Biomarkers in Bladder Cancer Surveillance
- 1Department of Medical Oncology, Mount Vernon Cancer Centre, Northwood, United Kingdom
- 2Department of Urology and Surgery, Lister Hospital, East and North Herts NHS Trust, Stevenage, United Kingdom
- 3School of Life and Medical Sciences, University of Hertfordshire, Hatfield, United Kingdom
Aim: This is a narrative review with an aim to summarise and describe urinary biomarkers in the surveillance of non-muscle-invasive bladder cancer (NMIBC). It provides a summary of FDA-approved protein biomarkers along with emerging ones which utilise genetic, epigenetic and exosomal markers. We discuss the current limitations of the available assays.
Background: Current guidelines advice a combination of cystoscopy, imaging,and urine cytology in diagnosis and surveillance. Although cytology has a high specificity, it is limited by low sensitivity particularly in low grade tumours. There are six FDA-approved urinary assays for diagnosis and surveillance of bladder cancer. They have shown to improve sensitivity and specificity to be used alongside cytology and cystoscopy but have a lower specificity in comparison to cytology and false positives often occur in benign conditions. Recent developments in laboratory techniques has allowed for use of markers which are RNA-, DNA-based as well as extracellular vesicles in the past decade.
Methods: Using the PubMed/Medline search engines as well as Google Scholar, we performed an online search using the terms “bladder cancer,” “non-muscle invasive bladder cancer,” and “urine biomarkers” with filter for articles in English published up to May 2021. Systematic reviews and original data of clinical trials or observational studies which contributed to the development of the biomarkers were collated.
Results: Biomarkers identified were divided into FDA-approved molecular biomarkers, protein biomarkers and gene-related biomarker with a table summarising the findings of each marker with the most relevant studies. The studies conducted were mainly retrospective. Due to the early stages of development, only a few prospective studies have been done for more recently developed biomarkers and limited meta-analyses are available.Therefore a detailed evaluation of these markers are still required to decide on their clinical use.
Conclusion: Advancements of analytical methods in BC has driven the research towards non-invasive liquid-based biomarkers in adjunct to urine cytology. Further large prospective studies are required to determine its feasibility in a clinical setting as they are not effective when used in isolation as they have their limitation. With the ongoing pandemic, other than reduction in costs and increased accuracy, the need for biomarkers to cope with delay in cystoscopies in diagnosis and surveillance is crucial. Thus clinical trials with direct comparison is required to improve patient care.
Introduction
Bladder cancer accounts for 90–95% of urothelial cancers. It is the eight most common cancer in women and fourth most common cancer in men (1). Most cases present with non-muscle invasive bladder cancer (NMIBC) and at early stages this carries a favourable prognosis. However, NMIBC accounts for 75% of cases and has a high recurrence rate of 80% in high-risk lesions and up to 50% in low risk. The 5 year survival rate is 94% if detected early and therefore early detection is imperative as intervention drastically influences overall survival (2).
Currently, bladder cystoscopy in combination with imaging of the upper urinary tract along with voided urine cytology as part of surveillance. NICE guidelines recommend cystoscopy to be done every 3 months for the first 2 years then every 6 months for the next 2 years then once a year thereafter. Cystoscopy is associated with complications such as a urinary tract infection, haematuria, pain. The utilisation of both imaging and cystoscopy is not effective in detecting smaller lesions. Urine cytology remains the most widely used non-invasive method for both diagnosis and surveillance of BC. Studies have shown a high specificity of 86% but this is limited by its low sensitivity of 48% as there is subjective nature when grading urothelial carcinoma on urine samples resulting in poor inter-observer variability (3). Although routinely used as the standard of truth for assessment of diagnostic accuracy, it is well-recognised that traditional cystoscopy with use of white light can lead to missing lesions that are present but not visible. New technologies exist to improve tumour visualisation. A recent study compared the use of blue light flexible cystoscopy with hexaminolevulinate (HAL, Hexvix®, Photocure ASA) with white light flexible cystoscopy for the detection of bladder cancer during surveillance, finding that 20.6 % (95% CI 11.5–32.7, p < 0.0001) of patients with recurrent cancer was seen only with blue light (4). The fact that a significant proportion of recurrences are missed under white light cystoscopy should be taken into consideration when assessing the sensitivity of new markers.
Urinary biomarkers play an important role in the future of precision medicine given the limitations of the current modalities being used given the specificity and sensitivity and need for invasive procedures to allow for surveillance. There is also a significant impact due to costs involved to healthcare services given the frequency and reliance on cystoscopy at present. This has led to the development of several non-invasive biomarkers which are now FDA approved. This is now particularly relevant with regard to low and intermediate risk patients who have had cystoscopies deferred with the ongoing pandemic. UroFollow is a multi-centre prospective trial exploring follow up using urine biomarkers in comparison to standard of care to explore if non-invasive methods are sufficient or patients with low grade or pTa G1–G2 BC (5). In addition to diagnostic accuracy, biomarkers need to be reproducible tests, affordable and easily implementable. This review's aim is to summarise biomarkers which have been identified for use in BC surveillance which are FDA-approved, commercially available and potential biomarkers in development.
FDA-Approved Molecular Biomarkers
The United States Food and Drug Administration (FDA) have currently approved 6 urinary assays to use alongside cystoscopy for diagnosis and surveillance. These include BTA stat (Polymedco), BTA TRAK (Polymedco), NMP22 enzyme linked immune-sorbent assay (ELISA) (Matritech), NMP22 BladderChek Test (Alere), uCyt (Scimedx) and UroVysion (Abbott Molecular).
NMP22
Nuclear matrix proteins are non chromatin structures which play several roles from DNA replication to gene expression and contributes to the infrastructure of the cell nucleus. During replication in healthy cells, NMP22 regulates the distribution of chromatin to daughter cells and this is normally at low levels. In urothelial tumours, levels of NMPs are high due to cell turnover from tumour apoptosis. NMP22 is one of them and it is the most investigated as an assay in both diagnosis and recurrence of bladder cancer.
Two modes of detection were FDA approved for both diagnosis and surveillance. NMP22 were initially detected with quantitative ELISA in a laboratory where cut-off values were utilised. The second was a qualitative point-of-care test, the NMP22 BladderChek where monoclonal antibodies are used to detect raised NMP22 levels in BC.
In 2015, Chou et al. had done a meta-analysis identifying qualitative NMP22 which has a sensitivity of 69% and specificity of 77% and qualitative NMP22 has 83% in specificity and 70% in sensitivity (6). A meta-analysis by Wang et al. in 2017 showed a pooled sensitivity from of 56% and specificity of 88% for bladder cancer detection from 19 studies (7). However the sensitivity was low when tumour stage and grade were considered with sensitivity increasing steadily with stage of 13.68, 29.49, and 74.03% for Ta to T1 and >T2, respectively. It was also found to have a better diagnostic performance in the Asian population. NMP22 measures the cell turnover that occurs with surface shedding from bladder tumour. This process occurs in benign conditions such as inflammation, infection, bladders stones and haematuria thus resulting in false-positive results.
