Cross-Sectional Analysis of Oral Healthcare vs. General Healthcare Utilization in Five Low- and Middle-Income Countries
- School of Public Health, University of California, Berkeley, Berkeley, CA, United States
Oral health is integral to overall health and is often neglected, especially in low- and middle-income countries (LMICs). Oral disease, including untreated dental caries, affects nearly 3.5 billion people globally, contributing to poor health and quality of life. To examine the relationship between the utilization of general healthcare and oral healthcare, we conducted an exploratory cross-sectional study of first-visit interview data collected from a convenience sample of 3,422 low-income mothers and 4,324 children aged 6 months through 6 years participating in a community-based oral health and nutrition program in five LMICs (Ecuador, El Salvador, India, Nepal, and Vietnam) from 2006–2015. We used descriptive and exploratory association analysis to identify patterns of oral healthcare utilization for mothers and children compared to medical care utilization, specifically maternal prenatal care and child immunizations. Overall, 89.6% of the mothers had received prenatal care for at least one child, but only 76.4% had ever received dental care and 50% were currently suffering from oral health symptoms, primarily oral pain. Mothers who received prenatal care were significantly more likely to have accessed dental care compared to those who had not received prenatal care (OR = 2.62, 95% CI: 2.06, 3.32). Overall, 95.4% of the children had current immunizations, but only 30.1% had ever received dental care, and 32.4% were currently suffering from oral pain. Children whose immunizations were up-to-date were more likely to have received dental care, with a significant association in Ecuador (OR = 3.29, 95% CI: 2.06, 5.30). Compared to utilization of general healthcare, oral healthcare was under-utilized by mothers and children in our sample from five LMICs. Integration of prevention- and treatment-oriented oral healthcare into primary medical care services, particularly prenatal care and child immunizations, could help increase access to oral healthcare and improve women's and children's oral health.
Introduction
Oral health is intimately linked with general health and has physiological, psychological, and social ramifications that affect well-being [1]. Oral disease, which includes dental caries and periodontal disease, affects nearly 3.5 billion people globally, making it the most prevalent non-communicable disease (NCD) [2]. Dental caries is the most common chronic childhood disease, affecting between 60 and 90% of children worldwide, and untreated dental caries in permanent teeth affects 35% of the global population [3]. Oral health also has a bidirectional relationship with other NCDs [4], such as cardiovascular disease and diabetes, through complex physiological interactions as well as shared risk factors such as tobacco use and high sugar consumption [5–8]. Nevertheless, oral health is often neglected, and oral healthcare is accessed differently from general healthcare, particularly in low- and middle-income countries (LMICs). In many LMICs, most carious lesions remain untreated due to inappropriate, unaffordable or unavailable oral healthcare services, contributing to poor overall health and quality of life [9].
Despite the fact that dental caries and periodontal disease are largely preventable, improvements in oral health and oral healthcare access have remained challenging, especially in LMICs [10–13]. Oral healthcare access ranges from 35% in low-income countries to 75% in upper-middle income countries [14]. Low oral healthcare access is driven in part by the routine omission of oral healthcare from Universal Health Coverage [15], as well as the biomedical model of dentistry that incentivizes treatment-oriented oral healthcare, including fillings, crowns, and extractions, over prevention-oriented oral healthcare such as routine checkups, cleanings, application of fluoride varnish, and oral hygiene instruction [16, 17]. This traditional model perpetuates the demand for highly-skilled dentists; however, in many LMICs, insufficient resources have been allotted to cultivate a prevention-oriented oral healthcare workforce and approach [10, 18]. Finally, the rise in the overconsumption of sugary food products, specifically sugar-sweetened beverages, has exacerbated oral disease and has contributed greatly to the lack of improvement in global oral health [19, 20].
In contrast, numerous improvements have been made in maternal and child health in recent decades. The estimated worldwide coverage of early prenatal care visits increased by 43.3%, from 40.9% in 1990 to 58.6% in 2013 [21]. According to UNICEF, global data show that 87% of pregnant women access prenatal care at least once during their pregnancy, and 59% receive four or more prenatal care visits [22]. Similarly, progress has been made in immunization coverage throughout the world since the establishment of the Expanded Programme on Immunization by the World Health Organization (WHO) in 1974. According to the WHO, despite disruption caused by the COVID-19 pandemic, 83% of infants worldwide received three doses of diphtheria-tetanus-pertussis vaccine in 2020 [23]. Altogether, these developments have improved accessibility to preventive medical care for mothers and children globally.
The rising prevalence of NCDs in LMICs, including oral disease, threatens the sustainability of Universal Health Coverage [24, 25]. Furthermore, the COVID-19 pandemic has highlighted the increasing need to maintain proper oral health and oral hygiene, such as regular dental visits, as poor oral health has been shown to exacerbate the severity of COVID-19 significantly [26]. Nevertheless, the consensus that oral health is integral to general health has not translated to widespread integration of these two health care domains. Understanding the relationship between the utilization of general preventive healthcare services and dental care, including both treatment- and prevention-oriented oral healthcare services, may illuminate opportunities to expand delivery of oral healthcare and improve overall population health. This cross-sectional study explores dental care and general preventive healthcare utilization in five LMICs (Ecuador, El Salvador, India, Nepal, and Vietnam) and identifies correlations between maternal prenatal care and child immunization access, and dental care utilization.
Materials and Methods
Ethical Approval
This family of studies on children's oral health was developed and conducted as a collaboration among University of California Berkeley with local country Ministries of Health, academic institutions, and non-governmental non-profit organizations. All study sites and protocols were approved by the Committee for the Protection of Human Subjects, the Institutional Review Board (IRB) at the University of California, Berkeley (#2010-06-1655, #2011-04-3176, #2011-04-3178, and #2012-11-4798). Additional approval was obtained, when required, by IRB reliance from the University of California, San Francisco, local ministries of health (El Salvador, Ecuador), health research council (Nepal), university (Vietnam), and non-profit organization directors (El Salvador, Ecuador, Vietnam, Nepal, and India).
