Factors Influencing Global Health Related Quality of Life in Elderly Cancer Patients: Results of a Secondary Data Analysis
Abstract
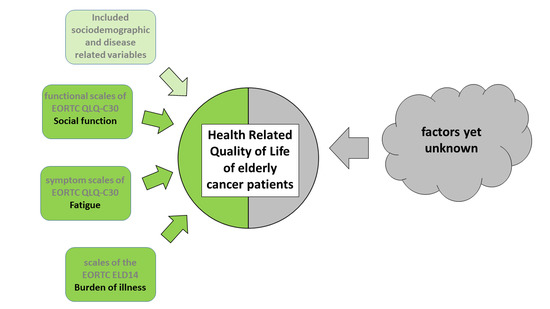
:1. Introduction
2. Material and Methods
2.1. HRQOL Questionnaires
2.2. Statistical Analyses
3. Results
Study Population
4. Discussion
4.1. Limitations of the Study
4.2. Implications for Future Research
Acknowledgements
Author Contributions
Conflicts of Interest
References
- Eichhorst, B.; Hallek, M.; Goede, V. New treatment approaches in CLL: Challenges and opportunities in the elderly. J. Geriatr. Oncol. 2016, 7, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Vigano, A.; Morais, J.A. The elderly patient with cancer: A holistic view. Nutrition 2015, 31, 587–589. [Google Scholar] [CrossRef] [PubMed]
- Burhenn, P.S.; McCarthy, A.L.; Begue, A.; Nightingale, G.; Cheng, K.; Kenis, C. Geriatric assessment in daily oncology practice for nurses and allied health care professionals: Opinion paper of the Nursing and Allied Health Interest Group of the International Society of Geriatric Oncology (SIOG). J. Geriatr. Oncol. 2016, 7, 315–324. [Google Scholar] [CrossRef] [PubMed]
- National Comprehensive Cancer Network (NCCN). Older Adult Oncology Version 2.2016; National Comprehensive Cancer Network: Fort Washington, PA, USA, 2016. [Google Scholar]
- Ferrans, C.E.; Zerwig, J.J.; Wilbur, J.E.; Larson, J.L. Conceptual Model of Health-Related Quality of Life. J. Nurs. Scholarsh. 2005, 37, 336–342. [Google Scholar] [CrossRef] [PubMed]
- Hollen, P.J.; Msaouel, P.; Gralla, R.J. Determining issues of importance for the evaluation of quality of life and patient-reported outcomes in breast cancer: Results of a survey of 1072 patients. Breast Cancer Res. Treat. 2015, 151, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Tremolada, M.; Taverna, L.; Bonichini, S.; Basso, G.; Pillon, M. Self-Esteem and Academic Difficulties in Preadolescents and Adolescents Healed from Paediatric Leukaemia. Cancers 2017, 9, 55. [Google Scholar] [CrossRef] [PubMed]
- Tremolada, M.; Bonichini, S.; Basso, G.; Pillon, M. Perceived social support and health-related quality of life in AYA cancer survivors and controls. Psychooncology 2016, 25, 1408–1417. [Google Scholar] [CrossRef] [PubMed]
- Meropol, N.J.; Egleston, B.L.; Buzaglo, J.S.; Benson, A.B.; Cegala, D.J.; Diefenbach, M.A.; Fleisher, L.; Miller, S.M.; Sulmasy, D.P.; Weinfurt, K.P. Cancer patient preferences for quality and length of life. Cancer 2008, 113, 3459–3466. [Google Scholar] [CrossRef] [PubMed]
- Baier, P.; Ihorst, G.; Wolff-Vorbeck, G.; Hull, M.; Hopt, U.; Deschler, B. Independence and health related quality of life in 200 onco-geriatric surgical patients within 6 months of follow-up: Who is at risk to lose? Eur. J. Surg. Oncol. 2016, 42, 1890–1897. [Google Scholar] [CrossRef] [PubMed]
- Puts, M.T.; Tapscott, B.; Fitch, M.; Howell, D.; Monette, J.; Wan-Chow-Wah, D.; Krzyzanowska, M.; Leighl, N.B.; Springall, E.; Alibhai, S.M. A systematic review of factors influencing older adults’ decision to accept or decline cancer treatment. Cancer Treat. Rev. 2015, 41, 197–215. [Google Scholar] [CrossRef] [PubMed]
