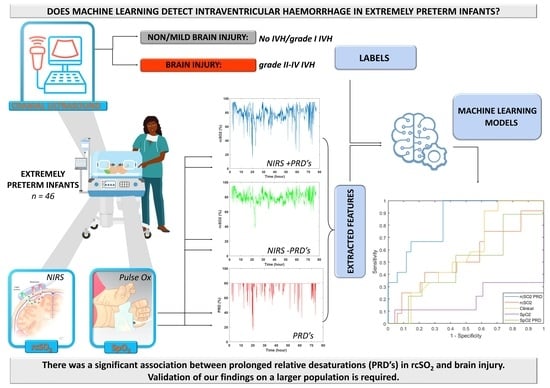
Machine Learning Detects Intraventricular Haemorrhage in Extremely Preterm Infants †
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Data Collection
2.3. Signal Processing
2.4. Extracting Prolonged Relative Desaturations
2.5. Feature Extraction
2.6. Machine Learning Models
2.7. Combining Models
2.8. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| rcSO2 | Regional cerebral oxygen saturation |
| SpO2 | Peripheral oxygen saturation |
| NIRS | Near-infrared spectroscopy |
| IVH | Intraventricular haemorrhage |
| PRD | Prolonged relative desaturation |
| US | Ultrasound |
| AUC | Area under the curve |
References
- Cheong, J.L.; Doyle, L.W.; Burnett, A.C.; Lee, K.J.; Walsh, J.M.; Potter, C.R.; Treyvaud, K.; Thompson, D.K.; Olsen, J.E.; Anderson, P.J.; et al. Association between Moderate and Late Preterm Birth and Neurodevelopment and Social-Emotional Development at Age 2 Years. JAMA Pediatr. 2017, 171, e164805. [Google Scholar] [CrossRef] [PubMed]
- Bulbul, L.; Elitok, G.K.; Ayyıldız, E.; Kabakcı, D.; Uslu, S.; Köse, G.; Tiryaki Demir, S.; Bulbul, A. Neuromotor Development Evaluation of Preterm Babies Less than 34 Weeks of Gestation with Bayley III at 18–24 Months. Biomed. Res. Int. 2020, 2020, 5480450. [Google Scholar] [CrossRef] [PubMed]
- Juul, S.E.; Wood, T.R.; Comstock, B.A.; Perez, K.; Gogcu, S.; Puia-Dumitrescu, M.; Berkelhamer, S.; Heagerty, P.J. Deaths in a Modern Cohort of Extremely Preterm Infants from the Preterm Erythropoietin Neuroprotection Trial. JAMA Netw. Open 2022, 5, e2146404. [Google Scholar] [CrossRef]
- Siffel, C.; Kistler, K.D.; Sarda, S.P. Global incidence of intraventricular hemorrhage among extremely preterm infants: A systematic literature review. J. Perinat. Med. 2021, 49, 1017–1026. [Google Scholar] [CrossRef] [PubMed]
- Allan, W.C.; Vohr, B.; Makuch, R.W.; Katz, K.H.; Ment, L.R. Antecedents of Cerebral Palsy in a Multicenter Trial of Indomethacin for Intraventricular Hemorrhage. Arch. Pediatr. Adolesc. Med. 1997, 151, 580–585. [Google Scholar] [CrossRef]
- Adams-Chapman, I.; Hansen, N.I.; Stoll, B.J.; Higgins, R. Neurodevelopmental outcome of extremely low birth weight infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics 2008, 121, e1167–e1177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hollebrandse, N.L.; Spittle, A.J.; Burnett, A.C.; Anderson, P.J.; Roberts, G.; Doyle, L.W.; Cheong, J.L.Y. School-age outcomes following intraventricular haemorrhage in infants born extremely preterm. Arch. Dis. Child. Fetal Neonatal Ed. 2021, 106, 4–8. [Google Scholar] [CrossRef] [PubMed]
- du Plessis, A.J.; Volpe, J.J. Perinatal brain injury in the preterm and term newborn. Curr. Opin. Neurol. 2002, 15, 151–157. [Google Scholar] [CrossRef]
- Matsushita, F.A.-O.; Krebs, V.L.J.; de Carvalho, W.B. Identifying clinical phenotypes in extremely low birth weight infants-an unsupervised machine learning approach. Eur. J. Pediatr. 2022, 181, 1085–1097. [Google Scholar] [CrossRef]
- Ng, I.A.-O.; da Costa, C.S.; Zeiler, F.A.; Wong, F.Y.; Smielewski, P.; Czosnyka, M.; Austin, T. Burden of hypoxia and intraventricular haemorrhage in extremely preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 2020, 105, 242–247. [Google Scholar] [CrossRef]