Study Design and Population
This is a cross-sectional descriptive study of a convenience sample of 3,422 low-income mothers and 4,324 children aged 6 months through 6 years who participated in a community-based program promoting child nutrition and oral health in two LMICs in Latin America (Ecuador and El Salvador) and three LMICs in Asia (India, Nepal, and Vietnam). The communities were rural (Ecuador, El Salvador, Nepal), urban (India, Nepal, Vietnam), and peri-urban (Vietnam). The local partner organizations identified study communities where they worked, and all mothers and children in the study age group were invited to participate. This paper presents data collected from 2006–2015: Ecuador from 2010–2013, El Salvador from 2006–2010 and 2014, Nepal and Vietnam from 2011–2013, and India from 2012–2015. For this analysis, we included only the first visits of mothers with the children present on that first visit. We excluded data from caregivers who were not the mothers of the children, and children outside the age range criteria to focus on the ages when primary teeth comprise the majority of a child's dentition [27].
Data Collection
In each site, trained local health workers provided mothers with a verbal explanation of the study in their native language, and obtained written/verbal informed consent for the mother's and child's participation. The consent forms and the surveys were validated through forward and back translation and pilot samples to confirm understanding of the questionnaire. Results using the questionnaires have been previously published [13, 28–31]. The survey was modified from the WHO oral health survey [32] and consisted of 49 questions: 20 questions regarding maternal background, nutrition and oral health history and habits, access to general healthcare and oral healthcare, and knowledge and beliefs about oral health and disease; and 29 questions about each child's nutrition and oral health history and habits, access to general healthcare and oral healthcare, and oral health status. In El Salvador, Ecuador, Nepal and India, trained volunteers and community health workers fluent in the local/native languages interviewed the mothers and completed both sections of the survey; and in Vietnam, the partner organization requested that the survey be completed directly by mothers since their education and literacy levels were high. Responses were recorded on paper forms before being entered into an Excel spreadsheet or immediately entered on computer tablets into a Qualtrics database.
Statistical Analysis
The entered data were cleaned and analyzed via RStudio (version 4.0.3, RStudio PBC, Boston, MA, USA) and Microsoft Excel (version 2201, Microsoft Corporation, Albuquerque, NM, USA). Missing data that could not be imputed were ignored in the final analysis. In our univariate analysis, we first calculated descriptive statistics such as averages, percentages, and ratios to identify patterns of oral healthcare utilization compared to medical care utilization among mothers and children. We then used Fisher's Exact Test, a procedure used for small sample sizes with one or more cells less than an expected value of 5, to calculate odds ratios and 95% confidence intervals to further estimate the effect size and confirm the directionality of the relationship between the utilization of any kind of dental care and preventive medical care, specifically maternal prenatal care and child immunizations. Where appropriate, we used the delta method to calculate the 95% confidence intervals for the ratios. Statistical significance was considered for p-values < 0.05.
Results
Mother and Child Demographic Characteristics
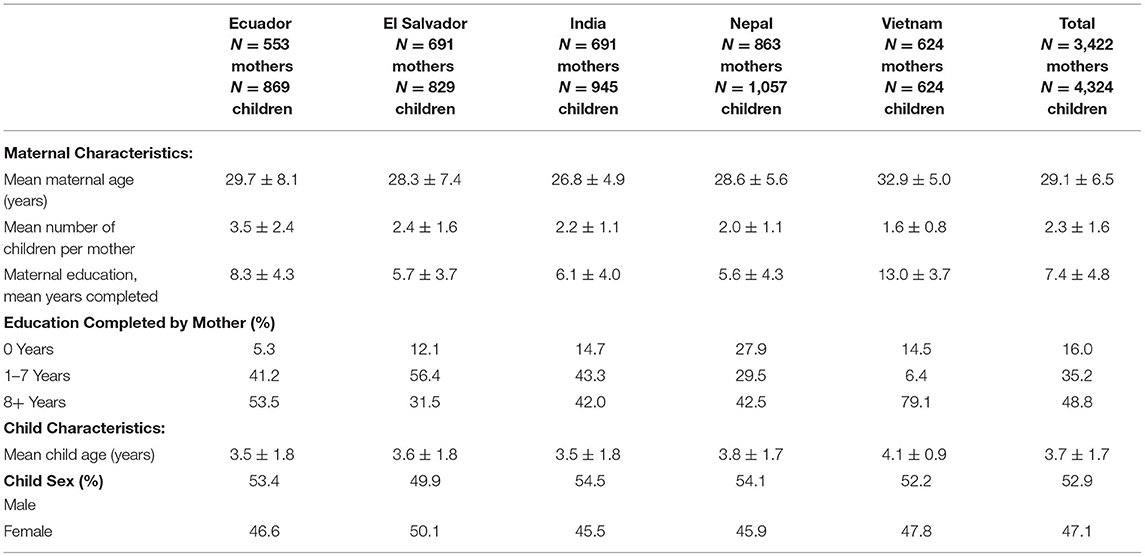
A total of 3,422 mothers and 4,324 children aged 6 months through 6 years were studied. Across all five countries, the mothers had a mean age of 29 years and had 2.3 children. Overall, mothers obtained roughly 7 years of education, and half of mothers (48.8%) had 8 years of schooling or more, one-third (35.2%) had some primary school level of education, and 1 in 6 (16.0%) had no formal education. The children had a mean age of 3.7 years, and a slightly greater proportion were male (52.9%) than female (47.1%) (Table 1).
