CrossRef]
- Mallow, E.B.; Fox, M.A. Phthalates and critically ill neonates: Device-related exposures and non-endocrine toxic risks. J. Perinatol. 2014, 34, 892–897. [Google Scholar] [CrossRef] [PubMed]
- Fischer Fumeaux, C.J.; Stadelmann Diaw, C.; Palmero, D.; M’Madi, F.; Tolsa, J.F. Phthalate exposure in the neonatal intensive care unit. Arch. Pediatr. 2015, 22, 203–210. [Google Scholar] [CrossRef]
- Stroustrup, A.; Bragg, J.B.; Busgang, S.A.; Andra, S.S.; Curtin, P.; Spear, E.A.; Just, A.C.; Arora, M.; Gennings, C. Sources of clinically significant neonatal intensive care unit phthalate exposure. J. Expo. Sci. Environ. Epidemiol. 2020, 30, 137–148. [Google Scholar] [CrossRef]
- Regulation (EC) No 1272/2008 of the European Parliament and of the Council of 16 December 2008 on Classification, Labelling and Packaging of Substances and Mixtures, Amending and Repealing Directives 67/548/EEC and 1999/45/EC, and Amending Regulation (EC) No 1907/2006 (Text with EEA Relevance). 2008. Available online: http://data.europa.eu/eli/reg/2008/1272/oj/eng (accessed on on 15 October 2020).
- Regulation (EU) 2017/745 of the European Parliament and of the Council of 5 April 2017 on Medical Devices, Amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and Repealing Council Directives 90/385/EEC and 93/42/EEC (Text with EEA Relevance). 2017. Available online: http://data.europa.eu/eli/reg/2017/745/oj/eng (accessed on on 15 October 2020).
- Barber, E.D.; Fox, J.A.; Giordano, C.J. Hydrolysis, absorption and metabolism of di(2-ethylhexyl) terephthalate in the rat. Xenobiotica 1994, 24, 441–450. [Google Scholar] [CrossRef]
- CPSC Staff Statement on University of Cincinnati Report “Toxicity Review for Di-2 Ethylhexyl Terephthalate (DEHT)”. 2018. Available online: https://www.cpsc.gov/s3fs-public/Toxicity%20Review%20of%20DEHT.pdf?FObpuBBqgypVtw7gIEGMFXHN5H7vbeEz (accessed on 15 October 2020).
- Eljezi, T.; Pinta, P.; Richard, D.; Pinguet, J.; Chezal, J.M.; Chagnon, M.C.; Sautou, V.; Grimandi, G.; Moreau, E. In vitro cytotoxic effects of DEHP-alternative plasticizers and their primary metabolites on a L929 cell line. Chemosphere 2017, 173, 452–459. [Google Scholar] [CrossRef] [PubMed]
- Faber, W.D.; Deyo, J.A.; Stump, D.G.; Navarro, L.; Ruble, K.; Knapp, J. Developmental toxicity and uterotrophic studies with di-2-ethylhexyl terephthalate. Birth Defects Res. B Dev. Reprod. Toxicol. 2007, 80, 396–405. [Google Scholar] [CrossRef]
- Kambia, N.K.; Séverin, I.; Farce, A.; Moreau, E.; Dahbi, L.; Duval, C.; Dine, T.; Sautou, V.; Chagnon, M.C. In vitro and in silico hormonal activity studies of di-(2-ethylhexyl)terephthalate, a di-(2 ethylhexyl) phthalate substitute used in medical devices, and its metabolites. J. Appl. Toxicol. 2019, 39, 1043–1056. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Villanger, G.D.; Drover, S.S.M.; Nethery, R.C.; Thomsen, C.; Sakhi, A.K.; Øvergaard, K.R.; Zeiner, P.; Hoppin, J.A.; Reichborn-Kjennerud, T.; Aase, H.; et al. Associations between urine phthalate metabolites and thyroid function in pregnant women and the influence of iodine status. Environ. Int. 2020, 137, 105509. [Google Scholar] [CrossRef] [PubMed]
