Time-Dependent Changes of Klotho and FGF-23 Levels after Kidney Transplantation: Role of Cold Ischemia Time, Renal Function and Graft Inflammation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Measurements of Serum Klotho and FGF-23
2.4. Histological Data
2.5. Statistical Analysis
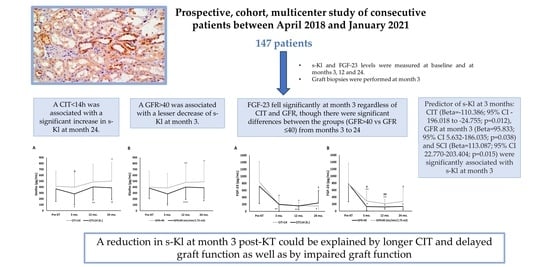
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hu, M.C.; Shi, M.; Zhang, J.; Addo, T.; Cho, H.J.; Barker, S.L.; Ravikumar, P.; Gillings, N.; Bian, A.; Sidhu, S.S.; et al. Renal Production, Uptake, and Handling of Circulating αKlotho. J. Am. Soc. Nephrol. 2016, 27, 79–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thongprayoon, C.; Neyra, J.A.; Hansrivijit, P.; Medaura, J.; Leeaphorn, N.; Davis, P.W.; Kaewput, W.; Bathini, T.; Salim, S.A.; Chewcharat, A.; et al. Serum Klotho in Living Kidney Donors and Kidney Transplant Recipients: A Meta-Analysis. J. Clin. Med. 2020, 9, 1834. [Google Scholar] [CrossRef] [PubMed]
- Gupta, M.; Orozco, G.; Rao, M.; Gedaly, R.; Malluche, H.H.; Neyra, J.A. The Role of Alterations in Alpha-Klotho and FGF-23 in Kidney Transplantation and Kidney Donation. Front. Med. 2022, 9, 803016. [Google Scholar] [CrossRef] [PubMed]
- Moreno, J.A.; Izquierdo, M.C.; Sanchez-Niño, M.D.; Suárez-Alvarez, B.; Lopez-Larrea, C.; Jakubowski, A.; Blanco, J.; Ramirez, R.; Selgas, R.; Ruiz-Ortega, M.; et al. The inflammatory cytokines TWEAK and TNFα reduce renal klotho expression through NFκB. J. Am. Soc. Nephrol. 2011, 22, 1315–1325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakanishi, K.; Nishida, M.; Harada, M.; Ohama, T.; Kawada, N.; Murakami, M.; Moriyama, T.; Yamauchi-Takihara, K. Klotho-related Molecules Upregulated by Smoking Habit in Apparently Healthy Men: A Cross-sectional Study. Sci. Rep. 2015, 5, 14230. [Google Scholar] [CrossRef] [Green Version]
- Maekawa, Y.; Ishikawa, K.; Yasuda, O.; Oguro, R.; Hanasaki, H.; Kida, I.; Takemura, Y.; Ohishi, M.; Katsuya, T.; Rakugi, H. Klotho suppresses TNF-alpha-induced expression of adhesion molecules in the endothelium and attenuates NF-kappaB activation. Endocrine 2009, 35, 341–346. [Google Scholar] [CrossRef]
- Tan, S.J.; Crosthwaite, A.; Langsford, D.; Obeysekere, V.; Ierino, F.L.; Roberts, M.A.; Hughes, P.D.; Hewitson, T.D.; Dwyer, K.M.; Toussaint, N.D. Mineral adaptations following kidney transplantation. Transpl. Int. 2017, 30, 463–473. [Google Scholar] [CrossRef] [Green Version]