Bladder Tumour Antigen (BTA) Assays
BTA tests detect human complement factor-H related protein in the urine which is produced by our bodies to protect cells from complement activation. It has an almost identical structure to the complement factor-H related protein produced by bladder cancer cells. There are two forms of BTA assays: (1) BTA Stat test: a “point-of-care (POC)” immunochromatographic assay which utilises five drops of urine to deliver a result within 5 min, and (2) BTA-TRAK test: standard quantitative ELISA measurement of the antigen. The FDA have approved them both for surveillance in BC in conjunction with cystoscopy only.
A meta-analysis conducted reviewing 13 studies identified specificity and sensitivity of BTA stat test to be 67 and 75%, respectively (8). Although BTA stat had shown higher sensitivity that urine cytology, the latter had better specificity. Chou et al. reviewed 22 studies identifying the sensitivity of BTA STAT was 64 % and specificity was 77%. For BTA-TRAK, four studies were evaluated and had similar results with a sensitivity of 65% and specificity was 74% (6). Similarly to other biomarkers, sensitivity had a positive correlation with increasing tumour grade of the BC.
Overall, the sensitivity and specificity of BTA Stat test ranges from 56 to 83% and 64 to 86% and with specificity up to 93% in individuals with benign conditions (9–12), and with BTA TRAK this ranges from 62 to 76% and 51 to 98% (13). Glas et al. carried out a meta-analysis and results of the bivariate analysis showed a sensitivity and specificity of cytology, BTA-Stat and BTA TRAK to be the following 55 and 94%; 70, 75, and 66%, and 65%, respectively (14). Given their lower specificities and similar issue of false positive results in benign conditions such as previous intravesical therapy, kidney stones, infection and presence of ureteric stents or nephrostomy tubes, theses tests are unable to replace cytology and can only be used concurrently as part of surveillance (9, 12, 15, 16).
UroVysion
UroVysion is a molecular test using multicolour fluorescence in situ hybridisation (FISH) assay to detect aneuploidy of chromosomes 3, 7, and 17 and loss of the p16 gene at the 9p21 locus which are genetic abnormalities seen in BC. A sample must have a minimum of 25 cells to be analysed and a positive test is defined by one of the following: (1) Four or more morphologically abnormal cells have polysomy of two or more chromosomes (3, 7, or 17) (2) ≥10 cells with gain of a single chromosome (3) homozygous deletion of 9p21 in 12 cells (16).
Pooled results from a meta-analysis of 13 studies showed a specificity of 83% and sensitivity of 72% in comparison to urine cytology with 96 and 42%, respectively (17). UroVysion showed the sensitivity and specificity of 75.6 and 84.8%, respectively for high grade UCC, 40.8 and 87.8%, respectively for lowgrade UCC (18). Thus it faced a similar challenge to biomarkers in detection of low grade or low stage tumours (19). However the advantage of this assay is the absence of benign conditions such as cystitis, inflammation or haematuria affecting results.
In surveillance, Yoder et al. identified over a period of 29 months that 65% of the cases with positive UroVysion but no visible lesions developed recurrence on follow-up but this was not the case for Dimashkieh et al. as where 46% (158 of 343) of patients who had positive UroVysion tests did not develop UCC during up to the 3 year follow-up (18, 20). Therefore there is variability in its clinical utility. There is also evidence to show its potential in assessing response to intravesical BCG therapy for NMIBC (21).
Immunocyt/Ucyt + Test
The Immunocyt/Ucyt+ test uses three fluorescent monoclonal antibodies (M344, LDQ10, and 19A211) which detect carcinoembryonic antigen and sulphated mucin glycoproteins on exfoliated urothelial cells in voided urine. Compoj et al. evaluated 7,244 cases and identified an overall sensitivity of 34.5% for cytology and 68.1% for uCyt+/ImmunoCyt and 97.9% for cytology, 72.3% for uCyt+/ImmunoCyt (22). There was a positive correlation with higher grade and specificity along with sensitivity as observed with other biomarkers. A meta-analysis identified a sensitivity of ImmunoCyt to be 75% and specificity was 78% and in comparison to NMP22, BTA and FISH, it had the highest pooled sensitivity (6). A split study comparing UroVysion, ImmunoCyt and cytology supported this with Immunocyst being more sensitive in detecting low grade tumours (23). Further meta-analysis also supported previous evidence to support the use of Immunocyt in combination with cytology in surveillance to reduce the frequency of follow up required in low risk cancers (24).
However, this test involves advanced technical expertise as a minimum of 500 cells need to be analysed for fluorescence to provide accurate results and thus there is interobserver variability and need for high cellularity specimens. It can be affected by benign conditions such as haematuria albeit not as easily as other biomarkers above (25).
Promising Protein Biomarkers
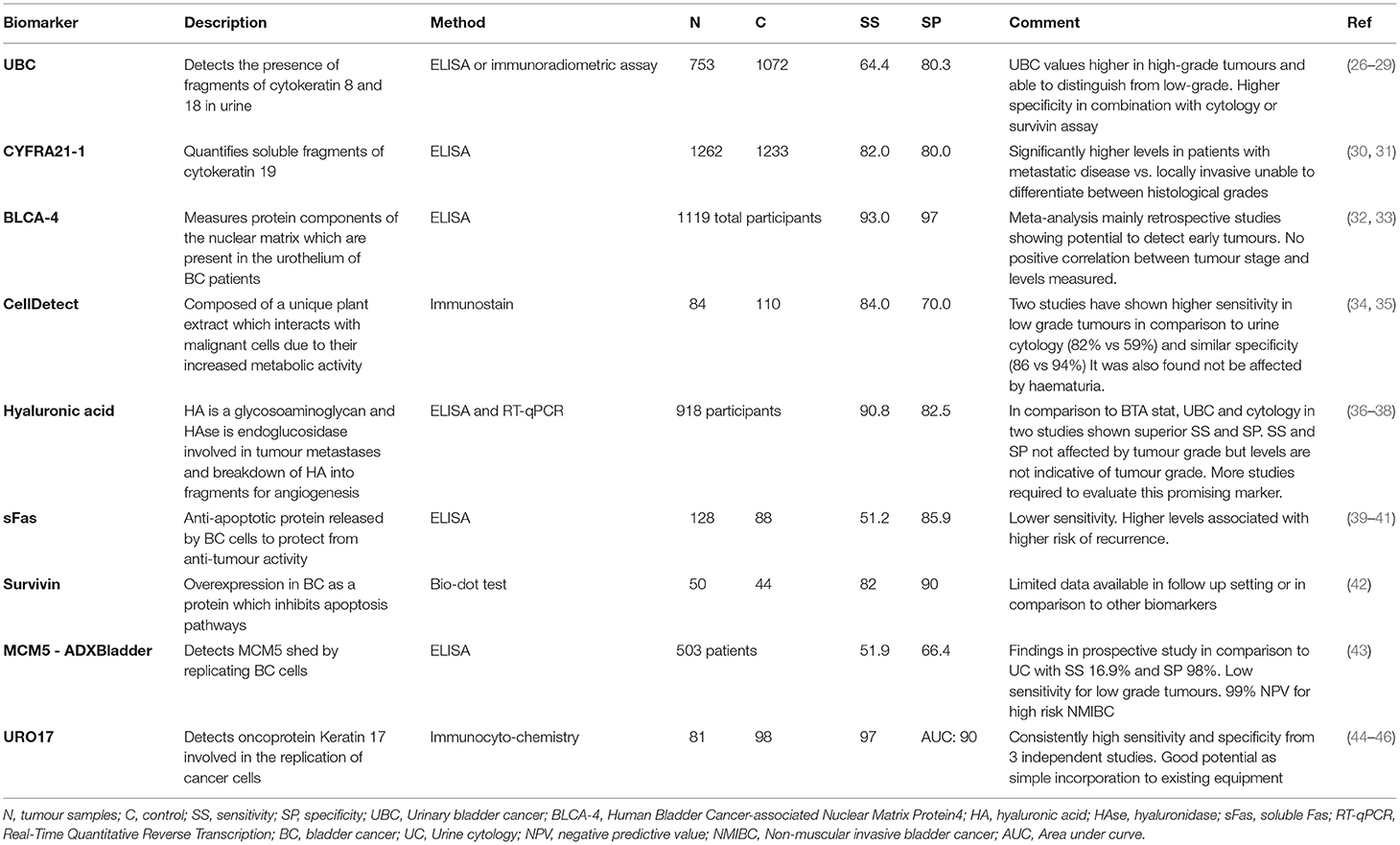
Table 1 summarises potential protein biomarkers which can be used in BC surveillance highlighting meta-analysis and most relevant study in the table.