- Noori, S.; McCoy, M.; Anderson, M.P.; Ramji, F.; Seri, I. Changes in cardiac function and cerebral blood flow in relation to peri/intraventricular hemorrhage in extremely preterm infants. J. Pediatr. 2014, 164, e261–e263. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, H.; Gregas, M.C.; Limperopoulos, C.; Zaretskaya, I.; Bassan, H.; Soul, J.S.; Di Salvo, D.N.; du Plessis, A.J. Elevated cerebral pressure passivity is associated with prematurity-related intracranial hemorrhage. Pediatrics 2009, 124, 302–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alderliesten, T.; Lemmers, P.M.; Smarius, J.J.; van de Vosse, R.E.; Baerts, W.; van Bel, F. Cerebral oxygenation, extraction, and autoregulation in very preterm infants who develop peri-intraventricular hemorrhage. J. Pediatr. 2013, 162, 698–704.e692. [Google Scholar] [CrossRef] [PubMed]
- Martini, S.; Czosnyka, M.; Smielewski, P.; Iommi, M.; Galletti, S.; Vitali, F.; Paoletti, V.; Camela, F.; Austin, T.; Corvaglia, L. Clinical determinants of cerebrovascular reactivity in very preterm infants during the transitional period. Pediatr. Res. 2022, 92, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Pavlek, L.R.; Mueller, C.; Jebbia, M.R.; Kielt, M.J.; Fathi, O. Near-Infrared Spectroscopy in Extremely Preterm Infants. Front. Pediatr. 2021, 8, 624113. [Google Scholar] [CrossRef] [PubMed]
- Kalteren, W.S.; Verhagen, E.A.; Mintzer, J.P.; Bos, A.F.; Kooi, E.M.W. Anemia and Red Blood Cell Transfusions, Cerebral Oxygenation, Brain Injury and Development, and Neurodevelopmental Outcome in Preterm Infants: A Systematic Review. Front. Pediatr. 2021, 9, 644462. [Google Scholar] [CrossRef]
- Plomgaard, A.M.; Alderliesten, T.; van Bel, F.; Benders, M.; Claris, O.; Cordeiro, M.; Dempsey, E.; Fumagalli, M.; Gluud, C.; Hyttel-Sorensen, S.; et al. No neurodevelopmental benefit of cerebral oximetry in the first randomised trial (SafeBoosC II) in preterm infants during the first days of life. Acta Paediatr. 2019, 108, 275–281. [Google Scholar] [CrossRef] [Green Version]
- van Bel, F.; Lemmers, P.; Naulaers, G. Monitoring neonatal regional cerebral oxygen saturation in clinical practice: Value and pitfalls. Neonatology 2008, 94, 237–244. [Google Scholar] [CrossRef]
- Hansen, M.L.; Hyttel-Sørensen, S.; Jakobsen, J.C.; Gluud, C.; Kooi, E.M.W.; Mintzer, J.; de Boode, W.P.; Fumagalli, M.; Alarcon, A.; Alderliesten, T.; et al. Cerebral near-infrared spectroscopy monitoring (NIRS) in children and adults: A systematic review with meta-analysis. Pediatr. Res. 2022. [Google Scholar] [CrossRef]
- Alderliesten, T.; Lemmers, P.M.; van Haastert, I.C.; de Vries, L.S.; Bonestroo, H.J.; Baerts, W.; van Bel, F. Hypotension in preterm neonates: Low blood pressure alone does not affect neurodevelopmental outcome. J. Pediatr. 2014, 164, 986–991. [Google Scholar] [CrossRef]
- Verhagen, E.A.; Van Braeckel, K.N.; van der Veere, C.N.; Groen, H.; Dijk, P.H.; Hulzebos, C.V.; Bos, A.F. Cerebral oxygenation is associated with neurodevelopmental outcome of preterm children at age 2 to 3 years. Dev. Med. Child. Neurol. 2015, 57, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Alderliesten, T.; Dix, L.; Baerts, W.; Caicedo, A.; van Huffel, S.; Naulaers, G.; Groenendaal, F.; van Bel, F.; Lemmers, P. Reference values of regional cerebral oxygen saturation during the first 3 days of life in preterm neonates. Pediatr. Res. 2016, 79, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Dix, L.M.; van Bel, F.; Baerts, W.; Lemmers, P.M. Comparing near-infrared spectroscopy devices and their sensors for monitoring regional cerebral oxygen saturation in the neonate. Pediatr. Res. 2013, 74, 557–563. [Google Scholar] [CrossRef] [PubMed]