Mothers' Access/Utilization of Dental Care vs. General Healthcare
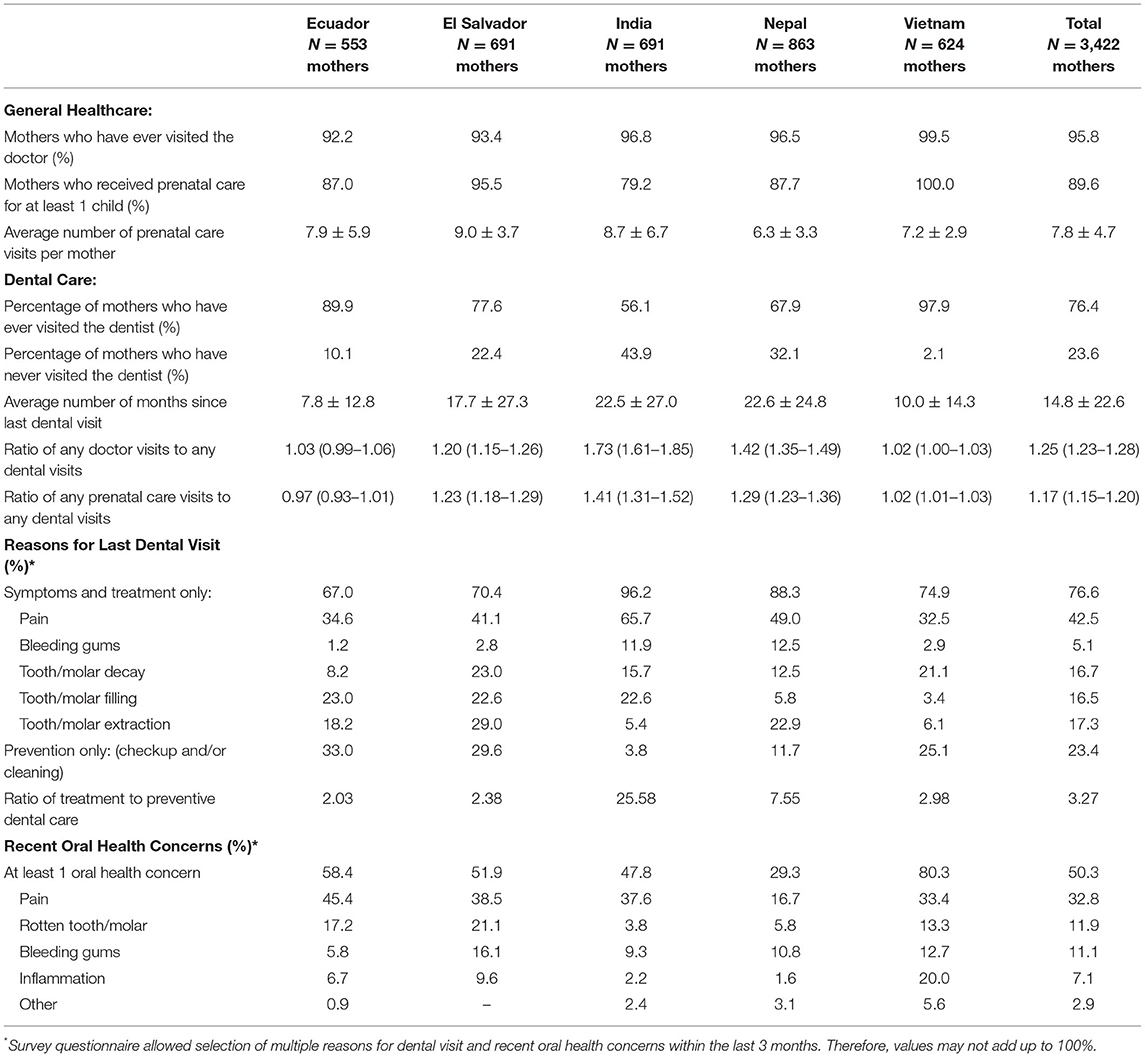
Across all five countries, nearly all mothers (95.8%) reported ever visiting the doctor (Table 2). Moreover, 9 out of 10 mothers (89.6%) had received prenatal care for at least one child present with her at the time of the interview, ranging from 79% in the India sample to 100% in the Vietnam sample. Overall, mothers reported an average of 7.8 prenatal care visits, ranging from roughly 6 in the Nepal sample to 9 in the El Salvador sample.
Overall, only three-quarters of mothers (76.4%) reported receiving any kind of dental care, with the lowest utilization (56.1%) occurring in the India sample. Across all five countries, mothers were 1.3 times (or 25%) more likely to have gone to a doctor for any reason than to have received any kind of dental care (95% CI: 1.23, 1.28), and 1.2 times (or 17%) more likely to have received prenatal care than to have received any kind of dental care (95% CI: 1.15, 1.20). The average time since the last dental care visit of any kind was 14.8 months, ranging from 7.8 months in the Ecuador sample to 23 months in the India and Nepal samples. Overall, dental visits that were driven by oral symptoms or were treatment-oriented were 3 times more common than those that were exclusively prevention-oriented, and the difference ranged from 2- to 3-fold in the Ecuador, El Salvador and Vietnam samples to 8-fold in the Nepal sample and 26-fold in the India sample. Overall, and in each country, dental pain was the most common symptom cited as motivating the last dental visit.
Half of mothers overall (50.3%) reported experiencing recent dental symptoms, ranging from 29% in the Nepal sample to 80% in the Vietnam sample. Dental pain was the most common symptom, reported by one-third (32.8%) of all mothers, ranging from 17% in the Nepal sample to 45% in the Ecuador sample.