The UK National Health Service (NHS) approved the usage of ADxBladder in BC detection. Three prospective studies have been done with only one in the surveillance setting (43). They reported an overall sensitivity ranging between 45–73%, specificity between 70–73%, and NPV between 74–100% and were superior to cytology (47). Given the turnaround time of 2h, it being relatively unaffected by benign conditions such as inflammation or haematuria and consisting of a single biomarker identifiable with ELISA which is readily available in labs and costing only £0.37 per person, this made ADxBladder a viable option (48). However, in comparison to other biomarkers identified, it has a low sensitivity and specificity as displayed in Table 1 and poor performance in detection of low grade tumours.
Of the new protein biomarkers that were introduced in recent years, URO17 test utilising Keratin 17 (K17) has shown especially promising results. Babu et al. had identified high sensitivity and specificity of URO17 of 100% using urine samples in a retrospective study (44). Interestingly, URO17 is able to detect both low and high grade cancers in patients presenting with haematuria, a previously excluded cohort, thus proving its benefit of use in a surveillance setting as well (45). There is a specificity of 96 and 92.7% in recurrent and newly diagnosed patients, respectively (44, 45). Given these outcomes and its easy adaptation to current equipment used, a larger prospective study in a surveillance setting would be beneficial in developing this into a promising protein biomarker test for non-invasive surveillance of NMIBC (45, 46).
Gene-Related Biomarkers
Genetic alterations has been explored as another avenue for detecting bladder cancer in surveillance. To discuss this further we will divide these into the following groups: DNA methylation markers, histone tail modifications, miRNA biomarkers, microsatellite analysis and multi-gene panels.
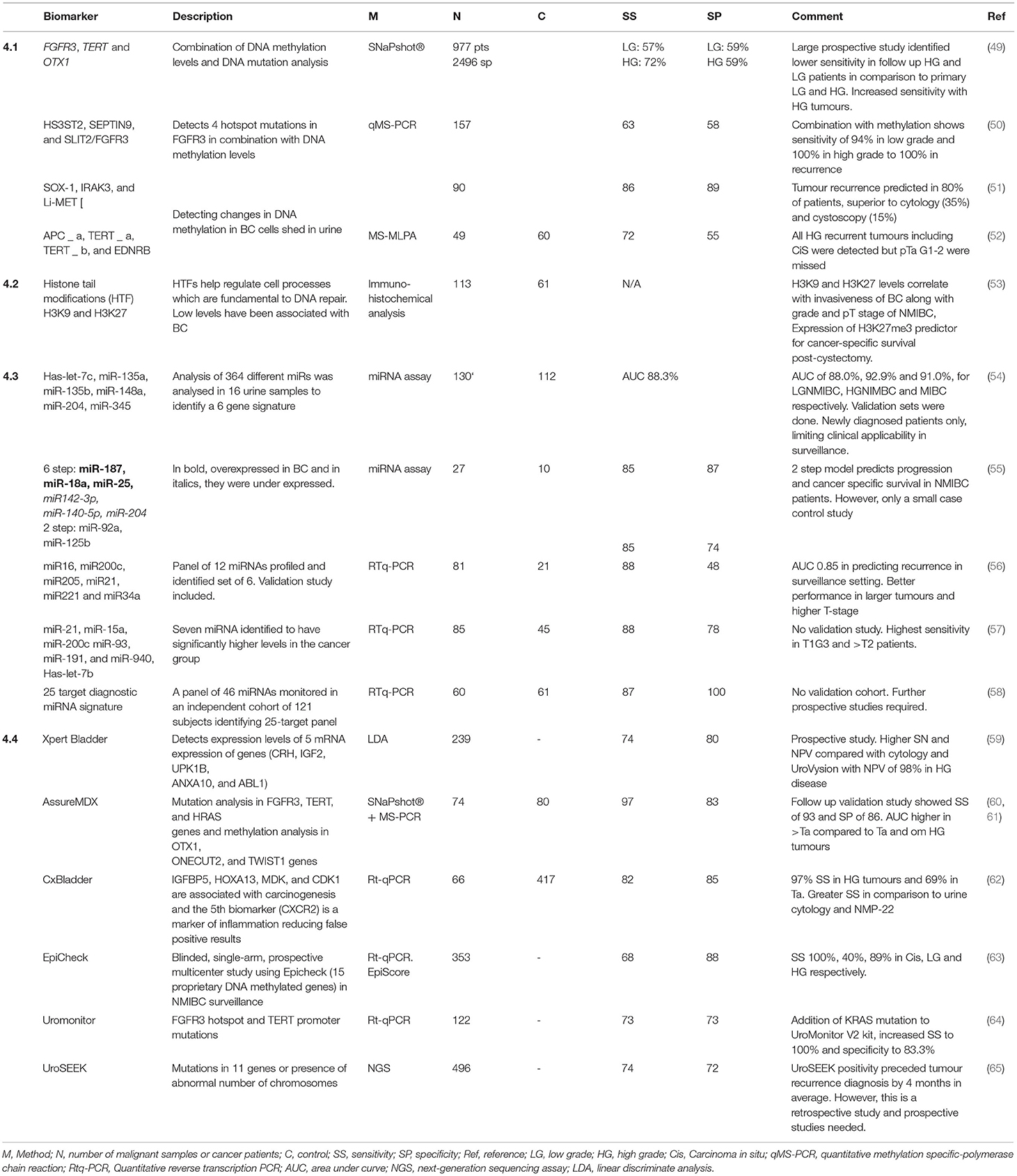
Table 2 summarises detection of genetic alterations to utilise as biomarkers listing the most relevant study accounting for those with the largest patient groups and most representative of the target group.