- Wilson, I.B.; Cleary, P.D. Linking Clinical Variables with Health-Related Quality of Life: A Conceptual Model of Patient Outcomes. JAMA 1995, 273, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Fayers, P.M.; Hand, D.J.; Bjordal, K.; Groenvold, M. Causal indicators in quality of life research. Qual. Life Res. 1997, 6, 393–406. [Google Scholar] [CrossRef] [PubMed]
- Hamidou, Z.; Dabakuyo, T.S.; Bonnetain, F. Impact of response shift on longitudinal quality-of-life assessment in cancer clinical trials. Expert Rev. Pharmacoecon. Outcomes Res. 2011, 11, 549–559. [Google Scholar] [CrossRef] [PubMed]
- Dabakuyo, T.S.; Guillemin, F.; Conroy, T.; Velten, M.; Jolly, D.; Mercier, M.; Causeret, S.; Cuisenier, J.; Graesslin, O.; Gauthier, M.; et al. Response shift effects on measuring post-operative quality of life among breast cancer patients: A multicenter cohort study. Qual. Life Res. 2013, 22, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Donohoe, J.E. To what extent can response shift theory explain the variation in prostate cancer patients’ reactions to treatment side-effects? A review. Qual. Life Res. 2011, 20, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Sprangers, M.A.G.; Schwartz, C.E. Integrating response shift into health-related quality of life research. Soc. Sci. Med. 1999, 48, 1507–1515. [Google Scholar] [CrossRef]
- Hinz, A.; Mehnert, A.; Dégi, C.; Reissmann, D.R.; Schotte, D.; Schulte, T. The relationship between global and specific components of quality of life, assessed with the EORTC QLQ-C30 in a sample of 2019 cancer patients. Eur. J. Cancer Care 2017, 26. [Google Scholar] [CrossRef] [PubMed]
- Giesinger, J.M.; Kieffer, J.M.; Fayers, P.M.; Groenvold, M.; Petersen, M.A.; Scott, N.W.; Sprangers, M.A.G.; Velikova, G.; Aaronson, N.K. Replication and validation of higher order models demonstrated that a summary score for the EORTC QLQ-C30 is robust. J. Clin. Epidemiol. 2016, 69, 79–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Efficace, F.; Rosti, G.; Breccia, M.; Cottone, F.; Giesinger, J.M.; Stagno, F.; Iurlo, A.; Russo Rossi, A.; Luciano, L.; Martino, B.; et al. The impact of comorbidity on health-related quality of life in elderly patients with chronic myeloid leukemia. Ann. Hematol. 2016, 95, 211–219. [Google Scholar] [CrossRef] [PubMed]
- McCabe, R.M.; Grutsch, J.F.; Braun, D.P.; Nutakki, S.B. Fatigue as a Driver of Overall Quality of Life in Cancer Patients. PLoS ONE 2015, 10, e0130023. [Google Scholar] [CrossRef] [PubMed]
- Cramarossa, G.; Chow, E.; Zhang, L.; Bedard, G.; Zeng, L.; Sahgal, A.; Vassiliou, V.; Satoh, T.; Foro, P.; Ma, B.B.; et al. Predictive factors for overall quality of life in patients with advanced cancer. Support. Care Cancer 2013, 21, 1709–1716. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, A.M.; Mayo, N.E.; Gagnon, B. Independent contributors to overall quality of life in people with advanced cancer. Br. J. Cancer 2013, 108, 1790–1800. [Google Scholar] [CrossRef] [PubMed]
- Quinten, C.; Coens, C.; Ghislain, I.; Zikos, E.; Sprangers, M.A.; Ringash, J.; Martinelli, F.; Ediebah, D.E.; Maringwa, J.; Reeve, B.B.; et al. The effects of age on health-related quality of life in cancer populations: A pooled analysis of randomized controlled trials using the European Organisation for Research and Treatment of Cancer (EORTC) QLQ-C30 involving 6024 cancer patients. Eur. J. Cancer 2015, 51, 2808–2819. [Google Scholar] [CrossRef] [PubMed]
