- 1Guangdong Mental Health Center, Guangdong Provincial People's Hospital (Guangdong Academy of Medical Sciences), Southern Medical University, Guangzhou, China
- 2Department of Psychology, School of Public Health, Southern Medical University, Guangzhou, China
- 3Department of Medical Statistics, School of Public Health, Sun Yat-sen University, Guangzhou, China
Aims: This study aimed to explore the dyadic effects of depression and anxiety on insomnia symptoms in Chinese older adults and their caregivers living in a community setting.
Methods: Data were collected from 1,507 pairs of older adults and their caregivers who were in the Guangdong Mental Health Survey in China. The 9-item Patient Health Questionnaire (PHQ-9), Generalized Anxiety Disorder module 7 (GAD-7), and Insomnia Severity Index (ISI) were used to measure depression, anxiety, and insomnia symptoms. Actor-Partner Interdependence Models (APIM) were used to determine whether anxiety or depression symptoms predicted individual or dyadic insomnia.
Results: Older adults' and caregivers' depression and anxiety had significant positive correlations with their own and their caregivers' insomnia symptoms (all P < 0.001). Actor effects were found between depression and insomnia symptoms in both older adults and caregivers (B = 0.695, P < 0.001; B = 0.547, P < 0.001, respectively), with one significant partner effects (B = 0.080, P = 0.007). Actor effects were also found between anxiety and insomnia symptoms in both older adults and caregivers (B = 0.825, P < 0.001; B = 0.751, P < 0.001, respectively), with one significant partner effects (B = 0.097, P = 0.004). However, the caregivers' depression and anxiety were not associated with older adults' insomnia symptoms in the APIM analyses.
Conclusions: Older adults and their caregivers had an interrelationship between psychological distress and insomnia. Consequently, healthcare providers might consider involving dyads when designing programs to reduce insomnia and improve psychological distress for family caregivers.
1. Introduction
China bears a heavy burden of disease due to its large population of older adults aged 65 or more, which accounts for 13.5% of the total population (1). China is already amongst the aging societies and the burden of diseases has subsequently risen as a result (2). Sleep disturbance, depressive and anxiety disorders are relatively prevalent psychiatric conditions in late life. A meta-analysis of older people in Europe and North America illustrated a lifetime prevalence of major depression of 16.5% (3). Similarly, a systematic review showed that the point prevalence of late-life mild depression varies from 0 to 18.6% (4). According to former findings, the current and lifetime prevalence rates of anxiety disorders among older adults were 14.2 and 30.0%, respectively (5). In addition, over half of older adults worldwide experienced trouble sleeping, and 20 to 40% reported insomnia (6). Mental health problems not only worsened older adults' quality of life and social function, but also increased caregiver burden.
Owing to the Chinese traditional Confucian contexts, China places a great importance on respecting and caring for older adults, as well as an old age of want. In China, older adults are generally living with spouse and/or children, which provides material, emotional, and other supports to older adults and promote interaction with family members (7). Family members are main providers of care for the Chinese older adults (8, 9). This brings the multiple burdens to family caregivers, including objective burdens (caregiving-related negative things and changes in physical health and behavior) and subjective burdens (emotional reactions such as anxiety, worry, frustration, and fatigue) (10). With the COVID-19 pandemic, quarantine was considered as a protective strategy and has a radical impact on older adults' lifestyle (11). Older adults were required to stay at home, it increases the caregiving load (12) and exacerbates generational family conflict with caregivers (13). Older adults had a higher risk of COVID-19 infection and mortality rate than other individuals, which can detriment their mental health (14, 15). Some studies showed that older adults with chronic disease and their family caregivers experienced more psychological distress, such as depression, anxiety and sleep problems (16–18). Many studies on mental health at work concentrated on the anxiety and depressive symptoms of caregivers (19). Previous research displayed that 46.8 and 29.8% of older adults' caregivers had anxiety and depressive symptoms during the COVID-19 outbreak (15). Another undesirable outcome of long-term care is insomnia. Financial strain, limited leisure time, social isolation, and somatic condition of cared-for people may contribute to psychological distress and insomnia of caregivers (20–23).
Multiple studies have examined the relationship between psychological distress and sleep problems in older adults and caregivers (24–27). But older adults-caregiver dyadic associations between psychiatric symptomatology and insomnia have not received adequate attention. Although anxiety, depression and sleep problems were often studied on an individual level, the effect of interpersonal factors has increasingly become the focus of researchers in recent years (28, 29). Analyses of the dyadic data indicated inter-person correlations between chronic disease patients' and their caregivers' emotions (e.g., anxiety, depression) (16–18). Similarly, the congruence in emotions and sleep has also been reported in cancer patients and their spouses (30).
However, very few studies focused on general aged population, and how the dyadic relationship of depression and anxiety affects insomnia among Chinese older adults and their family caregivers was even rarely mentioned in COVID-19 outbreak. This gap in the literature potentially restricts the development and application of dyad-based interventions. Therefore, this study aimed at examining whether there is a dyadic relationship between depression, anxiety and insomnia among Chinese older adults and their family caregivers during the COVID-19 outbreak.
We proposed three hypotheses as follows:
1. Hypothesis 0: Individuals' depression and anxiety were positively associated with their own insomnia (actor effects).
2. Hypothesis 1: Older adults' depression and anxiety were positively associated with their caregivers' insomnia (partner effects).
3. Hypothesis 2: Caregivers' depression and anxiety were positively associated with older adults' insomnia (partner effects).
2. Methods
2.1. Participants and procedure
Participants in this study were older adult-caregiver dyads drawn from the Guangdong Mental Health Survey in China, which was conducted from October 2021 to December 2021. The target sample was picked from community-dwelling residents adopting multistage stratified cluster sampling, which included all the 21 administrative regions of Guangdong province. In the first stage, probability proportional to size (PPS) sampling was applied to choose 3 to 5 districts or counties from each administrative region. In the second stage, based on the population size of each district or county, we chose 1 to 4 subdistricts or towns from each selected district or county. Subsequently, we chose 2 to 4 village councils or neighborhood committees from each subdistrict or town using PPS, and then 50 residents were picked from each neighborhood. Finally, one adult resident older than 18 years was randomly chosen from each family in the selected village council or neighborhood committee. The sample included 18,464 residents aged 18 years and above, of whom 4,018 were aged 65 or over and completed the survey. For the selected older adults, their family caregivers were invited to participate in this survey. For this study, the definition of family caregivers is family members who provides care (daily life) for older adults.