DNA Methylation Markers
Epigenetic alterations are part of the carcinogenesis. DNA hypermethylation of the CpG islands play a role in the promoter regions of tumour-suppressor genes. This mediates silencing of the affiliated gene which is a known phenomenon in BC. The hyper or hypomethylation of these genes can be detected in tumour cells that are shed into urine and aid diagnosis of BC. This has been reviewed in both primary and recurrent tumours. Bosschieter et al. evaluated 42 studies and identified 8 with high sensitivity and specificity with varying methodologies and heterogenous patient groups (66). Studies with promising results, had no independent validation data and Costa et al. with 94% specificity and 90% sensitivity did not report on tumour grade or stage (67). This is relevant as similarly to other reported biomarkers, results will vary with disease spectrum. As shown in Table 2 section DNA Methylation Markers studies in recurrence are listed but these are mainly small retrospective case-control studies (50). Beuker at al, as shown in Table 2, used a combination of this technique along with DNA mutation analysis with FGFR3 and TERT mutation analysis to improve detection rates showed similar results as increased sensitivity in high grade tumour cells likely due to increased shedding of BC cells (49). There is an insufficient amount of data due to variability in methodology, patient groups and gene panel selection. Studies have used it in combination with DNA mutation analysis.
Histone Tail Modifications
Other than epigenetic changes described above, another manifestation of this is histone lysine methylation (HxKy). Histone modifications help regulate numerous cell mechanisms such as chromosome condensation, DNA repair and transcription. The site and degree of histone methylation determines the transcriptional activity. H3K9, as mentioned in Table 2 section Histone Tail Modifications are associated with repressed transcription. Other potential histone modications identified are H3K4 and H3K20 methylation which were decreased in BC compared to normal patients and global H4K20me3 levels were predictive for bladder cancer-specific survival (68).
miRNA Biomarkers
Micro RNAs (miRNA) are short noncoding RNAs that regulate process post-transcriptionally and dysregulation leads to carcinogenesis. The aberrant expression of miRNA has led to its potential use as a biomarker. It can present in bodily fluids as they are protected by RNAse degradation because they are excreted as membrane-protected free circulating miRNAs or in extracellular vesicles (EVs) such as exosomes (69). Initially identification was done using qtPCR but now rapid profiling is done using microassays and miRNA sequencing (56).
Studies listed in Table 2 section miRNA Biomarkers are those with sensitivities of more than 80%. Multiple miRNA diagnostic assays had better sensitivity than single miRNA assays. Chen et al. carried out a meta-analysis 30 studies with 1019 BC patients and 690 controls identifying a pool sensitivity and specificity of 80 and 74%, respectively (70). The AUC for NMIBC was 0.84 and 0.76 for MIBC suggesting higher diagnostic ability in NMIBC patients. Another meta-analysis by Shi et al. evaluated 1,556 cases and 1,347 controls from 31 studies with a pooled specificity and sensitivity of 72 and 76%, respectively (71).
Most studies compared a heterogenous group of BC patients with controls. Study which explored the recurrence setting in both NMIBC and MIBC using miR-145 and miR-200a. This identified a sensitivity of 78% and specificity of 61% in NMIBC patients where lower levels of miR-145 associated with higher grade and lower levels of miR-200a independently predicted recurrence (72). Prospective trials in BC surveillance are required to validate the clinical applicability of this biomarker.
Multi-Gene Panels
Several assays detecting mRNA biomarkers have been conducted. Table 2 section Multi-Gene Panels summarises them. CxBladder has been extensively studied and has variations which include: (1) Cxbladder® Detect to detect bladder cancer in hematuria patients with a sensitivity of 82% and specificity of 85% (62). (2) Cxbladder® Triage which is used in hematuria patients to rule out BC with a sensitivity of 95% and negative predictive value of 97% (73). (3) Cxbladder® Monitor as a complement to surveillance. It has been compared with urine cytology, NMP22 BladderChek and NMP22 ELISA with a superior SS and SP of 91/96 vs. 22/87%, 11/87 and 26/86 % (74). Koya et al. implemented CxBladder Monitor (CxBM) into local guidelines whereby low risk patients had alternate annual CxBM and cystoscopy therearfter (75). They found that 77.8% of patients were safely managed by only one cystoscopy every 2 years, reducing the total number of annual cystoscopies by 39%. This was reflected in a real world data analysis identifying this advantage of CxBM in clinical practice to have driven its increased utility (76).
Other Possible Gene-Related Biomarkers
Microsatellite analysis (MSA) through PCR targets highly pleomorphic short tandem repeats (STR) which occur in cancer cells with loss of heterozygosity (LOH) causing microsatellite instability. This occurs because of epigenetic silencing or inactivation of the mismatch repair gene which play an integral part in the proliferation of cancer cells. The most common LOH is in chromosome nine but this is also seen to occur in chromosome 4, 8, 11, and 17p (77–80). In comparison to urine cytology, sensitivity was 97 vs. 79% with 95–100% in low grade tumours in a small study of 34 cancer patients with 21 cancer-free subjects (81). A prospective study of 228 patients undergoing BC surveillance had a specificity and sensitivity of 58 and 74%, respectively (82). A further prospective study of 91 patients evaluating MSA in combination with cytology had a sensitivity of 72% in G1–2 and 96% in G3. They found using LOH analysis to improve specificity and all recurrence cases were identified (83). Overall, this test has good sensitivity but difficult to incorporate into present laboratories due to its complexity. Larger prospective studies which include a validation cohort to assess feasibility is required.
Extracellular Vesicles and Exosomes
Exosomes are vesicles secreted by cells which mediate extracellular communication by transmitting proteins, lipids, miRNA, mRNA and long non-coding RNAs (lncRNA). Extracellular vesicles in BC cells carry a vast number of proteins which is utilised in angiogenesis and cell migration thus aiding further tumour progression which can be utilised as markers but possible novel therapeutic targets (84). Different analytical methods have identified various proteins and miRNAs in this rich extracellular environment. A small study isolated EV using microchip ELISA and found highly elevated EV levels in BC patients compared to controls (85). Profiling of proteomes in exosomes identified a correlation with tumour grade and the ability to predict recurrences with 1-antitrypsin and histone H2B1 exosome proteins (86). In another study, urinary EVs were isolated and deregulated miRNAs were identified as potential biomarkers, in particular, miR-375 for high-grade bladder cancer while miR-146a for low-grade patients (87).
EVs are promising as a source of biomarkers given the diverse cargoes EVs carry. However, there are several limitations such as isolation techniques and testing not being standardised and therefore it is difficult to compare results between groups given lack of reproducibility. Studies conducted are heterogenous and small without any validation sets (88). Optimisation of testing could lead to better EV studies allowing for real EV biomarker development in a clinical setting and could further inform us further on tumour biology.
Conclusion
This paper has highlighted the various biomarkers in urothelial cancer and their significance in early diagnosis of bladder cancer. Whilst it's important to have biomarkers in NMIBC, differences in sensitivity and specificity limits their use in the community. These biomarkers have a significant role in future diagnosis of bladder cancer, and future studies will guide clinicians in using the most appropriate marker for screening. The advancement in analytical methods in BC has driven the research towards non-invasive liquid-based biomarkers in adjunct to urine cytology. This paper provides evidence that a second modality of screening tool may be beneficial to use in the diagnostic algorithm for bladder cancer. Studies identifying its feasibility in a clinical enviroment is important as they have limitations when used in isolation. Given this is a narrative review, further evaluation of these promising markers is required in more depth in terms of a meta-analysis along with the development of prospective studies in a surveillance setting. Meta-analyses on the newer markers have not been conducted as there is variability in patient cohorts utilised and more studies need to be conducted to obtain sufficient data. In addition to this, majority of studies are in a restrospective setting and prospective studies need to be developed to be able to further evaluate their clinical feasibility.
