Assessment of Psychopathology in Adolescents with Insulin-Dependent Diabetes (IDD) and the Impact on Treatment Management
Abstract
:1. Introduction
2. Material and Methods
3. Results
- A.
- from 10 to 30 months (n = 13)
- B.
- from 31 to 60 months (n = 17)
- C.
- >60 months (n = 24)
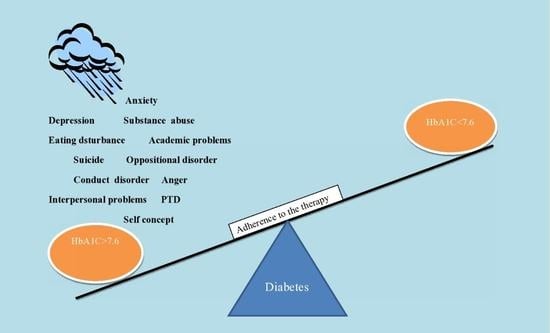
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Davies, M.J.; D’Alessio, D.A.; Fradkin, J.; Kernan, W.N.; Mathieu, C.; Mingrone, G.; Rossing, P.; Tsapas, A.; Wexler, G.J.; Buse, J.B. Management of hyperglycemia in type 2 diabetes: A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2018, 41, 2669–2701. [Google Scholar] [CrossRef] [Green Version]
- National Centre for Health Assessment and Promotion (CNEPSS), Romania StudiulCompSan 2017. Available online: http://insp.gov.ro/sites/cnepss/wp-content/uploads/2017/07/COMPSAN23 (accessed on 10 September 2020).
- Chew, B.H.; Sazlina, S.G.; Fernandez, A. Psychological aspects of diabetes care: Effecting behavioral change in patients. World J. Diabetes 2014, 5, 796–808. [Google Scholar] [CrossRef] [PubMed]
- Fritsch, S.L.; Overton, M.W.; Robbins, D.R. The interface of child mental health and juvenile diabetes mellitus. Pediatr. Clin. 2011, 58, 937–954. [Google Scholar] [CrossRef]
- Robertson, S.M.; Amspoker, A.B.; Cully, J.A.; Ross, E.L.; Naik, A.D. Affective symptoms and change in diabetes self-efficacy and glycemic control. Diabetes Med. 2013, 30, e189–e196. [Google Scholar] [CrossRef] [Green Version]
- Bernstein, C.M.; Stockwell, M.S.; Gallagher, M.P. Mental Health Issues in Adolescents and Young Adults with Type 1 Diabetes: Prevalence and Impact on Glycemic Control. Clin. Pediatr. 2013, 52, 10–15. [Google Scholar] [CrossRef]
- Lloyd, C. The effects of Diabetes on depression and depression on diabetes. Diabetes Voice 2008, 53, 23–26. [Google Scholar]
- Tareen, R.S.; Tareen, K. Psychosocial aspects of diabetes management: Dilemma of diabetes distress. Transl. Pediatr. 2017, 6, 383–396. [Google Scholar] [CrossRef] [Green Version]
- Robinson, M.E.; Simard, M.; Laroque, I.; Shah, J.; Nakhla, M.; Rahme, E. Risk of Psychiatric Disorders and Suicide Attempts in Emerging Adults With Diabetes. Diabetes Care 2020, 43, 484–486. [Google Scholar] [CrossRef] [PubMed]
- Dikel, W. Student Mental Health: A Guide for Teachers, School and District Leaders, School Psychologists and Nurses, Social Workers, Counselors, and Parents, 2nd ed.; W.W. Norton & Company: New York, NY, USA, 2019. [Google Scholar]
- Anderson, B.J.; Mansfield, A.K. Psychological issues in the treatment of diabetes. In Joslin’s Diabetes Deskbook, 2nd ed.; Beaser, R.S., Ed.; Joslin Diabetes Center: Boston, MA, USA, 2007; pp. 641–661. [Google Scholar]