- Ishida, H.; Nakamura, M.; Komaba, H.; Uehara, S.; Takiguchi, S.; Fukagawa, M. Post-kidney transplant soluble Klotho levels are determined by pretransplant soluble Klotho levels in both living donors and recipients. Clin. Exp. Nephrol. 2021, 25, 1367–1374. [Google Scholar] [CrossRef]
- Ferreira, A.C.; Mendes, M.; Silva, C.; Cotovio, P.; Aires, I.; Navarro, D.; Caeiro, F.; Ramos, R.; Salvador, R.; Correia, B.; et al. Improvement of Mineral and Bone Disorders After Renal Transplantation. Transplantation 2022, 106, e251–e261. [Google Scholar] [CrossRef]
- Kozakowski, N.; Herkner, H.; Eskandary, F.; Eder, M.; Winnicki, W.; Kläger, J.; Bond, G.; Kikic, Ž. An integrative approach for the assessment of peritubular capillaritis extent and score in low-grade microvascular inflammation-associations with transplant glomerulopathy and graft loss. Nephrol. Dial. Transpl. 2019, 34, 166–174. [Google Scholar] [CrossRef]
- Loupy, A.; Haas, M.; Solez, K.; Racusen, L.; Glotz, D.; Seron, D.; Nankivell, B.J.; Colvin, R.B.; Afrouzian, M.; Akalin, E.; et al. The Banff 2015 Kidney Meeting Report: Current Challenges in Rejection Classification and Prospects for Adopting Molecular Pathology. Am. J. Transpl. 2017, 17, 28–41. [Google Scholar] [CrossRef]
- Mehta, R.; Bhusal, S.; Randhawa, P.; Sood, P.; Cherukuri, A.; Wu, C.; Puttarajappa, C.; Hoffman, W.; Shah, N.; Mangiola, M.; et al. Short-term adverse effects of early subclinical allograft inflammation in kidney transplant recipients with a rapid steroid withdrawal protocol. Am. J. Transpl. 2018, 18, 1710–1717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rush, D.; Arlen, D.; Boucher, A.; Busque, S.; Cockfield, S.M.; Girardin, C.; Knoll, G.; Lachance, J.G.; Landsberg, D.; Shapiro, J.; et al. Lack of benefit of early protocol biopsies in renal transplant patients receiving TAC and MMF: A randomized study. Am. J. Transpl. 2007, 7, 2538–2545. [Google Scholar] [CrossRef] [PubMed]
- Castellano, G.; Intini, A.; Stasi, A.; Divella, C.; Gigante, M.; Pontrelli, P.; Franzin, R.; Accetturo, M.; Zito, A.; Fiorentino, M.; et al. Complement Modulation of Anti-Aging Factor Klotho in Ischemia/Reperfusion Injury and Delayed Graft Function. Am. J. Transpl. 2016, 16, 325–333. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, M.C.; Shi, M.; Zhang, J.; Quiñones, H.; Kuro-o, M.; Moe, O.W. Klotho deficiency is an early biomarker of renal ischemia-reperfusion injury and its replacement is protective. Kidney Int. 2010, 78, 1240–1251. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sun, C.Y.; Chang, S.C.; Wu, M.S. Suppression of Klotho expression by protein-bound uremic toxins is associated with increased DNA methyltransferase expression and DNA hypermethylation. Kidney Int. 2012, 81, 640–650. [Google Scholar] [CrossRef] [Green Version]