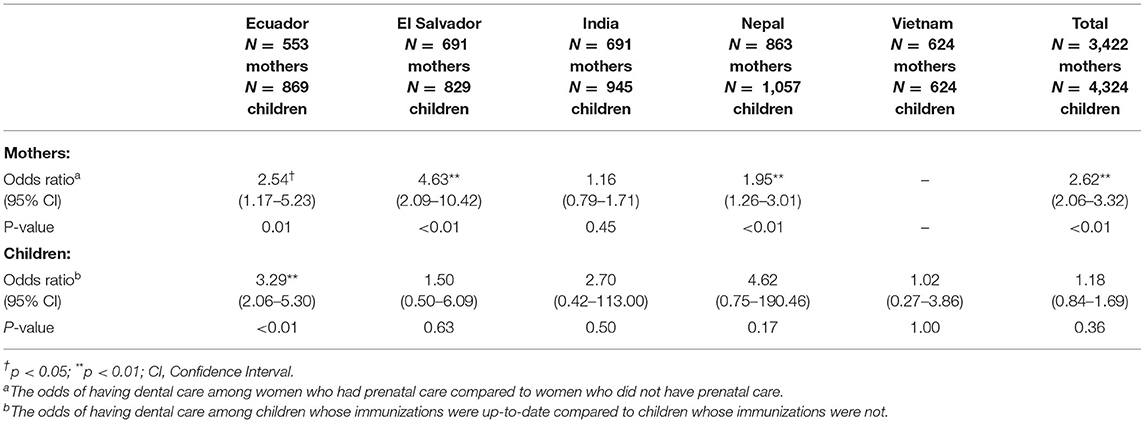
Receiving prenatal care was significantly associated with the utilization of any kind of dental care services (OR = 2.62; 95% CI: 2.06, 3.32). This association was statistically significant in all countries except India (OR = 1.16; 95% CI: 0.79, 1.71) and Vietnam (for which the OR could not be calculated since 100% of mothers reported receiving prenatal care for at least one child) (Table 4).
Children's Access/Utilization of Dental Care vs. General Healthcare
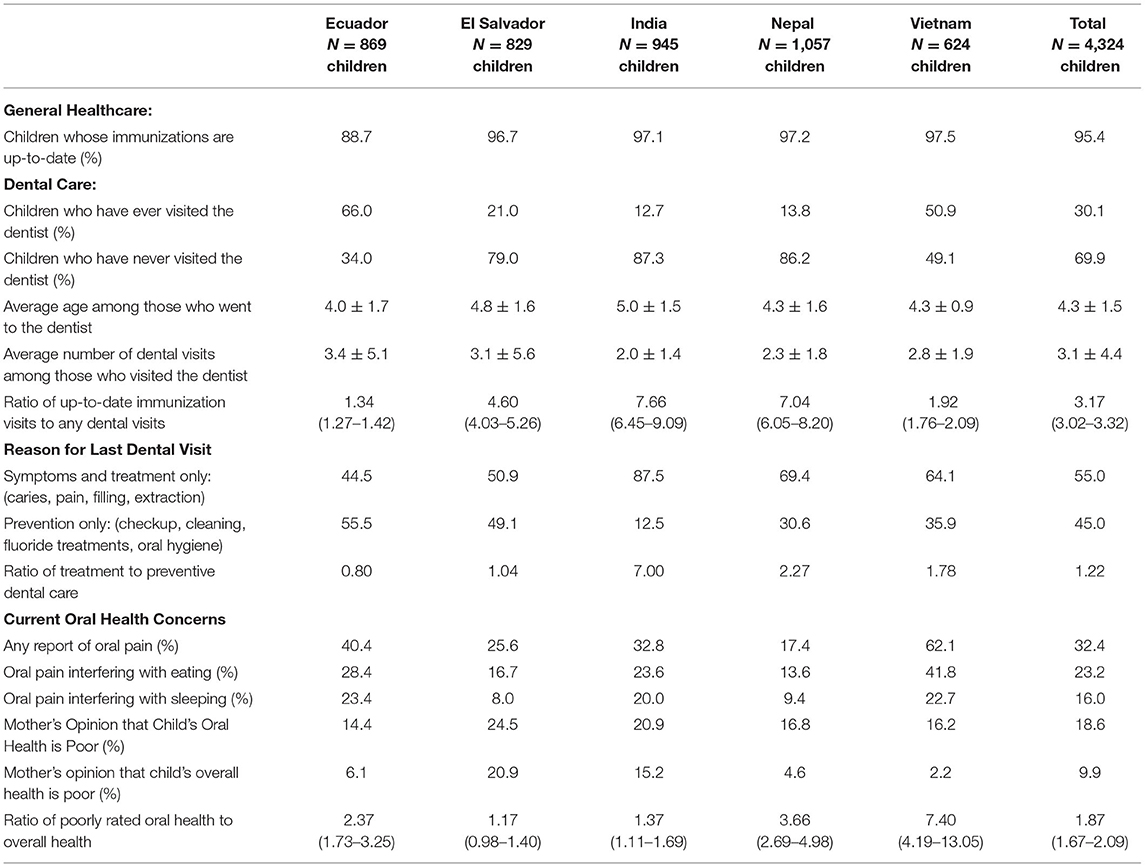
Across all five countries, nearly all children (95.4%) were reported to have up-to-date immunizations (Table 3). However, less than a third of children (30.1%) had ever visited a dentist. The average age of the children who had visited the dentist was 4.3 years and these children averaged 3 dental visits. Across all countries, 70% of children had never received any kind of dental care, ranging from 34% in the Ecuador sample to 86-87% in the Nepal and India samples. Across all five countries, children were over 3 times more likely to have been up-to-date with their immunizations than to have received any kind of dental care (95% CI: 3.02, 3.32), and the difference ranged up to 7- to 8-fold in the Nepal and India samples.