- Ghisari, M.; Bonefeld-Jorgensen, E.C. Effects of plasticizers and their mixtures on estrogen receptor and thyroid hormone functions. Toxicol. Lett. 2009, 189, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.-B.; Chuang, C.-J.; Su, P.-H.; Sun, C.-W.; Wang, C.-J.; Wu, M.-T.; Wang, S.-L. Prenatal and Childhood Exposure to Phthalate Diesters and Thyroid Function in a 9-Year Follow-up Birth Cohort Study: Taiwan Maternal and Infant Cohort Study. Epidemiol. Camb. Mass. 2017, 28 (Suppl. 1), S10–S18. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Moon, S.; Oh, B.-C.; Jung, D.; Choi, K.; Park, Y.J. Association Between Diethylhexyl Phthalate Exposure and Thyroid Function: A Meta-Analysis. Thyroid 2019, 29, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Zoeller, R.T.; Rivet, J. Timing of thyroid hormone action in the developing brain: Clinical observations and developmental findings. Neuroendocrinology 2004, 16, 809–818. [Google Scholar] [CrossRef]
- Vulsma, T. Impact of exposure to maternal PCBs and dioxins on the neonate’s thyroid hormone status. Epidemiology 2000, 11, 239–241. [Google Scholar] [CrossRef]
- De Cock, M.; Maas, Y.G.H.; Van de Bor, M. Does perinatal exposure to endocrine disruptors induce autism spectrum and attention deficit hyperactivity disorders? Rev. Acta Paediatr. 2012, 101, 811–818. [Google Scholar] [CrossRef] [PubMed]
- Qian, X.; Li, J.; Xu, S.; Wan, Y.; Li, Y.; Jiang, Y.; Zhao, H.; Zhou, Y.; Liao, J.; Liu, H.; et al. Prenatal exposure to phthalates and neurocognitive development in children at two years of age. Environ. Int. 2019, 131, 105023. [Google Scholar] [CrossRef]
- Nuti, F.; Hildenbrand, S.; Chelli, M.; Wodarz, R.; Papini, A.M. Synthesis of DEHP metabolites as biomarkers for GC–MS evaluation of phthalates as endocrine disrupters. Bioorg. Med. Chem. 2005, 13, 3461–3465. [Google Scholar] [CrossRef] [PubMed]
- Porterfield, S.P.; Hendrich, C.E. The role of thyroid hormones in prenatal and neonatal neurological development-current perspectives. Endocr. Rev. 1993, 14, 94–106. [Google Scholar] [PubMed]
- Bernal, J.; Nunez, J. Thyroid hormones and brain development. Eur. J. Endocrinol. 1995, 133, 390–398. [Google Scholar] [CrossRef]
- Hohenwarter, O.; Waltenberger, A.; Katinger, H. An in vitro test system for thyroid hormone action. Anal. Biochem. 1996, 234, 56–59. [Google Scholar] [CrossRef]
- Gutleb, A.C.; Meerts, I.A.T.M.; Bergsma, J.H.; Schriks, M.; Murk, A.J. T-Screen as a tool to identify thyroid hormone receptor active compounds. Environ. Toxicol. Pharmacol. 2005, 19, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, S.; Shimada, N.; Miyoshi, H.; Yamauchi, K. Detection of thyroid system-disrupting chemicals using in vitro and in vivo screening assays in Xenopus laevis. Toxicol. Sci. 2005, 88, 367–374. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ishihara, A.; Sawatsubashi, S.; Yamauchi, K. Endocrine disrupting chemicals: Interference of thyroid hormone binding to transthyretins and to thyroid hormone receptors. Mol. Cell. Endocrinol. 2003, 199, 105–117. [Google Scholar] [CrossRef]
- Dong, X.; Dong, J.; Zhao, Y.; Guo, J.; Wang, Z.; Liu, M.; Zhang, Y.; Na, X. Effects of Long-Term In Vivo Exposure to Di-2-Ethylhexylphthalate on Thyroid Hormones and the TSH/TSHR Signaling Pathways in Wistar Rats. Int. J. Environ. Res. Public Health 2017, 14, 44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, C.; Zhao, L.; Wei, L.; Li, L. DEHP reduces thyroid hormones via interacting with hormone synthesis-related proteins, deiodinases, transthyretin, receptors, and hepatic enzymes in rats. Environ. Sci. Pollut. Res. Int. 2015, 22, 12711–12719. [Google Scholar] [CrossRef] [PubMed]
- De Felice, M.; Pia Postiglione, M.; Di Lauro, R. Thyrotropin receptor signalling in development and differentiation of the thyroid gland: Insights from mouse models and human diseases. Endocrinology 2004, 145, 4062–4067. [Google Scholar] [CrossRef] [Green Version]