In this study, the inclusion criteria of older adults were: (1) community-living older adults aged 65 years or older, (2) fluent Chinese language speaking, (3) provided informed consent, and (4) the selected older adults have caregivers who agreed to participate in this study and provided an informed assent. Exclusion criteria were: (1) residing in a nursing home, (2) hospitalization during the study period.
A total of 1,507 dyads provided complete data out of the 4,018 older individuals who were invited to participate in this study. Thus, 1,507 dyads in total were included for dyadic analyses. The questionnaire had a 37.5% response to invitation rate.
Socio-demographics, health-related factors, and mental health were interviewed face-to-face by investigators who have gone through uniform training, using an electronic structured questionnaire at local health service centers. The Research protocol was approved by the Ethics Committee of the Guangdong Provincial People's Hospital, Guangdong Academy of Medical Sciences (Reference number: KY2020-268-01).
2.2. Measures
2.2.1. Mental health characteristics
Older adults and caregivers rated their own depression symptoms in the past year using the 9-item Patient Health Questionnaire (PHQ-9). The PHQ-9, a self-reported 4-point Likert scale, contained nine items that measure depression in the past years. The total score ranges from 0 to 27, with higher scores representing worse depressive symptoms. A total score of 5 or more was considered as having depression symptoms (31). The Chinese version of PHQ-9 has already been used in many studies and proved to be reliable and valid (32, 33). We use Cronbach's alpha coefficient to assess internal consistency reliability of the questionnaires. In this study population, Cronbach's alpha coefficient of PHQ-9 was 0.940 for older adults and 0.924 for caregivers.
The Generalized Anxiety Disorder-7 item (GAD-7) (34) was used to measure older adults' and caregivers' anxiety symptoms in the past year. The GAD-7 contains seven items rated on a 4-point Likert scale, measuring anxiety in the past years. The total score ranges from 0 to 21, and each item rated a score of 0 to 3 (“not at all,” “several days,” “more than half the days,” “almost every day”). GAD-7 score of 5 or more was considered having anxiety symptoms. Scores are summed, with higher scores indicating more serious anxiety. It has been proved to have acceptable reliability and validity in the Chinese population (35). In the current study, the Cronbach's alpha coefficient of GAD-7 for older adults and their caregivers were 0.917 and 0.894, respectively.
Older adults and caregivers reported their insomnia symptoms in the past month using Insomnia Severity Index (ISI) (36). The ISI embodies seven items scored from o to 4, assessing the severity of insomnia. The total score ranges from 0 to 21, with higher scores indicating more severe insomnia and a score of 7 or more representing insomnia symptoms (37, 38). The scale has shown good psychometric properties in China (39). In this study, the Cronbach's alpha coefficient of ISI was 0.929 and 0.893 for older adults and caregivers, respectively.
2.2.2. Socio-demographics and health-related factors
The socio-demographics data include age, gender, region (urban/rural), education status, monthly income, marital status, and occupation group. Education level was recoded into five categories: primary school or below, junior high school, senior high school, college, and graduate school or above. Monthly income was categorized into 4 classes: <3,500, 3,500–5,999, 6,000–8,999, >9,000 ¥. Occupation group was divided into four categories: government officer/teacher/healthcare provider, factory/business/agriculture/service industry employee, retired, and others (40, 41). Marital status was dichotomized: married/cohabitating, and single/widowed/divorced/separated. Smoking status was divided into two groups: not smoking (including past smoking) and current smoking. Current smoking was defined as smoking at least one cigarette per day and continuing to smoke in the past 6 months. Alcohol consumption was defined as drinking at least once a week. The definition of tea-drinking habits was those of participants drinking tea at least four times a week. The exercise habits in the past year were grouped into five levels: hardly exercise, occasionally exercise (1–3 times/month), sometimes exercise (1–2 times/week), often exercise (more than 3 times/week), and almost every day. Chronic diseases were self-report of doctor-diagnosis and were listed based on International Classification of Disease, 10th revision (ICD-10), which contained hypertension, diabetes, cardio vascular disease, cerebrovascular disease, chronic obstructive pulmonary disease (COPD), hyperlipidemia, arthritis, discogenic diseases, chronic gastroenteritis/peptic ulcer, gallstones/chronic cholecystitis, urolithiasis, chronic hepatitis/hepatocirrhosis, cataract/glaucoma, gout, nervous system disease, cancer and anemia. Participants were asked “In the past year, have you ever been diagnosed by a physician that you have any of chronic disease in the list?” The number of chronic diseases was calculated and divided into three groups: 0 (no chronic disease), 1 (one chronic disease), and ≥2 (the co-occurrence of two or more chronic diseases) (42).
2.3. Statistical analyses
The paired sample t-tests, McNemar tests and McNemar-Bowker tests were used to compare characteristics between older adults and caregivers. Spearman bivariate correlations were conducted to examine older adult-caregiver associations between all primary variables. An actor-partner interdependency model (APIM) was used to examine the actor and partner effects on insomnia. Actor effects refer to whether a person's PHQ-9 score is related to their own ISI score. Partner effects mean the association between an individual's PHQ-9 score and another individual's ISI score. We specified older adults' and caregivers' depressive symptoms and anxiety symptoms as predictors, respectively, and their insomnia symptoms as outcome variables in the APIM analyses. In the final model, older adults' and caregivers' age, gender, and region were added as covariates. Restricted maximum likelihood estimation methods were applied. Model fit was evaluated by using the chi-square statistic, root mean square error of approximation (RMSEA), comparative fit index (CFI), standardized root mean residual (SRMR), and goodness of fit index (GFI). APIM models were performed in AMOS 24.0 and the rest of data analyses were performed in SPSS 25.0. All statistical tests were two-tailed with the level of significance set as 0.05.
3. Results
3.1. Characteristics description
A total of 1,507 older adults and their corresponding primary caregivers participated in this study (3,014 individuals). Table 1 reports the distribution of older adults' and caregivers' characteristics.
