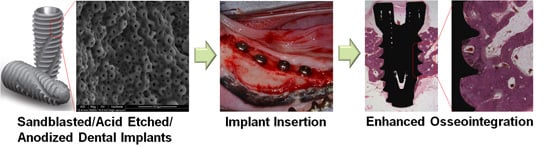
Cell Adhesion and in Vivo Osseointegration of Sandblasted/Acid Etched/Anodized Dental Implants
Abstract
:1. Introduction
2. Results
2.1. Surface Characterization

| Groups | Sa (μm) ± SD | Sq (μm) ± SD | Rt (μm) ± SD |
|---|---|---|---|
| Control | 0.08 ± 0.04 | 0.09 ± 0.02 | 1.95 ± 0.11 |
| SLA | 1.68 ± 0.22 | 2.15 ± 0.29 | 16.99 ± 3.09 |
| ANO | 0.52 ± 0.14 | 0.68 ± 0.19 | 6.44 ± 1.51 |
| Modi-ANO | 1.45 ± 0.25 | 1.85 ± 0.33 | 13.76 ± 2.69 |
| Groups | C (at%) | O (at%) | P (at%) | Ti (at%) |
|---|---|---|---|---|
| Control | 7.38 | 15.71 | 0.96 | 75.95 |
| SLA | – | 3.4 | – | 96.6 |
| ANO | 5.35 | 65.20 | 5.74 | 23.71 |
| Modi-ANO | 5.76 | 69.24 | 5.61 | 19.39 |
2.2. Cell Adhesion Testing


2.3. In Vivo Study
| Group | Number | BIC (Mean ± SD) (%) | ITBD (Mean ± SD) (%) |
|---|---|---|---|
| Control | 8 | 33.58 ± 8.63 ** | 34.90 ± 7.24 ** |
| SLA | 8 | 58.47 ± 12.89 * | 53.98 ± 13.77 |
| ANO | 8 | 59.62 ± 18.30 * | 61.64 ± 16.17 |
| Modi-ANO | 8 | 74.20 ± 10.89 | 60.80 ± 13.32 |

3. Discussion
4. Experimental Section
4.1. Materials
4.2. Surface Characterization by Scanning Electron Microscopy (SEM)
4.3. Surface Roughness Measurement
4.4. Cell Culture and Cell Adhesion Study
4.5. In Vivo Animal Study
4.5.1. Fabrication of Implants and Animals
4.5.2. Surgery for Tooth Extraction
4.5.3. Surgery for Implant Insertion and Postoperative Care

4.5.4. Animal Sacrifice and Histological Analysis
4.6. Statistical Analysis
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Heo, Y.Y.; Um, S.; Kim, S.K.; Park, J.M.; Seo, B.M. Responses of periodontal ligament stem cells on various Ti surfaces. Oral Dis. 2011, 17, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Nayab, S.N.; Jones, F.H.; Olsen, I. Effects of calcium ion-implantation of Ti on bone cell function in vitro. J. Biomed. Mater. Res. A 2007, 83, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Puleo, D.A.; Nanci, A. Understanding and controlling the bone-implant interface. Biomaterials 1999, 20, 2311–2321. [Google Scholar] [CrossRef] [PubMed]
- Pohler, O.E. Unalloyed Ti for implants in bone surgery. Injury 2000, 31 (Suppl. 4), 7–13. [Google Scholar] [CrossRef] [PubMed]
- Stanford, C.M. Surface modifications of dental implants. Aust. Dent. J. 2008, 53 (Suppl. 1), S26–S33. [Google Scholar] [CrossRef] [PubMed]
- Geetha, M.; Singh, A.K.; Asokamani, R.; Gongia, A.K. Ti based biomaterials, the ultimate choice for orthopaedic implants—A review. Prog. Mater. Sci. 2009, 54, 397–425. [Google Scholar] [CrossRef]
- Schliephake, H.; Schaweber, D. Chemical and biological functionalization of Ti for dental implants. J. Mater. Chem. 2008, 18, 2404–2414. [Google Scholar] [CrossRef]
- Wong, M.; Eulenberger, J.; Schenk, R.; Hunziker, E. Effect of surface topology on the osseointegration of implant materials in trabecular bone. J. Biomed. Mater. Res. 1995, 29, 1567–1575. [Google Scholar] [CrossRef] [PubMed]
- Wennerberg, A.; Albrektsson, T. Effects of Ti surface topography on bone integration: A systematic review. Clin. Oral Implant. Res. 2009, 20 (Suppl. 4), 172–184. [Google Scholar] [CrossRef]
- Beutner, R.; Michael, J.; Schwenzer, B.; Scharnweber, D. Biological nano-functionalization of Ti-based biomaterial surfaces: A flexible toolbox. J. R. Soc. Interface 2010, 7 (Suppl. 1), S93–S105. [Google Scholar] [CrossRef] [PubMed]