The ongoing pandemic has further accentuated the increasing need and relevance for biomarkers to cope with delay in cystoscopies in both diagnosis and surveillance. The use of more sensitive methods to detect true tumour recurrences could also play a role in assessment of the diagnostic accuracy of these markers, potentially reducing the number of cystoscopies for test-negative cases and introducing methods like blue light cystoscopy for test-positive cases. Further large, prospective clinical trials incorporating these biomarkers and usage of newer analytical methods in screening for high-risk patients and also in disease recurrence in will allow for its use in a clinical setting.
Author Contributions
SS collated and summarised studies to write up majority of this review. KN and AN were involved in editing. AS and NV contributed to the introduction and conclusion. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Richters A, Aben KKH, Kiemeney LALM. The global burden of urinary bladder cancer: an update. World J Urol. (2019) 38:1895–904. doi: 10.1007/s00345-019-02984-4
2. Cambier S, Sylvester RJ, Collette L, Gontero P, Brausi MA, Van Andel G, et al. EORTC nomograms and risk groups for predicting recurrence, progression, and disease-specific and overall survival in non–muscle-invasive stage Ta–T1 urothelial bladder cancer patients treated with 1–3 years of maintenance bacillus calmette-guérin. Eur Urol. (2016) 69:60–9. doi: 10.1016/j.eururo.2015.06.045
3. Reid MD, Osunkoya AO, Siddiqui MT, Looney SW. Accuracy of grading of urothelial carcinoma on urine cytology: an analysis of interobserver and intraobserver agreement. Int J Clin Exp Pathol. (2012) 5:882–91.
4. Daneshmand S, Patel S, Lotan Y, Pohar K, Trabulsi E, Woods M, et al. Efficacy and safety of blue light flexible cystoscopy with hexaminolevulinate in the surveillance of bladder cancer: a phase III, comparative, multicenter study. J Urol. (2018) 199:1158–65. doi: 10.1016/j.juro.2017.11.096
5. Benderska-Söder N, Hovanec J, Pesch B, Goebel PJ, Roghmann F, Noldus J, et al. Toward noninvasive follow-up of low-risk bladder cancer - rationale and concept of the urofollow trial. Urol Oncol. (2020) 38: 886–95. doi: 10.1016/j.urolonc.2020.01.006
6. Chou R, Gore JL, Buckley D, Fu R, Gustafson K, Griffin JC, et al. Urinary biomarkers for diagnosis of bladder cancer: a systematic review and meta-analysis. Ann Intern Med. (2015) 163:922–31. doi: 10.7326/M15-0997
7. Wang Z, Que H, Suo C, Han Z, Tao J, Huang Z, et al. Evaluation of the NMP22 BladderChek test for detecting bladder cancer: a systematic review and meta-analysis. Oncotarget. (2017) 8:100648–56. doi: 10.18632/oncotarget.22065
8. Guo A, Wang X, Gao L, Shi J, Sun C, Wan Z. Bladder tumour antigen (BTA stat) test compared to the urine cytology in the diagnosis of bladder cancer: a meta-analysis. Can Urol Assoc J. (2014) 8:E347–52. doi: 10.5489/cuaj.1668
9. Sarosdy MF, Hudson MLA, Ellis WJ, Soloway MS, White Rd, Sheinfeld J, et al. Improved detection of recurrent bladder cancer using the bard bta stat test. Urology. (1997) 50:349–53. doi: 10.1016/S0090-4295(97)00292-6
10. Pode DOV, Shapiro A, Wald M, Nativ O, Laufer M, Kaver I, et al. TEST. J Urol. (1999) 161:443–6. doi: 10.1016/S0022-5347(01)61918-9
11. Heicappell R, Schostak M, Müller M, Miller K. Evaluation of urinary bladder cancer antigen as a marker for diagnosis of transitional cell carcinoma of the urinary bladder. Scand J Clin Lab Invest. (2000) 60:275–82. doi: 10.1080/003655100750046431
12. Raitanen MP. The role of BTA stat Test in follow-up of patients with bladder cancer: results from FinnBladder studies. World J Urol. (2008) 26:45–50. doi: 10.1007/s00345-007-0230-3
13. Thomas L, Leyh H, Marberger M. Multicenter trial of the quantitative bta trak assay in the detection of bladder cancer. Clin Chem. (2021) 45:472–7.
14. Glas AS, Roos D, Deutekom M, Zwinderman AH, Bossuyt PM, Kurth KH. Tumor markers in the diagnosis of primary bladder cancer. A systematic review. J Urol. (2003) 169:1975–82. doi: 10.1097/01.ju.0000067461.30468.6d
15. Sharma S, Zippe CD, Pandrangi L, Nelson D, Agarwal A. Exclusion criteria enhance the specificity and positive predictive value of NMP22 and BTA stat. J Urol. (1999) 162:53–7. doi: 10.1097/00005392-199907000-00014
16. Lokeshwar VB, Habuchi T, Grossman HB, Murphy WM, Hautmann SH, Hemstreet GP III, et al. Bladder tumor markers beyond cytology: international consensus panel on bladder tumor markers. Urology. (2005) 66(Suppl 1):35–63. doi: 10.1016/j.urology.2005.08.064
17. Hajdinjak T. UroVysion FISH test for detecting urothelial cancers: meta-analysis of diagnostic accuracy and comparison with urinary cytology testing. Urolo Oncol. (2008) 26:646–51. doi: 10.1016/j.urolonc.2007.06.002
18. Dimashkieh H, Wolff DJ, Smith TM, Houser PM, Nietert PJ, Yang J. Evaluation of urovysion and cytology for bladder cancer detection: a study of 1835 paired urine samples with clinical and histologic correlation. Cancer Cytopathol. (2013) 121:591–7. doi: 10.1002/cncy.21327
19. Sokolova IA, Halling KC, Jenkins RB, Burkhardt HM, Meyer RG, Seelig SA, et al. The development of a multitarget, multicolor fluorescence in situ hybridization assay for the detection of urothelial carcinoma in urine. J Mol Diagn. (2000) 2:116–23. doi: 10.1016/S1525-1578(10)60625-3
20. Yoder BJ, Skacel M, Hedgepeth R, Babineau D, Ulchaker JC, Liou LS, et al. Reflex UroVysion testing of bladder cancer surveillance patients with equivocal or negative urine cytology: a prospective study with focus on the natural history of anticipatory positive findings. Am J Clin Pathol. (2007) 127:295–301. doi: 10.1309/ADJL7E810U1H42BJ
