Important Risk Factors in Patients with Nonvalvular Atrial Fibrillation Taking Dabigatran Using Integrated Machine Learning Scheme—A Post Hoc Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
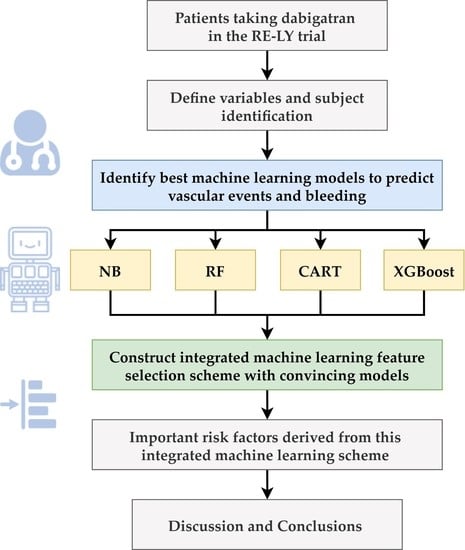
2.2. Proposed Integrated Machine Learning Scheme
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Feigin, V.L.; Stark, B.A.; Johnson, C.O.; Roth, G.A.; Bisignano, C.; Abady, G.G.; Abbasifard, M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abdi, V.; et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef]
- Go, A.S.; Hylek, E.M.; Phillips, K.A.; Chang, Y.; Henault, L.E.; Selby, J.V.; Singer, D.E. Prevalence of diagnosed atrial fibrillation in adults: National implications for rhythm management and stroke prevention: The An Ticoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001, 285, 2370–2375. [Google Scholar] [CrossRef] [PubMed]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; Castella, M.; Diener, H.-C.; Heidenbuchel, H.; Hendriks, J.; et al. ESC Scientific Document Group 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 2016, 37, 2893–2962. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, Y.-H.; See, L.-C.; Tu, H.-T.; Yeh, Y.-H.; Chang, S.-H.; Wu, L.-S.; Lee, H.-F.; Wang, C.-L.; Kuo, C.-F.; Kuo, C.-T. Efficacy and Safety of Apixaban, Dabigatran, Rivaroxaban, and Warfarin in Asians with Nonvalvular Atrial Fibrillation. J. Am. Heart Assoc. 2018, 7, e008150. [Google Scholar] [CrossRef] [Green Version]
- Chao, T.-F.; Chiang, C.-E.; Lin, Y.-J.; Chang, S.-L.; Lo, L.-W.; Hu, Y.-F.; Tuan, T.-C.; Liao, J.-N.; Chung, F.-P.; Chen, T.-J.; et al. Evolving changes of the use of oral anticoagulants and outcomes in patients with newly diagnosed atrial fibrillation in Taiwan. Circulation 2018, 138, 1485–1487. [Google Scholar] [CrossRef]
- Chan, Y.-H.; Chao, T.-F.; Chen, S.-W.; Lee, H.-F.; Yeh, Y.-H.; Huang, Y.-C.; Chang, S.-H.; Kuo, C.-T.; Lip, G.Y.H.; Chen, S.-A. Off-label dosing of non-vitamin K antagonist oral anticoagulants and clinical outcomes in Asian patients with atrial fibrillation. Heart Rhythm 2020, 17, 2102–2110. [Google Scholar] [CrossRef]
- Steinberg, B.A.; Shrader, P.; Thomas, L.; Ansell, J.; Fonarow, G.C.; Gersh, B.J.; Kowey, P.R.; Mahaffey, K.W.; Naccarelli, G.; Reiffel, J.; et al. Off-Label Dosing of Non-Vitamin K Antagonist Oral Anticoagulants and Adverse Outcomes: The ORBIT-AF II Registry. J. Am. Coll. Cardiol. 2016, 68, 2597–2604. [Google Scholar] [CrossRef]
- Yu, H.T.; Yang, P.-S.; Jang, E.; Kim, T.-H.; Uhm, J.-S.; Kim, J.-Y.; Pak, H.-N.; Lee, M.-H.; Lip, G.Y.H.; Joung, B. Label Adherence of Direct Oral Anticoagulants Dosing and Clinical Outcomes in Patients with Atrial Fibrillation. J. Am. Heart Assoc. 2020, 9, e014177. [Google Scholar] [CrossRef]
- Wu, X.; Hu, L.; Liu, J.; Gu, Q. Off-Label Underdosing or Overdosing of Non-vitamin K Antagonist Oral Anticoagulants in Patients with Atrial Fibrillation: A Meta-Analysis. Front. Cardiovasc. Med. 2021, 8, 724301. [Google Scholar] [CrossRef]
- Connolly, S.J.; Ezekowitz, M.D.; Yusuf, S.; Eikelboom, J.; Oldgren, J.; Parekh, A.; Pogue, J.; Reilly, P.A.; Themeles, E.; Varrone, J.; et al. Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2009, 361, 1139–1151. [Google Scholar] [CrossRef] [Green Version]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomstrom-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.-A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2020, 42, 373–498. [Google Scholar] [CrossRef]