- O’Toole, J.M.; Kenosi, M.; Finn, D.; Boylan, G.B.; Dempsey, E.M. Features of cerebral oxygenation detects brain injury in premature infants. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 3614–3617. [Google Scholar] [CrossRef]
- O’Toole, J.M.; Dempsey, E.M.; Boylan, G.B. Extracting transients from cerebral oxygenation signals of preterm infants: A new singular-spectrum analysis method. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018; pp. 5882–5885. [Google Scholar] [CrossRef]
- Dempsey, E.M.; Barrington, K.J.; Marlow, N.; O’Donnell, C.P.F.; Miletin, J.; Naulaers, G.; Cheung, P.Y.; Corcoran, J.D.; El-Khuffash, A.F.; Boylan, G.B.; et al. Hypotension in Preterm Infants (HIP) randomised trial. Arch. Dis. Child. Fetal Neonatal Ed. 2021, 106, 398–403. [Google Scholar] [CrossRef]
- Volpe, J.J. Neurology of the Newborn, 5th ed.; Saunders Elsevier: Philadelphia, PA, USA, 2008. [Google Scholar]
- Payne, A.H.; Hintz, S.R.; Hibbs, A.M.; Walsh, M.C.; Vohr, B.R.; Bann, C.M.; Wilson-Costello, D.E. Neurodevelopmental outcomes of extremely low-gestational-age neonates with low-grade periventricular-intraventricular hemorrhage. JAMA Pediatr. 2013, 167, 451–459. [Google Scholar] [CrossRef] [Green Version]
- Ouchi, E.; Usuniwa, H.; Nemoto, K.; Inagaki, T. Simultaneous measurement under resting-state of autonomic nervous activity and brain activity by near-infrared spectroscopy alone. Infrared Phys. Technol. 2022, 122, 104065. [Google Scholar] [CrossRef]
- Hessel, T.W.; Hyttel-Sorensen, S.; Greisen, G. Cerebral oxygenation after birth—A comparison of INVOS(®) and FORE-SIGHT™ near-infrared spectroscopy oximeters. Acta Paediatr. 2014, 103, 488–493. [Google Scholar] [CrossRef] [Green Version]
- Buekers, J.; Theunis, J.; De Boever, P.; Vaes, A.W.; Koopman, M.; Janssen, E.V.; Wouters, E.F.; Spruit, M.A.; Aerts, J.M. Wearable Finger Pulse Oximetry for Continuous Oxygen Saturation Measurements during Daily Home Routines of Patients with Chronic Obstructive Pulmonary Disease (COPD) over One Week: Observational Study. JMIR Mhealth Uhealth 2019, 7, e12866. [Google Scholar] [CrossRef]
- Ashoori, M.; Dempsey, E.M.; McDonald, F.B.; O’Toole, J.M. Sparse-Denoising Methods for Extracting Desaturation Transients in Cerebral Oxygenation Signals of Preterm Infants. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Guadalajara, Mexico, 1–5 November 2021; pp. 1010–1013. [Google Scholar] [CrossRef]
- Fan, J.; Upadhye, S.; Worster, A. Understanding receiver operating characteristic (ROC) curves. Cjem 2006, 8, 19–20. [Google Scholar] [CrossRef]
- Hansen, M.L.; Pellicer, A.; Hyttel-Sørensen, S.; Ergenekon, E.; Szczapa, T.; Hagmann, C.; Naulaers, G.; Mintzer, J.; Fumagalli, M.; Dimitriou, G.; et al. Cerebral Oximetry Monitoring in Extremely Preterm Infants. N. Engl. J. Med. 2023, 388, 1501–1511. [Google Scholar] [CrossRef]