- Boas, M.; Feldt-Rasmussen, U.; Skakkebaek, N.E.; Main, K.M. Environmental chemicals and thyroid function. Eur. J. Endocrinol. 2006, 154, 599–611. [Google Scholar] [CrossRef] [Green Version]
- Gao, H.; Wu, W.; Xu, Y.; Jin, Z.; Bao, H.; Zhu, P.; Su, P.; Sheng, J.; Hao, J.; Tao, F. Effects of Prenatal Phthalate Exposure on Thyroid Hormone Concentrations Beginning at The Embryonic Stage. Sci. Rep. 2017, 7, 13106. [Google Scholar] [CrossRef] [Green Version]
- Meeker, J.D.; Calafat, A.M.; Hauser, R. Di(2-ethylhexyl) phthalate metabolites may alter thyroid hormone levels in men. Environ. Health Perspect. 2007, 115, 1029–1034. [Google Scholar] [CrossRef]
- Wu, M.T.; Wu, C.F.; Chen, B.H.; Chen, E.K.; Chen, Y.L.; Shiea, J.; Lee, W.T.; Chao, M.C.; Wu, J.R. Intake of phthalate-tainted foods alters thyroid functions in Taiwanese children. PLoS ONE 2013, 8, e55005. [Google Scholar] [CrossRef]
- Chen, F.Y.; Wang, S.S.; Wang, S.L.; Wang, R.M. Troglitazone inhibits proliferation of GH3 cell in vitro. Acad. J. Sec. Mil. Med. Univ. 2008, 29, 1052–1055. [Google Scholar]
- Demirel, A.; Çoban, A.; Yıldırım, Ş.; Doğan, C.; Sancı, R.; İnce, Z. Hidden Toxicity in Neonatal Intensive Care Units: Phthalate Exposure in Very Low Birth Weight Infants. J. Clin. Res. Pediatr. Endocrinol. 2016, 8, 298–304. [Google Scholar] [CrossRef]
- Strømmen, K.; Lyche, J.L.; Blakstad, E.W.; Moltu, S.J.; Veierød, M.B.; Almaas, A.N.; Sakhi, A.K.; Thomsen, C.; Nakstad, B.; Brække, K.; et al. Increased levels of phthalates in very low birth weight infants with septicemia and bronchopulmonary dysplasia. Environ. Int. 2016, 89–90, 228–234. [Google Scholar] [CrossRef]
- Calafat, A.M.; Needham, L.L.; Silva, M.J.; Lambert, G. Exposure to di-(2-ethylhexyl) phthalate among premature neonates in a neonatal intensive care unit. Pediatrics 2004, 113, e429–e434. [Google Scholar] [CrossRef] [Green Version]
- Green, R.; Hauser, R.; Calafat, A.M.; Weuve, J.; Schettler, T.; Ringer, S.; Huttner, K.; Hu, H. Use of di(2-ethylhexyl) phthalate-containing medical products and urinary levels of mono(2-ethylhexyl) phthalate in neonatal intensive care unit infants. Environ. Health Perspect. 2005, 113, 1222–1225. [Google Scholar] [CrossRef] [Green Version]
- Pinguet, J.; Kerckhove, N.; Eljezi, T.; Lambert, C.; Moreau, E.; Bernard, L.; Boeuf, B.; Decaudin, B.; Genay, S.; Masse, M.; et al. New SPE-LC-MS/MS method for the simultaneous determination in urine of 22 metabolites of DEHP and alternative plasticizers from PVC medical devices. Talanta 2019, 198, 377–389. [Google Scholar] [CrossRef] [PubMed]
- Gaynor, J.W.; Ittenbach, R.F.; Calafat, A.M.; Burnham, N.B.; Bradman, A.; Bellinger, D.C.; Henretig, F.M.; Wehrung, E.E.; Ward, J.L.; Russell, W.W.; et al. Perioperative Exposure to Suspect Neurotoxicants From Medical Devices in Newborns With Congenital Heart Defects. Ann. Thorac. Surg. 2019, 107, 567–572. [Google Scholar] [CrossRef]
- Eckert, E.; Müller, J.; Höllerer, C.; Purbojo, A.; Cesnjevar, R.; Göen, T.; Münch, F. Plasticizer exposure of infants during cardiac surgery. Toxicol. Lett. 2020, 330, 7–13. [Google Scholar] [CrossRef]
- Lessmann, F.; Correia-Sá, L.; Calhau, C.; Domingues, V.F.; Weiss, T.; Brüning, T.; Koch, H.M. Exposure to the plasticizer di(2-ethylhexyl) terephthalate (DEHTP) in Portuguese children—Urinary metabolite levels and estimated daily intakes. Environ. Int. 2017, 104, 25–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bernard, L.; Eljezi, T.; Clauson, H.; Lambert, C.; Bouattour, Y.; Chennell, P.; Pereira, B.; Sautou, V.; ARMED Study Group. Effects of flow rate on the migration of different plasticizers from PVC infusion medical devices. PLoS ONE 2018, 13, e0192369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lessmann, F.; Schütze, A.; Weiss, T.; Langsch, A.; Otter, R.; Brüning, T.; Koch, H.M. Metabolism and urinary excretion kinetics of di(2-ethylhexyl) terephthalate (DEHTP) in three male volunteers after oral dosage. Arch. Toxicol. 2016, 90, 1659–1667. [Google Scholar] [CrossRef]