- Lip, G.Y.H.; Nieuwlaat, R.; Pisters, R.; Lane, D.A.; Crijns, H.J.G.M. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The euro heart survey on atrial fibrillation. Chest 2010, 137, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Pisters, R.; Lane, D.A.; Nieuwlaat, R.; de Vos, C.B.; Crijns, H.J.; Lip, G.Y. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: The Euro Heart Survey. Chest 2010, 138, 1093–1100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chao, T.-F.; Lip, G.Y.; Liu, C.-J.; Tuan, T.-C.; Chen, S.-J.; Wang, K.-L.; Lin, Y.-J.; Chang, S.-L.; Lo, L.-W.; Hu, Y.-F.; et al. Validation of a Modified CHA2DS2-VASc Score for Stroke Risk Stratification in Asian Patients with Atrial Fibrillation: A Nationwide Cohort Study. Stroke 2016, 47, 2462–2469. [Google Scholar] [CrossRef] [Green Version]
- Chang, G.; Xie, Q.; Ma, L.; Hu, K.; Zhang, Z.; Mu, G.; Cui, Y. Accuracy of HAS-BLED and other bleeding risk assessment tools in predicting major bleeding events in atrial fibrillation: A network meta-analysis. J. Thromb. Haemost. 2020, 18, 791–801. [Google Scholar] [CrossRef]
- Chen, L.Y.; Norby, F.L.; Chamberlain, A.M.; MacLehose, R.F.; Bengtson, L.G.S.; Lutsey, P.L.; Alonso, A. CHA2DS2-VASc Score and Stroke Prediction in Atrial Fibrillation in Whites, Blacks, and Hispanics. Stroke 2019, 50, 28–33. [Google Scholar] [CrossRef]
- Liu, Y.; Chen, P.-H.C.; Krause, J.; Peng, L. How to Read Articles That Use Machine Learning: Users’ Guides to the Medical Literature. JAMA 2019, 322, 1806–1816. [Google Scholar] [CrossRef]
- Wu, C.-W.; Shen, H.-L.; Lu, C.-J.; Chen, S.-H.; Chen, H.-Y. Comparison of Different Machine Learning Classifiers for Glaucoma Diagnosis Based on Spectralis OCT. Diagnostics 2021, 11, 1718. [Google Scholar] [CrossRef] [PubMed]
- Bertini, F.; Allevi, D.; Lutero, G.; Montesi, D.; Calzà, L. Automatic speech classifier for mild cognitive impairment and early dementia. ACM Trans. Comput. Healthc. 2022, 3, 1–11. [Google Scholar] [CrossRef]
- Li, J.; Tobore, I.; Liu, Y.; Kandwal, A.; Wang, L.; Nie, Z. Non-invasive monitoring of three glucose ranges based on ECG by using DBSCAN-CNN. IEEE J. Biomed. Health Inform. 2021, 25, 3340–3350. [Google Scholar] [CrossRef]
- Enayati, M.; Farahani, N.Z.; Skubic, M. Machine Learning Approach for motion artifact detection in Ballistocardiogram signals. In Proceedings of the 14th EAI International Conference on Pervasive Computing Technologies for Healthcare, Atlanta, GA, USA, 18–20 May 2020; pp. 406–410. [Google Scholar]
- Bertini, F.; Bergami, G.; Montesi, D.; Veronese, G.; Marchesini, G.; Pandolfi, P. Predicting frailty condition in elderly using multidimensional socioclinical databases. Proc. IEEE 2018, 106, 723–737. [Google Scholar] [CrossRef]
- Kamel, H.; Navi, B.B.; Parikh, N.S.; Merkler, A.E.; Okin, P.M.; Devereux, R.B.; Weinsaft, J.W.; Kim, J.; Cheung, J.W.; Kim, L.K.; et al. Machine Learning Prediction of Stroke Mechanism in Embolic Strokes of Undetermined Source. Stroke 2020, 51, e203–e210. [Google Scholar] [CrossRef] [PubMed]
- Chun, M.; Clarke, R.; Cairns, B.J.; Clifton, D.; Bennett, D.; Chen, Y.; Guo, Y.; Pei, P.; Lv, J.; Yu, C.; et al. Stroke risk prediction using machine learning: A prospective cohort study of 0.5 million Chinese adults. J. Am. Med. Inform. Assoc. 2021, 28, 1719–1727. [Google Scholar] [CrossRef] [PubMed]
- January, C.T.; Wann, L.S.; Calkins, H.; Chen, L.Y.; Cigarroa, J.E.; Cleveland, J.C., Jr.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; Furie, K.L.; et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration with the Society of Thoracic Surgeons. Circulation 2019, 140, e125–e151. [Google Scholar] [CrossRef] [PubMed]
- WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163. [Google Scholar] [CrossRef]
- Center for Drug Evaluation and Research (CDER), Guidance, Compliance, & Regulatory Information. Available online: https://www.fda.gov/drugs/guidance-compliance-regulatory-information (accessed on 2 March 2022).