- Mohile, S.G.; Heckler, C.; Fan, L.; Mustian, K.; Jean-Pierre, P.; Usuki, K.; Sprod, L.; Janelsins, M.; Purnell, J.; Peppone, L.; et al. Age-related Differences in Symptoms and Their Interference with Quality of Life in 903 Cancer Patients Undergoing Radiation Therapy. J. Geriatr. Oncol. 2011, 2, 225–232. [Google Scholar] [CrossRef] [PubMed]
- Waldmann, A.; Schubert, D.; Katalinic, A. Normative data of the EORTC QLQ-C30 for the German population: A population-based survey. PLoS ONE 2013, 8, e74149. [Google Scholar] [CrossRef] [PubMed]
- Wheelwright, S.; Darlington, A.S.; Fitzsimmons, D.; Fayers, P.; Arraras, J.I.; Bonnetain, F.; Brain, E.; Bredart, A.; Chie, W.C.; Giesinger, J.; et al. International validation of the EORTC QLQ-ELD14 questionnaire for assessment of health-related quality of life elderly patients with cancer. Br J. Cancer 2013, 109, 852–858. [Google Scholar] [CrossRef] [PubMed]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; Haes, J.C.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef] [PubMed]
- EORTC Quality of Life Group. EORTC QLQ-C30 Scoring Manual, 3rd ed.; EORTC Quality of Life Group: Brussels, Belgium, 2001. [Google Scholar]
- Van der Poel, M.W.M.; Oerlemans, S.; Schouten, H.C.; van de Poll-Franse, L.V. Elderly multiple myeloma patients experience less deterioration in health-related quality of life than younger patients compared to a normative population: A study from the population-based PROFILES registry. Ann. Hematol. 2015, 94, 651–661. [Google Scholar] [CrossRef] [PubMed]
- Gray, N.M.; Hall, S.J.; Browne, S.; Macleod, U.; Mitchell, E.; Lee, A.J.; Johnston, M.; Wyke, S.; Samuel, L.; Weller, D.; et al. Modifiable and fixed factors predicting quality of life in people with colorectal cancer. Br. J. Cancer 2011, 104, 1697–1703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liuu, E.; Canoui-Poitrine, F.; Tournigand, C.; Laurent, M.; Caillet, P.; Le Thuaut, A.; Vincent, H.; Culine, S.; Audureau, E.; Bastuji-Garin, S.; et al. Accuracy of the G-8 geriatric-oncology screening tool for identifying vulnerable elderly patients with cancer according to tumour site: The ELCAPA-02 study. J. Geriatr. Oncol. 2014, 5, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Scott, M. Applied Logistic Regression Analysis, 2nd ed.; Series: Quantitative Applications in the Social Sciences; Sage Publications: Thousand Oaks, CA, USA, 1997; Volume 106. [Google Scholar]
- Osoba, D. Interpreting the meaningfulness of changes in health-related quality of life scores: Lessons from studies in adults. Int. J. Cancer Suppl. 1999, 12, 132–137. [Google Scholar] [CrossRef]
- Sharma, M.; Loh, K.P.; Nightingale, G.; Mohile, S.G.; Holmes, H.M. Polypharmacy and potentially inappropriate medication use in geriatric oncology. J. Geriatr. Oncol. 2016, 7, 346–353. [Google Scholar] [CrossRef] [PubMed]
