Knowledge and Attitudes of Medical and Health Science Students in the United Arab Emirates toward Genomic Medicine and Pharmacogenomics: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Students’ Demographic and Academic Characteristics
3.2. Assessment of General Knowledge of Students on Genomic Medicine and PGX
3.3. Attitudes towards Genomic Medicine and PGX
3.3.1. Views and Considerations on Genomic Medicine and PGX
3.3.2. Desire to Participate
3.3.3. Accessibility and Availability of Genetic Testing
3.3.4. Concerns and Ethics Regarding Genomic Medicine and PGX
3.3.5. Outlooks on the Future of Genomic Medicine and PGX
4. Discussion
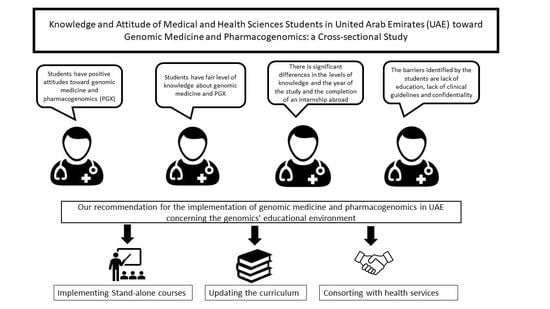
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gurwitz, D.; Weizman, A.; Rehavi, M. Education: Teaching pharmacogenomics to prepare future physicians and researchers for personalized medicine. Trends Pharm. Sci. 2003, 24, 122–125. [Google Scholar] [CrossRef]
- Pisanu, C.; Tsermpini, E.E.; Mavroidi, E.; Katsila, T.; Patrinos, G.P.; Squassina, A. Assessment of the pharmacogenomics educational environment in southeast Europe. Public Health Genom. 2014, 17, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Gurwitz, D. Pharmacogenetics education: 10 years of experience at Tel Aviv University. Pharmacogenomics 2010, 11, 647–649. [Google Scholar] [CrossRef] [PubMed]
- Alejielat, R.; Ejielat, Z.; Andrawes, S.; Mhaidat, N.M. An evaluation of the knowledge, opinions, expectations and concerns toward pharmacogenomics among Jordanian pharmacists. Pers. Med. 2016, 13, 143–154. [Google Scholar] [CrossRef] [Green Version]
- Giri, J.; Curry, T.B.; Formea, C.M.; Nicholson, W.T.; Rohrer Vitek, C.R. Education and knowledge in pharmacogenomics: Still a challenge? Clin. Pharm. 2018, 103, 752–755. [Google Scholar] [CrossRef]
- Karas Kuželički, N.; Prodan Žitnik, I.; Gurwitz, D.; Llerena, A.; Cascorbi, I.; Siest, S.; Simmaco, M.; Ansari, M.; Pazzagli, M.; DI Resta, C.; et al. Pharmacogenomics education in medical and pharmacy schools: Conclusions of a global survey. Pharmacogenomics 2019, 20, 643–657. [Google Scholar] [CrossRef] [Green Version]
- Mccullough, K.B.; Formea, C.M.; Berg, K.D.; Burzynski, J.A.; Cunningham, J.L.; Ou, N.N.; Rudis, M.I.; Stollings, J.L.; Nicholson, W.T. Assessment of the pharmacogenomics educational needs of pharmacists. Am. J. Pharm. Educ. 2011, 75. [Google Scholar] [CrossRef] [Green Version]
- Formea, C.M.; Nicholson, W.T.; McCullough, K.B.; Berg, K.D.; Berg, M.L.; Cunningham, J.L.; Merten, J.A.; Ou, N.N.; Stollings, J.L. Development and evaluation of a pharmacogenomics educational program for pharmacists. Am. J. Pharm. Educ. 2013, 77. [Google Scholar] [CrossRef]
- Higgs, J.E.; Andrews, J.; Gurwitz, D.; Payne, K.; Newman, W. Pharmacogenetics education in British medical schools. Genomic Med. 2008, 2, 101–105. [Google Scholar] [CrossRef] [Green Version]