- Lewis, D.D. Naive (Bayes) at forty: The independence assumption in information retrieval. In Machine Learning: ECML-98; Springer: Chemnitz, Germany, 1998; pp. 4–15. [Google Scholar] [CrossRef] [Green Version]
- Breiman, L. Random Forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef] [Green Version]
- Breiman, L.; Friedman, J.H.; Olshen, R.A.; Stone, C.J. Classification and Regression Trees. Biometrics 1984, 40, 874. [Google Scholar] [CrossRef] [Green Version]
- Chen, T.; Guestrin, C. XGBoost: A Scalable Tree Boosting System. In Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, San Francisco, CA, USA, 13–17 August 2016; pp. 785–794. [Google Scholar]
- Quesada, J.A.; Lopez-Pineda, A.; Gil-Guillén, V.F.; Durazo-Arvizu, R.; Orozco-Beltrán, D.; López-Domenech, A.; Carratalá-Munuera, C. Machine learning to predict cardiovascular risk. Int. J. Clin. Pract. 2019, 73, e13389. [Google Scholar] [CrossRef] [Green Version]
- Fernandez-Lozano, C.; Hervella, P.; Mato-Abad, V.; Rodríguez-Yáñez, M.; Suárez-Garaboa, S.; López-Dequidt, I.; Estany-Gestal, A.; Sobrino, T.; Campos, F.; Castillo, J.; et al. Random forest-based prediction of stroke outcome. Sci. Rep. 2021, 11, 10071. [Google Scholar] [CrossRef]
- Fonarow, G.C. Risk stratification for in-hospital mortality in acutely decompensated heart failure classification and regression tree analysis. JAMA 2005, 293, 572. [Google Scholar] [CrossRef] [Green Version]
- Xu, Y.; Yang, X.; Huang, H.; Peng, C.; Ge, Y.; Wu, H.; Wang, J.; Xiong, G.; Yi, Y. Extreme Gradient Boosting Model Has a Better Performance in Predicting the Risk of 90-Day Readmissions in Patients with Ischaemic Stroke. J. Stroke Cerebrovasc. Dis. 2019, 28, 104441. [Google Scholar] [CrossRef] [PubMed]
- Cui, M.; Gang, X.; Gao, F.; Wang, G.; Xiao, X.; Li, Z.; Wang, G. Risk assessment of sarcopenia in patients with type 2 diabetes mellitus using data mining methods. Front. Endocrinol. 2020, 3, 123. [Google Scholar] [CrossRef] [PubMed]
- Hajian-Tilaki, K. Receiver Operator Characteristic Analysis of Biomarkers Evaluation in Diagnostic Research. J. Clin. Diagn. Res. 2018, 12, LE01–LE08. [Google Scholar] [CrossRef]
- Kuhn, M. Caret: Classification and Regression Training. 2022. R Package Version, 6.0-91. Available online: https://CRAN.R-project.org/package=caret (accessed on 2 March 2022).
- Bolón-Canedo, V.; Alonso-Betanzos, A. Ensembles for Feature Selection: A Review and Future Trends. Inf. Fusion 2019, 52, 1–12. [Google Scholar] [CrossRef]
- Breiman, L.; Cutler, A.; Liaw, A.; Wiener, M. randomForest: Breiman and Cutler’s Random Forests for Classification and Regression. 2022. R Package Version, 4.7-1. Available online: https://CRAN.R-project.org/package=randomForest (accessed on 2 March 2022).
