- School of Management, Suzhou University, Suzhou, China
Introduction: This study aims to explore the influence mechanism of rural older adult health. By examining the mediating roles of education, income, and psychological capital in physical activity's impact on health, this study provides a reference for lifestyle interventions to improve the health level of rural older adults.
Methods: The analysis was conducted on a sample of 1778 rural older adults from CGSS2017, and data were analyzed using PROCESS V4.2 for multiple mediating effects.
Results: The findings indicate that physical activity impacts rural older adult health through multiple mediating pathways. The mediating role includes seven paths, comprising the independent effects of three mediating variables of income, education, and psychological capital, and the chain mediating effects generated together.
Discussion: Based on the influence mechanism of health on rural older adults, optimizing policy focus and developing a precise, interconnected, and sustainable health security system for older adults is necessary. These research results are of practical significance for advancing healthy aging in rural areas.
1. Introduction
Public health issues have become increasingly important to society, with health level a crucial measure of success (1, 2). Age and group disparities exist in health status, with older adults being particularly vulnerable (3). Health status is a significant factor that influences the life quality of older adults (4). Healthy aging is essential for economic and social development and is the foundation for formulating various social public policies (5). While life expectancy is increasing, the period of illness is disproportionately expanding (6), and chronic diseases in older adults are a significant health concern (7). Older adults require health care and nursing services, with rural older adults particularly needing attention (8, 9).
The issue of rural aging is a major global challenge (10). The diversity of rural areas is an essential consideration in rural aging (11), where, health risk factors and social and economic factors can influence healthy aging in rural areas (12). Changes in the economic structure have reduced rural families' dependence on the land. In contrast, changes in intergenerational relationships have led to declining traditional values and a lack of appropriate social security systems for rural older adults (13). As a result, rural older adults are a particularly fragile group (14) with high levels of disability (15) and caregiving challenges (16), and about one-third of rural older adults experience depressive symptoms (17). Rural older adults are also at risk of social isolation (18), experiencing social disconnectedness (19). In the context of population aging, exploring the mechanism of health influence on rural older adults can provide for policymaking to improve their health level.
Health is the ability to adapt and self-manage, encompassing physical and mental health (20). It is an essential capability, and all individual activities are based on it (21). Health has personal and public attributes and is the foundation for accumulating human capital (22). Health status results from continuous accumulation throughout life and will decline with age (23). The incidence of health problems varies at different life cycle stages (24). Relative economic backwardness, inadequate medical resources, and lagging health security systems in rural areas have resulted in a long-term accumulation of health disadvantages for older rural adults throughout their lifecycles (25). As a vulnerable group, they are more likely to encounter health risks (26). Cancer incidence and mortality rates among rural residents are higher than those in urban areas (27), and improving the health of older rural adults is vital to healthy aging (28).
Lifestyle, personal, and social factors impact the health of older rural adults (17, 18). Previous research has shown that regarding lifestyle, physical activity, social interaction (29), and diet (30) affect the health of older rural adults. Regarding personal factors, gender (31), income (32), education (33), and marital status (34) all affect the health of older rural adults. Living arrangements are a personal choice for older rural adults (35). They prefer to stay at home and in the community (36), with aging in place (37). Spouses can provide daily care and emotional support (34), and living arrangements and support from children can affect the health of older rural adults (38). Regarding social factors, healthcare needs in rural areas are not being met (39), and healthcare practices affect the health of older rural adults (40, 41). Community resources, infrastructure (42), internet use, and the digital divide (43) affect depression levels in older rural adults. Environmental factors (44) and pollution (45) also affect the health of older rural adults. Health influencing factors result from the interaction and accumulation of multiple factors, which can affect sustainable livelihoods and improve the quality of life for older rural adults (46). Therefore, this study aims to investigate the specific mechanism of rural older adult health.
2. Literature review
Physical activity significantly impacts health (47, 48). It is part of a healthy lifestyle (49, 50), and WHO believes physical activity can improve all aspects of health and provide multiple benefits (51). Physical activity effectively augments health beyond pharmaceutical treatments, lowering disease incidence, improving quality of life, and increasing healthy lifespan (52, 53). Sedentary behavior is a risk factor for older adult health (54) and contributes to overall mortality risk (55). Increasing physical activity is an essential strategy for preventing chronic disease (56) and can reverse its effects (57). A linear relationship exists between physical activity and health status (58). Physical activity is a health-promoting behavior (59). Lack of exercise leads to health risks (60, 61). Appropriate physical activity can improve health levels and reduce disability risk in older adults (15, 62), helping to alleviate the trend of disability in older adults (63). Physical activity can prevent frailty (64), delay the development of frailty (65), relieve depression, reduce anxiety, and improve mental health. These outcomes have been observed in residents of different countries (66, 67). Moreover, physical activity strengthens older adults' cognitive function (68). It is a low-cost and effective cognitive function intervention (47, 69). Previous literature has established the impact of physical activity on health. This study primarily concerns how physical activity affects older rural adult health.
Education affects health, providing positive returns on investment (70). The theory of acquired effectiveness states that education is the most critical factor affecting individual health. It endows individuals with various resources, enhancing their sense of control over life and promoting a healthy lifestyle (71). Education and health are both human capital and are mutually reinforcing (72). According to the cumulative advantage and disadvantage hypothesis, the advantages of factors such as education will gradually strengthen. Health differences will continue to expand as health results from accumulated social capital and experience (73). Acceptance and decisions of health risks by older rural adults relate to their level of education, and the level of education has a significant positive effect on the health of older rural adults (33).
Income affects health (74). It is a core indicator of social and economic status, with higher income leading to more robust investment in health capabilities. Income inequality is the main factor of population health differences, and increasing the income of vulnerable groups can reduce health inequality and improve health levels (75). In rural areas, family pension functions are magnified, following the labor lifestyle of living and working into old age and continuously bringing income to the family (6). The increase in income positively affects health as a family's economic support (76). A significant relationship exists between income inequality and health (77). The pension level of older rural adults is low, and pension affects health (32). Medical expenditure is the primary source of the vulnerability of individual and family economic statuses (24), and poverty has a detrimental effect on the health of older rural adults (78).
Psychological capital (PsyCap) affects health (79). It is a core psychological resource, an individual's positive psychological state, including hope, efficacy, resilience, and optimism (80), with developability (81). As a personal resource, psychological capital affects mental health over time (82). It is related to positive emotions, guiding individuals to produce positive behaviors (83), and psychological capital affects successful aging (84). According to the expansion and construction theory of positive emotions, individuals with high psychological capital have more flexible cognitive and behavioral models. They are more likely to obtain energy from the outside when facing external risks (85). Positive psychological capital can protect individuals' health from harm in adversity (86). Psychological capital can improve health levels and alleviate depression in older rural adults (79, 87).