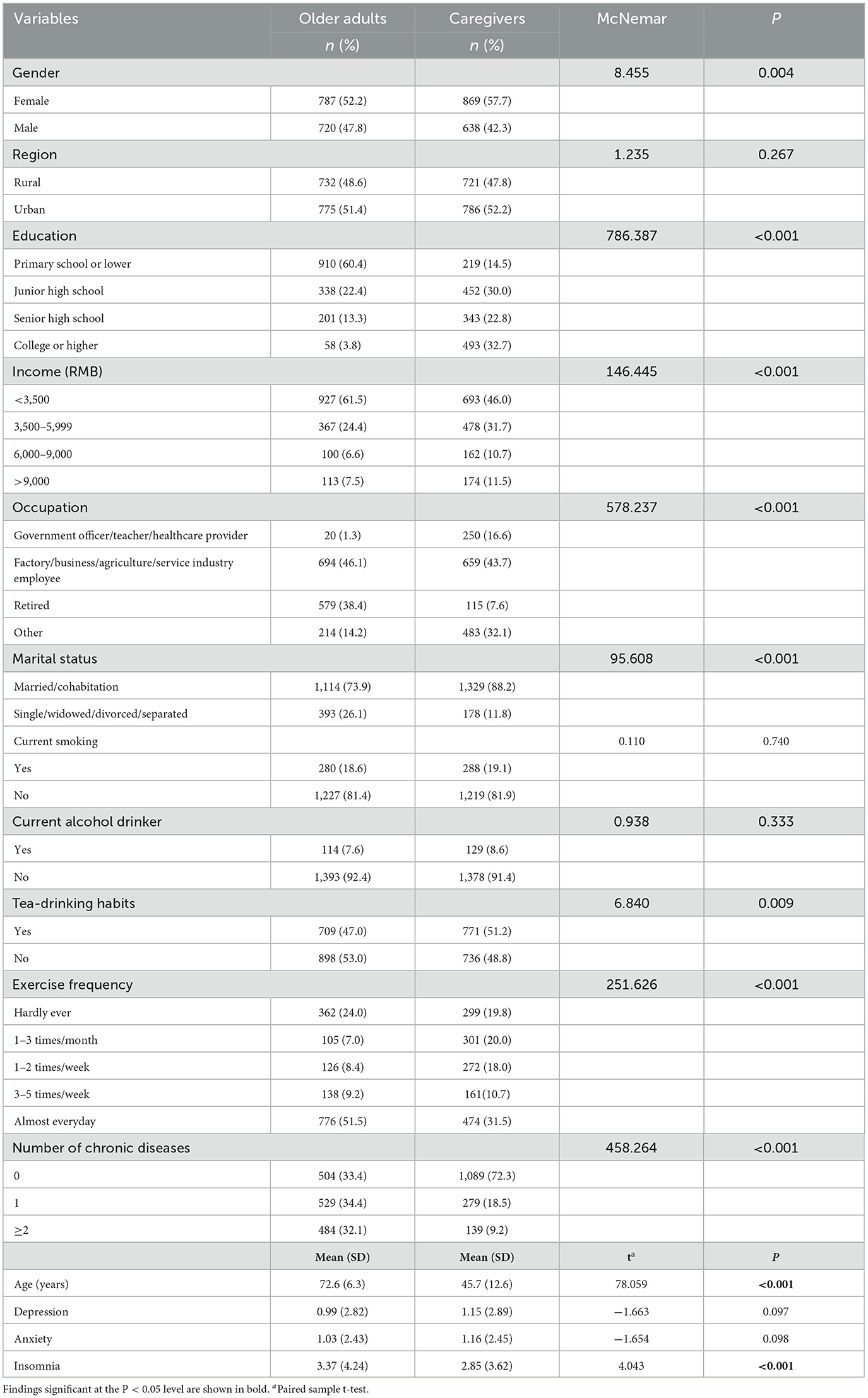
Table 1. Sociodemographic, health related factors and mental health characteristics of older adults and their caregivers (N = 1,507 dyads).
3.2. Bivariate correlations
All bivariate correlations are presented in Table 2. For the older adults, their insomnia was significantly positively correlated to their own depression (r = 0.397, P < 0.001) and anxiety (r = 0.450, P < 0.001), and was also correlated to their caregivers' depression (r = 0.135, P < 0.001) and anxiety (r = 0.167, P < 0.001). In addition, the older adults' depression, anxiety and insomnia were associated with the caregiver's depression (r = 0.238, P < 0.001), anxiety (r = 0.271, P < 0.001), and insomnia (r = 0.247, P < 0.001), respectively. The levels of older adult-caregiver correlation among depression, anxiety, and insomnia were lower than those of intra-subject correlation (r = 0.135 to 0.271 vs. r = 0.397 to 0.587, respectively).
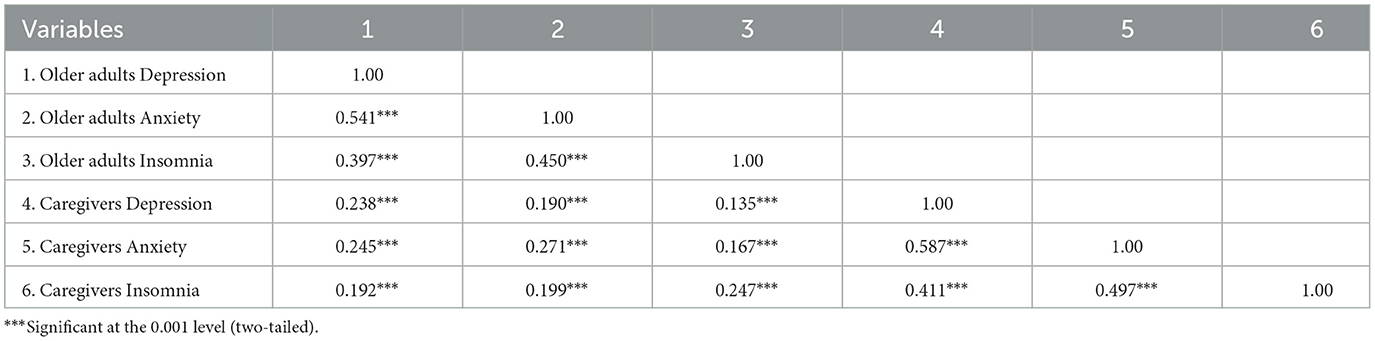
Table 2. Bivariate correlation matrices of depression, anxiety and insomnia for older adults and caregivers (r).