21. Savic S, Zlobec I, Thalmann GN, Engeler D, Schmauss M, Lehmann K, et al. The prognostic value of cytology and fluorescence in situ hybridization in the follow-up of nonmuscle-invasive bladder cancer after intravesical Bacillus Calmette-Guerin therapy. Int J Cancer. (2009) 124:2899–904. doi: 10.1002/ijc.24258
22. Comploj E, Mian C, Ambrosini-Spaltro A, Dechet C, Palermo S, Trenti E, et al. uCyt+/ImmunoCyt and cytology in the detection of urothelial carcinoma: an update on 7422 analyses. Cancer Cytopathol. (2013) 121:392–7. doi: 10.1002/cncy.21287
23. Sullivan PS, Nooraie F, Sanchez H, Hirschowitz S, Levin M, Rao PN, et al. Comparison of immunoCyt, UroVysion, and urine cytology in detection of recurrent urothelial carcinoma cancer. Cytopathology. (2021) 117:167–73. doi: 10.1002/cncy.20026
24. He H, Han C, Hao L, Zang G. ImmunoCyt test compared to cytology in the diagnosis of bladder cancer: A meta-analysis. Oncol Lett. (2016) 12:83–8. doi: 10.3892/ol.2016.4556
25. Todenhöfer T, Hennenlotter J, Tews V, Gakis G, Aufderklamm S, Kuehs U, et al. Impact of different grades of microscopic hematuria on the performance of urine-based markers for the detection of urothelial carcinoma. Urol Oncol. (2013) 31:1148–54. doi: 10.1016/j.urolonc.2011.10.011
26. Ecke TH, Weiß S, Stephan C, Hallmann S, Arndt C, Barski D, et al. UBC® Rapid Test. A Urinary Point-of-Care (POC) assay for diagnosis of bladder cancer with a focus on non-muscle invasive high-grade tumors: results of a multicenter-study. Int J Mol Sci. (2018) 19:3841. doi: 10.3390/ijms19123841
27. Lu P, Cui J, Chen K, Zhang J, Tao J, Han Z, et al. Diagnostic accuracy of the UBC® Rapid Test for bladder cancer: a meta-analysis. Oncol Lett. (2021) 16:3770–8. doi: 10.3892/ol.2018.9089
28. Gleichenhagen J, Arndt C, Casjens S, Meinig C, Gerullis H, Raiko I, et al. Evaluation of a New Surviving ELISA and UBC® rapid for the detection of bladder cancer in urine. Int J Mol Sci. (2018) 19:226. doi: 10.3390/ijms19010226
29. D'Costa JJ, Goldsmith JC, Wilson JS, Bryan RT, Ward DG. A systematic review of the diagnostic and prognostic value of urinary protein biomarkers in urothelial bladder cancer. Bladder Cancer. (2016) 2:301–17. doi: 10.3233/BLC-160054
30. Guo X-G, Long J-J. Cytokeratin-19 fragment in the diagnosis of bladder carcinoma. Tumor Biol. (2016) 37:14329–30. doi: 10.1007/s13277-016-5223-7
31. Kuang L, Song W, Qing H, Yan S, Song F. CYFRA21-1 levels could be a biomarker for bladder cancer: a meta-analysis. Genet Mol Res. (2015) 14:3921–31. doi: 10.4238/2015.April.27.6
32. Alavi A, Izadpanahi M-H, Haghshenas L, Faridizad R, Eslami M-J, Ghadimi K. Comparing urine levels of BLCA-4 nuclear matrix protein in patients with bladder cancer and non-bladder cancer. Int J Physiol Pathophysiol Pharmacol. (2019) 11:289–92.
33. Cai Q, Wu Y, Guo Z, Gong R, Tang Y, Yang K, et al. Urine BLCA-4 exerts potential role in detecting patients with bladder cancers: a pooled analysis of individual studies. Oncotarget. (2015) 6:37500. doi: 10.18632/oncotarget.6061
34. Davis N, Shtabsky A, Lew S, Rona R, Leibovitch I, Nativ O, et al. A novel urine-based assay for bladder cancer diagnosis: multi-institutional validation study. Eur Urol Focus. (2018) 4:388–94. doi: 10.1016/j.euf.2016.10.004
35. Nativ O, Halachmi S, Biton K, Zlotnik M, Yoffe C, Davis N, et al. PD19-09 PERFORMANCE OF A NOVEL URINE-BASED BIOMARKER FOR THE MONITORING OF BLADDER CANCER RECURRENCE. J Urol. (2017) 197:e368–82. doi: 10.1016/j.juro.2017.02.882
36. Liang Z, Zhang Q, Wang C, Shi F, Cao H, Yu Y, et al. Hyaluronic acid/Hyaluronidase as biomarkers for bladder cancer: a diagnostic meta-analysis. Neoplasma. (2017) 64:901–8. doi: 10.4149/neo_2017_612
37. Lokeshwar VB, Schroeder GL, Selzer MG, Hautmann SH, Posey JT, Duncan RC, et al. Bladder tumor markers for monitoring recurrence and screening comparison of hyaluronic acid hyaluronidase and BTA-Stat tests. Cancer. (2002) 95:61–72. doi: 10.1002/cncr.10652
38. Schroeder GL, Lorenzo-Gomez M-F, Hautmann SH, Friedrich MG, Ekici S, Huland H, et al. A side by side comparison of cytology and biomarkers for bladder cancer detection. J Urol. (2004) 172:1123–6. doi: 10.1097/01.ju.0000134347.14643.ab
39. Srivastava AK, Singh PK, Singh D, Dalela D, Rath SK, Bhatt ML. Clinical utility of urinary soluble Fas in screening for bladder cancer. Asia Pac J Clin Oncol. (2016) 12:e215–21. doi: 10.1111/ajco.12165
40. Yang H, Li H, Wang Z, Gao J, Guo Y. Is urinary soluble Fas an independent predictor of non-muscle-invasive bladder cancer? A prospective chart study. Urol Int. (2013) 91:456–61. doi: 10.1159/000350752
41. Svatek RS, Herman MP, Lotan Y, Casella R, Hsieh JT, Sagalowsky AI, et al. Soluble Fas a promising novel urinary marker for the detection of recurrent superficial bladder cancer. Cancer. (2006) 106:1701–7. doi: 10.1002/cncr.21795
42. Kenney DM, Geschwindt RD, Kary MR, Linic JM, Sardesai NY, Li Z-Q. Detection of newly diagnosed bladder cancer, bladder cancer recurrence and bladder cancer in patients with hematuria using quantitative rt-PCR of urinary surviving. Tumor Biol. (2007) 28:57–62. doi: 10.1159/000099033
43. Gontero P, Montanari E, Roupret M, Longo F, Stockley J, Kennedy A, et al. Comparison of the performances of the ADXBLADDER test and urinary cytology in the follow-up of non-muscle-invasive bladder cancer: a blinded prospective multicentric study. BJU Int. (2021) 127:198–204. doi: 10.1111/bju.15194
44. Babu S, Mockler DC, Roa-Peña L, Szygalowicz A, Kim NW, Jahanfard S, et al. Keratin 17 is a sensitive and specific biomarker of urothelial neoplasia. Mod Pathol. (2019) 32:717–24. doi: 10.1038/s41379-018-0177-5
45. Vasdev N, Hampson A, Agarwal S, Swamy R, Chilvers M, Hampson A, et al. The role of URO17™ biomarker to enhance diagnosis of urothelial cancer in new haematuria patients – first European data. (2020) 2:46–52. doi: 10.1002/bco2.50