- Lutz, R.; Srour, S.; Nonhoff, J.; Weisel, T.; Damien, C.J.; Schlegel, K.A. Biofunctionalization of Ti implants with a biomimetic active peptide (P-15) promotes early osseointegration. Clin. Oral Implant. Res. 2010, 21, 726–734. [Google Scholar] [CrossRef]
- Wennerberg, A.; Albrektsson, T. On implant surfaces: A review of current knowledge and opinions. Int. J. Oral Maxillofac. Implant. 2010, 25, 63–74. [Google Scholar]
- Buser, D.; Broggini, N.; Wieland, M.; Schenk, R.K.; Denzer, A.J.; Cochran, D.L.; Hoffmann, B.; Lussi, A.; Steinemann, S.G. Enhanced bone apposition to a chemically modified SLA Ti surface. J. Dent. Res. 2004, 83, 529–533. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Schenk, R.K.; Steinemann, S.; Fiorellini, J.P.; Fox, C.H.; Stich, H. Influence of surface characteristics on bone integration of Ti implants. A histomorphometric study in miniature pigs. J. Biomed. Mater. Res. 1991, 25, 889–902. [Google Scholar] [CrossRef] [PubMed]
- Sul, Y.T.; Johansson, C.B.; Petronis, S.; Krozer, A.; Jeong, Y.; Wennerberg, A.; Albrektsson, T. Characteristics of the surface oxides on turned and electrochemically oxidized pure Ti implants up to dielectric breakdown: The oxide thickness, micropore configurations, surface roughness, crystal structure and chemical composition. Biomaterials 2002, 23, 491–501. [Google Scholar] [CrossRef] [PubMed]
- Macak, J.M.; Tsuchiya, H.; Taveira, L.; Ghicov, A.; Schmuki, P. Self-organized nanotubular oxide layers on Ti-6Al-7Nb and Ti-6Al-4V formed by anodization in NH4F solutions. J. Biomed. Mater. Res. A 2005, 75, 928–933. [Google Scholar] [CrossRef] [PubMed]
- Sul, Y.T. The significance of the surface properties of oxidized Ti to the bone response: Special emphasis on potential biochemical bonding of oxidized Ti implant. Biomaterials 2003, 24, 3893–3907. [Google Scholar] [CrossRef] [PubMed]
- Sul, Y.T.; Johansson, C.; Wennerberg, A.; Cho, L.R.; Chang, B.S.; Albrektsson, T. Optimum surface properties of oxidized implants for reinforcement of osseointegration: Surface chemistry, oxide thickness, porosity, roughness, and crystal structure. Int. J. Oral Maxillofac. Implant. 2005, 20, 349–359. [Google Scholar]
- Deligianni, D.D.; Katsala, N.; Ladas, S.; Sotiropoulou, D.; Amedee, J.; Missirlis, Y.F. Effect of surface roughness of the Ti alloy Ti-6Al-4V on human bone marrow cell response and on protein adsorption. Biomaterials 2001, 22, 1241–1251. [Google Scholar] [CrossRef] [PubMed]
- Lamers, E.; Walboomers, X.F.; Domanski, M.; te Riet, J.; van Delft, F.C.; Luttge, R.; Winnubst, L.A.; Gardeniers, H.J.; Jansen, J.A. The influence of nanoscale grooved substrates on osteoblast behavior and extracellular matrix deposition. Biomaterials 2010, 31, 3307–3316. [Google Scholar] [CrossRef] [PubMed]
- Mendonca, G.; Mendonca, D.B.; Aragao, F.J.; Cooper, L.F. The combination of micron and nanotopography by H2SO4/H2O2 treatment and its effects on osteoblast-specific gene expression of hMSCs. J. Biomed. Mater. Res. A 2010, 94, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Albrektsson, T.; Wennerberg, A. Oral implant surfaces: Part 1—Review focusing on topographic and chemical properties of different surfaces and in vivo responses to them. Int. J. Prosthodont. 2004, 17, 536–543. [Google Scholar] [PubMed]
- Le Guehennec, L.; Soueidan, A.; Layrolle, P.; Amouriq, Y. Surface treatments of Ti dental implants for rapid osseointegration. Dent. Mater. 2007, 23, 844–854. [Google Scholar] [CrossRef] [PubMed]