Overall, of the 30.1% of children who had ever visited a dentist, over half (55%) of the visits were driven by oral symptoms or were treatment-oriented whether in conjunction with a prevention-oriented service or not, while less than half (45%) of visits consisted exclusively of prevention-oriented services such as checkups, cleanings, application of fluoride treatments, and oral hygiene education. Treatment-oriented dental visits were 1.2-times more common than those that were exclusively prevention-oriented, and the difference ranged up to 7-fold in the India sample. Overall, one-third (32.4%) of children were reported to currently complain of oral pain, ranging from 17% in the Nepal sample to 62% in the Vietnam sample. Furthermore, 1 in 4 children (23.2%) were reported to have oral pain that interfered with eating, and 1 in 6 children (16%) to have oral pain that interfered with sleeping.
Mothers consistently rated their child's oral health as inferior to their child's overall health. Collectively, a designation of “poor oral health” was nearly twice as common as that of “poor overall health,” with differences ranging to nearly 4-fold in the Nepal sample to over 7-fold in the Vietnam sample.
Being current with immunizations was significantly associated with utilization of any kind of dental care services only in Ecuador (OR = 3.29; 95% CI: 2.06, 5.30). This association was not significant overall, likely due to the low proportion of children who had ever seen a dentist (OR = 1.18; 95% CI: 0.84, 1.69) (Table 4).
Discussion
This cross-sectional study of a convenience sample of mothers and children from five LMICs (Ecuador, El Salvador, India, Nepal, and Vietnam) described the disparity between maternal-child utilization of general healthcare and dental care services, and explored the relationship between access to preventive medical care and dental care. Mothers, and especially children, had greater utilization of preventive medical care services than dental care services of any kind, including both treatment- and prevention-oriented services, and mothers and children who accessed preventive medical care services had a greater likelihood of utilizing any kind of dental care services.
Mothers primarily sought dental care services for themselves and their children to treat oral pain, commonly from severely-decayed teeth. Collectively, one-third of the mothers had experienced oral pain within the last 3 months and one-third of the children were experiencing oral pain at the time of the interview. Because dental care is often utilized only when symptoms arise, treatment is frequently limited to emergency care such as dental extraction, a common practice in many LMICs [33–35]. Antibiotics are also commonly given to treat abscesses, which can contribute to the proliferation of antibiotic-resistant bacterial strains [36], and analgesics including opioids are commonly given to treat pain, which can contribute to opioid addiction and overdoses [37]. Furthermore, temporary palliative dental treatment, as opposed to definitive care, contributes to the persistence of chronic dental symptoms [38–40]. This misutilization of oral healthcare has been attributed in part to prohibitive costs of care, prompting the need to restructure the traditional model of dentistry and the delivery of oral healthcare services [15, 41, 42].
Few studies have specifically compared the utilization of prenatal care services to the utilization of dental care services. Our exploratory study estimated that mothers were 1.2 times more likely to have ever received prenatal care compared to any kind of dental care (including both treatment-oriented and exclusively prevention-oriented visits). This estimate is consistent with other studies in Sudan and the Solomon Islands which found greater odds of utilization of dental care services given participation in preventive measures such as health screenings [43, 44]. Our study also estimated that children were over 3 times more likely to be up-to-date with immunizations than to have received any kind of dental care. Previous studies by Chi et al. and Tiwari et al. showed that children who received well-child checkups were more likely to access preventive dental care, and that a greater number of well-child checkups was associated with earlier preventive dental care visits among children [45, 46].
A growing body of evidence demonstrates that increasing the accessibility and utilization of oral healthcare for pregnant women and children improves oral health outcomes for both. Studies in Saudi Arabia found that women who visited the dentist regularly had increased oral health knowledge about methods to prevent caries in children [47, 48]. A 2-year randomized controlled trial that examined the impact of an oral health promotion program among Australian Aboriginal pregnant women and their children found that children in the intervention group had a lower incidence of caries at 2 years compared to those in the control [49], and a recent meta-analysis found that children whose mothers received prenatal oral healthcare had a reduced incidence of early childhood caries up to age 4 [50].
The relationships found in our study between the utilization of preventive medical care and any kind of dental care among mothers and children advance the argument for integration of oral healthcare services within the existing primary healthcare infrastructure, particularly in LMICs. This would enable the transition of the oral healthcare model from one that is emergency-oriented and palliative to one that is truly preventive. Prevention-oriented oral healthcare services that could be delivered within the existing primary healthcare infrastructure and entail minimal training to providers include oral health education with dietary counseling, application of fluoride varnish, oral hygiene instruction, and dispensing of low-cost fluoride toothpaste and toothbrushes. Preventive services such as teeth cleanings and sealants could also be delivered within the primary healthcare infrastructure, but require more training and necessitate an expansion of the oral healthcare workforce. Treatment-oriented services may also be provided within the existing primary healthcare infrastructure. The application of silver diamine fluoride is one therapeutic service that requires few dental tools. Atraumatic restorative technique restorations require more dental equipment, but with proper training could be delivered by mid-level oral healthcare providers. More complicated cases would be referred to dentists and other oral healthcare specialists.
The concept of integration is not new. Since 2002, the WHO's Basic Package of Oral Care (BPOC) has been the framework recommended for integration within primary healthcare and includes urgent oral treatment, atraumatic restorative treatment, and affordable fluoride toothpaste [51]. Nevertheless, for some of the aforementioned reasons, there has been very little improvement in global oral health. In 2021, the WHO renewed its commitment to advancing BPOC [52], and over the past year has been developing a set of oral health strategies to address the remaining challenges. The strategies include integration of oral health as part of Universal Health Coverage agendas, promotion of oral health and prevention of oral disease from individual education to national policies, and development of an oral healthcare workforce that includes mid-level oral healthcare providers, community health workers as well as primary care physicians and nurses [53].