- Pessoa, L. On the relationship between emotion and cognition. Nat. Rev. Neurosci. 2008, 9, 148–158. [Google Scholar] [CrossRef]
- Toni, G.; Berioli, M.G.; Cerquilini, L.; Ceccarini, G.; Grohmann, U.; Principi, N.; Esposito, S. Eating Disorders and Disordered Eating Symptoms in Adolescents with Type 1 Diabetes. Nutrients 2017, 9, 906. [Google Scholar] [CrossRef] [Green Version]
- Kınık, M.F.; Gonulu, F.V.; Vatansever, Z.; Karakaya, I. Diabulimia, a Type I diabetes mellitus-specific eating disorder. Turk. Arch. Pediatr. 2017, 52, 46–49. [Google Scholar] [CrossRef]
- Larrañaga, A.; Docet, M.F.; Garcia-Mayor, R.V. Disordered eating behaviors in type 1 diabetic patients. World J. Diabetes 2011, 2, 189–195. [Google Scholar] [CrossRef]
- Candler, T.; Murphy, R.; Pigott, A.; Gregory, J.W. Fifteen-minute consultation: Diabulimia and disordered eating in childhood diabetes. Arch. Dis. Child. Educ. Pract. 2018, 103, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Mc Sharry, J.; Moss-Morris, R.; Kendrick, T. Illness perceptions and glycaemic control in diabetes: A systematic review with meta-analysis. Diabet. Med. 2011, 28, 1300–1310. [Google Scholar] [CrossRef]
- Thoolen, B.J.; de Ridder, D.; Bensing, J.; Gorter, K.; Rutten, G. Beyond good intentions: The role of proactive coping inachieving sustained behavioural change in the context of diabetes management. Psychol. Health 2009, 24, 237–254. [Google Scholar] [CrossRef] [Green Version]
- Telford, K.; Kralik, D.; Koch, T. Acceptance and denial: Implications for people adapting to chronic illness: Literature review. J. Adv. Nurs. 2006, 55, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Bury, M. Chronic illness as biographical disruption. In Sociology of Health and Illness; Foundation for the Sociology of Health & Illness: Leeds, UK, 1982; Volume 4, pp. 125–239. [Google Scholar] [CrossRef]
- Fisher, L.; Danielle, M.; Polonsky, W.H.; Mullan, J. When Is Diabetes Distress Clinically Meaningful?: Establishing cut points for the Diabetes Distress. Diabetes Care 2012, 35, 259–264. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kessler, R.C.; Chiu, W.T.; Demler, O.; Merikangas, K.R.; Walters, E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 617–627. [Google Scholar] [CrossRef] [Green Version]
- Reynold, W. Adolescent Psychopathology Scale-Short Form: Professional Manual; Psychological Assesment Resources: Lutz, FL, USA, 2000. [Google Scholar]
- Balaj, A.; Miclea, M.; Albu, M. APS-SF–Scală de Evaluare a Tulburărilor din Adolescenţă; CBB Journal: Cluj, Romania, 2012; Volume XV, pp. 529–551. [Google Scholar]
- American Diabetes Association. Children and adolescents.11. In Standards of Medical Care in Diabetes 2015. Diabetes Care 2015, 38 (Suppl. S1), S70–S76.