- Tsermpini, E.E.; Stamopoulou, T.; Kordou, Z.; Barba, E.; Siamoglou, S.; Stathoulias, A.; Patrinos, G.P. Continuous pharmacogenomics and genomic medicine education for healthcare professionals through electronic educational courses. Future Med. 2019, 16, 189–193. [Google Scholar] [CrossRef]
- Green, J.S.; Obrien, T.J.; Chiappinelli, V.A.; Harralson, A.F. Pharmacogenomics instruction in US and Canadian medical schools: Implications for personalized medicine. Pharmacogenomics 2010, 11, 1331–1340. [Google Scholar] [CrossRef] [PubMed]
- Gurwitz, D.; Lunshof, J.E.; Dedoussis, G.; Flordellis, C.S.; Fuhr, U.; Kirchheiner, J.; Licinio, J.; Llerena, A.; Manolopoulos, V.G.; Sheffield, L.J.; et al. Pharmacogenomics education: International Society of Pharmacogenomics recommendations for medical, pharmaceutical, and health schools Deans of Education. Pharmacogenomics J. 2005, 5, 221–225. [Google Scholar] [CrossRef] [PubMed]
- Abdela, O.A.; Bhagavathula, A.S.; Gebreyohannes, E.A.; Tegegn, H.G. Ethiopian health care professionals’ knowledge, attitude, and interests toward pharmacogenomics. Pharmgenomics Pers. Med. 2017, 10, 279–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muzoriana, N.; Gavi, S.; Nembaware, V.; Dhoro, M.; Matimba, A. Knowledge, Attitude, and Perceptions of Pharmacists and Pharmacy Students towards Pharmacogenomics in Zimbabwe. Pharmacy 2017, 5, 36. [Google Scholar] [CrossRef] [Green Version]
- McMahon, T.; Tucci, J. The perceptions of pharmacists in Victoria, Australia on pharmacogenetics and its implications. Pharm. Pract. (Granada) 2011, 9, 141–147. [Google Scholar] [CrossRef]
- Albassam, A.; Alshammari, S.; Ouda, G.; Koshy, S.; Awad, A. Knowledge, perceptions and confidence of physicians and pharmacists towards pharmacogenetics practice in Kuwait. PLoS ONE 2018, 13, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Elewa, H.; Alkhiyami, D.; Alsahan, D.; Abdel-Aziz, A. A survey on the awareness and attitude of pharmacists and doctors towards the application of pharmacogenomics and its challenges in Qatar. J. Eval. Clin. Pract. 2015, 21, 703–709. [Google Scholar] [CrossRef] [Green Version]
- Carver, R.B.; Castéra, J.; Gericke, N.; Evangelista, N.A.M.; El-Hani, C.N. Young adults’ belief in genetic determinism, and knowledge and attitudes towards modern genetics and genomics: The PUGGS questionnaire. PLoS ONE 2017, 12, 1–24. [Google Scholar] [CrossRef]
- Murphy, J.E.; Green, J.S.; Adams, L.A.; Squire, R.B.; Kuo, G.M.; Mckay, A. Pharmacogenomics in the curricula of colleges and schools of pharmacy in the United States. Am. J. Pharm. Educ. 2010, 74, 7. [Google Scholar] [CrossRef] [Green Version]
- Johansen Taber, K.A.; Dickinson, B.D. Pharmacogenomic knowledge gaps and educational resource needs among physicians in selected specialties. Pharmgenomics. Pers. Med. 2014, 7, 145–162. [Google Scholar] [CrossRef] [Green Version]