Our study has identified specific opportunities for integration between preventive medical care and oral healthcare, including both prevention- and treatment-oriented services. Our finding that 90% of mothers had received prenatal care with approximately 8 prenatal care visits provides ample opportunities for integration. Similarly, our finding that 95% of children were up-to-date with their immunizations, which entails multiple visits from infancy through preschool-age [54], allows abundant opportunities for integrative services. This would vastly improve oral healthcare access for the 70% of young children in our sample who had never received any kind of dental care. One such case of this integration is the Cambodia Smile program, where trained non-dental primary healthcare workers in immunization clinics provided oral health education and fluoride varnish applications. They found that children in the intervention were 6 times less likely to experience early childhood caries at the age of 2, families experienced improved oral health-related quality of life compared to the control group, and health workers and families found the intervention highly acceptable [55].
This study contributes to the literature by identifying maternal-child oral health concerns and suggesting a specific pathway to improve access to prevention- and treatment-oriented oral healthcare. While our study did not set out to compare differences among countries, the geographically diverse nature of our sample is a notable strength in bringing this global issue to light. The method of convenience sampling was both a strength as it allowed for the inclusion of geographically diverse communities and a study limitation as it can result in selection bias and restrict the generalizability of the findings. Other limitations include survey responses having been affected by recall bias, as mothers were asked about past visits, and information bias if mothers selected answers that they felt the interviewer wanted to hear. As a community-based study, there was inevitably clustering at the community level, for which this exploratory analysis did not account. Finally, given the cross-sectional study design, temporality between preventive medical care and dental care cannot be established. Further research is needed to confirm these findings and test the recommended interventions in a wide range of LMIC settings.
Conclusion
This study identifies opportunities for integration of oral healthcare services into the existing primary healthcare infrastructure. While prenatal care and child immunization services are widely accessible, general dental care is under-utilized, and a large proportion of mothers and young children are suffering from untreated oral disease and pain. Access to prevention- and treatment-oriented oral healthcare services could be vastly improved by integration into primary healthcare settings, particularly prenatal care and child immunizations services.
Data Availability Statement
The original datasets analyzed in this study are not publicly available in accordance with participant privacy, informed consent forms that did not include release of the data, and the study's approved IRB protocols. However, the minimal dataset necessary to interpret, replicate and build upon the findings of this study are available from the senior author [KS-G] upon reasonable request.
Author Contributions
KS-G: conceptualization and data curation. SS and MT: formal statistical analysis. MT: writing—original draft. SS and KS-G: writing—review and editing. SS: visualization and preparation of tables. All authors made significant contribution to the conception or design of the work or to the acquisition, analysis, or interpretation of data. All authors contributed to the article and approved the submitted version.
Funding
There was no funding for this analysis. Funding for the collection of the original data used in this analysis was supported by small grants from UC Berkeley Professional Development Fund, UC Berkeley Center for Health Research, UC Berkeley Health Research for Action, UC Berkeley Blum Center Big Ideas Fund, UC Berkeley Undergraduate Research Apprenticeship Program, American Academy of Pediatrics I-CATCH, Global Healing, America Nepal Medical Foundation, Jewish Women's Foundation of New York, and donations to the Children's Oral Health and Nutrition Project charitable fund at UC Berkeley. Support for open-access publication fees was provided by the Berkeley Research Impact Initiative (BRII) at the UC Berkeley Library.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to express our sincere gratitude to the funders of the original research study, the dedicated leadership and staff of our partner organizations, the generosity of hundreds of local-country and student volunteers, the invaluable guidance of local-country and international dental professionals, and the patience and openness of the thousands of study participants who endured the time-consuming study procedures and shared their personal experiences with the hope of improving the health of their families and communities.
References
1. Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, Weyant RJ, et al. New definition for oral health developed by the FDI world dental federation opens the door to a universal definition of oral health. J Am Dent Assoc. (1939) 147:915–7. doi: 10.1016/j.adaj.2016.10.001
2. GBD Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1789–858. doi: 10.1016/S0140-6736(18)32279-7
3. Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. Global burden of untreated caries: a systematic review and metaregression. J Dent Res. (2015) 94:650–8. doi: 10.1177/0022034515573272
4. Croser D. Oral health waits another seven UN years. Br Dent J. (2018) 225:927–9. doi: 10.1038/sj.bdj.2018.1021
5. Sheiham A, Watt RG. The common risk factor approach: a rational basis for promoting oral health. Community Dent Oral Epidemiol. (2000) 28:399–406. doi: 10.1034/j.1600-0528.2000.028006399.x
6. Taylor JJ, Preshaw PM, Lalla E. A review of the evidence for pathogenic mechanisms that may link periodontitis and diabetes. J Clin Periodontol. (2013) 40:S113–34. doi: 10.1111/jcpe.12059
7. Wojtkowska A, Zapolski T, Wysokińska-Miszczuk J, Wysokiński AP. The inflammation link between periodontal disease and coronary atherosclerosis in patients with acute coronary syndromes: case-control study. BMC Oral Health. (2021) 21:5. doi: 10.1186/s12903-020-01356-4
8. Pitts NB, Twetman S, Fisher J, Marsh PD. Understanding dental caries as a non-communicable disease. Br Dent J. (2021) 231:749–53. doi: 10.1038/s41415-021-3775-4
9. FDI World Dental Federation. Oral health worldwide. (2015). Available online at: https://www.fdiworlddental.org/sites/default/files/2020-11/2015_wohd-whitepaper-oral_health_worldwide.pdf (accessed November 26,2021).