- Haugland, T.; Wahl, A.K.; Hofoss, D.; DeVon, H.A. Association between general self-efficacy, social support, cancer-related stress and physical health-related quality of life: A path model study in patients with neuroendocrine tumors. Health Qual. Life Outcomes 2016, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shelby, R.A.; Edmond, S.N.; Wren, A.A.; Keefe, F.J.; Peppercorn, J.M.; Marcom, P.K.; Blackwell, K.L.; Kimmick, G.G. Self-efficacy for coping with symptoms moderates the relationship between physical symptoms and well-being in breast cancer survivors taking adjuvant endocrine therapy. Support. Care Cancer 2014, 22, 2851–2859. [Google Scholar] [CrossRef] [PubMed]
| Sociodemographic Data | n = 518 | n = 341 |
|---|---|---|
| Sex | ||
| Male | 253 (48.8) | 173 (50.7) |
| Female | 264 (51.0) | 168 (49.3) |
| Missing | 1 (0.2) | 0 (0) |
| Age | Mean: 77.3; SD: 4.9 | Mean: 77.0; SD: 4.7 |
| <80 | 365 (70.5) | 246 (72.1) |
| 80–85 | 118 (22.8) | 78 (22.9) |
| >85 | 35 (6.8) | 17 (5.0) |
| Education | ||
| No education/primary education | 187 (36.1) | 136 (39.9) |
| Secondary education | 184 (35.5) | 119 (34.9) |
| College | 88 (17.0) | 50 (14.9) |
| University | 50 (9.7) | 34 (10.0) |
| Missing | 9 (1.7) | 2 (0.6) |
| Employment Level | ||
| Unskilled | 130 (25.1) | 102 (29.9) |
| Skilled | 155 (29.9) | 97 (28.4) |
| Admin | 125 (24.1) | 85 (24.9) |
| Professional | 85 (16.4) | 56 (16.4) |
| Missing | 23 (4.4) | 1 (0.3) |
| Living | ||
| Alone | 131 (25.3) | 78 (22.9) |
| With Family | 359 (69.3) | 278 (75.7) |
| Supported | 8 (1.5) | 5 (1.5) |
| Missing | 20 (3.9) | 0 (0) |
| Children | ||
| No children | 41 (7.9) | 20 (5.9) |
| One or more children | 459 (88.6) | 321 (94.1) |
| Missing | 18 (3.5) | 0 (0) |
| Carer Support | ||
| At home | 273 (52.7) | 192 (56.3) |
| Easily available | 136 (26.3) | 95 (27.9) |
| Not available | 55 (10.6) | 32 (9.4) |
| Carer for other | 18 (3.5) | 12 (3.5) |
| Missing | 36 (7.0) | 10 (2.9) |
| Disease and Therapy Related Data | n = 518 | n = 341 |
|---|---|---|
| Primary Cancer Localisation | ||
| Breast | 91 (17.6) | 58 (17.0) |
| Colorectal | 87 (16.8) | 63 (18.5) |
| Lung | 63 (12.2) | 52 (15.2) |
| Ovary | 23 (4.4) | 17 (5.0) |
| Prostate | 75 (14.5) | 53 (15.5) |
| Upper GI | 21 (4.1) | 14 (4.1) |
| Haematological | 54 (10.4) | 10 (2.9) |
| Other | 104 (20.1) | 74 (21.7) |
| Disease stage | ||
| Not metastatic | 306 (59.1) | 212 (62.2) |
| Metastatic | 176 (34.0) | 129 (37.8) |
| Missing | 36 (7.0) | 0 (0) |
| Disease Progression | ||
| Yes | 54 (10.4) | 39 (11.4) |
| No | 464 (89.6) | 302 (88.6) |
| Therapy | ||
| Surgery | 253 (48.8) | 190 (55.7) |
| Chemotherapy | 300 (57.9) | 211 (61.9) |
| Radiotherapy | 205 (39.6) | 133 (39.0) |
| Hormonal Therapy | 93 (18.0) | 61 (17.9) |
| Treatment Intention | ||
| Curative | 288 (55.6) | 208 (61.0) |
| Palliative | 189 (36.5) | 133 (39.0) |
| Missing | 41 (7.9) | 0 (0) |
| Toxicity Level of Therapy | ||
| Low | 484 (93.4) | 313 (91.8) |
| Severe | 34 (6.6) | 28 (8.2) |
| Missing | 36 (7.0) | 0 (0) |
| ECOG-Status | ||
| Good (0–2) | 434 (83.8) | 312 (91.5) |
| Poor (3,4) | 45 (8.7) | 29 (8.5) |
| Missing | 39 (7.5) | 0 (0) |
| Charlson Comorbidity Index | Mean: 0.7, SD: 1.1 | Mean: 0.6, SD: 1.0 |
| Number of comorbidities/patient | Min.: 0, Max.: 4 | Min.: 0, Max.: 4 |
| No Comorbidity (score 0) | 321 (62.0) | 213 (62.5) |
| At least one Comorbidity (score > 0) | 197 (38.0) | 128 (37.5) |
| Frequent Comorbidities | ||
| Cardiovascular disease | 104 (20.1) | 64 (18.8) |
| Diabetes | 72 (13.9) | 46 (13.5) |
| Pulmonary disease | 31 (6.0) | 18 (5.3) |