- Kim, W.Y.; Kim, H.S.; Oh, M.; Shin, J.G. Survey of physicians’ views on the clinical implementation of pharmacogenomics-based personalized therapy. Transl. Clin. Pharm. 2020, 28, 34–42. [Google Scholar] [CrossRef]
- Plunkett-Rondeau, J.; Hyland, K.; Dasgupta, S. Training future physicians in the era of genomic medicine: Trends in undergraduate medical genetics education. Genet. Med. 2015, 17, 927–934. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Talwar, D.; Chen, W.J.; Yeh, Y.L.; Foster, M.; Al-Shagrawi, S.; Chen, L.S. Characteristics and evaluation outcomes of genomics curricula for health professional students: A systematic literature review. Genet. Med. 2019, 21, 1675–1682. [Google Scholar] [CrossRef]
- Jarrar, Y.; Mosleh, R.; Hawash, M.; Jarrar, Q. Knowledge and attitudes of pharmacy students towards pharmacogenomics among universities in Jordan and west bank of Palestine. Pharmgenomics Pers. Med. 2019, 12, 247–255. [Google Scholar] [CrossRef] [Green Version]
- Laskey, S.L.; Williams, J.; Pierre-Louis, J.; O’Riordan, M.A.; Matthews, A.; Robin, N.H. Attitudes of African American premedical students toward genetic testing and screening. Genet. Med. 2003, 5, 49–54. [Google Scholar] [CrossRef] [Green Version]
- Olwi, D.; Merdad, L.; Ramadan, E. Knowledge of genetics and attitudes toward genetic testing among college students in Saudi Arabia. Public Health Genomics 2016, 19, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Mavroidopoulou, V.; Xera, E.; Mollaki, V. Awareness, attitudes and perspectives of direct-to-consumer genetic testing in Greece: A survey of potential consumers. J. Hum. Genet. 2015, 60, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Cameron, L.D.; Reeve, J. Risk perceptions, worry, and attitudes about genetic testing for breast cancer susceptibility. Psychol. Health 2006, 21, 211–230. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, H.; Phillips, L.A.; Burns, E. The Common-Sense Model of Self-Regulation (CSM): A dynamic framework for understanding illness self-management. J. Behav. Med. 2016, 39, 935–946. [Google Scholar] [CrossRef]
- Mills, R.; Haga, S.B. Clinical delivery of pharmacogenetic testing services: A proposed partnership between genetic counselors and pharmacists. Pharmacogenomics 2013, 14, 957–968. [Google Scholar] [CrossRef] [Green Version]
- Kennedy, M.J. Personalized medicines—Are pharmacists ready for the challenge? Integr. Pharm. Res. Pract. 2018, 7, 113–123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shanti, H.; Chouchane, L.; Badii, R.; Gallouzi, I.E.; Gasparini, P. Genetic testing and genomic analysis: A debate on ethical, social and legal issues in the Arab world with a focus on Qatar. J. Transl. Med. 2015, 13, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wauters, A.; Van Hoyweghen, I. Concerns about genetic discrimination after regulation: A qualitative study of the situation regarding BRCA and Huntington’s disease in Belgium. Laws 2018, 7, 17. [Google Scholar] [CrossRef] [Green Version]