3.3. Actor-partner interdependence models
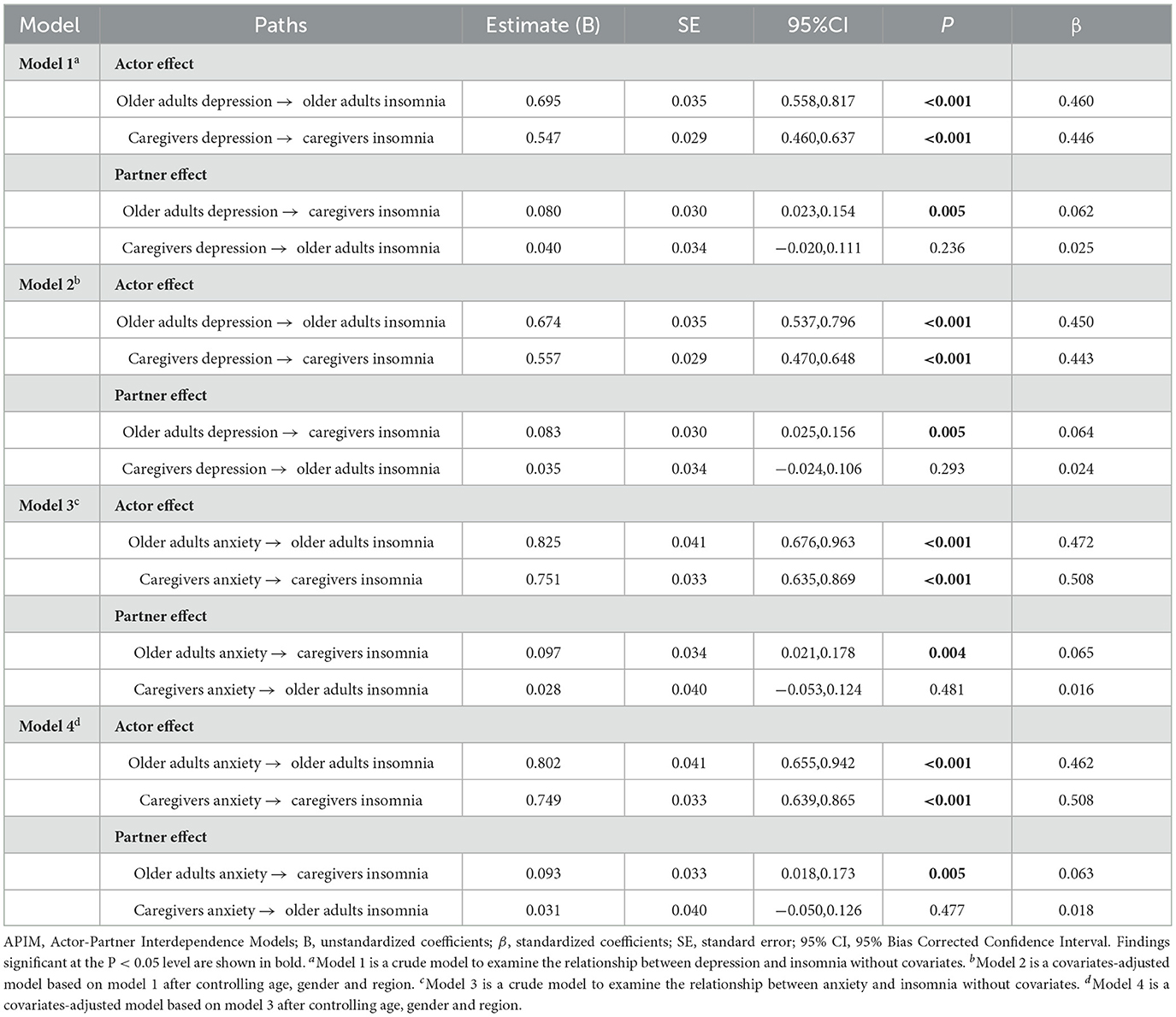
Two hypotheses were examined and four APIMs were established (Table 3). The collective covariates associated with insomnia for the older adults and caregivers contained age, gender and region, which were ultimately considered into our models as control variables to help explain interdependence among older adults and caregivers' insomnia (P < 0.05). Screening results of covariates are shown in Supplementary material (Table S1).
Interdependence among older adults-caregivers dyads' depression and insomnia were explored without adjusting for covariates. Firstly, the overall Chi-square testing of distinguishability was significant ( = 10.377, P = 0.006, CFI = 0.989, GFI = 0.997, RMSEA = 0.053, SRMR = 0.019), indicating that actor and partner effects were statistically distinguished between older adults and their caregivers. Accordingly, dyadic interdependence was further analyzed and illustrated in Figure 1A.
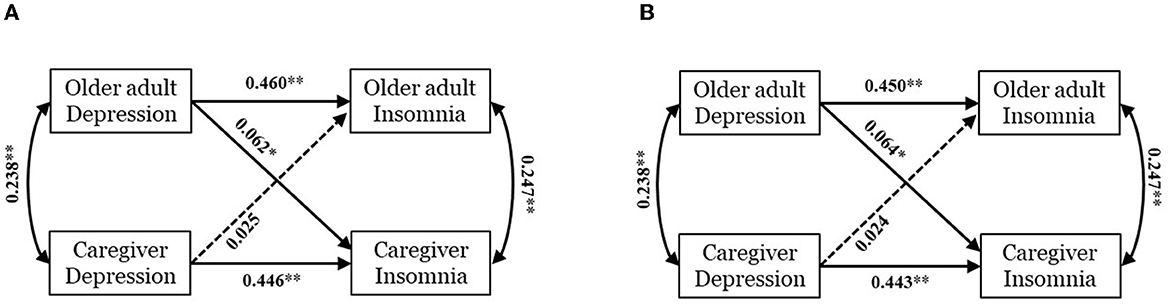
Figure 1. Actor–partner interdependence model of depression and insomnia within older adults-caregivers dyads. Model (A) is a crude model without covariates. Model (B) is an adjusted model controlling age, gender and region. Standardized coefficients (β) are presented on straight lines with single arrow and correlation coefficients are reported on curves with double-headed arrows. A solid line and dotted line represent significant path and non-significant one respectively. *p < 0.01; **p < 0.001.