Health is a complex and comprehensive issue that requires a comprehensive measurement approach. Healthy aging emphasizes the centrality of functional ability, which encompasses personal capabilities, environmental features, and their combination (5). In the functional-centered healthy aging paradigm, physical activity and psychological capital reflect personal capabilities, while education and income are environmental features (88). Previous studies have identified physical activity, income, education, and psychological capital as predictors of health. However, how these variables interact with each other to influence health has not been thoroughly analyzed, and the underlying mechanisms are unclear.
Based on the findings of the studies described above concerning possible predictors of the health of older rural adults, this study examines the following hypotheses:
Hypothesis 1: Education plays a mediating role in the relationship between physical activity and health.
Hypothesis 2: Income plays a mediating role in the relationship between physical activity and health.
Hypothesis 3: Psychological capital plays a mediating role in the relationship between physical activity and health.
Hypothesis 4: Education, income, and psychological capital have multiple mediating effects between physical activity and health.
This study uses income, education, and psychological capital as mediating variables to construct a multiple mediating effect model and test physical activity pathways affecting the health of older rural adults.
3. Methods
3.1. Data sources
This study utilized data from the 2017 China General Social Survey (CGSS), a publicly available data source collecting data at multiple levels, including individuals, households, communities, and society, since 2003. The CGSS is widely used to study social issues due to its high data quality (89), strong applicability, and representativeness (90). After cleaning the original data, urban residents were excluded, followed by individuals below 60, resulting in a sample of older rural adults 60 and above. After removing missing and invalid samples, 1,778 valid samples were obtained, covering 26 provinces and cities in China and comprising 920 males and 858 females. The data contains comprehensive information on the individual characteristics and family situations of older adult respondents, providing robust data support for studying the relationship between physical activity and the health of older rural adults.
3.2. Measurements
The dependent variable was health, measured by physical and mental health (1). The question “How do you feel about your current physical health?” (70) assessed physical health. The re-coded question “How often do you feel depressed or discouraged?” (90) assessed mental health, with higher scores indicating better health. The independent variable was physical activity, measured by the question, “In the past year, do you often participate in physical activity during your leisure time?” (91). Answers were re-coded as never or rarely (0) and daily or several times a week (1).
Education, income, and psychological capital were the mediating variables. Education was measured by educational attainment (70). Income was measured by household economic status (91, 92). Psychological capital has four primary positive psychological resources, assessed by the indicators in the survey questionnaire (80, 93).
The hope dimension was measured by the questions “When things are uncertain, I usually expect things to turn out for the best” and “Overall, I expect more good things to happen to me than bad things.” The efficacy dimension was measured by “I think I am quite successful now.” The resilience dimension was measured by the questions “I am currently doing my best to pursue my goals” and “There are many solutions to the problems I am facing now.” Finally, the optimism dimension was measured by the questions “I have a positive attitude toward my future” and “I often get upset about small things.” After re-coding the reverse questions and summing up the scores, the higher the composite variable, the better the psychological capital. The four-dimensional psychological capital evaluation index had a Cronbach's α of 0.719, indicating a high level of reliability.
Based on previous studies, control variables included gender (31), marital status (34), and living arrangements (16, 94), all of which were represented as dummy variables.
3.3. Statistical analysis
Data were analyzed using PROCESS V4.2 for multiple mediating effects, which improved the accuracy of the estimation compared to the ordinary mediating effect model (95). The mediating effects were tested using the bootstrap method with 5,000 repeated sampling.
4. Results
4.1. Descriptive statistics and correlation analysis
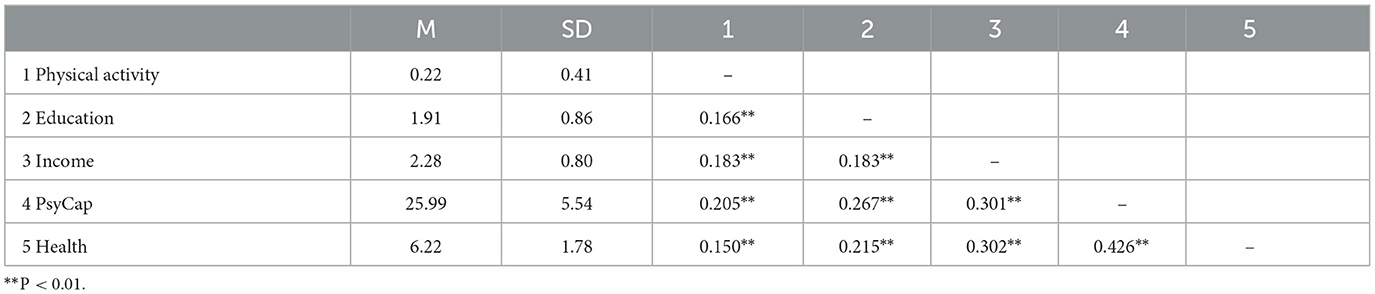
The descriptive statistics and correlation analysis results of the study variables are shown in Table 1. The Spearman correlation coefficient revealed that physical activity, education, income, and psychological capital were significantly positively correlated with health.
4.2. Regression analysis
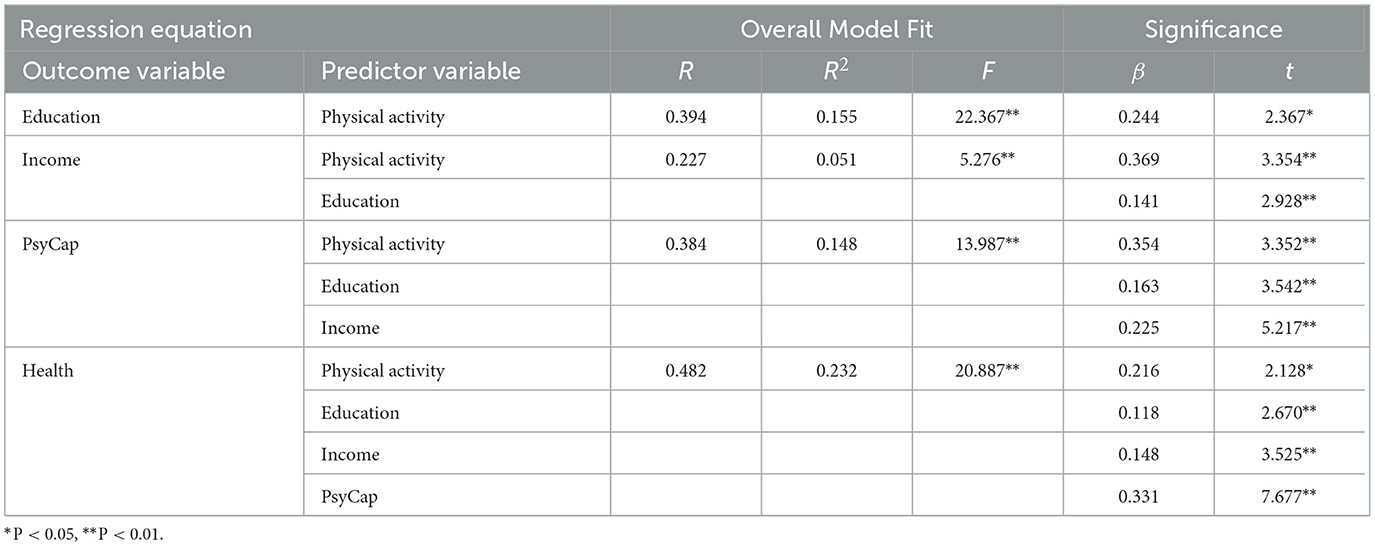
The results of the regression are presented in Table 2. Physical activity significantly positively predicted education (β = 0.244, p < 0.05), income (β =0.369, p < 0.01), and PsyCap (β = 0.354, p < 0.01). When physical activity, education, income, and PsyCap were entered into the regression equation simultaneously, physical activity (β = 0.216, p < 0.05), education (β = 0.118, p < 0.01), income (β = 0.148, p < 0.01), and PsyCap (β = 0.331, p < 0.01) significantly predicted the health of older rural adults.