| Renal failure | 18 (3.5) | 9 (2.6) |
| Liver disease | 16 (3.1) | 11 (3.2) |
| G8 Items (dichotomized) | ||
| Food intake poor | 172 (33.2) | 118 (34.6) |
| Weight loss > 3 kg | 122 (23.6) | 88 (25.9) |
| Unable to leave the house | 87 (16.8) | 55 (16.1) |
| Dementia or depression | 52 (10.0) | 33 (9.7) |
| Malnutrition | 54 (10.4) | 40 (11.7) |
| >Three medications | 272 (52.5) | 190 (55.7) |
| Own health status perceived poor | 180 (34.7) | 128 (37.5) |
| Age > 80 | 161 (31.1) | 99 (29.0) |
| G8 total Score | M: 12.5, SD: 2.9 | M: 12.7, SD: 3.0 |
| Missing | 19 (3.7) | 0 (0) |
| Variable | Total Sample (n = 518) | Complete Data Sets Included in Analyses (n = 341) | ||
|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | |
| QLQ-C30 global health status | 513 | 65.2 (21.9) | 341 | 65.6 (21.6) |
| QLQ-C30 symptom scales | ||||
| Fatigue | 505 | 35.6 (27.5) | 341 | 35.1 (27.3) |
| Nausea/vomiting | 512 | 7.0 (15.8) | 341 | 7.0 (15.7) |
| Pain | 507 | 21.2 (27.6) | 341 | 20.0 (25.9) |
| Dyspnoea | 513 | 23.2 (30.6) | 341 | 22.1 (30.2) |
| Insomnia | 510 | 27.2 (33.1) | 341 | 26.4 (32.7) |
| Appetite loss | 513 | 18.7 (30.9) | 341 | 18.9 (30.7) |
| Constipation | 514 | 21.0 (29.0) | 341 | 22.0 (29.1) |
| Diarrhoea | 513 | 8.9 (20.5) | 341 | 9.5 (21.5) |
| Financial problems | 513 | 8.7 (21.1) | 341 | 9.9 (22.7) |
| QLQ-C30 functioning scales | ||||
| Physical Function | 508 | 73.3 (23.7) | 341 | 74.3 (32.9) |
| Role Function | 514 | 70.8 (32.8) | 341 | 71.6 (32.4) |
| Emotional Function | 506 | 82.2 (20.3) | 341 | 82.7 (19.6) |
| Cognitive Function | 509 | 83.3 (20.6) | 341 | 84.2 (20.3) |
| Social Function | 506 | 77.8 (29.4) | 341 | 77.6 (29.1) |
| QLQ-ELD14 scales | ||||
| Mobility | 503 | 28.4 (28.5) | 341 | 27.9 (29.0) |
| Joint Stiffness | 518 | 30.1 (32.4) | 341 | 28.6 (31.8) |
| Family Support | 484 | 70.7 (34.7) | 341 | 71.0 (35.2) |
| Worries about others | 493 | 39.6 (33.0) | 341 | 41.2 (33.6) |
| Future worries | 505 | 34.0 (31.9) | 341 | 31.6 (32.5) |
| Maintaining purpose | 511 | 64.6 (29.8) | 341 | 63.7 (30.9) |
| Burden of illness | 506 | 41.7 (32.7) | 341 | 42.2 (32.6) |
| Variable | Model 1 | Model 2 | Model 3 | Model 4 (Final Model) | ||||
|---|---|---|---|---|---|---|---|---|
| Regression Coefficient | Confidence Interval (95%) | Regression Coefficient | Confidence Interval (95%) | Regression Coefficient | Confidence Interval (95%) | Regression Coefficient | Confidence Interval (95%) | |
| Fixed and disease related variables | ||||||||
| Age | 0.170 | −0.279; 0.619 | −0.102 | −0.478; 0.275 | −0.099 | −0.480; 0.281 | −0.100 | −0.481; 0.281 |
| Sex | −2.992 | −7.151; 1.167 | 1.153 | −2.425; 4.732 | 1.615 | −1.988; 5.218 | 1.980 | −1.663; 5.624 |
| Disease stage * | −1.951 | −7.385; 3.482 | 1.953 | −2.635; 6.540 | 2.134 | −2.358; 6.627 | 2.309 | −2.188; 6.805 |
| Disease progression * | −3.93 | −11.099; 3.239 | −2.291 | −8.258; 3.677 | −2.996 | −8.795; 2.802 | −3.105 | −8.888; 2.677 |
| Treatment intention * | −2.071 | −7.381; 3.238 | −2.569 | −6.972; 1.834 | −1.466 | −5.765; 2.832 | −2.097 | −6.411; 2.217 |
| ECOG status * | −8.78 | −16.704; −0.855 | −0.936 | −7.718; 5.845 | 4.087 | −3.260; 11.435 | 4.311 | −3.086; 11.708 |
| Toxicity level * | −5.749 | −13.739; 2.242 | 3.215 | −3.624; 10.054 | 3.592 | −3.022; 10.205 | 4.165 | −2.464; 10.794 |