- Hansen, M.L.; Pellicer, A.; Gluud, C.; Dempsey, E.; Mintzer, J.; Hyttel-Sørensen, S.; Heuchan, A.M.; Hagmann, C.; Ergenekon, E.; Dimitriou, G.; et al. Cerebral near-infrared spectroscopy monitoring versus treatment as usual for extremely preterm infants: A protocol for the SafeBoosC randomised clinical phase III trial. Trials 2019, 20, 811. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suppan, E.; Pichler, G.; Binder-Heschl, C.; Schwaberger, B.; Urlesberger, B. Three Physiological Components That Influence Regional Cerebral Tissue Oxygen Saturation. Front. Pediatr. 2022, 10, 913223. [Google Scholar] [CrossRef] [PubMed]
- Bresesti, I.; Avian, A.; Bruckner, M.; Binder-Heschl, C.; Schwaberger, B.; Baik-Schneditz, N.; Schmölzer, G.; Pichler, G.; Urlesberger, B. Impact of bradycardia and hypoxemia on oxygenation in preterm infants requiring respiratory support at birth. Resuscitation 2021, 164, 62–69. [Google Scholar] [CrossRef] [PubMed]
- Janaillac, M.; Beausoleil, T.P.; Barrington, K.J.; Raboisson, M.J.; Karam, O.; Dehaes, M.; Lapointe, A. Correlations between near-infrared spectroscopy, perfusion index, and cardiac outputs in extremely preterm infants in the first 72 h of life. Eur. J. Pediatr. 2018, 177, 541–550. [Google Scholar] [CrossRef] [PubMed]
- Sweet, D.; Bevilacqua, G.; Carnielli, V.; Greisen, G.; Plavka, R.; Didrik, S.O.; Simeoni, U.; Speer, C.P.; Soler, A.; Valls, I.; et al. European consensus guidelines on the management of neonatal respiratory distress syndrome. Zhonghua Er Ke Za Zhi 2008, 46, 30–34. [Google Scholar] [CrossRef] [PubMed]
- The American Academy of Pediatrics and the American College of Obstetricians and Gynecologists. Guidelines for Perinatal Care; American Academy of Pediatrics: Elk Grove Village, IL, USA, 2007. [Google Scholar]
- Askie, L.M.; Darlow, B.A.; Finer, N.; Schmidt, B.; Stenson, B.; Tarnow-Mordi, W.; Davis, P.G.; Carlo, W.A.; Brocklehurst, P.; Davies, L.C.; et al. Association between Oxygen Saturation Targeting and Death or Disability in Extremely Preterm Infants in the Neonatal Oxygenation Prospective Meta-analysis Collaboration. JAMA 2018, 319, 2190–2201. [Google Scholar] [CrossRef] [Green Version]
- Sullivan, B.A.; Wallman-Stokes, A.; Isler, J.; Sahni, R.; Moorman, J.R.; Fairchild, K.D.; Lake, D.E. Early Pulse Oximetry Data Improves Prediction of Death and Adverse Outcomes in a Two-Center Cohort of Very Low Birth Weight Infants. Am. J. Perinatol. 2018, 35, 1331–1338. [Google Scholar] [CrossRef]
- Vesoulis, Z.A.; Bank, R.L.; Lake, D.; Wallman-Stokes, A.; Sahni, R.; Moorman, J.R.; Isler, J.R.; Fairchild, K.D.; Mathur, A.M. Early hypoxemia burden is strongly associated with severe intracranial hemorrhage in preterm infants. J. Perinatol. 2019, 39, 48–53. [Google Scholar] [CrossRef]
- Zanelli, S.A.-O.; Abubakar, M.; Andris, R.; Patwardhan, K.; Fairchild, K.D.; Vesoulis, Z.A. Early Vital Sign Differences in Very Low Birth Weight Infants with Severe Intraventricular Hemorrhage. Am. J. Perinatol. 2021, in press. [Google Scholar] [CrossRef]
- DeMeulenaere, S. Pulse Oximetry: Uses and Limitations. J. Nurse Pract. 2007, 3, 312–317. [Google Scholar] [CrossRef]
- Pritišanac, E.; Urlesberger, B.; Schwaberger, B.; Pichler, G. Accuracy of Pulse Oximetry in the Presence of Fetal Hemoglobin-A Systematic Review. Children 2021, 8, 361. [Google Scholar] [CrossRef] [PubMed]