4.3. Mechanism analysis
Physical activity significantly predicted health (β = 0.465, p < 0.01). A chained mediating effect test was conducted using PROCESS, with older rural adults' health as the dependent variable and physical activity as the independent variable, incorporating mediating and control variables. Figure 1 depicts the results. Education, income, and psychological capital play a chained mediating role between physical activity and health.
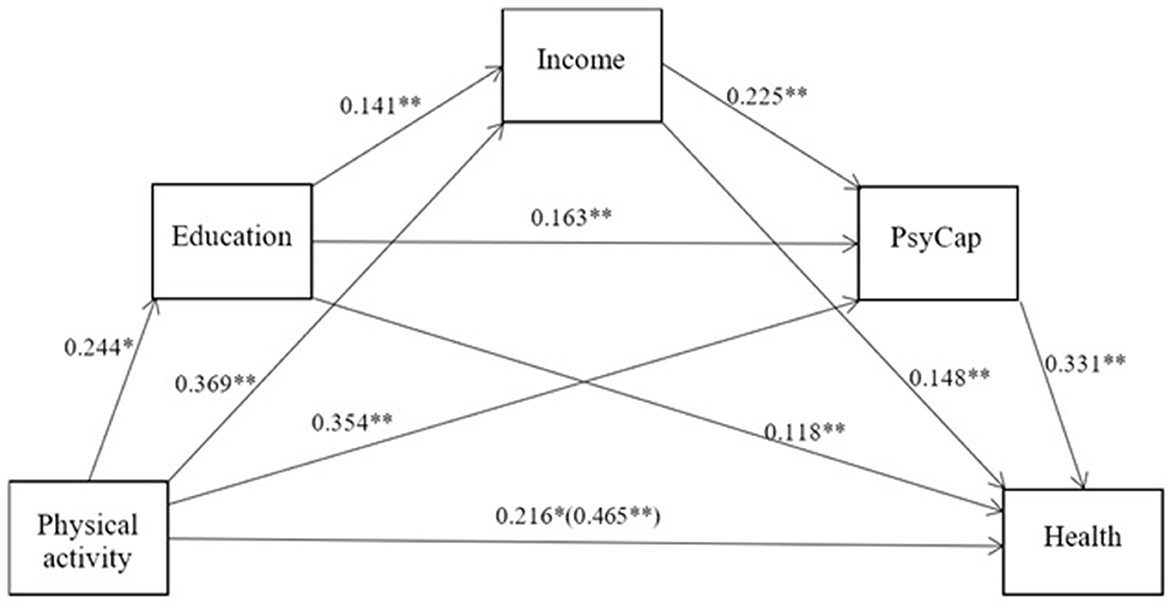
Figure 1. Chain mediating model of physical activity, education, income, and PsyCap. *P < 0.05, **P < 0.01.
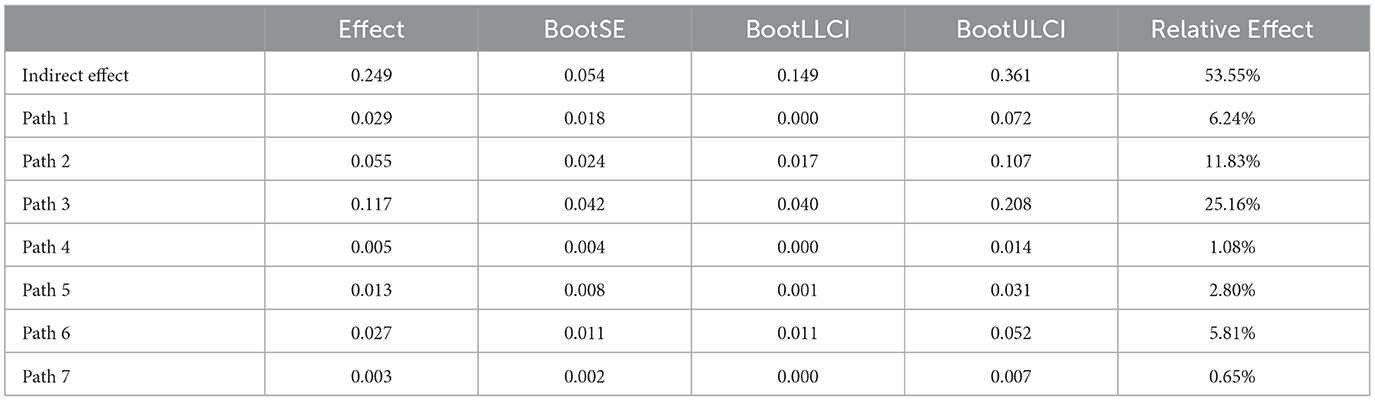
Table 3 shows the confidence intervals of the indirect effects, found to be statistically significant using the Bootstrap method. Enhancing physical activity, education, income, and psychological capital can effectively improve the health level of older rural adults. The results indicated that the indirect effect was 0.029 in path 1 with education as the mediator, 0.055 in path 2 with income as the mediator, 0.117 in path 3 with psychological capital as the mediator, 0.005 in path 4 with education and income as the mediators, 0.013 in path 5 with education and psychological capital as the mediators, 0.027 in path 6 with income and psychological capital as the mediators, and 0.003 in path with education, income, and psychological capital as the mediators. Hypotheses 1, 2, and 3 have been confirmed.
The mediating effect test results demonstrated that physical activity influences health through multiple mediations of education, income, and psychological capital. Therefore, Hypothesis 4 has also been validated. With a total mediating effect of 0.249, they account for 53.55% of the total effect of physical activity on the health of older rural adults.
5. Discussion
Enhancing the health level of older rural adults requires identifying the mechanism of influence. Research findings indicate that education, income, and psychological capital are the mechanisms by which physical activity impacts the health of older rural adults. Physical activity can improve overall health in older adults and has significant benefits (96). Moreover, physical activity is positively related to and is critical in achieving healthy aging (97). It can be initiated from an early life cycle stage, with robust plasticity, lower cost, and more significant benefit in intervening against and preventing health risks. Intervening with physical activity for older adults is a cost-effective way to improve their health (98). Enhancing physical fitness can lead to lifelong health benefits, enhance the quality of life of older rural adults, and result in sustained health benefits (48, 99, 100).