- Sammons, R.L.; Lumbikanonda, N.; Gross, M.; Cantzler, P. Comparison of osteoblast spreading on microstructured dental implant surfaces and cell behaviour in an explant model of osseointegration. A scanning electron microscopic study. Clin. Oral Implant. Res. 2005, 16, 657–666. [Google Scholar] [CrossRef]
- Zhao, G.; Zinger, O.; Schwartz, Z.; Wieland, M.; Landolt, D.; Boyan, B.D. Osteoblast-like cells are sensitive to submicron-scale surface structure. Clin. Oral Implant. Res. 2006, 17, 258–264. [Google Scholar] [CrossRef]
- Dohan Ehrenfest, D.M.; Coelho, P.G.; Kang, B.S.; Sul, Y.T.; Albrektsson, T. Classification of osseointegrated implant surfaces: Materials, chemistry and topography. Trends Biotechnol. 2010, 28, 198–206. [Google Scholar]
- Webster, T.J.; Ergun, C.; Doremus, R.H.; Siegel, R.W.; Bizios, R. Enhanced functions of osteoblasts on nanophase ceramics. Biomaterials 2000, 21, 1803–1810. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.H.; Finones, R.R.; Daraio, C.; Chen, L.H.; Jin, S. Growth of nano-scale hydroxyapatite using chemically treated Ti oxide nanotubes. Biomaterials 2005, 26, 4938–4943. [Google Scholar] [CrossRef] [PubMed]
- Sul, Y.T.; Johansson, C.B.; Jeong, Y.; Wennerberg, A.; Albrektsson, T. Resonance frequency and removal torque analysis of implants with turned and anodized surface oxides. Clin. Oral Implant. Res. 2002, 13, 252–259. [Google Scholar] [CrossRef]
- De Angelis, E.; Ravanetti, F.; Cacchioli, A.; Corradi, A.; Giordano, C.; Candiani, G.; Chiesa, R.; Gabbi, C.; Borghetti, P. Attachment, proliferation and osteogenic response of osteoblast-like cells cultured on Ti treated by a novel multiphase anodic spark deposition process. J. Biomed. Mater. Res. B 2009, 88, 280–289. [Google Scholar]
- Rupp, F.; Scheideler, L.; Olshanska, N.; de Wild, M.; Wieland, M.; Geis-Gerstorfer, J. Enhancing surface free energy and hydrophilicity through chemical modification of microstructured Ti implant surfaces. J. Biomed. Mater. Res. A 2006, 76, 323–334. [Google Scholar] [CrossRef] [PubMed]
- Bornstein, M.M.; Valderrama, P.; Jones, A.A.; Wilson, T.G.; Seibl, R.; Cochran, D.L. Bone apposition around two different sandblasted and acid-etched Ti implant surfaces: A histomorphometric study in canine mandibles. Clin. Oral Implant. Res. 2008, 19, 233–241. [Google Scholar] [CrossRef]
- Barrere, F.; Layrolle, P.; van Blitterswijk, C.A.; de Groot, K. Biomimetic calcium phosphate coatings on Ti6AI4V: A crystal growth study of octacalcium phosphate and inhibition by Mg2+ and HCO3. Bone 1999, 25 (Suppl. 2), S107–S111. [Google Scholar] [CrossRef]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.-H.; Park, K.; Choi, K.-H.; Kim, S.-H.; Kim, S.E.; Jeong, C.-M.; Huh, J.-B. Cell Adhesion and in Vivo Osseointegration of Sandblasted/Acid Etched/Anodized Dental Implants. Int. J. Mol. Sci. 2015, 16, 10324-10336. https://doi.org/10.3390/ijms160510324
Kim M-H, Park K, Choi K-H, Kim S-H, Kim SE, Jeong C-M, Huh J-B. Cell Adhesion and in Vivo Osseointegration of Sandblasted/Acid Etched/Anodized Dental Implants. International Journal of Molecular Sciences. 2015; 16(5):10324-10336. https://doi.org/10.3390/ijms160510324
Chicago/Turabian StyleKim, Mu-Hyon, Kyeongsoon Park, Kyung-Hee Choi, Soo-Hong Kim, Se Eun Kim, Chang-Mo Jeong, and Jung-Bo Huh. 2015. "Cell Adhesion and in Vivo Osseointegration of Sandblasted/Acid Etched/Anodized Dental Implants" International Journal of Molecular Sciences 16, no. 5: 10324-10336. https://doi.org/10.3390/ijms160510324