- Shah, S.N.; Shaheen, S. Biotechnological research. Biotechnol. Res. 2016, 2, 173–175. [Google Scholar]
- Mitropoulos, K.; Al Jaibeji, H.; Forero, D.A.; Laissue, P.; Wonkam, A.; Lopez-Correa, C.; Mohamed, Z.; Chantratita, W.; Lee, M.T.M.; Llerena, A.; et al. Success stories in genomic medicine from resource-limited countries. Hum. Genom. 2015, 9, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Berlin, D.S.; Person, M.G.; Mittal, A.; Oppezzo, M.A.; Chin, D.B.; Starr, B.; Klein, T.E.; Schwartz, D.L.; Altman, R.B. DNATwist: A web-based tool for teaching middle and high school students about pharmacogenomics. Clin. Pharm. 2010, 87, 393–395. [Google Scholar] [CrossRef] [Green Version]
- Gálvez-Peralta, M.; Szklarz, G.D.; Geldenhuys, W.J.; Lockman, P.R. An effective approach to teaching pharmacogenomics in the first year of pharmacy curriculum. Am. J. Pharm. Educ. 2018, 82, 6345. [Google Scholar] [CrossRef]
- Hoehndorf, R.; Dumontier, M.; Gkoutos, G.V. Identifying aberrant pathways through integrated analysis of knowledge in pharmacogenomics. Bioinformatics 2012, 28, 2169–2175. [Google Scholar] [CrossRef]
- Duong, B.Q.; Arwood, M.J.; Hicks, J.K.; Beitelshees, A.L.; Franchi, F.; Houder, J.T.; Limdi, N.A.; Cook, K.J.; Obeng, A.O.; Petry, N.; et al. Development of customizable implementation guides to support clinical adoption of pharmacogenomics: Experiences of the implementing genomics in practice (ignite) network. Pharmgenomics Pers. Med. 2020, 13, 217–226. [Google Scholar] [CrossRef]
- Van Den Boom, D.; Wjst, M.; Everts, R.E. Chapter 4: MALDI-TOF mass spectrometry. Methods Mol. Biol. 2013, 1015, 71–85. [Google Scholar] [CrossRef]
- Barh, D.; Dhawan, D.; Ganguly, N.K. Omics for personalized medicine. Omics Pers. Med. 2013, 1–832. [Google Scholar] [CrossRef]
- Ta, R.; Cayabyab, M.A.S.; Coloso, R. Precision medicine: A call for increased pharmacogenomic education. Pers. Med. 2019, 16, 233–245. [Google Scholar] [CrossRef]
- Mitropoulou, C.; Litinski, V.; Kabakchiev, B.; Rogers, S.; Patrinos, G.P. PARC report: Health outcomes and value of personalized medicine interventions: Impact on patient care. Pharmacogenomics 2020. [Google Scholar] [CrossRef]
- Knowles, L.; Luth, W.; Bubela, T. Paving the road to personalized medicine: Recommendations on regulatory, intellectual property and reimbursement challenges. J. Law Biosci. 2017, 4, 453–506. [Google Scholar] [CrossRef] [Green Version]




| Count (%) | |
|---|---|
| Gender | |
| Female | 421 (82.7%) |
| Male | 88 (17.3%) |
| Age Group | |
| <18 | 69 (13.5%) |
| 18–28 | 388 (76.1%) |