- Muñoz-Castañeda, J.R.; Herencia, C.; Pendón-Ruiz de Mier, M.V.; Rodriguez-Ortiz, M.E.; Diaz-Tocados, J.M.; Vergara, N.; Martínez-Moreno, J.M.; Salmerón, M.D.; Richards, W.G.; Felsenfeld, A.; et al. Differential regulation of renal Klotho and FGFR1 in normal and uremic rats. FASEB J. 2017, 31, 3858–3867. [Google Scholar] [CrossRef] [Green Version]
- Hernández, D.; Vázquez, T.; Alonso-Titos, J.; León, M.; Caballero, A.; Cobo, M.A.; Sola, E.; López, V.; Ruiz-Esteban, P.; Cruzado, J.M.; et al. Impact of HLA Mismatching on Early Subclinical Inflammation in Low-Immunological-Risk Kidney Transplant Recipients. J. Clin. Med. 2021, 10, 1934. [Google Scholar] [CrossRef]
- Mehta, R.B.; Tandukar, S.; Jorgensen, D.; Randhawa, P.; Sood, P.; Puttarajappa, C.; Zeevi, A.; Tevar, A.D.; Hariharan, S. Early subclinical tubulitis and interstitial inflammation in kidney transplantation have adverse clinical implications. Kidney Int. 2020, 98, 436–447. [Google Scholar] [CrossRef]
- Alvarez-Cienfuegos, A.; Cantero-Nieto, L.; Garcia-Gomez, J.A.; Robledo, G.; González-Gay, M.A.; Ortego-Centeno, N. FGF23-Klotho axis in patients with rheumatoid arthritis. Clin. Exp. Rheumatol. 2020, 38, 50–57. [Google Scholar]
- Martín-González, C.; Espelosín-Ortega, E.; Abreu-González, P.; Fernández-Rodríguez, C.; Vera-Delgado, V.E.; González-Navarrete, L.; García-Rodríguez, A.; Riera, A.M.; González-Reimers, E. Klotho Levels and Their Relationship with Inflammation and Survival among Alcoholic Patients. Biomolecules 2022, 12, 1151. [Google Scholar] [CrossRef] [PubMed]
- Abdelmalik, P.A.; Stevens, R.D.; Singh, S.; Skinner, J.; Carhuapoma, J.R.; Noel, S.; Johns, R.; Fuchs, R.J. Anti-aging factor, serum alpha-Klotho, as a marker of acute physiological stress, and a predictor of ICU mortality, in patients with septic shock. J. Crit. Care 2018, 44, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.D.; Podvin, S.; Gillespie, E.; Leeman, S.E.; Abraham, C.R. Insulin stimulates the cleavage and release of the extracellular domain of Klotho by ADAM10 and ADAM17. Proc. Natl. Acad. Sci. USA 2007, 104, 19796–19801. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.D.; Tung, T.Y.; Liang, J.; Zeldich, E.; Tucker Zhou, T.B.; Turk, B.E.; Abraham, C.R. Identification of cleavage sites leading to the shed form of the anti-aging protein klotho. Biochemistry 2014, 53, 5579–5587. [Google Scholar] [CrossRef] [Green Version]