5.1. Independent mediating effects
Previous studies have found a relationship between physical activity and education, and education has been linked to health (71, 101). Physical activity and education are forms of cultural capital that positively influence rural resident health (92), thus supporting the findings of a mediating effect study of these variables. While some studies have suggested a link between education and physical activity (102–104), identifying causal relationships requires specific research contexts and a constant conjunction of variables (105). In this study, from a physical activity perspective, education, income, and psychological capital as mediators can help to understand the relationship between physical activity and health (95). In addition, physical activity has been identified as an effective way for individuals to increase their income (91).
Furthermore, physical activity can improve health by enhancing economic status (106). Personal wealth has been found to affect health (107). It has been suggested that the fewer public products and services provided by society, the more significant personal income is to health (108), consistent with the mediating effects of physical activity-income-health. Physical activity has been found to predict psychological capital positively (109). In addition, physical activity may foster and improve psychological capital (81, 110), which is related to health. The theory of planned behavior suggests that behavior beliefs affect attitude formation (111). Older rural adults believe that physical activity will affect health and build psychological capital, consistent with the mediating effects of physical activity-PsyCap-health.
5.2. Multiple mediating effects
Physical activity has been identified as a preventive health behavior (112), which can be explained by the Health Belief Model (113). It has been found that there is a positive correlation between physical activity and educational level (71), as individuals accumulate human capital through education, which can help them to increase their income (114). Income is economic capital that provides access to more health resources (92). Previous studies have shown that physical activity affects education and income (115). Education level and income are two indicators of social and economic status (116), and it has been observed that older adults' health is positively associated with these factors (117). Furthermore, research has shown that education affects health through income (118), which aligns with the mediating effects of physical activity-education-income-health.
Physical activity is linked to educational level. Individuals having higher educational levels exhibit a better social mentality, higher cognitive level, and more optimistic attitudes (71, 101). The Human Capital Theory suggests that education can affect health through psychological resources (119). Education is a dividing line for health. Individuals shape psychological capital through the educational process, which promotes health behavior intentions to reduce risks (120), thus explaining the mediating effect of physical activity-education-PsyCap-health.
Previous studies have demonstrated that physical activity can bring more income to individuals, with an income effect (121, 122), and income can improve social and economic status (91). Physical activity is cultural, and income is economic capital. Moreover, the durable elements of psychological capital constitute social capital (123). All of these forms of capital are integrated within individuals, mutually influencing and interacting with each other. Health is human capital, affected by cultural, economic, and social capital (79), consistent with the mediating effects of physical activity-income-PsyCap-health.
The Grossman health demand model can explain the multiple mediating model path constructed. This model postulates that health is a durable capital stock (124) with dual attributes of consumption and investment (22). Individual health stock decreases with age. However, it can be augmented through investment (124). Physical activity and education are considered health investment behaviors. Education influences resources and determines the efficiency of health investment. People with higher educational levels tend to have larger incomes, which can be used to purchase wellness services and invest in health capital. Moreover, education affects livelihood resilience (125), forming positive psychological capital in increasing investment and affecting older rural adults' health. The research results confirm the Grossman model.
5.3. Implications
When confronted with unpredictable future health-related risks (126), developing coping strategies and institutional safeguards to optimize policy focus and ensure the social effectiveness of policies is required (70). In addition, an age-friendly, sustainable health security system for older rural adults should be established to promote healthy aging in rural areas (127).
First, when constructing a multi-dimensional health security system for older rural adults, factors such as education, physical activity, and psychological capital should be considered to bring universal health benefits to older rural adults. Particular attention should be paid to older rural adults with low income, low educational levels, and low psychological capital. In addition, precise identification mechanisms for vulnerable groups should be established to ensure they can enjoy policy benefits.
Second, health education is crucial. Education transmits health concepts and prevention information and actively guides older rural adults to engage in physical activity. It encourages effective health decision-making, cultivating healthy lifestyles and health literacy (128), and reducing risks.
Third, creating public service facilities suitable for physical activity and considering the needs of older adults with an inclusive approach is essential. These facilities will provide quality public services, upgrade educational levels and expand income sources for older adults. Furthermore, they will refine social security systems and bolster the psychological capital of older rural adults.
5.4. Limitations and future research
Compared with previous studies, this paper makes several possible contributions. First, based on verifying the effect of physical activity on health using CGSS data, this paper uses income, education, and psychological capital as transmission paths. It uses mediating effect model to study how physical activity impacts the health of older rural adults. Second, prior literature has largely overlooked psychological capital's role in the association between physical activity and health. This paper employs psychological capital as a mediating factor to investigate the health of older rural adults. Third, by leveraging multiple mediating effects to elucidate the health of older rural adults, seven pathways were identified, thus augmenting the existing empirical research.
The core value of this research lies in investigating the effect of physical activity on the health of older rural adults and the mediating roles of education, income, and psychological capital. However, this study has some limitations. First, the health of older rural adults is affected by numerous factors. A considerable time lag may occur, and the effects are cumulative. Thus, only physical activity's influence on health has been studied, which cannot fully explain the long-term dynamic evolution of older rural adults' health. This area requires further exploration.
Regarding influence mechanisms, only education, income, and psychological capital are discussed, which overlooks other aspects. Future research should explore other mechanisms to supplement this paper's findings. Finally, research on older rural adult health should be expanded. More extensive research will help to balance instrumental and value rationality and benefit older rural adults' health and well-being.
6. Conclusions
Health is a universal desire and necessity for human beings. It serves as significant human capital, promotes individual capability, and is an essential resource for society. This study, from the perspective of income, education, and psychological capital, examines the influence mechanism of physical activity on older rural adult health. The findings suggest that income, education, and psychological capital are mediating variables for physical activity to affect older rural adults' health. Physical activity affects the health of older rural adults through multiple mediating effects of income, education, and psychological capital. This mediation effect includes seven paths, including the independent effect of the mediating variable and the chain mediating effect generated together. In light of the mechanism of health influence on older rural adults, this research optimizes the policy focus and constructs a precise, interconnected, and sustainable health security system. The research results are of practical significance for advancing healthy aging in rural areas.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found at: http://cgss.ruc.edu.cn/index.htm.
Author contributions
YS designed the study, performed the statistical analysis, wrote the first draft, polished the manuscript, and approved the submitted version.
Funding
This research was supported by the Anhui Province Social Science Innovation and Development Research Project (2021CX119), Anhui Universities Quality Engineering Project (2021shsjkc024), The Ministry of Education's Industry-University Cooperation Collaborative Education Project (202101291015), Anhui Universities Quality Engineering Project (2018mooc586), and the Horizontal Project of Suzhou University (2022xhx076).