46. Babu S, Kim NW, Wu M, Chan I, Escobar-Hoyos LF, Shroyer KR. Keratin 17 is a novel cytologic biomarker for urothelial carcinoma diagnosis. Am J Clin Pathol. (2021) doi: 10.1093/ajcp/aqab050
47. Wolfs JRE, Hermans TJN, Koldewijn EL, van de Kerkhof D. Novel urinary biomarkers ADXBLADDER and bladder EpiCheck for diagnostics of bladder cancer: a review. Urol Oncol. (2021) 39:161–70. doi: 10.1016/j.urolonc.2020.11.014
48. Dudderidge T, Nabi G, Mom J, Umez-Eronini N, Hrouda D, Cresswell J, et al. A novel non-invasive aid for bladder cancer diagnosis: a prospective, multi-centre study to evaluate the ADXBLADDER test. Eur Urol Suppl. (2018) 17:31424. doi: 10.1016/S1569-9056(18)31835-9
49. Beukers W, van der Keur KA, Kandimalla R, Vergouwe Y, Steyerberg EW, Boormans JL, et al. FGFR3, TERT and OTX1 as a Urinary Biomarker Combination for Surveillance of Patients with Bladder Cancer in a Large Prospective Multicenter Study. J Urol. (2017) 197:1410–8. doi: 10.1016/j.juro.2016.12.096
50. Roperch J-P, Grandchamp B, Desgrandchamps F, Mongiat-Artus P, Ravery V, Ouzaid I, et al. Promoter hypermethylation of HS3ST2, SEPTIN9 and SLIT2 combined with FGFR3 mutations as a sensitive/specific urinary assay for diagnosis and surveillance in patients with low or high-risk non-muscle-invasive bladder cancer. BMC Cancer. (2016) 16:1–9. doi: 10.1186/s12885-016-2748-5
51. Su S-F, de Castro Abreu AL, Chihara Y, Tsai Y, Andreu-Vieyra C, Daneshmand S, et al. A panel of three markers hyper-and hypomethylated in urine sediments accurately predicts bladder cancer recurrence. Clin Cancer Res. (2014) 20:1978–89. doi: 10.1158/1078-0432.CCR-13-2637
52. Zuiverloon TC, Beukers W, van der Keur KA, Munoz JR, Bangma CH, Lingsma HF, et al. A methylation assay for the detection of non-muscle-invasive bladder cancer (NMIBC) recurrences in voided urine. BJU Int. (2012) 109:941–8. doi: 10.1111/j.1464-410X.2011.10428.x
53. Liu J, Li Y, Liao Y, Mai S, Zhang Z, Liu Z, et al. High expression of H3K27me3 is an independent predictor of worse outcome in patients with urothelial carcinoma of bladder treated with radical cystectomy. Biomed Res Int. (2013) 2013:390482. doi: 10.1155/2013/390482
54. Hofbauer SL, de Martino M, Lucca I, Haitel A, Susani M, Shariat SF, et al. A urinary microRNA (miR) signature for diagnosis of bladder cancer. Urol Oncol. (2018) 36:531.e1–8. doi: 10.1016/j.urolonc.2018.09.006
55. Mengual L, Lozano JJ, Ingelmo-Torres M, Gazquez C, Ribal MJ, Alcaraz A. Using microRNA profiling in urine samples to develop a non-invasive test for bladder cancer. Int J Cancer. (2013) 133:2631–41. doi: 10.1002/ijc.28274
56. Sapre N, Anderson PD, Costello AJ, Hovens CM, Corcoran NM. Gene-based urinary biomarkers for bladder cancer: an unfulfilled promise? Urol Oncol. (2014) 32:48.e9–17. doi: 10.1016/j.urolonc.2013.07.002
57. Long JD, Sullivan TB, Humphrey J, Logvinenko T, Summerhayes KA, Kozinn S, et al. A non-invasive miRNA based assay to detect bladder cancer in cell-free urine. Am J Transl Res. (2015) 7:2500–9.
58. Urquidi V, Netherton M, Gomes-Giacoia E, Serie DJ, Eckel-Passow J, Rosser CJ, et al. A microRNA biomarker panel for the non-invasive detection of bladder cancer. Oncotarget. (2016) 7:86290–9. doi: 10.18632/oncotarget.13382
59. Valenberg FJPv, Hiar AM, Wallace E, Bridge JA, Mayne DJ, Beqaj S, et al. Prospective validation of an mRNA-based urine test for surveillance of patients with bladder cancer. Eur Urol. (2019) 75:853–60. doi: 10.1016/j.eururo.2018.11.055
60. van Kessel KEM, Van Neste L, Lurkin I, Zwarthoff EC, Van Criekinge W. Evaluation of an epigenetic profile for the detection of bladder cancer in patients with hematuria. J Urol. (2016) 195:601–7. doi: 10.1016/j.juro.2015.08.085
61. van Kessel KEM, Beukers W, Lurkin I, Ziel-van der Made A, van der Keur KA, Boormans JL, et al. Validation of a DNA methylation-mutation urine assay to select patients with hematuria for cystoscopy. J Urol. (2017) 197(3 Part 1):590–5. doi: 10.1016/j.juro.2016.09.118
62. O'Sullivan P, Sharples K, Dalphin M, Davidson P, Gilling P, Cambridge L, et al. A multigene urine test for the detection and stratification of bladder cancer in patients presenting with hematuria. J Urol. (2012) 188:741–7. doi: 10.1016/j.juro.2012.05.003
63. Witjes JA, Morote J, Cornel EB, Gakis G, van Valenberg FJP, Lozano F, et al. Performance of the Bladder EpiCheck. Methylation test for patients under surveillance for non muscle-invasive bladder cancer: results of a multicenter, prospective, blinded clinical trial. Eur Urol Oncol. (2018) 1:307–13. doi: 10.1016/j.euo.2018.06.011
64. Batista R, Vinagre J, Prazeres H, Sampaio C, Peralta P, Conceicao P, et al. Validation of a novel, sensitive, and specific urine-based test for recurrence surveillance of patients with non-muscle-invasive bladder cancer in a comprehensive multicenter study. Front Genet. (2019) 10:1237. doi: 10.3389/fgene.2019.01237
65. Pena MDCR, Springer SU, Taheri D, Li L, Tregnago AC, Eich M-L, et al. Performance of novel non-invasive urine assay UroSEEK in cohorts of equivocal urine cytology. Virchows Archiv. (2019) 476:423–9. doi: 10.1007/s00428-019-02654-1
66. Bosschieter J, Lutz C, Segerink LI, Vis AN, Zwarthoff EC, van Moorselaar RJ, et al. The diagnostic accuracy of methylation markers in urine for the detection of bladder cancer: a systematic review. Epigenomics. (2018) 10:673–87. doi: 10.2217/epi-2017-0156
67. Costa VL, Henrique R, Danielsen SA, Duarte-Pereira S, Eknaes M, Skotheim RI, et al. Three epigenetic biomarkers, GDF15, TMEFF2, and VIM, accurately predict bladder cancer from DNA-based analyses of urine samples. (1557–3265 (Electronic)). 16:584–51. doi: 10.1158/1078-0432.CCR-10-1312