| N = 146 | |
|---|---|
| Donor age (years) | 56.4 ± 11.6 |
| Expanded criteria donor, n (%) | 77 (52.7) |
| Donor after cardiac death, n (%) | 46 (31.5) |
| Recipient age (years) | 55.9 ± 12.7 |
| Recipient weight (kg) | 73.1 ± 14.4 |
| Recipient BMI (kg/m2) | 22.3 ± 7.3 |
| Male, n (%) | 93 (63.7) |
| Prior CVD, n (%) | 20 (13.7) |
| Hemodialysis, n (%) | 120 (82.2) |
| Current smoker, n (%) | 18 (12.6) |
| Cause of ESRD, n (%) | |
| Glomerulonephritis | 23 (15.8) |
| Diabetes | 24 (16.4) |
| ADPKD | 25 (17.1) |
| Interstitial nephropathy | 7 (4.8) |
| Autoimmune | 5 (3.4) |
| Nephrosclerosis | 11 (7.5) |
| Unknown | 36 (24.7) |
| Other | 15 (10.3) |
| Induction therapy, n (%) | |
| None | 22 (15.1) |
| Basiliximab | 51 (34.9) |
| Thymoglobulin | 73 (50) |
| CIT (h) | 13.4 ± 3.5 |
| Re-transplantation, n (%) | 12 (8.2) |
| DGF, n (%) | 51 (35.4) |
| Diabetes, n (%) | 38 (26) |
| Hypertension, n (%) | 125 (85.6) |
| Maximum PRA (%) | 16.7 ± 33.8 |
| Total HLA mismatches (n) | 6.9 ± 1.7 |
| Previous transfusions (n) | 0.23 ± 0.42 |
| Serum calcium (mg/dL) | 7.9 ± 0.6 |
| Serum phosphate (mg/dL) | 5.6 ± 1.6 |
| PTH (pg/mL) | 425.1 ± 331.5 |
| Serum klotho levels (pg/mL) | 434.5 ± 253.3 |
| Serum FGF-23 levels (pg/mL) | 780.6 ± 568.3 |
| Serum TNF levels (pg/mL) | 8.8 ± 13.8 |
| Serum TWEAK levels (pg/mL) | 437.5 ± 269.6 |
| Vitamin D treatment, n (%) | 40 (27.4) |
| CIT < 14 h (n = 75) | CIT ≥ 14 h (n = 71) | p | |
|---|---|---|---|
| Donor age (years) | 56.2 ± 12.4 | 55.6 ± 13.1 | 0.786 |
| Expanded criteria donor, n (%) | 41 (54.7) | 36 (50.7) | 0.632 |
| Donor after cardiac death, n (%) | 29 (38.7) | 17 (23.9) | 0.056 |
| Recipient age (years) | 56 ± 12.5 | 56.7 ± 10.7 | 0.727 |
| Recipient weight (kg) | 71.3 ± 12.5 | 76.2 ± 19.6 | 0.079 |
| Recipient BMI (kg/m2) | 21.5 ± 3.2 | 23.3 ± 9.9 | 0.164 |
| Male, n (%) | 43 (57.3) | 50 (70.4) | 0.100 |
| Prior CVD, n (%) | 9 (12) | 11 (15.5) | 0.540 |
| Hemodialysis, n (%) | 60 (80) | 60 (84.5) | 0.328 |
| Current smoker, n (%) | 6 (8.1) | 12 (17.4) | 0.246 |
| Cause of ESRD, n (%) | 0.340 | ||
| Glomerulonephritis | 13 (17.3) | 10 (14.1) | |
| Diabetes | 11 (14.7) | 13 (18.3) | |
| ADPKD | 13 (17.3) | 12 (16.9) | |
| Interstitial nephropathy | 5 (6.7) | 2 (2.8) | |
| Autoimmune | 5 (6.7) | 0 (0) | |
| Nephrosclerosis | 6 (8) | 5 (7) | |
| Unknown | 16 (21.3) | 20 (28.2) | |