Acknowledgments
The author would like to thank the editors and reviewers.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rudnicka E, Napierała P, Podfigurna A, Meczekalski B, Smolarczyk R, Grymowicz M. The world health organization (WHO) approach to healthy ageing. Maturitas. (2020) 139:6–11. doi: 10.1016/j.maturitas.2020.05.018
2. Hertzman C, Siddiqi A. Population health and the dynamics of collective development. Successful Soc Inst Cult Affect Health. (2009) 17:23–52. doi: 10.1017/CBO9780511816192.003
3. Grundy E. Ageing and vulnerable elderly people: European perspectives. Ageing Soc. (2006) 26:105–34. doi: 10.1017/S0144686X05004484
4. Zhang W, Fu M. The health status of the Chinese older adults and its trends in 2010 2020: evidence from the population census and sampling data. Chin J Pop Sci. (2022) 212:17–31. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFD&dbname=CJFDLAST2022&filename=ZKRK202205003&v= (accessed March 31, 2023).
5. Beard JR, Officer A, de Carvalho IA, Sadana R, Pot AM, Michel J-P, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet. (2016) 387:2145–54. doi: 10.1016/S0140-6736(15)00516-4
6. Chen Y, Sun Y. Amplification and reduction: the hidden facts in China's ageing population and the implications for ageing measurement and theory. Pop Res. (2023) 47:3–22. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFD&dbname=CJFDAUTO&filename=RKYZ202301001&v= (accessed March 31, 2023).
7. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in china and its provinces, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
8. Ge Y, Wang L, Feng W, Zhang B, Liu S, Ke Y. The challenge and strategy selection of healthy aging in China. Manage World. (2020) 36:86–96. doi: 10.19744/j.cnki.11-1235/f.2020.0055
9. Goins RT, Williams KA, Carter MW, Spencer SM, Solovieva T. Perceived barriers to health care access among rural older adults: a qualitative study. J Rural Health. (2005) 21:206–13. doi: 10.1111/j.1748-0361.2005.tb00084.x
10. Rigg J, Phongsiri M, Promphakping B, Salamanca A, Sripun M. Who will tend the farm? Interrogating the ageing Asian farmer. J Peasant Stu. (2020) 47:306–25. doi: 10.1080/03066150.2019.1572605
11. Glasgow N, Brown DL. Rural ageing in the United States: trends and contexts. J Rural Stud. (2012) 28:422–31. doi: 10.1016/j.jrurstud.2012.01.002
12. Davis S, Bartlett H. Healthy ageing in rural Australia: issues and challenges. Australas J Ageing. (2008) 27:56–60. doi: 10.1111/j.1741-6612.2008.00296.x
13. Bhat AK, Dhruvarajan R. Ageing in India: drifting intergenerational relations, challenges and options. Ageing Soc. (2001) 21:621–40. doi: 10.1017/S0144686X0100842X
14. Xu J, Li S, Wu Z, Liu W. The vulnerability assessment of family support for the older adults in rural China: an empirical study based on data from Anhui. Population Res. (2019) 43:91–101. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFD&dbname=CJFDLAST2019&filename=RKYZ201901007&v= (accessed March 31, 2023).
15. Zhang X, Li W, Dai J, Zhang X. An analysis of urban-rural difference of self-care ability of seniors—an empirical analysis based on CHARLS (2018) data. Population Dev. (2022) 28:129–142. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFD&dbname=CJFDLAST2022&filename=SCRK202204011&v= (accessed March 31, 2023).
16. Yu Y, Chen J. Living in the Neighborhood or Living Together? Residential arrangement and cognitive health of the older adults in rural China. J Financ Econ. (2020) 46:49–63. doi: 10.16538/j.cnki.jfe.2020.08.004
17. Buys L, Roberto KA, Miller E, Blieszner R. Prevalence and predictors of depressive symptoms among rural older Australians and Americans. Austr J Rural Health. (2008) 16:33–9. doi: 10.1111/j.1440-1584.2007.00948.x
18. Baernholdt M, Yan G, Hinton I, Rose K, Mattos M. Quality of life in rural and urban adults 65 years and older: findings from the national health and nutrition examination survey. J Rural Health. (2012) 28:339–47. doi: 10.1111/j.1748-0361.2011.00403.x
19. Zhang D, Lin Z, Chen F, Li S. Reconfiguring social disconnectedness and its link to psychological well-being among older adults in rural China. J Appl Gerontol. (2023) 42:99–110. doi: 10.1177/07334648221124915
20. Huber M, Knottnerus JA, Green L, Van Der Horst H, Jadad AR, Kromhout D, et al. How should we define health? BMJ. (2011) 343:4163. doi: 10.1136/bmj.d4163
21. Miletzki J, Broten N. An Analysis of Amartya Sen's: Development as Freedom. Wood Dale, IL: Macat Library. (2017).
23. Dannefer D. Systemic and reflexive: foundations of cumulative dis/advantage and life-course processes. J Gerontol. (2020) 75:1249–63. doi: 10.1093/geronb/gby118
24. He M, Ding J. The effect of the affordability of health insurance on smoothing health risk——evidence from low- and middle-income medical insurance participants. Econ Persp. (2022) 734:83–102. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFD&dbname=CJFDLAST2022&filename=JJXD202204006&v= (accessed March 31, 2023).
25. Zhang Y, Yuan W. Does pension reduce the health risk of rural elderly? Also on the synergy of community older adults care services J Financ Econ. (2022) 48:49–63. doi: 10.16538/j.cnki.jfe.20220714.403
26. Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. (2006) 27:167–94. doi: 10.1146/annurev.publhealth.27.021405.102103
27. Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer Statistics in China, 2015. J Clin. (2016) 66:115–32. doi: 10.3322/caac.21338
28. Yu Y, Feng J. The dynamics of health of the older adults and the implications for healthy aging. World Econ Papers. (2017) 238:1–16. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFD&dbname=CJFDLAST2017&filename=SZWH201703001&v= (accessed March 31, 2023).