- Schriks, M.; Vrabie, C.M.; Gutleb, A.C.; Faassen, E.J.; Rietjens, I.M.; Murk, A.J. T-screen to quantify functional potentiating, antagonistic and thyroid hormone-like activities of poly halogenated aromatic hydrocarbons (PHAHs). Toxicol. Vitr. 2006, 20, 490–498. [Google Scholar] [CrossRef] [PubMed]
- Sirbasku, D.A. Thyroid hormone dependent pituitary tumor cell growth in serum-free chemically defined culture. A new regulatory role for apotransferrin. Biochemistry 1991, 30, 7466–7477. [Google Scholar] [CrossRef]
- Souza, P.C.; Puhl, A.C.; Martinez, L.; Aparicio, R.; Nascimento, A.S.; Figueira, A.C.; Nguyen, P.; Webb, P.; Skaf, M.S.; Polikarpov, I. Identification of a new hormone-binding site on the surface of thyroid hormone receptor. Mol. Endocrinol. 2014, 28, 534–545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dow, R.L.; Schneider, S.R.; Paight, E.S.; Hank, R.F.; Chiang, P.; Cornelius, P.; Lee, E.; Newsome, W.P.; Swick, A.G.; Spitzer, J.; et al. Discovery of a Novel Series of 6-Azauracil-Based Thyroid Hormone Receptor Ligands: Potent, TRbeta Subtype-Selective Thyromimetics. Bioorg. Med. Chem. Lett. 2003, 13, 379–382. [Google Scholar] [CrossRef]





| Compounds Studied | In Silico Studies 1 Affinity toward TRα1 | In Vitro Studies Agonist/Antagonist Activities on Cell Proliferation |
|---|---|---|
| DEHP DEHT MEHT | 0 0 ++ | NT NT +++ antagonist or cytotoxic |
| MEHP | +++ | ++ agonist |
| 5-OH-MEHT | +/− | 0 |
| 5-OH-MEHP | ++++ | ++++ agonist and synergic activities |
| 5-oxo-MEHT | 0 | + antagonist |
| 5-oxo-MEHP | + | ++ antagonist or cytotoxic |
| 5-cx-MEHT | 0 | 0 |
| 5-cx-MEHP | 0 | 0 |
| DEHP Metabolites | DEHT Metabolites |
|---|---|
MEHP: mono-(2-ethylhexyl)phthalate | MEHT or MEHTP: mono-(2-ethylhexyl)terephthalate |
5-oxo-MEHP or MEOHP: mono-(2-ethyl-5-oxohexyl)phthalate | 5-oxo-MEHT or MEOHTP: mono-(2-ethyl-5-oxohexyl)terephthalate |
5-OH-MEHP or MEHHP: mono-(2-ethyl-5-hydroxyhexyl)phthalate | 5-OH-MEHT or MEHHTP: mono-(2-ethyl-5-hydroxyhexyl)terephthalate |
5-cx-MEHP or MECPP: mono-(2-ethyl-5-carboxypentyl)phthalate | 5-cx-MEHT or MECPTP: mono-(2-ethyl-5-carboxypentyl)terephthalate |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kambia, N.; Séverin, I.; Farce, A.; Dahbi, L.; Dine, T.; Moreau, E.; Sautou, V.; Chagnon, M.-C. Comparative Effects of Di-(2-ethylhexyl)phthalate and Di-(2-ethylhexyl)terephthalate Metabolites on Thyroid Receptors: In Vitro and In Silico Studies. Metabolites 2021, 11, 94. https://doi.org/10.3390/metabo11020094
Kambia N, Séverin I, Farce A, Dahbi L, Dine T, Moreau E, Sautou V, Chagnon M-C. Comparative Effects of Di-(2-ethylhexyl)phthalate and Di-(2-ethylhexyl)terephthalate Metabolites on Thyroid Receptors: In Vitro and In Silico Studies. Metabolites. 2021; 11(2):94. https://doi.org/10.3390/metabo11020094
Chicago/Turabian StyleKambia, Nicolas, Isabelle Séverin, Amaury Farce, Laurence Dahbi, Thierry Dine, Emmanuel Moreau, Valérie Sautou, and Marie-Christine Chagnon. 2021. "Comparative Effects of Di-(2-ethylhexyl)phthalate and Di-(2-ethylhexyl)terephthalate Metabolites on Thyroid Receptors: In Vitro and In Silico Studies" Metabolites 11, no. 2: 94. https://doi.org/10.3390/metabo11020094