- Sankaran, V.G.; Orkin, S.H. The switch from fetal to adult hemoglobin. Cold Spring Harb. Perspect. Med. 2013, 3, a011643. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Clinical Features | Brain Injury (n = 12) | No/Mild Injury (n = 34) |
|---|---|---|
| Sex (male) (% of the total number of infants in the group) | 8 (67%) | 17 (50%) |
| Hypotension (% of the total number of infants in the group) | 7 (58%) | 13 (38%) |
| Inotrope administration (% of the total number of infants in the group) | 3 (25%) | 6 (18%) |
| Chorioamnionitis (% of the total number of infants in the group) | 0 (0%) | 5 (15%) |
| Gestational age (days) Mean (SD) | 178.5 (7.5) | 181.3 (8.8) |
| Birth weight (g) Mean (SD) | 769.2 (173.7) | 766.8 (151.5) |
| APGAR score (5 min) Mean (SD) | 7.0 (2.0) | 6.9 (1.9) |
| Head circumference (cm) Mean (SD) | 23.3 (1.5) | 23.3 (1.5) |
| Model | AUC | 95% Confidence Interval |
|---|---|---|
| Clinical data | 0.575 | 0.390–0.759 |
| rcSO2 | 0.532 | 0.312–0.740 |
| rcSO2 without PRDs | 0.542 | 0.331–0.741 |
| rcSO2 PRDs | 0.846 * | 0.720–0.948 |
| rcSO2 and clinical data | 0.571 | 0.390–0.756 |
| rcSO2 without PRDs and clinical data | 0.591 | 0.396–0.777 |
| rcSO2 PRDs and clinical data | 0.860 * | 0.742–0.957 |
| SpO2 | 0.198 | 0.000–0.459 |
| SpO2 without PRDs | 0.261 | 0.061–0.545 |
| SpO2 PRDs | 0.493 | 0.264–0.741 |
| SpO2 and clinical data | 0.324 | 0.133–0.546 |
| SpO2 without PRDs and clinical data | 0.348 | 0.151–0.579 |
| SpO2 PRDs and clinical data | 0.454 | 0.235–0.697 |
| rcSO2 time spent below 63% | 0.593 | 0.399–0.775 |
| SpO2 time spent below 85% | 0.522 | 0.277–0.759 |
| Feature | AUC | 95% Confidence Interval |
|---|---|---|
| Frequency of the transients per hour | 0.409 | 0.201–0.619 |
| Total power | 0.368 | 0.191–0.560 |
| Envelope (mean) | 0.397 | 0.214–0.592 |
| Envelope (standard deviation) | 0.539 | 0.352–0.738 |
| Hjorth parameters (activity) | 0.603 | 0.399–0.802 |
| Hjorth parameters (mobility) | 0.409 | 0.214–0.602 |
| Hjorth parameters (complexity) | 0.569 | 0.353–0.775 |
| Inter-spike interval (mean) | 0.532 | 0.306–0.748 |
| Inter-spike interval (standard deviation) | 0.505 | 0.282–0.714 |
| Time spent below 63% | 0.691 | 0.494–0.861 |
| Nadir amplitude of PRDs (mean) | 0.733 * | 0.530–0.919 |
| Slope down (mean) | 0.689 | 0.474–0.883 |
| Slope up (mean) | 0.669 | 0.477–0.838 |
| Duration of the PRDs (mean) | 0.603 | 0.422–0.770 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ashoori, M.; O’Toole, J.M.; O’Halloran, K.D.; Naulaers, G.; Thewissen, L.; Miletin, J.; Cheung, P.-Y.; EL-Khuffash, A.; Van Laere, D.; Straňák, Z.; et al. Machine Learning Detects Intraventricular Haemorrhage in Extremely Preterm Infants. Children 2023, 10, 917. https://doi.org/10.3390/children10060917
Ashoori M, O’Toole JM, O’Halloran KD, Naulaers G, Thewissen L, Miletin J, Cheung P-Y, EL-Khuffash A, Van Laere D, Straňák Z, et al. Machine Learning Detects Intraventricular Haemorrhage in Extremely Preterm Infants. Children. 2023; 10(6):917. https://doi.org/10.3390/children10060917
Chicago/Turabian StyleAshoori, Minoo, John M. O’Toole, Ken D. O’Halloran, Gunnar Naulaers, Liesbeth Thewissen, Jan Miletin, Po-Yin Cheung, Afif EL-Khuffash, David Van Laere, Zbyněk Straňák, and et al. 2023. "Machine Learning Detects Intraventricular Haemorrhage in Extremely Preterm Infants" Children 10, no. 6: 917. https://doi.org/10.3390/children10060917