- Therneau, T.; Atkinson, B. Rpart: Recursive Partitioning and Regression Trees. 2022. R Package Version, 4.1.16. Available online: https://CRAN.R-project.org/package=rpart (accessed on 2 March 2022).
- Chen, T.; He, T.; Benesty, M.; Khotilovich, V.; Tang, Y.; Cho, H.; Chen, K.; Mitchell, R.; Cano, I.; Zhou, T.; et al. Xgboost: Extreme Gradient Boosting. 2022. R Package Version, 1.5.2.1. Available online: https://CRAN.R-project.org/package=xgboost (accessed on 2 March 2022).
- Roever, C.; Raabe, N.; Luebke, K.; Ligges, U.; Szepannek, G.; Zentgraf, M.; Meyer, D. klaR: Classification and Visualization. 2020. R Package Version, 0.6-15. Available online: https://CRAN.R-project.org/package=klaR (accessed on 2 March 2022).
- Poredos, P.; Orehek, M.; Tratnik, E. Smoking is associated with dose-related increase of intima-media thickness and endothelial dysfunction. Angiology 1999, 50, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Albertsen, I.E.; Rasmussen, L.H.; Lane, D.A.; Overvad, T.F.; Skjøth, F.; Overvad, K.; Lip, G.Y.H.; Larsen, T.B. The impact of smoking on thromboembolism and mortality in patients with incident atrial fibrillation: Insights from the Danish Diet, Cancer, and Health study. Chest 2014, 145, 559–566. [Google Scholar] [CrossRef]
- Nakagawa, K.; Hirai, T.; Ohara, K.; Fukuda, N.; Numa, S.; Taguchi, Y.; Dougu, N.; Takashima, S.; Nozawa, T.; Tanaka, K.; et al. Impact of persistent smoking on long-term outcomes in patients with nonvalvular atrial fibrillation. J. Cardiol. 2015, 65, 429–433. [Google Scholar] [CrossRef] [Green Version]
- Chamberlain, A.M.; Agarwal, S.K.; Folsom, A.R.; Duval, S.; Soliman, E.Z.; Ambrose, M.; Eberly, L.E.; Alonso, A. Smoking and incidence of atrial fibrillation: Results from the Atherosclerosis Risk in Communities (ARIC) study. Heart Rhythm 2011, 8, 1160–1166. [Google Scholar] [CrossRef] [Green Version]
- Nathisuwan, S.; Dilokthornsakul, P.; Chaiyakunapruk, N.; Morarai, T.; Yodting, T.; Piriyachananusorn, N. Assessing evidence of interaction between smoking and warfarin: A systematic review and meta-analysis. Chest 2011, 139, 1130–1139. [Google Scholar] [CrossRef] [Green Version]
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R.; et al. Heart disease and stroke statistics-2018 update a report from the American Heart Association. Circulation 2018, 137, E67–E492. [Google Scholar] [CrossRef]
- Pullicino, P.M.; Halperin, J.L.; Thompson, J.L. Stroke in patients with heart failure and reduced left ventricular ejection fraction. Neurology 2000, 54, 288–294. [Google Scholar] [CrossRef] [PubMed]
- Freudenberger, R.S.; Hellkamp, A.S.; Halperin, J.L.; Poole, J.; Anderson, J.; Johnson, G.; Mark, D.B.; Lee, K.L.; Bardy, G.H.; Investigators, S.-H. Risk of thromboembolism in heart failure: An analysis from the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT). Circulation 2007, 115, 2637–2641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lip, G.Y. Does atrial fibrillation confer a hypercoagulable state? Lancet 1995, 346, 313–1314. [Google Scholar] [CrossRef]
- Georgiadis, D.; Sievert, M.; Cencetti, S.; Uhlmann, F.; Krivokuca, M.; Zierz, S.; Werdan, K. Cerebrovascular reactivity is impaired in patients with cardiac failure. Eur. Heart J. 2000, 21, 407–413. [Google Scholar] [CrossRef] [Green Version]