29. Schmidt LL, Johnson S, Genoe MR, Jeffery B, Crawford J. Social interaction and physical activity among rural older adults: a scoping review. J Aging Phys Act. (2022) 30:495–509. doi: 10.1123/japa.2021-0046
30. Zhao H, Andreyeva T. Diet quality and health in older americans. Nutrients. (2022) 14:1198. doi: 10.3390/nu14061198
31. Ross CE, Masters RK, Hummer RA. Education and the gender gaps in health and mortality. Demography. (2012) 49:1157–83. doi: 10.1007/s13524-012-0130-z
32. Riumallo-Herl C, Aguila E. The effect of old-age pensions on health care utilization patterns and insurance uptake in Mexico. BMJ Glob Health. (2019) 4:e001771. doi: 10.1136/bmjgh-2019-001771
33. Zhu Y, Wang H, Zhu Y. The influence of grandchild care and agricultural work on the health of rural older adults. J China Univ Geosci. (2022) 22:112–27. doi: 10.16493/j.cnki.42-1627/c.2022.04.011
34. Li Q, Zhao R, Zhang T. How does becoming widowed affect the rural older adults health? based on the data of CHARLS. Nankai Econ Studies. (2022) 224:157–176. doi: 10.14116/j.nkes.2022.02.010
35. Chen SHZ, Lou VWQ. Residential reasoning: how childless older adults choose between ageing in place (AIP) and institutionalisation in rural China. Ageing Soc. (2023) 43:516–34. doi: 10.1017/S0144686X2100074X
36. Anderson EM, Larkins S, Beaney S, Ray RA. Should i stay or go: rural ageing, a time for reflection. Geriatrics. (2018) 3:49. doi: 10.3390/geriatrics3030049
37. Henning-Smith C, Lahr M, Mulcahy J, MacDougall H. Unmet needs for help with mobility limitations among older adults aging in place: the role of rurality. J Aging Health. (2023) doi: 10.1177/08982643231151777
38. Silverstein M, Cong Z, Li S. Intergenerational transfers and living arrangements of older people in rural China: Consequences for psychological well-being. J Gerontol Soc Sci. (2006) 61:S256–66. doi: 10.1093/geronb/61.5.S256
39. Gao Q, Prina M, Wu Y-T, Mayston R. Unmet healthcare needs among middle-aged and older adults in China. Age a Ageing. (2022) 51:afab235. doi: 10.1093/ageing/afab235
40. Rush KL, Singh S, Seaton CL, Burton L, Li E, Jones C, et al. Telehealth use for enhancing the health of rural older adults: a systematic mixed studies review. Gerontologist. (2022) 62:E564–77. doi: 10.1093/geront/gnab141
41. Intarot W. Understanding the effect of using music therapy programme without music therapists for seniors with early stage of dementia in Thailand: a preliminary study. Int J Interdis Res. (2018) 7:781. doi: 10.2139/ssrn.3226781
42. Li LW, Liu J, Zhang Z, Xu H. Late-life depression in Rural China: do village infrastructure and availability of community resources matter? Int J Geriatr Psychiatry. (2015) 30:729–36. doi: 10.1002/gps.4217
43. Li L, Jin G, Guo Y, Zhang Y, Jing R. Internet access, support, usage divides, and depressive symptoms among older adults in China: a nationally representative cross-sectional study. J Affect Disord. (2023) 323:514–23. doi: 10.1016/j.jad.2022.12.001
44. Winterton R, Warburton J, Keating N, Petersen M, Berg T, Wilson J. Understanding the influence of community characteristics on wellness for rural older adults: a meta-synthesis. J Rural Stud. (2016) 45:320–7. doi: 10.1016/j.jrurstud.2015.12.010
45. Wang Y, Xiong H, Chen C. Agricultural non-point source pollution and health of the elderly in rural China. PLoS ONE. (2022) 17:e0274027. doi: 10.1371/journal.pone.0274027
46. Gao B, Li C, Li S. Follow-up supportive policy, resource endowments, and livelihood risks of anti-poverty relocated households: evidence from Shaanxi Province. Econ Geography. (2022) 42:168–77.
47. Raafs BM, Karssemeijer EG, Van der Horst L, Aaronson JA, Rikkert MGO, Kessels RP. Physical exercise training improves quality of life in healthy older adults: a meta-analysis. J Aging Phys Act. (2020) 28:81–93. doi: 10.1123/japa.2018-0436
48. Warburton DE, Bredin SS. Health benefits of physical activity: a systematic review of current systematic reviews. Curr Opin Cardiol. (2017) 32:541–56. doi: 10.1097/HCO.0000000000000437
49. Cockerham WC. Health lifestyle theory and the convergence of agency and structure. J Health Soc Behav. (2005) 46:51–67. doi: 10.1177/002214650504600105
50. Whangmahaporn P, Simmonds P, Whangmahaporn B. Factors affecting quality of life of the elderly in Thailand. Asian Political Sci Rev. (2018) 2:833. doi: 10.2139/ssrn.3304833
51. Organization WH. Global Action Plan on Physical Activity 2018-2030: More Active People for a Healthier World. Vienna: World Health Organization. (2019).
52. Campisi J, Kapahi P, Lithgow GJ, Melov S, Newman JC, Verdin E. From discoveries in ageing research to therapeutics for healthy ageing. Nature. (2019) 571:183–92. doi: 10.1038/s41586-019-1365-2
53. Whangmahaporn P. The development of operational achievements in the elderly quality of life development and career promotion centers of Thailand. Int J Interdis Res. (2019) 8:135. doi: 10.2139/ssrn.3398135
54. Copeland JL, Ashe MC, Biddle SJH, Brown WJ, Buman MP, Chastin S, et al. Sedentary time in older adults: a critical review of measurement, associations with health, and interventions. Br J Sports Med. (2017) 51:1539. doi: 10.1136/bjsports-2016-097210
55. van der Ploeg HP, Chey T, Korda RJ, Banks E, Bauman A. Sitting time and all-cause mortality risk in 222 497 australian adults. Arch Intern Med. (2012) 172:494–500. doi: 10.1001/archinternmed.2011.2174
56. Beck AM, Serrano NH, Toler A, Brownson RC. Multilevel correlates of domain-specific physical activity among rural adults - a cross-sectional study. BMC Public Health. (2022) 22:2150. doi: 10.1186/s12889-022-14634-3
57. McPhee JS, French DP, Jackson D, Nazroo J, Pendleton N, Degens H. Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology. (2016) 17:567–80. doi: 10.1007/s10522-016-9641-0
58. Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: the evidence. CMAJ. (2006) 174:801–9. doi: 10.1503/cmaj.051351
59. Tiaotrakul A, Koeipakvaen T, Sertbudra P. The development of physical activity leaders using a contemplative education approach to promote wellness among the elderly. Int J Interdis Res. (2019) 8:7090. doi: 10.2139/ssrn.3547090
60. Rhodes RE, Janssen I, Bredin SS, Warburton DE, Bauman A. Physical activity: health impact, prevalence, correlates and interventions. Psychol Health. (2017) 32:942–75. doi: 10.1080/08870446.2017.1325486
61. Lee I-M, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. (2012) 380:219–29. doi: 10.1016/S0140-6736(12)61031-9
62. Pahor M, Guralnik JM, Ambrosius WT, Blair S, Bonds DE, Church TS, et al. Effect of structured physical activity on prevention of major mobility disability in older adults the life study randomized clinical trial. JAMA. (2014) 311:2387–96. doi: 10.1001/jama.2014.5616