| Other | 6 (8) | 9 (12.7) | |
| Induction therapy, n (%) | 0.023 | ||
| None | 8 (10.7) | 14 (18.6) | |
| Basiliximab | 21 (28) | 30 (42.9) | |
| Thymoglobulin | 46 (61.3) | 27 (38.6) | |
| PTDM, n (%) | 21 (27.9) | 24 (34.2) | 0.540 |
| Maximum PRA (%) | 17.2 ± 33.9 | 16.3 ± 33.9 | 0.871 |
| DGF, n (%) | 18 (24.3) | 33 (47.1) | 0.004 |
| Acute rejection, n (%) | 12 (15.7) | 17 (23.9) | 0.308 |
| Glycemia (mg/dL) | 114.2 ± 69.9 | 105.2 ± 44.9 | 0.373 |
| HbA1c (%) | 6.03 ± 1.4 | 6.02 ± 0.9 | 0.988 |
| Total cholesterol (mg/dL) | 175.8 ± 39.1 | 169.5 ± 42.9 | 0.400 |
| HDL cholesterol (mg/dL) | 55.5 ± 17.4 | 48.9 ± 15.9 | 0.035 |
| LDL cholesterol (mg/dL) | 91.9 ± 33.2 | 89.4 ± 29.8 | 0.677 |
| Triglycerides (mg/dL) | 136.1 ± 73.6 | 152.2 ± 84.6 | 0.260 |
| Serum calcium (mg/dL) | 9.3 ± 0.5 | 9.3 ± 0.7 | 0.685 |
| Serum phosphate (mg/dL) | 3.2 ± 0.7 | 3.3 ± 0.7 | 0.166 |
| FEPhos (%) | 31.5 ± 14.4 | 34.6 ± 16.5 | 0.300 |
| PTH (pg/mL) | 103.8 ± 64.4 | 114.7 ± 89.1 | 0.442 |
| Hypertension, n (%) | 66 (88.0) | 59 (83.1) | 0.399 |
| SBP (mmHg) | 125.7 ± 10.8 | 128.9 ± 10.9 | 0.104 |
| DBP (mmHg) | 72.4 ± 8.6 | 73.2 ± 7.8 | 0.573 |
| Tacrolimus levels (ng/mL) | 9.8 ± 3.4 | 9.8 ± 3.3 | 0.939 |
| Previous transfusions (n) | 0.22 ± 0.42 | 0.25 ± 0.43 | 0.704 |
| Total HLA mismatches (n) | 6.9 ± 1.8 | 7.01 ± 1.7 | 0.605 |
| Proteinuria (mg/24 h.) | 328 ± 324.6 | 358.6 ± 390.7 | 0.732 |
| eGFR CKD-EPI (mL/min/1.73 m2) | 45.5 ± 15.4 | 40.2 ± 17.2 | 0.072 |
| ΔCr (mg/dL) | −0.17 ± 0.36 | −0.37 ± 0.55 | 0.014 |
| Serum klotho levels (pg/mL) | 420.8 ± 241.8 | 318.2 ± 215.3 | 0.052 |
| Serum FGF-23 levels (pg/mL) | 174.8 ± 217.5 | 246.9 ± 371.8 | 0.340 |
| Serum TNF levels (pg/mL) | 7.1 ± 10.7 | 3.7 ± 5.3 | 0.096 |
| Serum TWEAK levels (pg/mL) | 444 ± 363.7 | 418.9 ± 218.1 | 0.738 |
| Vitamin D treatment, n (%) | 20 (27.8) | 20 (29) | 0.614 |
| GFR ≤ 40 (n = 55) | GFR > 40 (n = 68) | p | |
|---|---|---|---|
| Donor age (years) | 58.7 ± 9.7 | 53.9 ± 12.1 | 0.018 |
| Expanded criteria donor, n (%) | 36 (65.5) | 29 (42.6) | 0.012 |
| Donor after cardiac death, n (%) | 16 (29.1) | 20 (29.4) | 0.969 |
| Recipient age (years) | 56.3 ± 11.1 | 54.4 ± 14 | 0.426 |
| Recipient weight (kg) | 75.5 ± 15.5 | 72.6 ± 18.5 | 0.354 |
| Recipient BMI (kg/m2) | 22.4 ± 4.2 | 22.5 ± 9.8 | 0.938 |
| Male, n (%) | 37 (67.3) | 41 (60.3) | 0.242 |
| Prior CVD, n (%) | 5 (9.1) | 10 (14.7) | 0.344 |
| Hemodialysis, n (%) | 46 (83.6) | 55 (80.9) | 0.898 |