- Patel, M.R.; Mahaffey, K.W.; Garg, J.; Pan, G.; Singer, D.E.; Hacke, W.; Breithardt, G.; Halperin, J.L.; Hankey, G.J.; Piccini, J.P.; et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N. Engl. J. Med. 2011, 365, 883–891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Granger, C.B.; Alexander, J.H.; McMurray, J.J.V.; Lopes, R.D.; Hylek, E.M.; Hanna, M.; Al-Khalidi, H.R.; Ansell, J.; Atar, D.; Avezum, A.; et al. Apixaban versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2011, 365, 981–992. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giugliano, R.P.; Ruff, C.T.; Braunwald, E.; Murphy, S.A.; Wiviott, S.D.; Halperin, J.L.; Waldo, A.L.; Ezekowitz, M.D.; Weitz, J.I.; Špinar, J.; et al. Edoxaban versus Warfarin in Patients with Atrial Fibrillation. N. Engl. J. Med. 2013, 369, 2093–2104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qamar, A.; Bhatt, D.L. Stroke Prevention in Atrial Fibrillation in Patients with Chronic Kidney Disease. Circulation 2016, 133, 1512–1515. [Google Scholar] [CrossRef]
- Bonde, A.N.; Lip, G.Y.H.; Kamper, A.-L.; Fosbøl, E.L.; Staerk, L.; Carlson, N.; Torp-Pedersen, C.; Gislason, G.; Olesen, J.B. Renal Function and the Risk of Stroke and Bleeding in Patients with Atrial Fibrillation: An Observational Cohort Study. Stroke 2016, 47, 2707–2713. [Google Scholar] [CrossRef] [Green Version]
- Shlipak, M.G.; Fried, L.F.; Crump, C.; Bleyer, A.J.; Manolio, T.A.; Tracy, R.P.; Furberg, C.D.; Psaty, B.M. Elevations of inflammatory and procoagulant biomarkers in elderly persons with renal insufficiency. Circulation 2002, 107, 87–92. [Google Scholar] [CrossRef] [Green Version]
- Pavord, S.; Myers, B. Bleeding and thrombotic complications of kidney disease. Blood Rev. 2011, 25, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.T.; Magno, C.P.; Lane, K.T.; Hinojosa, M.W.; Lane, J.S. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: Findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J. Am. Coll. Surg. 2008, 207, 928–934. [Google Scholar] [CrossRef] [PubMed]
- Calle, E.E.; Thun, M.J.; Petrelli, J.M.; Rodriguez, C.; Heath, C.W., Jr. Body-mass index and mortality in a prospective cohort of US adults. N. Engl. J. Med. 1999, 341, 1097–1105. [Google Scholar] [CrossRef]
- Zhu, W.; Wan, R.; Liu, F.; Hu, J.; Huang, L.; Li, J.; Hong, K. Relation of Body Mass Index with Adverse Outcomes among Patients with Atrial Fibrillation: A Meta-Analysis and Systematic Review. J. Am. Heart Assoc. 2016, 5, e004006. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.R.; Choi, E.K.; Jung, J.H.; Park, S.H.; Han, K.D.; Oh, S.; Lip, G.Y. Body Mass Index and Clinical Outcomes in Asian Patients with Atrial Fibrillation Receiving Oral Anticoagulation. Stroke 2021, 52, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Hellwig, T.; Gulseth, M. Pharmacokinetic and pharmacodynamic drug interactions with new oral anticoagulants: What do they mean for patients with atrial fibrillation? Ann. Pharmacother. 2013, 47, 1478–1487. [Google Scholar] [CrossRef] [PubMed]
- U.S. Food and Drug Administration. Drugs@FDA: FDA Approved Drug Products. Available online: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm (accessed on 3 March 2022).