Older adults' and caregivers' more serious depression was related to their own more serious insomnia (BOlderadults = 0.695, 95% CI: 0.558~0.817, P < 0.001; BCaregivers = 0.547, 95% CI: 0.460~0.637, P < 0.001) and thus significant actor effects were found. In the partner effect, older adults' depression was associated with caregivers' insomnia (B = 0.080, 95% CI: 0.023~0.154, P = 0.005), whereas caregivers' depression was not associated with older adults' insomnia (B = 0.040, 95% CI:−0.020~0.100, P = 0.236).
After adjusting age, gender and region, the APIM performing impact of depression on insomnia was reconstructed as shown in Figure 1B. As with initial crude model (model 1), the actor and partner effects of adjusted model (model 2) were also distinguishable. Two actor effects and one partner effect have been identified: older adults' depression positively impacted their own and caregivers' insomnia (BOlderadults = 0.674, 95% CI: 0.537~0.796, P < 0.001; BCaregivers = 0.557, 95% CI: 0.470~0.648, P < 0.001), while caregivers' depression only had a positive effect on their own insomnia (B = 0.083, 95% CI: 0.025~0.156, P = 0.005), but not on older adults' insomnia (B = 0.035, 95% CI: −0.024~0.106, P = 0.293). More details of APIM results are summarized in Table 3.
We analyzed dyadic interdependence between older adults and caregivers about impact of anxiety on insomnia. The global model also displayed adequate fit ( = 2.653, P = 0.265, CFI = 0.999, GFI = 0.999, RMSEA = 0.015, SRMR = 0.010). Greater older adults' and caregivers' anxiety was significantly correlated to their own greater insomnia (BOlderadults = 0.825, 95% CI: 0.676~0.963, P < 0.001; BCaregivers = 0.751, 95% CI: 0.635~0.869, P < 0.001). Furthermore, partner effect from older adults' anxiety to caregivers' insomnia was observed (B = 0.097, 95% CI: 0.021~0.178, P = 0.004), but corresponding effect from caregivers' anxiety to older adults' insomnia was not found (B = 0.028, 95% CI:−0.053~0.124, P = 0.481). Figure 2A and Table 3 show the coefficients and effects of each path.
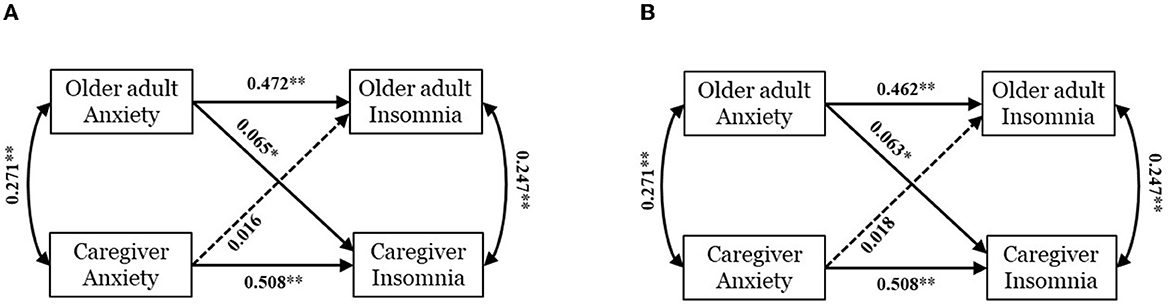
Figure 2. Actor–partner interdependence model of anxiety and insomnia within older adults-caregivers dyads. Model (A) is a crude model without covariates. Model (B) is an adjusted model controlling age, gender and region. Standardized coefficients (β) are presented on straight lines with single arrow and correlation coefficients are reported on curves with double-headed arrows. A solid line and dotted line represent significant path and non-significant one respectively. *p < 0.01; **p < 0.001.
Considering covariates, the adjusted model is depicted in Figure 2B and Table 3. We found two significant actor effects: older adults' and caregivers' anxiety worsen their own insomnia (BOlderadults = 0.802, 95% CI: 0.655~0.942, P < 0.001; BCaregivers = 0.749, 95% CI: 0.639~0.865, P < 0.001), and one partner effect of older adults' anxiety aggravated caregivers' insomnia (B = 0.093, 95% CI: 0.018~0.173, P = 0.005). No partner effect for caregivers' anxiety on older adults' insomnia was identified (B = 0.031, 95% CI: −0.050~0.126, P = 0.477).
4. Discussion
This study added to the evidence on the partner effects of depression and anxiety on insomnia in community-living older adults and their family caregivers in China. We found significant older adults-caregiver associations in depression, anxiety, and insomnia. Specifically, older adults' and caregivers' depression and anxiety had an influence on their own insomnia (actor effects); older adults' depression and anxiety had an influence on caregivers' insomnia (partner effects). Our findings indicate that it is feasible to embed emotional interventions for older adults within family care support services.
We found significant correlations in depression, anxiety and insomnia between older adults and caregivers, representing emotional contagion occurred in the family's environment (43), which is consistent with previous studies on patients with cancer (44). The psychological distress of patients and family caregivers are closely linked (45). These results could be explained by emotional contagion theory, in which emotional state can be transmitted from one person to another through nonverbal communication information during social interactions (46). Secondly, according to the interdependence theory, older adults and family caregivers are in the same social system, and they can influence each other (47). Stay-at-home orders during the COVID-19 outbreak increased family conflict and financial strain (48). Such stress may affect caregivers' sleep. Future study should pay attention to the nature of the interactions between the caregivers and the older adults in family environment other than material supports to older adults.
Consistent with earlier studies (30, 49), we found a significant actor effect of older adults' depression or anxiety on their own insomnia, which fully supports our hypothesis 0. Depression or anxiety in older adults can influence their sleep quality, and this also appears to be the case for caregivers. Present day research considers insomnia as a transdiagnostic symptom for many mental disorders, and it has been found that the relationship between depression and insomnia is bidirectional: people with depression have changes in sleep, and insomnia increases the risk of depression (50). Similar to depression, the APMI showed that more anxiety symptoms were associated with severe insomnia. Previous epidemiological research has shown that people with anxiety have a high prevalence of sleep problems (51). Anxiety is particularly characterized by a state of mental hyperarousal, which can display as a lower wake threshold, increasing the likelihood of sleep disturbance in reaction to external stimuli. Insomnia can be caused by false beliefs, bad sleep habits, somatic hyperarousal, and mental hyperarousal (52). Relaxation techniques used in Cognitive Behavioral Therapy for Insomnia (CBT-I) may help improve anxiety status by reducing hyperarousal (53). The successful use of relaxation techniques in CBT-I demonstrated that insomnia is caused by anxiety in certain extent.