10. Kassebaum NJ, Smith A, Bernabé E, Fleming TD, Reynolds AE, Vos T, et al. Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990-2015: a systematic analysis for the global burden of diseases, injuries, and risk factors. J Dent Res. (2017) 96:380–7. doi: 10.1177/0022034517693566
11. Peres MA, Macpherson L, Weyant RJ, Daly B, Venturelli R, Mathur MR, et al. Oral diseases: a global public health challenge. Lancet. (2019) 394:249–60. doi: 10.1016/S0140-6736(19)31146-8
12. Riggs E, Kilpatrick N, Slack-Smith L, Chadwick B, Yelland J, Muthu MS, et al. Interventions with pregnant women, new mothers and other primary caregivers for preventing early childhood caries. Cochrane Database Syst Rev. (2019) 2019:CD012155. doi: 10.1002/14651858.CD012155.pub2
13. Huang D, Sokal-Gutierrez K, Chung K, Lin W, Khanh LN, Chung R, et al. Maternal and child nutrition and oral health in urban Vietnam. Int J Environ Res Public Health. (2019) 16:2579. doi: 10.3390/ijerph16142579
14. Hosseinpoor AR, Itani L, Petersen PE. Socio-economic inequality in oral healthcare coverage: results from the world health survey. J Dent Res. (2012) 91:275–81. doi: 10.1177/0022034511432341
15. Wang TT, Mathur MR, Schmidt H. Universal health coverage, oral health, equity and personal responsibility. Bull World Health Organ. (2020) 98:719–21. doi: 10.2471/BLT.19.247288
16. Grytten J. Payment systems and incentives in dentistry. Community Dent Oral Epidemiol. (2017) 45:1–11. doi: 10.1111/cdoe.12267
17. Watt RG, Daly B, Allison P, Macpherson L, Venturelli R, Listl S, et al. (2019). Ending the neglect of global oral health: time for radical actionLancet. (2019) 394:261–72. doi: 10.1016/S0140-6736(19)31133-X
18. Bastani P, Mohammadpour M, Mehraliain G, Delavari S, Edirippulige S. What makes inequality in the area of dental and oral health in developing countries? A scoping review. Cost Eff Resour Alloc. (2021) 19:54. doi: 10.1186/s12962-021-00309-0
19. Kearney J. Food consumption trends and drivers. Philos Trans R Soc Lond B, Biol Sci. (2010) 365:2793–807. doi: 10.1098/rstb.2010.0149
20. Popkin BM, Hawkes C. Sweetening of the global diet, particularly beverages: patterns, trends, and policy responses. Lancet Diabetes Endocrinol. (2016) 4:174–86. doi: 10.1016/S2213-8587(15)00419-2
21. Moller AB, Petzold M, Chou D, Say L. Early antenatal care visit: a systematic analysis of regional and global levels and trends of coverage from 1990 to 2013. Lancet Glob Health. (2017) 5:e977–83. doi: 10.1016/S2214-109X(17)30325-X
22. UNICEF. Antenatal Care. (2021) Available online at: https://data.unicef.org/topic/maternal-health/antenatal-care/ (accessed May 22, 2022).
23. World Health Organization. Immunization Coverage. (2021). Available online at: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage (accessed May 22, 2022).
24. Beran D, Pedersen HB, Robertson J. Noncommunicable diseases, access to essential medicines and universal health coverage. Glob Health Action. (2019) 12:1670014. doi: 10.1080/16549716.2019.1670014
25. Singh Thakur J, Nangia R, Singh S. Progress and challenges in achieving noncommunicable diseases targets for the sustainable development goals. FASEB BioAdvances. (2021) 3:563–8. doi: 10.1096/fba.2020-00117
26. Glenn Katie. Poor Oral Health May Impact COVID-19 Severity, Especially for Cardiac Patients. (2021). Available online at: https://www.acc.org/about-acc/press-releases/2021/10/07/12/57/poor-oral-health-may-impact-covid-19-severity-especially-for-cardiac-patients (accessed February 6, 2022).
27. ADA Division of Communications Journal Journal of the American Dental Association ADA ADA Council on Scientific Affairs. For the dental patient. Tooth eruption: the primary teeth. J Am Dent Assoc. (2005) 136:1619. doi: 10.14219/jada.archive.2005.0095
28. So M, Ellenikiotis YA, Husby HM, Paz CL, Seymour B, Sokal-Gutierrez K. Early childhood dental caries, mouth pain, and malnutrition in the ecuadorian amazon region. Int J Environ Res Public Health. (2017) 14:550. doi: 10.3390/ijerph14050550
29. Dabiri D, Fontana M, Kapila Y, Eckert G, Sokal-Gutierrez K. Community-based assessment and intervention for early childhood caries in rural El Salvador. Int Dent J. (2016) 66:221–8. doi: 10.1111/idj.12228
30. Athavale P, Khadka N, Roy S, Mukherjee P, Chandra Mohan D, Turton BB, et al. Early childhood junk food consumption, severe dental caries, and undernutrition: a mixed-methods study from Mumbai, India. Int J Environ Res Public Health. (2020) 17:8629. doi: 10.3390/ijerph17228629
31. Tsang C, Sokal-Gutierrez K, Patel P, Lewis B, Huang D, Ronsin K. et al. Early childhood oral health and nutrition in urban and rural Nepal. Int J Environ Res Public Health. (2019) 16:2456. doi: 10.3390/ijerph16142456
32. World Health Organization. Oral Health Surveys: Basic Methods, 5th Edition. (2013). Available online at: https://www.who.int/publications/i/item/9789241548649
33. Kandelman D, Arpin S, Baez RJ, Baehni PC, Petersen PE. Oral health care systems in developing and developed countries. Periodontology. (2000) 60:98–109. doi: 10.1111/j.1600-0757.2011.00427.x
34. Tepe JH, Tepe LJ. A model for mission dentistry in a developing country. Front Public Health. (2017) 5:119. doi: 10.3389/fpubh.2017.00119
35. Curtis DC, Ortega F, Monar J, Bay R C, Eckhart S, Thompson P. Assessing self-reported oral health status of three Andean indigenous communities in Ecuador. J Int Oral Health. (2017) 9:207–12. doi: 10.4103/jioh.jioh_164_17
36. Haque M, Sartelli M, Haque SZ. Dental infection and resistance-global health consequences. Dent J. (2019) 7:22. doi: 10.3390/dj7010022
37. Dana R, Azarpazhooh A, Laghapour N, Suda KJ, Okunseri C. Role of dentists in prescribing opioid analgesics and antibiotics: an overview. Dent Clin North Am. (2018) 62:279–94. doi: 10.1016/j.cden.2017.11.007
38. Sun BC, Chi DL, Schwarz E, Milgrom P, Yagapen A, Malveau S, et al. Emergency department visits for nontraumatic dental problems: a mixed-methods study. Am J Public Health. (2015) 105:947–55. doi: 10.2105/AJPH.2014.302398
39. Timmerman A, Parashos P. Management of dental pain in primary care. Aust Prescr. (2020) 43:39–44. doi: 10.18773/austprescr.2020.010
40. Keels MA, Vo A, Casamassimo PS, Litch CS, Wright R. Denial of Access to Operating Room Time in Hospitals for Pediatric Dental Care. (2021). Available online at: https://www.aapd.org/globalassets/media/advocacy/ord.pdf (Accessed March 19, 2022).