- Chang, S.-H.; Chou, I.-J.; Yeh, Y.-H.; Chiou, M.-J.; Wen, M.-S.; Kuo, C.-T.; See, L.-C.; Kuo, C.-F. Association between Use of Non-Vitamin K Oral Anticoagulants with and without Concurrent Medications and Risk of Major Bleeding in Nonvalvular Atrial Fibrillation. JAMA 2017, 318, 1250–1259. [Google Scholar] [CrossRef]
- Pham, P.; Schmidt, S.; Lesko, L.; Lip, G.Y.H.; Brown, J.D. Association of Oral Anticoagulants and Verapamil or Diltiazem with Adverse Bleeding Events in Patients with Nonvalvular Atrial Fibrillation and Normal Kidney Function. JAMA Netw. Open 2020, 3, e203593. [Google Scholar] [CrossRef]
- Vandiver, J.W.; Diane Beavers, K. Combining oral anticoagulation and antiplatelet therapies: Appropriate patient selection. J. Thromb. Thrombolysis 2018, 45, 423–431. [Google Scholar] [CrossRef]


| Variables | Description | Units | |
|---|---|---|---|
| V1 | Sex | 0: Male; 1: Female | - |
| V2 | Age | 1: <65; 2: ≥65 and <75; 3: ≥75 | years |
| V3 | BMI | 1: <18.5; 2: ≥18.5 and <30; 3: ≥30 | kg/m2 |
| V4 | Body weight | 0: <60; 1: ≥60 | kg |
| V5 | Ethnicity | 0: Arab/others; 1: European | - |
| V6 | Hypertension history | 0: Record of hypertension that required medical treatment); 1: No | - |
| V7 | Kidney function (GFR) | 1: <30; 2: ≥30 and <50; 3: ≥50 | mL/min/1.73 m2 |
| V8 | Previous stroke history | 0: History of stroke or TIA; 1: No | - |
| V9 | Previous bleeding history | 0: History of bleeding; 1: No | - |
| V10 | Concomitant use of drugs | 0: Concomitant use of verapamil, diltiazem, antithrombotic agent, NSAID, or COX inhibitor; 1: No | - |
| V11 | History of MI | 0: History of MI; 1: No | - |
| V12 | History of DM | 0: History of DM; 1: No | - |
| V13 | History of CHF | 0: Medical history of CHF or heart echo revealed ejection fraction <40%; 1: No | - |
| V14 | Smoking | 1: Never; 2: Current smoker; 3: Former smoker | - |
| V15 | History of systemic embolism | 0: History of systemic embolism; 1: No | - |
| V16 | Liver function abnormality # | 0: Presence of liver function abnormality 1: No | - |
| V17 | Anemia | 0: Hemoglobin ≥10; 1: <10 | g/dL |
| V18 | Medicine dosage (dabigatran) | 0: 110 mg twice per day 1: 150 mg twice per day | - |
| P1 | Vascular events † | 0: No vascular event happened within the first year of follow-up 1: Yes | - |
| P2 | Bleeding events * | 0: No bleeding event happened within the first year of follow-up 1: Yes | - |
| Characteristics | Metrics |
|---|---|
| V1 Sex | N (%) |
| 0: Male | 7519 (63.70) |
| 1: Female | 4284 (36.30) |
| V2 Age (years) | N (%) |
| 1: <65 | 1982 (16.79) |
| 2: ≥65 and <75 | 5123 (43.41) |
| 3: ≥75 | 4697 (39.80) |
| V3 BMI (kg/m2) | N (%) |
| 1: <18.5 | 123 (1.04) |
| 2: ≥18.5 and <30 | 7589 (64.30) |
| 3: ≥30 | 4091 (34.66) |
| V4 Body weight | N (%) |
| 0: <60 | 1098 (9.30) |
| 1: ≥60 | 10,705 (90.70) |
| V5 Ethnicity | N (%) |
| 0: Arab/others | 3594 (30.45) |
| 1: European | 8209 (69.55) |
| V6 Hypertension history | N (%) |
| 0: Record of hypertension that required medical treatment | 9301 (78.80) |
| 1: No | 2502 (21.20) |
| V7 Kidney function (GFR) | N (%) |
| 1: <30 | 45 (0.38) |
| 2: ≥30 and <50 | 2245 (19.02) |
| 3: ≥50 | 9513 (80.60) |
| V8 Previous stroke history | N (%) |
| 0: Yes | 2366 (20.05) |
| 1: No | 9437 (79.95) |
| V9 Previous bleeding history | N (%) |
| 0: Yes | 774 (6.56) |
| 1: No | 11,029 (93.44) |
| V10 Concomitant use of drugs | N (%) |
| 0: Yes | 2845 (24.10) |