63. Söderhamn O, Lindencrona C, Ek A-C. Ability for self-care among home dwelling elderly people in a health district in Sweden. Int J Nurs Stud. (2000) 37:361–8. doi: 10.1016/S0020-7489(00)00015-8
64. Dent E, Morley JE, Cruz-Jentoft AJ, Woodhouse L, Rodríguez-Mañas L, Fried LP, et al. Physical frailty: ICFSR international clinical practice guidelines for identification and management. J Nutr Health Aging. (2019) 23:771–87. doi: 10.1007/s12603-019-1273-z
65. Haskell WL, Blair SN, Hill JO. Physical activity: health outcomes and importance for public health policy. Prev Med. (2009) 49:280–2. doi: 10.1016/j.ypmed.2009.05.002
66. Schuch FB, Vancampfort D, Firth J, Rosenbaum S, Ward PB, Silva ES, et al. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiatry. (2018) 175:631–48. doi: 10.1176/appi.ajp.2018.17111194
67. Kazeminia M, Salari N, Vaisi-Raygani A, Jalali R, Abdi A, Mohammadi M, et al. The effect of exercise on anxiety in the older adults worldwide: a systematic review and meta-analysis. Health Qual Life Outcomes. (2020) 18:1–8. doi: 10.1186/s12955-020-01609-4
68. Angevaren M, Aufdemkampe G, Verhaar HJJ, Aleman A, Vanhees L. Physical activity and enhanced fitness to improve cognitive function in older people without known cognitive impairment. Cochrane Datab Syst Rev. (2008) 2:CD005381. doi: 10.1002/14651858.CD005381.pub3
69. Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: recommendation from the american college of sports medicine and the american heart association. Circulation. (2007) 116:1094. doi: 10.1249/mss.0b013e3180616aa2
70. Hu A. Can education make us healthier? An urban-rural comparative analysis based on the chinese general social survey of 2010. Soc Sci China. (2015) 36:64–82. doi: 10.1080/02529203.2015.1001321
71. Mirowsky J. Education, Social Status, and Health. Lonodn: Routledge. (2017). doi: 10.4324/9781351328081
73. DiPrete TA, Eirich GM. Cumulative advantage as a mechanism for inequality: a review of theoretical and empirical developments. Annu Rev Sociol. (2006) 32:271–97. doi: 10.1146/annurev.soc.32.061604.123127
74. Subramanian SV, Kawachi I. Income inequality and health: what have we learned so far? Epidemiol Rev. (2004) 26:78–91. doi: 10.1093/epirev/mxh003
75. Lynch J, Smith GD, Harper SA, Hillemeier M, Ross N, Kaplan GA, et al. Is income inequality a determinant of population health? Part 1 a systematic review. Milbank Q. (2004) 82:5–99. doi: 10.1111/j.0887-378X.2004.00302.x
76. Liu C, Yi F, Xu Z. Parental health: time vs money, which is more important? The influence of rural labor migration re-evaluation. Manage World. (2017) 286:74–87. doi: 10.19744/j.cnki.11-1235/f.2017.07.007
77. Matthew P, Brodersen DM. Income inequality and health outcomes in the United States: an empirical analysis. Soc Sci J. (2018) 55:432–42. doi: 10.1016/j.soscij.2018.05.001
78. Liu J, Zhang Y. Impact of poverty on the health status of rural residents and its mechanisms: evidence from china household finance survey. J China Agric Univ. (2021) 38:55–71. doi: 10.13240/j.cnki.caujsse.2021.03.005
79. Chi S. Social networks, psychological capital and health comparison of urban and rural residents. Pop Dev. (2014) 20:96–103. doi: 10.3969/j.issn.1674-1668.2014.03.015
80. Luthans F, Youssef-Morgan CM. Psychological capital: An evidence-based positive approach. Annu Rev Organ Psychol Organ Behav. (2017) 4:339–66. doi: 10.1146/annurev-orgpsych-032516-113324
81. Luthans F, Youssef CM, Avolio BJ. Psychological Capital: Developing the Human Competitive Edge. Oxford University Press (2006). doi: 10.1093/acprof:oso/9780195187526.001.0001
82. Avey JB, Luthans F, Smith RM, Palmer NF. Impact of positive psychological capital on employee well-being over time. J Occup Health Psychol. (2010) 15:17. doi: 10.1037/a0016998
83. Avey JB, Wernsing TS, Luthans F. Can positive employees help positive organizational change? Impact of psychological capital and emotions on relevant attitudes and behaviors. J Appl Behav Sci. (2008) 44:48–70. doi: 10.1177/0021886307311470
84. Li M, Luo H, Qian Y, Niu Y. The influence of psychological capital and OPS on successful aging. Chin J Appl Psychol. (2016) 22:153–61. doi: 10.3969/j.issn.1006-6020.2016.02.006
85. Fredrickson BL. The role of positive emotions in positive psychology: the broaden-and-build theory of positive emotions. Am Psychol. (2001) 56:218. doi: 10.1037/0003-066X.56.3.218
86. Luthar SS. Resilience in development: A synthesis of research across five decades. Developmental psychopathology. Risk Disorder Adapt. (2015) 3:739–95. doi: 10.1002/9780470939406.ch20
87. Huang L, Wang F, Zhang H, Yang S. Mediating effect of psychological capital between loneliness and depression in rural empty nest older adults. Chin J Health Statistics. (2021) 38:280–2. Available online at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CJFD&dbname=CJFDLAST2021&filename=ZGWT202102031&v= (accessed March 31, 2023).
88. Cesari M, de Carvalho IA, Thiyagarajan JA, Cooper C, Martin FC, Reginster J-Y, et al. Evidence for the domains supporting the construct of intrinsic capacity. J Gerontol Biol Sci Med Sci. (2018) 73:1653–60. doi: 10.1093/gerona/gly011
89. Bian Y, Li L. The chinese general social survey (2003-8) sample designs and data evaluation. Chin Sociol Rev. (2012) 45:70–97. doi: 10.2753/CSA2162-0555450104
90. Fang H. An empirical study of the influence of social capital on the health of urban and rural older adults——based on CGSS mixed section data. J Agric Univ. (2020) 146:88–97. doi: 10.13300/j.cnki.hnwkxb.2020.02.011
91. Zhong H, Wang Z, Gao Y. Can participate in physical exercise improve socio-economic status? An empirical study based on the cgss2015 survey data. J Wuhan Inst Phys Educ. (2020) 54:38–46. doi: 10.15930/j.cnki.wtxb.2020.01.006
92. Wang H. The effect and mechanism of cultural capital on the health of rural residents–empirical analysis based on CGSS (2017). Soc Sci Ningxia. (2021) 227:126–137. doi: 10.3969/j.issn.1002-0292.2021.03.015
93. Luthans F, Youssef CM. Human, social, and now positive psychological capital management: Investing in people for competitive advantage. (2004) 33:143–160. doi: 10.1016/j.orgdyn.2004.01.003
94. Henning-Smith C, Gonzales G. The relationship between living alone and self-rated health varies by age: evidence from the national health interview survey. J Appl Gerontol. (2020) 39:971–80. doi: 10.1177/0733464819835113
95. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: Guilford Publications. (2017).