- Rewers, M.J.; Pillay, K.; de Beaufort, C.; Craig, M.E.; Hanas, H.; Acerini, C.L.; Maahs, D.M. International Society for Pediatric and Adolescent Diabetes (ISPAD). Clinical Practice Consensus Guidelines 2014. Pediatr. Diabetes 2014, 15 (Suppl. S2), 102–114. [Google Scholar] [CrossRef]
- Goebel-Fabbri, A.E.; Fikkan, J.; Franko, D.L.; Pearson, K.; Anderson, B.J.; Weinger, K. Insulin restriction and associated morbidity and mortality in women with type 1 diabetes. Diabetes Care 2008, 31, 415–419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dindelegan, C.; David, D. Psihopatologie și Psihologie Clinică; Institutul Europen: București, Romania, 2012; Volume 1. [Google Scholar]
- Picardi, A.; Giuliani, E.; Gigantesco, A. Genes and environment in attachment. Neurosci. Biobehav. Rev. 2020, 112, 254–269. [Google Scholar] [CrossRef]
- Bruch, H. Obesity and Anorexia Nervosa: Psychosocial Aspects. Aust. N. Z. J. Psychiatry 1975, 9, 159–161. [Google Scholar] [CrossRef] [PubMed]
- Folkman, S.; Moskowitz, J.T. Positive affect and other side of coping. Am. Psychol. 2000, 55, 647–654. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, J.S. Depression. In Type 1 Diabetes Sourcebook; Peters, A., Laffel, L., Eds.; American Diabetes Association: Alexandria, VA, USA, 2013; pp. 169–179. [Google Scholar]
- White, N.D. Alcohol Use in Young Adults with Type 1 Diabetes Mellitus. Am. J. Lifestyle Med. 2017, 11, 433–435. [Google Scholar] [CrossRef]
- Graue, M.; Wentzel-Larsen, T.; Bru, E.; Hanestad, B.R.; Svik, O. The coping styles of adolescents with type 1 diabetes are associated with degree of metabolic control. Diabetes Care 2004, 27, 1313–1317. [Google Scholar] [CrossRef] [Green Version]
- Iacob, O.M.; Bacarea, A.; Ruta, F.D.; Bacarea, V.C.; Gliga, F.I.; Buicu, F.; Tarcea, M.; Avram, C.; Costea, G.C.; Sin, A.I. Anthropometric indices of the newborns related with some lifestyle parameters of women during pregnancy in Tirgu Mures region-a pilot study. Progr. Nutr. 2018, 20, 585–591. [Google Scholar] [CrossRef]
- Avram, C.; Avram, L.; Ruta, F.; Georgescu, I.M.; Rus, V. Consumer profile in terms of food label reading in Mures county, Romania—A pilot study. Prog. Nutr. 2020, 22, 4. [Google Scholar] [CrossRef]
- Avram, C.; Avram, L.; Olah, P.; Rus, V.; Georgescu, I.M.; Bucur, O.M.; Florina, R. Knowledge about food additives among adults—Pilot study. Prog. Nutr. 2021, 23, 1. [Google Scholar] [CrossRef]
- Izard, C.E.; King, K.A.; Trentacosta, C.J.; Morgan, J.K.; Laurenceau, J.P.; Krauthamer-Ewing, E.S.; Finlon, K.J. Accelerating the development of emotion competence in Head Start children: Effects on adaptive and maladaptive behavior. Dev. Psychopathol. 2008, 20, 369–397. [Google Scholar] [CrossRef]
- Lachin, J.M.; McGee, P.; Palmer, J.P. DCCT/EDIC Research Group Impact of C-peptide preservation on metabolic and clinical outcomes in the diabetes control and complications trial. Diabetes 2014, 63, 739–748. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Demographic Characteristics | IDD Patients (n = 54) | Control Group (n = 52) | p |
|---|---|---|---|
| Mean/SD (Age) | 15.28/1.774 | 14.38/1.619 | |
| Early stage (10–14 years old) | 37% (n = 20) | 53.8% (n = 28) | p =0.08 |