| 1: No | 8958 (75.90) |
| V11 History of myocardial infarction | N (%) |
| 0: Yes | 1982 (16.79) |
| 1: No | 9821 (83.21) |
| V12 History of diabetes mellitus | N (%) |
| 0: Yes | 2739 (23.21) |
| 1: No | 9064 (76.79) |
| V13 History of congestive heart failure | N (%) |
| 0: Yes | 4125 (34.95) |
| 1: No | 7678 (65.05) |
| V14 Smoking | N (%) |
| 1: Never | 5781 (48.98) |
| 2: Current | 867 (7.35) |
| 3: Former | 5155 (43.68) |
| V15 History of systemic embolism | N (%) |
| 0: Yes | 306 (2.59) |
| 1: No | 11,497 (97.41) |
| V16 Liver function abnormality | N (%) |
| 0: Presence of liver function abnormality | 84 (0.71) |
| 1: No | 11,719 (99.29) |
| V17 Anemia | N (%) |
| 0: Hemoglobin ≥10 g/dL | 11,773 (99.75) |
| 1: Hemoglobin <10 g/dL | 30 (0.25) |
| V18 Medicine dosage (dabigatran) | N (%) |
| 1: 110 mg | 5870 (49.73) |
| 2: 150 mg | 5933 (50.27) |
| P1 Vascular events | N (%) |
| 0: No | 11,485 (97.31) |
| 1: Yes | 318 (2.69) |
| P2 Bleeding events | N (%) |
| 0: No | 9565 (81.04) |
| 1: Yes | 2238 (18.96) |
| Methods | Hyperparameters | Best Value | Meanings |
|---|---|---|---|
| CART | minispilt | 20 | The minimum number of observations that must exist in a node for a split to be attempted. |
| minibucket | 20 | The minimum number of observations in any terminal node. | |
| maxdepth | 10 | The maximum depth of any node of the final tree. | |
| xval | 10 | Number of cross-validations. | |
| cp | 0.0013 | Complexity parameter: The minimum improvement in the model needed at each node. | |
| RF | ntree | 500 | The number of trees in forest. |
| mtry | 2 | The number of predictors sampled for splitting at each node. | |
| NB | fL | 1 | Adjustment of Laplace smoother. |
| usekernel | FALSE | Using kernel density estimate for continuous variable versus a Gaussian density estimate. | |
| adjust | 1 | Adjust the bandwidth of the kernel density. | |
| XGBoost | nrounds | 100 | The number of boosted trees. |
| maximum depth | 2 | The maximum depth of a tree. | |
| learning rate | 0.4 | Shrinkage coefficient of tree. | |
| gamma | 0 | The minimum loss reduction. | |
| subsample | 1 | Subsample ratio of columns when building each tree. | |
| colsample_bytree | 0.8 | Subsample ratio of columns when constructing each tree. | |
| rate_drop | 0.01 | Rate of trees dropped. | |
| skip_drop | 0.95 | Probability of skipping the dropout procedure during a boosting iteration. | |
| min_child_weight | 1 | The minimum sum of instance weight. |
| Methods | Accuracy Mean (SD) | Sensitivity Mean (SD) | Specificity Mean (SD) | AUC Mean (SD) |
|---|---|---|---|---|
| (a) Vascular events | ||||
| LGR | 0.574 (0.03) | 0.571 (0.04) | 0.707 (0.03) | 0.674 (0.00) |
| NB | 0.569 (0.03) | 0.565 (0.03) | 0.711 (0.04) | 0.674 (0.00) |
| RF | 0.890 (0.03) | 0.898 (0.03) | 0.599 (0.04) | 0.780 (0.01) |
| CART | 0.599 (0.09) | 0.598 (0.10) | 0.621 (0.09) | 0.637 (0.00) |
| XGBoost | 0.646 (0.09) | 0.645 (0.09) | 0.693 (0.04) | 0.717 (0.04) |
| (b) Bleeding | ||||
| LGR | 0.604 (0.03) | 0.622 (0.05) | 0.527 (0.05) | 0.605 (0.00) |
| NB | 0.599 (0.01) | 0.613 (0.02) | 0.537 (0.02) | 0.603 (0.00) |
| RF | 0.757 (0.01) | 0.822 (0.02) | 0.479 (0.02) | 0.684 (0.00) |
| CART | 0.787 (0.07) | 0.959 (0.12) | 0.052 (0.16) | 0.467 (0.03) |
| XGBoost | 0.625 (0.03) | 0.650 (0.05) | 0.517 (0.05) | 0.618 (0.00) |