68. Schneider AC, Heukamp LC, Rogenhofer S, Fechner G, Bastian PJ, von Ruecker A, et al. Global histone H4K20 trimethylation predicts cancer-specific survival in patients with muscle-invasive bladder cancer. BJU Int. (2011) 108:E290–6. doi: 10.1111/j.1464-410X.2011.10203.x
69. Cortez MA, Bueso-Ramos C, Ferdin J, Lopez-Berestein G, Sood AK, Calin GA. MicroRNAs in body fluids–the mix of hormones and biomarkers. Nat Rev Clin Oncol. (2011) 8:467–77. doi: 10.1038/nrclinonc.2011.76
70. Chen L, Cui Z, Liu Y, Bai Y, Lan F. MicroRNAs as biomarkers for the diagnostics of bladder cancer: a meta-analysis. Clin Lab. (2015) 61:1101–8. doi: 10.7754/Clin.Lab.2015.150204
71. Shi H-B, Yu J-X, Yu J-X, Feng Z, Zhang C, Li G-Y, et al. Diagnostic significance of microRNAs as novel biomarkers for bladder cancer: a meta-analysis of ten articles. World J Surg Oncol. (2017) 15:1–10. doi: 10.1186/s12957-017-1201-9
72. Yun SJ, Jeong P, Kim W-T, Kim TH, Lee Y-S, Song PH, et al. Cell-free microRNAs in urine as diagnostic and prognostic biomarkers of bladder cancer. Int J Oncol. (2012) 41:1871–8. doi: 10.3892/ijo.2012.1622
73. Darling D, Luxmanan C, O'Sullivan P, Lough T, Suttie J. Clinical utility of cxbladder for the diagnosis of urothelial carcinoma. Adv Ther. (2017) 34:1087–96. doi: 10.1007/s12325-017-0518-7
74. Lotan Y, O'Sullivan P, Raman JD, Shariat SF, Kavalieris L, Frampton C, et al. Clinical comparison of noninvasive urine tests for ruling out recurrent urothelial carcinoma. Urol Oncol. (2017) 35:531.e15–e22. doi: 10.1016/j.urolonc.2017.03.008
75. Koya M, Osborne S, Chemaslé C, Porten S, Schuckman A, Kennedy-Smith A. An evaluation of the real world use and clinical utility of the cxbladder monitor assay in the follow-up of patients previously treated for bladder cancer. BMC Urol. (2020) 20:1–9. doi: 10.1186/s12894-020-0583-0
76. Lough T, Luo Q, O'Sullivan P, Chemaslé C, Stotzer M, Suttie J, et al. Clinical utility of cxbladder monitor for patients with a history of urothelial carcinoma: a physician-patient real-world clinical data analysis. Oncol Ther. (2018) 6:73–85. doi: 10.1007/s40487-018-0059-5
77. Mao L, Lee DJ, Tockman MS, Erozan YS, Askin F, Sidransky D. Microsatellite alterations as clonal markers for the detection of human cancer. Proc Nat Acad Sci. (1994) 91:9871–5. doi: 10.1073/pnas.91.21.9871
78. Orlow I, Lianes P, Lacombe L, Dalbagni G, Reuter VE, Cordon-Cardo C. Chromosome 9 allelic losses and microsatellite alterations in human bladder tumors. Cancer Res. (1994) 54:2848–51.
79. Simon R, Bürger H, Brinkschmidt C, Böcker W, Hertle L, Terpe HJ. Chromosomal aberrations associated with invasion in papillary superficial bladder cancer. J Pathol. (1998) 185:345–doi: 10.1002/(SICI)1096-9896(199808)185:4<345::AID-PATH109>3.0.CO;2-0
80. Takahashi T, Habuchi T, Kakehi Y, Mitsumori K, Akao T, Terachi T, et al. Clonal and chronological genetic analysis of multifocal cancers of the bladder and upper urinary tract. Cancer Res. (1998) 58:5835–41.
81. Seripa D, Parrella P, Gallucci M, Gravina C, Papa S, Fortunato P, et al. Sensitive detection of transitional cell carcinoma of the bladder by microsatellite analysis of cells exfoliated in urine. Int J Cancer. (2001) 95:364–9. doi: 10.1002/1097-0215(20011120)95:6<364::AID-IJC1064>3.0.CO;2-V
82. van der Aa MN, Zwarthoff EC, Steyerberg EW, Boogaard MW, Nijsen Y, van der Keur KA, et al. Microsatellite analysis of voided-urine samples for surveillance of low-grade non-muscle-invasive urothelial carcinoma: feasibility and clinical utility in a prospective multicenter study (Cost-Effectiveness of Follow-Up of Urinary Bladder Cancer trial [CEFUB]). Eur Urol. (2009) 55:659–68. doi: 10.1016/j.eururo.2008.05.001
83. Frigerio S, Padberg BC, Strebel RT, Lenggenhager DM, Messthaler A, Abdou M-T, et al. Improved detection of bladder carcinoma cells in voided urine by standardized microsatellite analysis. Int J Cancer. (2007) 121:329–38. doi: 10.1002/ijc.22690
84. Beckham CJ, Olsen J, Yin PN, Wu CH, Ting HJ, Hagen FK, et al. Bladder cancer exosomes contain EDIL-3/Del1 and facilitate cancer progression. J Urol. (2014) 192:583–92. doi: 10.1016/j.juro.2014.02.035
85. Liang L-G, Kong M-Q, Zhou S, Sheng Y-F, Wang P, Yu T, et al. An integrated double-filtration microfluidic device for isolation, enrichment and quantification of urinary extracellular vesicles for detection of bladder cancer. Sci Rep. (2017) 7:1–10. doi: 10.1038/srep46224
86. Lin S-Y, Chang C-H, Wu H-C, Lin C-C, Chang K-P, Yang C-R, et al. Proteome profiling of urinary exosomes identifies alpha 1-antitrypsin and H2B1K as diagnostic and prognostic biomarkers for urothelial carcinoma. Sci Rep. (2016) 6:1–12. doi: 10.1038/srep34446
87. Andreu Z, Oshiro RO, Redruello A, López-Martín S, Gutiérrez-Vázquez C, Morato E, et al. Extracellular vesicles as a source for non-invasive biomarkers in bladder cancer progression. Eur J Pharm Sci. (2017) 98:70–9. doi: 10.1016/j.ejps.2016.10.008
Keywords: biomarker, bladder cancer, surveillance, non-muscular invasive bladder cancer, cancer screening
Citation: Sugeeta SS, Sharma A, Ng K, Nayak A and Vasdev N (2021) Biomarkers in Bladder Cancer Surveillance. Front. Surg. 8:735868. doi: 10.3389/fsurg.2021.735868
Received: 03 July 2021; Accepted: 25 August 2021;
Published: 28 September 2021.
Edited by:
Daniele Castellani, Polytechnic University of Le Marche, ItalyReviewed by:
Bryan Kwun-Chung Cheng, United Christian Hospital, Hong Kong SAR, ChinaPeter Ka-Fung Chiu, The Chinese University of Hong Kong, China
Bogdan Geavlete, St. John Hospital Emergency Clinic, Romania
Copyright © 2021 Sugeeta, Sharma, Ng, Nayak and Vasdev. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nikhil Vasdev, nikhil.vasdev@nhs.net
 Sukumar S. Sugeeta
Sukumar S. Sugeeta Anand Sharma
Anand Sharma Kenrick Ng
Kenrick Ng Arvind Nayak2
Arvind Nayak2  Nikhil Vasdev
Nikhil Vasdev