| Current smoker, n (%) | 6 (10.9) | 9 (13.4) | 0.243 |
| Cause of ESRD, n (%) | 0.260 | ||
| Glomerulonephritis | 6 (10.9) | 11 (16.2) | |
| Diabetes | 14 (25.5) | 7 (10.3) | |
| ADPKD | 10 (18.2) | 11 (16.2) | |
| Interstitial nephropathy | 1 (1.8) | 4 (5.9) | |
| Autoimmune | 1 (1.8) | 4 (5.9) | |
| Nephrosclerosis | 5 (9.1) | 4 (5.9) | |
| Unknown | 11 (20) | 20 (29.4) | |
| Other | 7 (12.7) | 7 (10.3) | |
| Induction therapy, n (%) | 0.165 | ||
| None | 5 (9.1) | 11 (16.4) | |
| Basiliximab | 24 (43.6) | 19 (28.4) | |
| Thymoglobulin | 26 (47.3) | 38 (55.2) | |
| CIT (h) | 14 ± 3.5 | 13.1 ± 3.5 | 0.141 |
| PTDM, n (%) | 19 (34.5) | 20 (30) | 0.680 |
| DGF, n (%) | 28 (50.9) | 16 (23.5) | 0.002 |
| Acute rejection, n (%) | 17 (30) | 6 (8.3) | 0.009 |
| Maximum PRA (%) | 13.9 ± 29.7 | 20.4 ± 38.3 | 0.302 |
| Glycemia (mg/dL) | 110.5 ± 57.8 | 105.3 ± 52.2 | 0.601 |
| HbA1c (%) | 6.3 ± 1.4 | 5.8 ± 0.9 | 0.041 |
| Total cholesterol (mg/dL) | 169.1 ± 39.5 | 175.8 ± 42.2 | 0.398 |
| HDL cholesterol (mg/dL) | 49.1 ± 18.6 | 56 ± 15.9 | 0.042 |
| LDL cholesterol (mg/dL) | 85 ± 28.8 | 94.1 ± 33.7 | 0.148 |
| Triglycerides (mg/dL) | 156.7 ± 95.3 | 134.7 ± 62.1 | 0.161 |
| Serum calcium (mg/dL) | 9.2 ± 0.7 | 9.3 ± 0.5 | 0.836 |
| Serum phosphate (mg/dL) | 3.3 ± 0.8 | 3.2 ± 0.6 | 0.320 |
| FEPhos (%) | 28.6 ± 12.4 | 40.4 ± 16.6 | <0.001 |
| PTH (pg/mL) | 117.7 ± 96.3 | 101.0 ± 58.9 | 0.270 |
| Hypertension, n (%) | 45 (81.8) | 60 (88.2) | 0.317 |
| SBP (mmHg) | 129.5 ± 10.4 | 125.8 ± 11.6 | 0.093 |
| DBP (mmHg) | 73.8 ± 8.9 | 72.3 ± 7.9 | 0.352 |
| Tacrolimus levels (ng/mL) | 9.9 ± 3.8 | 9.7 ± 3.1 | 0.808 |
| Previous transfusions (n) | 0.24 ± 0.43 | 0.28 ± 0.45 | 0.658 |
| Total HLA mismatches (n) | 6.96 ± 1.8 | 6.97 ± 1.6 | 0.982 |
| Proteinuria (mg/24 h.) | 422.9 ± 508.6 | 256.2 ± 145.3 | 0.124 |
| eGFR CKD-EPI (mL/min/1.73 m2) | 29.2 ± 7.8 | 53.9 ± 12.9 | <0.001 |
| Serum klotho levels (pg/mL) | 304.9 ± 180.4 | 398.1 ± 244.8 | 0.079 |
| Serum FGF-23 levels (pg/mL) | 335.2 ± 422.9 | 121.4 ± 117 | 0.018 |
| Serum TNF levels (pg/mL) | 5.1 ± 6.2 | 5.9 ± 10.7 | 0.716 |
| Serum TWEAK levels (pg/mL) | 425.9 ± 338.3 | 445.9 ± 285.6 | 0.796 |
| Vitamin D treatment, n (%) | 18 (33.3) | 16 (23.9) | 0.255 |
| NI (n = 32) | SCI (N = 65) | p | |
|---|---|---|---|
| g (0–3) | 0.06 ± 0.35 | 0.23 ± 0.49 | 0.058 |
| ptc (0–3) | 0.38 ± 0.61 | 0.69 ± 0.66 | 0.028 |
| t (0–3) | 0.22 ± 0.42 | 1.34 ± 0.57 | <0.001 |
| i (0–3) | 0.22 ± 0.61 | 1.26 ± 0.48 | <0.001 |
| v (0–3) | 0 | 0.11 ± 0.48 | 0.070 |