| Risk Factors | Average Ranking of 10 Times RF | Average Ranking of 10 Times XGBoost | Average Ranking of the 2 Models | Final Ranking in Predicting Vascular Events |
|---|---|---|---|---|
| Age | 1 | 5.2 | 3.1 | 1 |
| History of congestive heart failure | 4.6 | 2.1 | 3.35 | 2 |
| History of myocardial infarction | 4 | 2.8 | 3.4 | 3 |
| Smoking | 2.2 | 5.6 | 3.9 | 4 |
| Kidney function | 5.9 | 6.1 | 6 | 5 |
| BMI | 3.5 | 10.5 | 7 | 6 |
| Ethnicity | 7.8 | 7.3 | 7.55 | 7 |
| History of diabetes mellitus | 8.6 | 7 | 7.8 | 8 |
| Medicine dosage (dabigatran) | 8.5 | 7.5 | 8 | 9 |
| Previous stroke history | 9.4 | 9.6 | 9.5 | 10 |
| Body weight | 12.2 | 8.9 | 11.05 | 11 |
| Concomitant use of drugs | 14.3 | 9.8 | 12.05 | 12 |
| Hypertension history | 11.8 | 13.2 | 12.5 | 13 |
| Sex | 11.7 | 14.3 | 13 | 14 |
| Previous bleeding history | 14.5 | 14 | 14.25 | 15 |
| History of systemic embolism | 16.3 | 14.8 | 15.55 | 16 |
| Liver function abnormality | 16.7 | 15 | 15.85 | 17 |
| Anemia | 18 | 18 | 18 | 18 |
| Risk Factors | Average Ranking of 10 Times RF | Average Ranking of 10 Times XGBoost | Average Ranking of the 2 Models | Final Ranking in Predicting Bleeding |
|---|---|---|---|---|
| Age | 1 | 1.3 | 1.15 | 1 |
| Kidney function | 3.2 | 3.5 | 3.35 | 2 |
| Smoking | 2.1 | 4.7 | 3.4 | 3 |
| Previous bleeding history | 4.7 | 2.4 | 3.55 | 4 |
| Concomitant use of drugs | 4.8 | 5 | 4.9 | 5 |
| Medicine dosage (dabigatran) | 7 | 6.7 | 6.85 | 6 |
| BMI | 5.2 | 9.6 | 7.4 | 7 |
| History of myocardial infarction | 9.2 | 6.1 | 7.65 | 8 |
| History of congestive heart failure | 10.1 | 10.3 | 10.2 | 9 |
| Ethnicity | 9.1 | 12.2 | 10.65 | 10 |
| Sex | 10.8 | 11.3 | 10.55 | 11 |
| History of diabetes mellitus | 12.8 | 11.5 | 12.15 | 12 |
| Previous stroke history | 11 | 14.2 | 12.6 | 13 |
| Hypertension history | 14 | 12.6 | 13.3 | 14 |
| Body weight | 15 | 12.3 | 13.65 | 15 |
| History of systemic embolism | 16 | 13 | 14.5 | 16 |
| Liver function abnormality | 17 | 17 | 17 | 17 |
| Anemia | 18 | 17.4 | 17.7 | 18 |
| Average Ranking of Variables | Variable of Prediction of Vascular Events | Variable of Prediction of Bleeding |
|---|---|---|
| 1 | Age | Age |
| 2 | History of CHF | Kidney function |
| 3 | History of MI | Smoking |
| 4 | Smoking | Previous bleeding history |
| 5 | Kidney function | Concomitant use of drugs |
| 6 | BMI | Medicine dosage (dabigatran) |
| 7 | Ethnicity | BMI |
| 8 | History of diabetes mellitus | History of MI |
| 9 | Medicine dosage (dabigatran) | History of CHF |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Y.-C.; Cheng, Y.-C.; Jhou, M.-J.; Chen, M.; Lu, C.-J. Important Risk Factors in Patients with Nonvalvular Atrial Fibrillation Taking Dabigatran Using Integrated Machine Learning Scheme—A Post Hoc Analysis. J. Pers. Med. 2022, 12, 756. https://doi.org/10.3390/jpm12050756
Huang Y-C, Cheng Y-C, Jhou M-J, Chen M, Lu C-J. Important Risk Factors in Patients with Nonvalvular Atrial Fibrillation Taking Dabigatran Using Integrated Machine Learning Scheme—A Post Hoc Analysis. Journal of Personalized Medicine. 2022; 12(5):756. https://doi.org/10.3390/jpm12050756
Chicago/Turabian StyleHuang, Yung-Chuan, Yu-Chen Cheng, Mao-Jhen Jhou, Mingchih Chen, and Chi-Jie Lu. 2022. "Important Risk Factors in Patients with Nonvalvular Atrial Fibrillation Taking Dabigatran Using Integrated Machine Learning Scheme—A Post Hoc Analysis" Journal of Personalized Medicine 12, no. 5: 756. https://doi.org/10.3390/jpm12050756