| Food intake (G8) * | 13.915 | 8.398; 19.431 | 3.997 | −1.285; 9.280 | 2.323 | −2.843; 7.490 | 2.507 | −2.656; 7.669 |
| Weight loss (G8) * | −1.678 | −7.589; 4.234 | −1.166 | −6.088; 3.755 | −1.032 | −5.809; 3.744 | −1.053 | −5.890; 3.785 |
| >Three medications (G8) * | 8.239 | 3.879; 12.599 | 4.941 | 1.286; 8.596 | 3.435 | −0.236; 7.107 | 2.922 | −0.777; 6.622 |
| Charlson Comorbidity Index * | −2.302 | −6.705; 2.1 | −0.268 | −3.943; 3.407 | −0.228 | −3.838; 3.382 | 0.261 | −3.389; 3.911 |
| EORTC QLQ-C30 symptom scales | ||||||||
| Fatigue | −0.365 | −0.463; −0.267 | −0.243 | −0.353; −0.134 | −0.223 | −0.334; −0.112 | ||
| Nausea/vomiting | 0.027 | −0.100; 0.154 | 0.022 | −0.102; 0.146 | 0.035 | −0.090; 0.159 | ||
| Pain | −0.097 | −0.180; −0.014 | −0.083 | −0.164; −0.002 | −0.067 | −0.150; 0.015 | ||
| Dyspnoea | 0.047 | −0.021; 0.116 | 0.051 | −0.017; 0.119 | 0.048 | −0.020; 0.117 | ||
| Insomnia | −0.021 | −0.078; 0.037 | −0.002 | −0.059; 0.054 | 0.002 | −0.055; 0.059 | ||
| Appetite loss | −0.061 | −0.143; 0.020 | −0.038 | −0.119; 0.043 | −0.049 | −0.130; 0.033 | ||
| Constipation | −0.034 | −0.096; 0.029 | −0.024 | −0.085; 0.037 | −0.031 | −0.092; 0.029 | ||
| Diarrhoea | −0.066 | −0.149; 0.017 | −0.060 | −0.141; 0.021 | −0.059 | −0.140; 0.021 | ||
| Financial problems | −0.116 | −0.198; −0.034 | −0.011 | −0.102; 0.080 | −0.014 | −0.107; 0.079 | ||
| EORTC QLQ-C30 functioning scales | ||||||||
| Physical Function | 0.173 | 0.041; 0.305 | 0.114 | −0.034; 0.262 | ||||
| Role Function | 0.025 | −0.055; 0.105 | 0.022 | −0.059; 0.102 | ||||
| Emotional Function | 0.040 | −0.059; 0.140 | 0.015 | −0.086; 0.116 | ||||
| Cognitive Function | 0.020 | −0.080; 0.120 | −0.002 | −0.103; 0.099 | ||||
| Social Function | 0.137 | 0.054; 0.221 | 0.099 | 0.008; 0.191 | ||||
| EORTC QLQ-ELD14 scales | ||||||||
| Mobility | −0.035 | −0.140; 0.071 | ||||||
| Joint Stiffness | −0.064 | −0.126; −0.002 | ||||||
| Family Support | 0.005 | −0.050; 0.060 | ||||||
| Worries about others | −0.006 | −0.064; 0.052 | ||||||
| Future worries | −0.005 | −0.074; 0.063 | ||||||
| Maintaining purpose | 0.019 | −0.041; 0.079 | ||||||
| Burden of illness | −0.071 | −0.141; −0.001 | ||||||
| Model R2 (adjusted) | 0.203 | 0.460 | 0.497 | 0.504 | ||||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmidt, H.; Nordhausen, T.; Boese, S.; Vordermark, D.; Wheelwright, S.; Wienke, A.; Johnson, C.D. Factors Influencing Global Health Related Quality of Life in Elderly Cancer Patients: Results of a Secondary Data Analysis. Geriatrics 2018, 3, 5. https://doi.org/10.3390/geriatrics3010005
Schmidt H, Nordhausen T, Boese S, Vordermark D, Wheelwright S, Wienke A, Johnson CD. Factors Influencing Global Health Related Quality of Life in Elderly Cancer Patients: Results of a Secondary Data Analysis. Geriatrics. 2018; 3(1):5. https://doi.org/10.3390/geriatrics3010005
Chicago/Turabian StyleSchmidt, Heike, Thomas Nordhausen, Stephanie Boese, Dirk Vordermark, Sally Wheelwright, Andreas Wienke, and Colin D. Johnson. 2018. "Factors Influencing Global Health Related Quality of Life in Elderly Cancer Patients: Results of a Secondary Data Analysis" Geriatrics 3, no. 1: 5. https://doi.org/10.3390/geriatrics3010005