41. Bernabé E, Masood M, Vujicic M. The impact of out-of-pocket payments for dental care on household finances in low and middle income countries. BMC Public Health. (2017) 17:109. doi: 10.1186/s12889-017-4042-0
42. Chen J, Duangthip D, Gao SS, Huang F, Anthonappa R, Oliveira BH, et al. Oral health policies to tackle the burden of early childhood caries: a review of 14 countries/regions. Front Oral Health. (2021) 2:670154. doi: 10.3389/froh.2021.670154
43. Pengpid S, Peltzer K. Prevalence and correlates of dental service utilisation among a national general adult population sample in Sudan. BMC Oral Health. (2021) 21:61. doi: 10.1186/s12903-021-01422-5
44. Pengpid S, Peltzer K. Prevalence and correlates of dental service utilization among adults in Solomon Islands. J Int Soc Prev Community Dent. (2021) 11:166–72. doi: 10.4103/jispcd.JISPCD_400_20
45. Chi DL, Momany ET, Jones MP, Kuthy RA, Askelson NM, Wehby GL, et al. Relationship between medical well baby visits and first dental examinations for young children in Medicaid. Am J Public Health. (2013) 103:347–54. doi: 10.2105/AJPH.2012.300899
46. Tiwari T, Rai N, Brow A, Tranby EP, Boynes SG. Association between medical well-child visits and dental preventive visits: a big data report. JDR Clin Trans Res. (2019) 4:239–45. doi: 10.1177/2380084419841850
47. Gaffar BO, El Tantawi M, Al-Ansari A, AlAgl AS. Association between oral health knowledge and practices of Saudi pregnant women in Dammam, Saudi Arabia. East Mediterr Health J. (2016) 22:411–6. doi: 10.26719/2016.22.6.411
48. Albasry Z, Alhaddad B, Benrashed MA, Al-Ansari A, Nazir MA. A cross-sectional analysis of dental care utilization among pregnant women in Saudi Arabia. Open Access Maced J Med Sci. (2019) 7:4131–6. doi: 10.3889/oamjms.2019.870
49. Jamieson L, Smithers L, Hedges J, Parker E, Mills H, Kapellas K, et al. Dental disease outcomes following a 2-year oral health promotion program for Australian aboriginal children and their families: a 2-arm parallel, single-blind, randomised controlled trial. EClinicalMedicine. (2018) 1:43–50. doi: 10.1016/j.eclinm.2018.05.001
50. Xiao J, Alkhers N, Kopycka-Kedzierawski DT, Billings RJ, Wu TT, Castillo DA, et al. Prenatal oral health care and early childhood caries prevention: a systematic review and meta-analysis. Caries Res. (2019) 53:411–21. doi: 10.1159/000495187
51. Frencken JE, Holmgren C, van Palenstein Helderman W. Basic Package of Oral Care (BPOC). (2002). Available online at: http://www.chdentalinstitute.org/images/bpoc.pdf (accessed May 13, 2022).
52. World Health Organization. World Health Assembly Paves the Way for Better Oral Health Care. (2021). Available online at: https://www.who.int/news/item/27-05-2021-world-health-assembly-resolution-paves-the-way-for-better-oral-health-care (accessed August 16, 2021).
53. World Health Organization. Follow-Up to the Political Declaration of the Third High-Level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Disease. (2022). Available online at: https://apps.who.int/gb/ebwha/pdf_files/WHA75/A75_10Add1-en.pdf (accessed April 30, 2022).
54. Organización Panamericana de la Salud. Prevención y manejo integral de las enfermedades orales. (ISBN 978-92-75-31798-3). Organización Mundial de la Salud (2013). Available online at: https://www.paho.org/sofar/documents/Modulo-I.pdf (accessed on January 31, 2022).
Keywords: oral health, dental care, prenatal care, child immunizations, LMICs, dental caries, healthcare, maternal-child health
Citation: Susarla SM, Trimble M and Sokal-Gutierrez K (2022) Cross-Sectional Analysis of Oral Healthcare vs. General Healthcare Utilization in Five Low- and Middle-Income Countries. Front. Oral. Health 3:911110. doi: 10.3389/froh.2022.911110
Received: 02 April 2022; Accepted: 31 May 2022;
Published: 23 June 2022.
Edited by:
Callum Durward, University of Puthisastra, CambodiaReviewed by:
Maha El Tantawi, Alexandria University, EgyptLivia Ottolenghi, Sapienza University of Rome, Italy
Copyright © 2022 Susarla, Trimble and Sokal-Gutierrez. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sita Manasa Susarla, manasasusarla@berkeley.edu; Margaret Trimble, margarettrimble@berkeley.edu
†These authors have contributed equally to this work and share first authorship
 Sita Manasa Susarla
Sita Manasa Susarla Margaret Trimble
Margaret Trimble Karen Sokal-Gutierrez
Karen Sokal-Gutierrez