The partial partner effect of depression or anxiety on insomnia was observed in this study: older adults' depression or anxiety had an effect on caregivers' insomnia, while caregivers' depression or anxiety had no effect on older adults' insomnia. Hypothesis 1 was supported and Hypothesis 2 was not supported. This is in line with the results of a previous study of patients and their carers (30). However, a former study in couples found that between-person effect was stronger than the within-person effect, and that anxiety symptoms predicted more aspects of sleep than depression (54). When an individual shared a bed with a partner, anxiety status might increase the risk of waking up, whereas depression, which is a psychomotor retardation, might not produce the same risk of waking up. In the current sample, caregivers are family member of older adults, including spouses, daughters, sons, kins or daughters-in-law. We cannot distinguish family caregivers' relationship to older adults. To remedy this defect of the study design, the covariate age was adjusted in APIM analyses due to the age of the spouse was greater than daughters, sons, kins or daughters-in-law. Though the main results did not change, these results should be viewed with some caution. Future research should focus on caregivers from specific gender group or different relationships, and use methods with better ecological validity and involve longitudinal and causal study designs. One possible reason why caregivers' depression or anxiety did not have a partner effect on older adults' insomnia is the difference in roles. Caregiving activities can disturb caregivers' daily lives, causing physical, emotional and financial stress, and finally consuming their energy (10). We guess, as care recipients, older adults are more likely to be influenced by the reality of caregivers' care activities than by the caregivers' emotions. Therefore, further research is needed to confirm our speculation.
Overall, this study added to the literature on psychological distress and insomnia within the older adults-caregiver dyads, and explored the between-person effects of emotion. Previous studies of psychological distress and insomnia among older adults and caregivers examined unidirectional effects instead of mutual effects in focus. However, care recipients and caregivers have a close relationship and may influence each other through emotional, cognitive and behavioral clues in social interactions, and may eventually affect the health of the caregivers (23, 55). There are several limitations in this study. First, we didn't distinguish the roles of informal family caregivers (spouse caregiver, son caregiver, or daughter caregiver). Second, Selection bias may exist in this study. The general demographics are significantly different between the two groups of older adults. For more information, see the Supplementary material (Table S2). The rest of 2,511 older adults did not report having caregiver or their caregiver declined to participate in this study. Third, the cross-sectional design did not allow us to produce causal relationships. Fourth, the results from the provincial data could not be generalized to the whole country.
5. Conclusion
Psychological distress in older adults may affect the sleep of their caregivers. Healthcare providers should provide mental health services based on family or group interaction. Our findings highlight the need for older adult-caregiver dyad interventions and strategies for managing older adults' emotions in the treatment of insomnia in family caregivers.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Guangdong Provincial People's Hospital, Guangdong Academy of Medical Sciences (Reference number: KY2020-268-01). The patients/participants provided their written informed consent to participate in this study.
Author contributions
K-RD: conceptualization, methodology, formal analysis, investigation, writing-original draft, and writing—review and editing. W-QX: methodology, writing-original draft, and writing—review and editing. Y-YH: formal analysis, investigation, and writing—review and editing. J-HH: writing-review and editing. W-YT: resources and supervision. JL: methodology. C-LH: conceptualization. F-JJ: conceptualization, resources, and supervision. S-BW: conceptualization, methodology, investigation, writing-original draft, and writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Social Science Foundation of China (Grant No. 19ZDA360), the National Natural Science Foundation of China (Grant No. 81803302), and the Guangzhou Science and Technology Plan Project (Grant No. 202002030484). The funding agencies had no role in the design and execution of the study, the collection, management, analysis, and interpretation of the data, or the preparation, review, or approval of the manuscript.
Acknowledgments
Authors thank all participants involved in this study and related workers.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1163867/full#supplementary-material
References
1. National bureau of statistics of China. Communiqué of the Seventh National Population Census (No. 5). (stats.gov.cn) (2021). Available online at: http://www.stats.gov.cn/english/PressRelease/202105/t20210510_1817190.html (accessed October 08, 2022).
2. Hu D, Yan W, Zhu J, Zhu Y, Chen J. Age-related disease burden in China, 1997-2017: findings from the global burden of disease study. Front Public Health. (2021) 9:638704. doi: 10.3389/fpubh.2021.638704
3. Volkert J, Schulz H, Härter M, Wlodarczyk O, Andreas S. The prevalence of mental disorders in older people in Western countries-a meta-analysis. Ageing Res Rev. (2013) 12:339–53. doi: 10.1016/j.arr.2012.09.004
4. Polyakova M, Sonnabend N, Sander C, Mergl R, Schroeter ML, Schroeder J, et al. Prevalence of minor depression in elderly persons with and without mild cognitive impairment: a systematic review. J Affect Disord. (2014) 152–4:28–38. doi: 10.1016/j.jad.2013.09.016