| 29–39 | 38 (7.5%) |
| 40–50 | 6 (1.2%) |
| University Location | |
| Al Ain | 245 (68.6%) |
| Dubai | 83 (16.5%) |
| Sharjah | 55 (10.9%) |
| Abu Dhabi | 17 (3.4%) |
| Ajman | 1 (0.2%) |
| Fujairah | 1 (0.2%) |
| Ras Al Khaimah | 1 (0.2%) |
| Program | |
| Medicine | 265 (52.2%) |
| Pharmacy | 149 (29.3%) |
| Laboratory | 35 (6.9%) |
| Other a | 59 (11.6%) |
| Knowledge Questions | Correct Answer | Answered “True” n (%) | Answered “False” n (%) | Answered “Do not Know” n (%) |
|---|---|---|---|---|
| 1. Humans have 48 chromosomes. | False | 149 | 350 | 7 |
| (29.4%) | (69.2%) | (1.4%) | ||
| 2. Adenine (A) only pairs with cytosine (C) and Thymine (T) only pairs with Guanine (G). | False | 79 | 385 | 42 |
| (15.6%) | (76.1%) | (8.3%) | ||
| 3. Pharmacogenomics seeks to individualize therapy based on patient’s genetic profile. | True | 418 | 12 | 76 |
| (82.6%) | (2.4%) | (15%) | ||
| 4. Genetic changes can cause adverse reactions. | True | 426 | 20 | 60 |
| (84.2%) | (4.0%) | (11.9%) | ||
| 5. Pharmacogenomics testing is recommended by FDA for certain drugs. | True | 261 | 25 | 220 |
| (51.6%) | (4.9%) | (43.5%) | ||
| 6. Genetic changes can affect the patient’s response to certain drug. | True | 455 | 11 | 40 |
| (89.9%) | (2.2%) | (7.9%) | ||
| 7. Genes can be activated or deactivated by other genes. | True | 412 | 16 | 78 |
| (81.4%) | (3.2%) | (15.4%) | ||
| 8. Every cell of the body contains the whole genome. | False | 314 | 112 | 80 |
| (62.1%) | (22.1%) | (15.8%) | ||
| 9. Environmental factors, such as cigarette smoke, can affect gene activity. | True | 423 | 43 | 40 |
| (83.6%) | (8.5%) | (7.9%) |
| Level of Knowledge | |||||
|---|---|---|---|---|---|
| Mean Score (± SD) | Good | Fair | Poor | p-Value | |
| Overall | 5.4 (± 2.7) | 219 (42.9%) | 191 (37.5%) | 100 (19.6%) | |
| Gender | 0.47 | ||||
| Female | 5.3 (± 2.7) | 176 (41.8%) | 161 (38.2%) | 84 (20.0%) | |
| Male | 5.6 (± 2.6) | 43 (48.9%) | 30 (34.1%) | 15 (17.0%) | |
| Age group | 0.56 | ||||
| <18 | 5.0 (± 2.5) | 23 (33.3%) | 31 (44.9%) | 15 (21.7%) | |
| 18–28 | 5.5 (± 2.8) | 177 (45.6%) | 137 (35.3%) | 74 (19.1%) | |
| 29–39 | 5.3 (± 2.8) | 14 (36.8%) | 16 (42.1%) | 8 (21.1%) | |
| 40–50 | 5.0 (± 2.6) | 2 (33.3%) | 3 (50.0%) | 1 (16.7%) | |
| Program | 0.12 | ||||
| Medicine | 5.5 (± 2.7) | 123 (46.4%) | 95 (35.8%) | 47 (17.7%) | |
| Pharmacy | 5.6 (± 2.7) | 69 (46.3%) | 52 (34.9%) | 28 (18.8%) | |
| Laboratory | 4.7 (± 2.9) | 11 (31.4%) | 15 (42.9%) | 9 (25.7%) | |
| Other | 4.8 (± 2.4) | 16 (27.1%) | 29 (49.2%) | 14 (23.7%) | |
| Degree | 0.44 | ||||
| Bachelor | 6.4 (± 1.7) | 185 (44.5%) | 148 (35.6%) | 83 (20.0%) | |
| Master | 5.9 (± 1.5) | 14 (33.3%) | 20 (47.6%) | 8 (19.0%) | |
| PhD | 6.6 (± 1.2) | 19 (40.4%) | 20 (42.6%) | 8 (17.0%) | |
| Other | 5.8 (± 1.0) | 1 (25.0%) | 3 (75.0%) | 0 (0.0%) | |
| Year of study (Bachelor) | 0.00 * | ||||