| Middle stage (15–17 years old) | 51.9% (n = 28) | 40.4% (n = 21) | p = 0.23 |
| Late adolescence (18–24 years old) | 11.1% (n = 6) | 5.8% (n = 3) | p = 0.32 |
| Gender | |||
| -Female | 38.9% (n = 21) | 50% (n = 26) | p = 0.24 |
| -Male | 61.1% (n = 33) | 50% (n = 26) | p = 0.24 |
| Urban/rural | |||
| -Urban | 98.1% (n = 53) | 100% (n = 52) | p = 0.32 |
| -Rural | 1.9% (n = 1) | 0% (n= 0) | p = 0.32 |
| Level of education | |||
| -Primary school | 51.9% (n = 28) | 61.5% (n = 32) | p = 0.31 |
| -High school | 48.1% (n = 26) | 38.5% (n = 20) | p = 0.31 |
| Variable | HbA1c > 7.6 m 1 | HbA1c < 7.6 m 2 | t | df | Sig 2 Tailed | d-Cohen |
|---|---|---|---|---|---|---|
| CND | 3.60 | 0.05 | 7.47 | 34.84 | 0.001 | 2.65 |
| ODD | 7.34 | 1.11 | 8.42 | 46.99 | 0.001 | 2.57 |
| SUB | 0.77 | 0.11 | 3.61 | 44.71 | 0.001 | 1.13 |
| AVP | 8.34 | 0.53 | 7.48 | 37.87 | 0.001 | 2.54 |
| ADP | 7.46 | 1.42 | 8.60 | 49.06 | 0.001 | 2.57 |
| GAD | 9.49 | 2.68 | 6.57 | 51.95 | 0.001 | 1.90 |
| PTSD | 8.11 | 1.74 | 6.05 | 51.70 | 0.001 | 1.76 |
| DEP | 9.43 | 1.84 | 6.44 | 45.72 | 0.001 | 1.99 |
| EAT | 2.91 | 0.95 | 2.61 | 51.91 | 0.012 | 0.75 |
| SUI | 1.57 | 0.05 | 4.67 | 35.80 | 0.001 | 1.63 |
| SCP | 8.66 | 2.26 | 6.91 | 51.75 | 0.001 | 2.01 |
| IPP | 8.66 | 0.95 | 7.08 | 48.31 | 0.001 | 2.13 |
| DEF | 0.80 | 2.63 | −5.17 | 27.12 | 0.001 | 2.07 |
| CNR | 0.31 | 0.68 | −1.60 | 22.95 | 0.123 | 0.69 |
| Variables | M | SD | Correlation | |
|---|---|---|---|---|
| 1 | HbA1C | 9.03 | 2.401 | - |
| 2 | CND | 2.35 | 2.816 | 813 ** |
| 3 | ODD | 5.15 | 4.436 | 860 ** |
| 4 | SUB | 0.54 | 0.84 | 590 ** |
| 5 | AVP | 5.59 | 6.141 | 851 ** |
| 6 | ADP | 5.33 | 4.207 | 834 ** |
| 7 | GAD | 7.09 | 5.349 | 755 ** |
| 8 | PTSD | 5.87 | 5.370 | 739 ** |
| 9 | DEP | 6.76 | 6.381 | 766 ** |
| 10 | EAT | 2.22 | 3.214 | 364 ** |
| 11 | SUI | 1.04 | 1.693 | 712 ** |
| 12 | SCP | 6.41 | 4.939 | 792 ** |
| 13 | IPP | 5.94 | 6.026 | 830 ** |
| Dependent Variable | Mean Female | Mean Male | t | df. | Sig. | D |
|---|---|---|---|---|---|---|
| GAD | 9.48 | 5.58 | 2.512 | 30.140 | 0.018 | 0.938 |
| PTSD | 8.71 | 4.06 | 3.092 | 30.522 | 0.004 | 1.148 |
| DEP | 9.43 | 5.06 | 2.335 | 30.022 | 0.026 | 0.874 |
| EAT | 4.86 | 0.55 | 5.283 | 22.972 | 0.000 | 2.261 |
| SUI | 1.71 | 0.61 | 2.100 | 24.929 | 0.046 | 0.862 |
| IPP | 8.24 | 4.48 | 2.098 | 29.866 | 0.044 | 0.787 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lica, M.M.; Papai, A.; Salcudean, A.; Crainic, M.; Covaciu, C.G.; Mihai, A. Assessment of Psychopathology in Adolescents with Insulin-Dependent Diabetes (IDD) and the Impact on Treatment Management. Children 2021, 8, 414. https://doi.org/10.3390/children8050414
Lica MM, Papai A, Salcudean A, Crainic M, Covaciu CG, Mihai A. Assessment of Psychopathology in Adolescents with Insulin-Dependent Diabetes (IDD) and the Impact on Treatment Management. Children. 2021; 8(5):414. https://doi.org/10.3390/children8050414
Chicago/Turabian StyleLica, Maria Melania, Annamaria Papai, Andreea Salcudean, Maria Crainic, Cristina Georgeta Covaciu, and Adriana Mihai. 2021. "Assessment of Psychopathology in Adolescents with Insulin-Dependent Diabetes (IDD) and the Impact on Treatment Management" Children 8, no. 5: 414. https://doi.org/10.3390/children8050414