96. Hamer M, Lavoie KL, Bacon SL. Taking up physical activity in later life and healthy ageing: the english longitudinal study of ageing. Br J Sports Med. (2014) 48:239–43. doi: 10.1136/bjsports-2013-092993
97. Daskalopoulou C, Stubbs B, Kralj C, Koukounari A, Prince M, Prina AM. Physical activity and healthy ageing: a systematic review and meta-analysis of longitudinal cohort studies. Ageing Res Rev. (2017) 38:6–17. doi: 10.1016/j.arr.2017.06.003
98. Jorge S-P, David N-V, Alba G-C, German V-R, Antonio CJ. Health economic evaluation of exercise interventions in people over 60 years old: a systematic review. Exp Gerontol. (2022) 161:111713. doi: 10.1016/j.exger.2022.111713
99. Zhu W, Chi A, Sun Y. Physical activity among older Chinese adults living in urban and rural areas: a review. J Sport Health Sci. (2016) 5:281–6. doi: 10.1016/j.jshs.2016.07.004
100. Sun F, Norman IJ, While AE. Physical activity in older people: a systematic review. BMC Public Health. (2013) 13:1–17. doi: 10.1186/1471-2458-13-449
101. Pfeifer C, Cornelißen T. The impact of participation in sports on educational attainment—New evidence from Germany. Econ Educ Rev. (2010) 29:94–103. doi: 10.1016/j.econedurev.2009.04.002
102. Kari JT, Viinikainen J, Böckerman P, Tammelin TH, Pitkänen N, Lehtimäki T, et al. Education leads to a more physically active lifestyle: evidence based on Mendelian randomization. Scand J Med Sci Sports. (2020) 30:1194–204. doi: 10.1111/sms.13653
103. Shaw BA, Spokane LS. Examining the association between education level and physical activity changes during early old age. J Aging Health. (2008) 20:767–87. doi: 10.1177/0898264308321081
104. Orhan R. The effect of school education on students' participation in sports and physical activity and profiles of individuals with physical activity and fitness habits in Turkey. Afr Educ Res J. (2020) 8:287–97.
105. Hume D. An Enquiry Concerning Human Understanding: A Critical Edition. Oxford: Oxford University Press. (2000).
106. Xu J, Yang S. Influence and mechanism of public sports service on residents' happiness: an empirical study based on CGSS (2017) micro survey data. J Wuhan Inst Phys Educ. (2021) 55:26–32.
107. Hoffmann R, Kröger H, Geyer S. Social causation versus health selection in the life course: does their relative importance differ by dimension of SES? Soc Indic Res. (2019) 141:1341–67. doi: 10.1007/s11205-018-1871-x
108. Marmot M. The influence of income on health: views of an epidemiologist. Health Aff. (2002) 21:31–46. doi: 10.1377/hlthaff.21.2.31
109. Jiao L, Fan W, Zhang G. The effect of physical activity at home on adolescents' boredom under the COVID-19 epidemic in China: A moderated mediating model. Chin J special education. (2020) 77–82. doi: 10.3969/j.issn.1007-3728.2020.10.013
110. Tan Y, Zhang W, Zhang T. An empirical study of influence of physical exercise on subjective well-being of members of spontaneous sports group based on mediating effect of psychological capital. J Wuhan Inst Phys Educ. (2020) 54:64–71. doi: 10.15930/j.cnki.wtxb.2020.09.009
111. Ajzen I. From Intentions to Actions: A Theory of Planned Behavior. Cham: Springer. (1985). doi: 10.1007/978-3-642-69746-3_2
112. Contoyannis P, Jones AM. Socio-economic status, health and lifestyle. J Health Econ. (2004) 23:965–95. doi: 10.1016/j.jhealeco.2004.02.001
113. Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. (1974) 2:328–35. doi: 10.1177/109019817400200403
114. Mirowsky J, Ross CE. Education, personal control, lifestyle and health: a human capital hypothesis. Res Aging. (1998) 20:415–49. doi: 10.1177/0164027598204003
115. Barron JM, Ewing BT, Waddell GR. The effects of high school athletic participation on education and labor market outcomes. Re Econ Stat. (2000) 82:409–21. doi: 10.1162/003465300558902
116. Lutfey K, Freese J. Toward some fundamentals of fundamental causality: socioeconomic status and health in the routine clinic visit for diabetes. Am J Sociol. (2005) 110:1326–72. doi: 10.1086/428914
117. Lu J, Guo R. An empirical study on health and health inequality of chinese older adults: based on regional and community perspective. Population J. (2017) 39:57–67. doi: 10.16405/j.cnki.1004-129X.2017.02.006
118. Ross CE, Wu C. The links between education and health. Am Sociol Rev. (1995) 719–745. doi: 10.2307/2096319
119. Herd P. Education and health in late-life among high school graduates: Cognitive versus psychological aspects of human capital. J Health Soc Behav. (2010) 51:478–96. doi: 10.1177/0022146510386796
120. Maloney EK, Lapinski MK, Witte K. Fear appeals and persuasion: a review and update of the extended parallel process model. Soc Personal Psychol Compass. (2011) 5:206–19. doi: 10.1111/j.1751-9004.2011.00341.x
121. Lechner M, Sari N. Labor market effects of sports and exercise: evidence from Canadian panel data. Labour Econ. (2015) 35:1–15. doi: 10.1016/j.labeco.2015.04.001
122. Cheng Z. Can exercise habit bring higher incomes? South China J Econ. (2020) 370:121–140. doi: 10.19592/j.cnki.scje.371089
123. Hosen R. Education and capital development: Capital as durable personal, social, economic and political influences on the happiness of individuals. Education. (2003) 123:123. Available online at: https://link.gale.com/apps/doc/A100806941/AONE?u=anon~4967d464&sid=googleScholar&xid=f51e0793 (accessed March 31, 2023).
124. Grossman M. On the concept of health capital and the demand for health. J Polit Econ. (1972) 80:223–55. doi: 10.1086/259880
125. Cutler DM, Lleras-Muney A. Understanding differences in health behaviors by education. J Health Econ. (2010) 29:1–28. doi: 10.1016/j.jhealeco.2009.10.003
127. McCrillis E, Skinner MW, Colibaba A. Developing rural insights for building age-friendly communities. J Rural Stud. (2021) 81:336–44. doi: 10.1016/j.jrurstud.2020.10.053
Keywords: physical activity, older rural adults, psychological capital, multiple mediating, health
Citation: Sun Y (2023) Physical activity's impact on rural older adult health: The multiple mediating effects of education, income, and psychological capital. Front. Public Health 11:1173217. doi: 10.3389/fpubh.2023.1173217
Received: 24 February 2023; Accepted: 28 March 2023;
Published: 17 April 2023.
Edited by:
Kittisak Jermsittiparsert, University of City Island, CyprusReviewed by:
Nai Peng Tey, University of Malaya, MalaysiaSrirath Gohwong, Kasetsart University, Thailand
Copyright © 2023 Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yujin Sun, szxyshx@163.com
 Yujin Sun
Yujin Sun