| ci (0–3) | 0.34 ± 0.48 | 0.48 ± 0.62 | 0.248 |
| ct (0–3) | 0.31 ± 0.47 | 0.48 ± 0.62 | 0.149 |
| cg (0–3) | 0 | 0 | - |
| cv (0–3) | 0.75 ± 0.84 | 0.63 ± 0.82 | 0.507 |
| ah (0–3) | 0.34 ± 0.55 | 0.57 ± 0.75 | 0.096 |
| mm (0–3) | 0.06 ± 0.25 | 0.15 ± 0.51 | 0.235 |
| IFTA (0–3) | 0.22 ± 0.71 | 0.35 ± 0.72 | 0.383 |
| ct + ci | 0.66 ± 0.94 | 0.95 ± 1.22 | 0.188 |
| ct + ci + cg + cv | 1.41 ± 1.46 | 1.59 ± 1.64 | 0.603 |
| Tacrolimus levels (ng/mL) | 9.73 ± 3.16 | 9.41 ± 3.31 | 0.658 |
| Serum klotho levels (pg/mL) | 351.4 ± 210.4 | 386.2 ± 247.1 | 0.529 |
| FGF-23 levels (pg/mL) | 122.7 ± 63.1 | 197.4 ± 172.3 | 0.055 |
| Variable | Beta | Standardized Beta Coefficient | 95% CI | p Value |
|---|---|---|---|---|
| CIT (<14 h vs. ≥14 h) | −110.386 | −0.225 | −196.018–(−24.755) | 0.012 |
| Basal s-Kl (pg/mL) | 0.641 | 0.651 | 0.473–0.809 | 0.000 |
| Recipient age (y) | 1.708 | 0.084 | −1.755–5.171 | 0.328 |
| ECD (%) | −66.998 | −0.135 | −157.093–23.097 | 0.142 |
| SCI (%) | 113.087 | 0.212 | 22.770−203.404 | 0.015 |
| eGFR (>40 vs. ≤40 mL/min/1.73 m2) | 95.833 | 0.195 | 5.632−186.035 | 0.038 |
| FEPhos (%) | 2.062 | 0.129 | −1.068–5.192 | 0.193 |
| Proteinuria (mg/24 h) | 0.043 | 0.050 | −0.106–0.191 | 0.570 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vazquez-Sanchez, T.; Sanchez-Niño, M.D.; Ruiz-Esteban, P.; López, V.; León, M.; Caballero, A.; Ruiz-Escalera, J.F.; Ortiz, A.; Torres, A.; Rodriguez, M.; et al. Time-Dependent Changes of Klotho and FGF-23 Levels after Kidney Transplantation: Role of Cold Ischemia Time, Renal Function and Graft Inflammation. J. Clin. Med. 2023, 12, 4486. https://doi.org/10.3390/jcm12134486
Vazquez-Sanchez T, Sanchez-Niño MD, Ruiz-Esteban P, López V, León M, Caballero A, Ruiz-Escalera JF, Ortiz A, Torres A, Rodriguez M, et al. Time-Dependent Changes of Klotho and FGF-23 Levels after Kidney Transplantation: Role of Cold Ischemia Time, Renal Function and Graft Inflammation. Journal of Clinical Medicine. 2023; 12(13):4486. https://doi.org/10.3390/jcm12134486
Chicago/Turabian StyleVazquez-Sanchez, Teresa, Maria Dolores Sanchez-Niño, Pedro Ruiz-Esteban, Veronica López, Myriam León, Abelardo Caballero, Juan Francisco Ruiz-Escalera, Alberto Ortiz, Armando Torres, Mariano Rodriguez, and et al. 2023. "Time-Dependent Changes of Klotho and FGF-23 Levels after Kidney Transplantation: Role of Cold Ischemia Time, Renal Function and Graft Inflammation" Journal of Clinical Medicine 12, no. 13: 4486. https://doi.org/10.3390/jcm12134486