5. Riedel-Heller SG, Busse A, Angermeyer MC. The state of mental health in old-age across the 'old' European Union– a systematic review. Acta Psychiatr Scand. (2006) 113:388–401. doi: 10.1111/j.1600-0447.2005.00632.x
6. Siu PM, Yu AP, Tam BT, Chin EC, Yu DS, Chung KF, et al. Effects of tai chi or exercise on sleep in older adults with insomnia: a randomized clinical trial. JAMA Netw Open. (2021) 4:e2037199. doi: 10.1001/jamanetworkopen.2020.37199
7. Lou VW, Ng JW. Chinese older adults' resilience to the loneliness of living alone: a qualitative study. Aging Ment Health. (2012) 16:1039–46. doi: 10.1080/13607863.2012.692764
8. Luo J, Zhou Y, Liu H, Hu J. Factors related to the burden of family caregivers of elderly patients with spinal tumours in Northwest China. BMC Neurol. (2020) 20:69. doi: 10.1186/s12883-020-01652-0
9. Chen S, Cui Y, Ding Y, Sun C, Xing Y, Zhou R, et al. Prevalence and risk factors of dysphagia among nursing home residents in eastern China: a cross-sectional study. BMC Geriatr. (2020) 20:352. doi: 10.1186/s12877-020-01752-z
10. Pinquart M, Sörensen S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: a meta-analysis. J Gerontol B Psychol Sci Soc Sci. (2003) 58:P112–28. doi: 10.1093/geronb/58.2.P112
11. Carriedo A, Cecchini JA, Fernandez-Rio J, Méndez-Giménez A. COVID-19, psychological well-being and physical activity levels in older adults during the nationwide lockdown in Spain. Am J Geriatr Psychiatry. (2020) 28:1146–55. doi: 10.1016/j.jagp.2020.08.007
12. Chiu MYL, Leung CLK, Li BKK, Yeung D, Lo TW. Family caregiving during the COVID-19 pandemic: factors associated with anxiety and depression of carers for community-dwelling older adults in Hong Kong. BMC Geriatr. (2022) 22:125. doi: 10.1186/s12877-021-02741-6
13. Guo Y, Cheng C, Zeng Y, Li Y, Zhu M, Yang W, et al. Mental health disorders and associated risk factors in quarantined adults during the COVID-19 outbreak in China: cross-sectional study. J Med Internet Res. (2020) 22:e20328. doi: 10.2196/20328
14. Grolli RE, Mingoti MED, Bertollo AG, Luzardo AR, Quevedo J, Réus GZ, et al. Impact of COVID-19 in the mental health in elderly: psychological and biological updates. Mol Neurobiol. (2021) 58:1905–16. doi: 10.1007/s12035-020-02249-x
15. Li Q, Zhang H, Zhang M, Li T, Ma W, An C, et al. Mental health multimorbidity among caregivers of older adults during the COVID-19 epidemic. Am J Geriatr Psychiatry. (2021) 29:687–97. doi: 10.1016/j.jagp.2021.01.006
16. Ivziku D, Clari M, Piredda M, De Marinis MG, Matarese M. Anxiety, depression and quality of life in chronic obstructive pulmonary disease patients and caregivers: an actor-partner interdependence model analysis. Qual Life Res. (2019) 28:461–72. doi: 10.1007/s11136-018-2024-z
17. Gustavsson-Lilius M, Julkunen J, Keskivaara P, Lipsanen J, Hietanen P. Predictors of distress in cancer patients and their partners: the role of optimism in the sense of coherence construct. Psychol Health. (2012) 27:178–95. doi: 10.1080/08870446.2010.484064
18. Bouchard K, Gareau A, Gallant NL, Lalande K, Greenman PS, Sztajerowska K, et al. Dyadic effects of anxiety and depression on quality of life among couples facing cardiovascular disease. J Psychosom Res. (2021) 149:110601. doi: 10.1016/j.jpsychores.2021.110601
19. Kayaalp A, Page KJ, Rospenda KM. Caregiver burden, work-family conflict, family-work conflict, and mental health of caregivers: a mediational longitudinal study. Work Stress. (2021) 35:217–40. doi: 10.1080/02678373.2020.1832609
20. Pristavec T. The burden and benefits of caregiving: a latent class analysis. Gerontologist. (2019) 59:1078–91. doi: 10.1093/geront/gny022
21. Simpson C, Carter P. Dementia behavioural and psychiatric symptoms: effect on caregiver's sleep. J Clin Nurs. (2013) 22:3042–52. doi: 10.1111/jocn.12127
22. Liu S, Li C, Shi Z, Wang X, Zhou Y, Liu S, et al. Caregiver burden and prevalence of depression, anxiety and sleep disturbances in Alzheimer's disease caregivers in China. J Clin Nurs. (2017) 26:1291–300. doi: 10.1111/jocn.13601
23. Lin IF, Fee HR, Wu HS. Negative and positive caregiving experiences: a closer look at the intersection of gender and relatioships. Fam Relat. (2012) 61:343–58. doi: 10.1111/j.1741-3729.2011.00692.x
24. Kok RM, Reynolds CF 3rd. Management of depression in older adults: a review. JAMA. (2017) 317:2114–22. doi: 10.1001/jama.2017.5706
25. Chen CT, Tung HH, Fang CJ, Wang JL, Ko NY, Chang YJ, et al. Effect of music therapy on improving sleep quality in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. (2021) 69:1925–32. doi: 10.1111/jgs.17149
26. Felipe SGB, Oliveira CES, Silva C, Mendes PN, Carvalho KM, Lopes Silva-Júnior F, et al. Anxiety and depression in informal caregivers of dependent elderly people: an analytical study. Rev Bras Enferm. (2020) 73:e20190851. doi: 10.1590/0034-7167-2019-0851
27. Alberts NM, Hadjistavropoulos HD, Pugh NE, Jones SL. Dementia anxiety among older adult caregivers: an exploratory study of older adult caregivers in Canada. Int Psychogeriatr. (2011) 23:880–6. doi: 10.1017/S1041610211000299
28. Troxel WM. It's more than sex: exploring the dyadic nature of sleep and implications for health. Psychosom Med. (2010) 72:578–86. doi: 10.1097/PSY.0b013e3181de7ff8
29. Terrone G, Mangialavori S, Lanza di Scalea G, Cantiano A, Temporin G, Ducci G, et al. The relationship between dyadic adjustment and psychiatric symptomatology in expectant couples: an actor-partner interdependency model approach. J Affect Disord. (2020) 273:468–75. doi: 10.1016/j.jad.2020.05.040
30. Chan JSM, Yu NX, Chow AYM, Chan CLW, Chung KF, Ho RTH, et al. Dyadic associations between psychological distress and sleep disturbance among Chinese patients with cancer and their spouses. Psychooncology. (2017) 26:856–61. doi: 10.1002/pon.4240
31. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
32. Chen S, Chiu H, Xu B, Ma Y, Jin T, Wu M, et al. Reliability and validity of the PHQ-9 for screening late-life depression in Chinese primary care. Int J Geriatr Psychiatry. (2010) 25:1127–33. doi: 10.1002/gps.2442
33. Chin WY, Choi EP, Chan KT, Wong CK. The psychometric properties of the center for epidemiologic studies depression scale in Chinese primary care patients: factor structure, construct validity, reliability, sensitivity and responsiveness. PLoS ONE. (2015) 10:e0135131. doi: 10.1371/journal.pone.0135131
34. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
35. Zhou Y, Xu J, Rief W. Are comparisons of mental disorders between Chinese and German students possible? an examination of measurement invariance for the PHQ-15, PHQ-9 and GAD-7. BMC Psychiatry. (2020) 20:480. doi: 10.1186/s12888-020-02859-8
36. Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. (2011) 34:601–8. doi: 10.1093/sleep/34.5.601
37. Michaud AL, Zhou ES, Chang G, Recklitis CJ. Validation of the Insomnia Severity Index (ISI) for identifying insomnia in young adult cancer survivors: comparison with a structured clinical diagnostic interview of the DSM-5 (SCID-5). Sleep Med. (2021) 81:80–5. doi: 10.1016/j.sleep.2021.01.045
38. Smith MT, Wegener ST. Measures of sleep: the insomnia severity index, Medical Outcomes Study (MOS) sleep scale, Pittsburgh Sleep Diary (PSD), and Pittsburgh Sleep Quality Index (PSQI). Arthr Care Res. (2003) 49:S184–96. doi: 10.1002/art.11409
39. Yu DS. Insomnia Severity Index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs. (2010) 66:2350–9. doi: 10.1111/j.1365-2648.2010.05394.x
40. Huang J, Duan Z, Wang Y, Redmon PB, Eriksen MP. Use of Electronic Nicotine Delivery Systems (ENDS) in China: evidence from citywide representative surveys from five Chinese cities in 2018. Int J Environ Res Public Health. (2020) 17:2541. doi: 10.3390/ijerph17072541
41. Beer P, Mulder RH. The effects of technological developments on work and their implications for continuous vocational education and training: a systematic review. Front Psychol. (2020) 11:918. doi: 10.3389/fpsyg.2020.00918
42. Fortin M, Stewart M, Poitras ME, Almirall J, Maddocks H. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med. (2012) 10:142–51. doi: 10.1370/afm.1337
43. Wróbel M, Imbir KK. Broadening the perspective on emotional contagion and emotional mimicry: the correction hypothesis. Perspect Psychol Sci. (2019) 14:437–51. doi: 10.1177/1745691618808523
44. Segrin C, Badger TA, Sikorskii A, Pasvogel A, Weihs K, Lopez AM, et al. Longitudinal dyadic interdependence in psychological distress among Latinas with breast cancer and their caregivers. Support Care Cancer. (2020) 28:2735–43. doi: 10.1007/s00520-019-05121-4
45. Díaz-Cordobés JL, Pérez M, Soto-Rubio A. COPD at the end of life: predictors of the emotional distress of patients and their family caregivers. PLoS ONE. (2020) 15:e0240821. doi: 10.1371/journal.pone.0240821
46. Hatfield E, Cacioppo JT, Rapson RL. Emotional contagion. Curr Dir Psychol Sci. (1993) 2:96–100. doi: 10.1017/CBO9781139174138
47. Rusbult CE, Van Lange PA. Interdependence, interaction, and relationships. Annu Rev Psychol. (2003) 54:351–75. doi: 10.1146/annurev.psych.54.101601.145059
48. Freisthler B, Gruenewald PJ, Tebben E, Shockley McCarthy K, Price Wolf J. Understanding at-the-moment stress for parents during COVID-19 stay-at-home restrictions. Soc Sci Med. (2021) 279:114025. doi: 10.1016/j.socscimed.2021.114025
49. Otto AK, Gonzalez BD, Heyman RE, Vadaparampil ST, Ellington L, Reblin M. Dyadic effects of distress on sleep duration in advanced cancer patients and spouse caregivers. Psychooncology. (2019) 28:2358–64. doi: 10.1002/pon.5229
50. Riemann D, Krone LB, Wulff K, Nissen C. Sleep, insomnia, and depression. Neuropsychopharmacology. (2020) 45:74–89. doi: 10.1038/s41386-019-0411-y
51. Chellappa SL, Aeschbach D. Sleep and anxiety: from mechanisms to interventions. Sleep Med Rev. (2022) 61:101583. doi: 10.1016/j.smrv.2021.101583
52. Molen YF, Carvalho LB, Prado LB, Prado GF. Insomnia: psychological and neurobiological aspects and non-pharmacological treatments. Arq Neuropsiquiatr. (2014) 72:63–71. doi: 10.1590/0004-282X20130184
53. Chan NY, Chan JWY, Li SX, Wing YK. Non-pharmacological approaches for management of insomnia. Neurotherapeutics. (2021) 18:32–43. doi: 10.1007/s13311-021-01029-2
54. Walters EM, Phillips AJ, Hamill K, Norton PJ, Drummond SP. Anxiety predicts dyadic sleep characteristics in couples experiencing insomnia but not in couples without sleep disorders. J Affect Disord. (2020) 273:122–30. doi: 10.1016/j.jad.2020.04.031
Keywords: depression, anxiety, insomnia, older adults, actor-partner interdependence model
Citation: Ding K-R, Xu W-Q, He Y-Y, Hu J-H, Tan W-Y, Liao J, Hou C-L, Jia F-J and Wang S-B (2023) Depression, anxiety and insomnia in Chinese older adults and their family caregivers during the COVID-19 pandemic: an actor-partner interdependence model approach. Front. Public Health 11:1163867. doi: 10.3389/fpubh.2023.1163867
Received: 11 February 2023; Accepted: 12 June 2023;
Published: 27 June 2023.
Edited by:
Naseem Akhtar Qureshi, Al-Falah University, IndiaReviewed by:
Birsen Altay, Ondokuz Mayis University, TürkiyeMing Zhang, Third Affiliated Hospital of Sun Yat-sen University, China
Sujata Sethi, Pandit Bhagwat Dayal Sharma University of Health Sciences, India
Copyright © 2023 Ding, Xu, He, Hu, Tan, Liao, Hou, Jia and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shi-Bin Wang, spiriorwang@126.com; Fu-Jun Jia, jiafujun@gdph.org.cn
†These authors have contributed equally to this work
 Kai-Rong Ding
Kai-Rong Ding Wen-Qi Xu
Wen-Qi Xu Yong-Yi He1,2
Yong-Yi He1,2 Jia-Hui Hu
Jia-Hui Hu Jing Liao
Jing Liao Cai-Lan Hou
Cai-Lan Hou Shi-Bin Wang
Shi-Bin Wang