| First | 5.1 (± 2.0) | 11 (5.9%) | 29 (19.6%) | 13 (15.7%) | |
| Second | 6.4 (± 1.7) | 37 (20.0%) | 22 (14.9%) | 15 (18.1%) | |
| Third | 7.0 (± 1.4) | 52 (28.1%) | 26 (17.6%) | 22 (26.5%) | |
| Fourth | 6.6 (± 1.6) | 55 (29.7%) | 35 (26.3%) | 20 (24.1%) | |
| Fifth | 6.5 (± 1.5) | 23 (12.4%) | 12 (8.1%) | 7 (8.4%) | |
| Sixth | 6.1 (± 1.3) | 5 (2.7%) | 12 (8.1%) | 3 (3.6%) | |
| Other | 5.8 (± 1.2) | 2 (1.1%) | 12 (8.1%) | 3 (3.6%) | |
| Year of study (Master) | 0.35 | ||||
| First | 5.8 (± 1.4) | 5 (35.7%) | 9 (45.0%) | 3 (37.5%) | |
| Second | 5.8 (± 1.6) | 5 (35.7%) | 10 (50.0%) | 3 (37.5%) | |
| Third | 6.3 (± 1.2) | 2 (14.3%) | 1 (5.0%) | 2 (25.0%) | |
| Other | 7.5 (± 0.7) | 2 (14.3%) | 0 (0.0%) | 0 (0.0%) | |
| Year of study (PhD) | 0.08 | ||||
| First | 6.2 (± 1.1) | 7 (36.8%) | 12 (60.0%) | 1 (12.5%) | |
| Second | 6.9 (± 1.2) | 5 (26.3%) | 4 (20.0%) | 1 (12.5%) | |
| Third | 7.0 (± 1.3) | 3 (15.8%) | 3 (15.0%) | 2 (25.0%) | |
| Fourth | 7.5 (± 0.6) | 4 (21.1%) | 0 (0.0%) | 4 (50.0%) | |
| Fifth | 5.0 (± 0.0) | 0 (0.0%) | 1 (5.0%) | 0 (0.0%) | |
| Previous exposure to genetic issues | 0.56 | ||||
| Yes | 5.9 (± 2.1) | 94 (45.2%) | 92 (44.2%) | 22 (10.6%) | |
| No | 6.0 (± 2.2) | 125 (49.6%) | 99 (39.3%) | 28 (11.1%) | |
| Completed PGX/pharmacogenetics training or education | 0.00 * | ||||
| Yes | 6.5 (± 2.2) | 110 (62.5%) | 51 (29.0%) | 15 (8.5%) | |
| No | 5.6 (± 2.1) | 109 (38.4%) | 140 (49.3%) | 35 (12.3%) | |
| Completed internship or study abroad program | 0.00 * | ||||
| Yes | 5.9 (± 2.2) | 191 (47.0%) | 169 (41.6%) | 46 (11.3%) | |
| No | 3.2 (± 3.4) | 29 (27.4%) | 22 (20.8%) | 55 (51.9%) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rahma, A.T.; Elsheik, M.; Elbarazi, I.; Ali, B.R.; Patrinos, G.P.; Kazim, M.A.; Alfalasi, S.S.; Ahmed, L.A.; Al Maskari, F. Knowledge and Attitudes of Medical and Health Science Students in the United Arab Emirates toward Genomic Medicine and Pharmacogenomics: A Cross-Sectional Study. J. Pers. Med. 2020, 10, 191. https://doi.org/10.3390/jpm10040191
Rahma AT, Elsheik M, Elbarazi I, Ali BR, Patrinos GP, Kazim MA, Alfalasi SS, Ahmed LA, Al Maskari F. Knowledge and Attitudes of Medical and Health Science Students in the United Arab Emirates toward Genomic Medicine and Pharmacogenomics: A Cross-Sectional Study. Journal of Personalized Medicine. 2020; 10(4):191. https://doi.org/10.3390/jpm10040191
Chicago/Turabian StyleRahma, Azhar T., Mahanna Elsheik, Iffat Elbarazi, Bassam R. Ali, George P. Patrinos, Maitha A. Kazim, Salma S. Alfalasi, Luai A. Ahmed, and Fatma Al Maskari. 2020. "Knowledge and Attitudes of Medical and Health Science Students in the United Arab Emirates toward Genomic Medicine and Pharmacogenomics: A Cross-Sectional Study" Journal of Personalized Medicine 10, no. 4: 191. https://doi.org/10.3390/jpm10040191