- 1Department of Physical Education, Southeast University, Nanjing, China
- 2China Volleyball College, Beijing Sport University, Beijing, China
- 3Department of Physical Education, Tangshan Normal University, Tangshan, China
- 4School of Rehabilitation, Sport and Psychology, AECC University College, Bournemouth, United Kingdom
- 5Institute for Health and Sport, Victoria University, Melbourne, VIC, Australia
- 6Institute of Physiotherapy and Rehabilitation Sciences, Peoples University of Medical and Health Sciences for Women, Nawabshah, Pakistan
- 7Health and Exercise Science Laboratory, Institute of Sports Science, Seoul National University, Seoul, South Korea
- 8Physical Education Unit, School of Humanities and Social Science, The Chinese University of Hong Kong-Shenzhen, Shenzhen, China
- 9Department of Physical Education Teaching, Shanghai Sanda University, Shanghai, China
- 10Exercise Psychophysiology Laboratory, Institute of KEEP Collaborative Innovation, School of Psychology, Shenzhen University, Shenzhen, China
Objective: The purpose of this research was to investigate the prevalence of lifestyle behaviors and suicide-related behaviors and the association between them using a nationally representative sample of adolescents from the USA.
Methods: 13,677 high school students aged 14-18 years were included in this cross-sectional study. The research data were retrieved from the Youth Risk Behavior Surveillance System Survey in 2019. All data on age, sex, grade, race, physical activity, television time, fruit intake, and suicide-related behavior were self-reported by students. Logistic regression models were adopted to examine the association between lifestyle behaviors and the suicide-related behaviors.
Results: Students who played video/computer games for ≥2 h had higher risk of suicide attempt (OR = 1.55, 95%CI: 1.30-1.85). Daily sleep duration of ≤8 h was positively associated with considering a suicide attempt (OR = 1.99, 95%CI: 1.62-2.43). In addition, participants who did not engage in any sport team were more likely to report considering a suicide attempt (OR = 1.50, 95%CI: 1.24-1.81).
Conclusion: This research suggests that some lifestyle behaviors (e.g., time for video or computer use, sleep duration, sports team participation, regular breakfast intake, and substance use) are associated with increased risk of suicidal behavior and ideation in high school students. To identify the specific effect of multiple lifestyle factors in influencing the risk of suicide-related behaviors in high school students, longitudinal studies are warranted in future.
Introduction
The World Health Organization (WHO) data suggests that suicide has become one of the major global public health issues. Suicide has become the fourth leading cause of death among adolescents aged between 15 and 19 years (1). A study undertaken in the United States of America (USA) showed that there was an increase by 24% in the rate of suicide from 1999 to 2014 (2). The most recent WHO data from 2019 reveals that globally over 700,000 individuals commit suicide every year (1). The loss of life not only affects the families and communities but also places the burden of care for those left behind on the healthcare system. For example, a recent study by Shepard et al. (3) indicated that suicide-related costs (including suicide attempts) in the United States had reached approximately $94 billion (3). Furthermore, the estimated economic costs of youth suicide in Australia was about $AUD 500 million. To this end, effective suicide prevention strategy is urgently needed.
The physiological and psychological mechanisms that explain why individuals commit suicide still remain largely unknown (4). Recently, researchers have investigated the relationship of different modifiable risk factors, including physical activity (PA), sedentary behavior (e.g., video game or TV watching), adequate sleep duration, and sufficient nutrition with suicide-related behaviors (e.g., considering suicide, attempted suicide, and having a suicide plan). A recent meta-analytical review (5, 6) indicated an association between higher PA levels and lower suicidal ideation (7). Even low levels of PA was found to be associated with a lower risk for suicidal ideation (8). In contrast, sedentary adolescents have been found to have a greater risk for indulging in suicide-related behaviors (9, 10). In addition, other modifiable lifestyle behaviors including sleep duration, dietary habits (e.g., breakfast, fruit, and milk) (9, 11), and substance use (12, 13) have been studied in relation to suicide-related behaviors.
The above-mentioned lifestyle behaviors (e.g., PA, sedentary behavior, sleep duration, and/or dietary habits) have been shown to be associated with suicide-related behaviors, but the majority of previous studies have focused on one or two lifestyle behaviors or low-to-middle income countries, limiting researchers' comprehensive understanding of the associations between lifestyle behaviors and suicide-related behaviors. For example, a lifestyle study indicated that harmful consumption, sedentary behavior, and sexual risk behaviors were associated with the increased risk of suicide attempt among Namibia adolescents (14). It could be argued that multiple lifestyle behaviors act together and are likely to affect suicide-related behaviors. In addition, previous studies included multiple lifestyle behaviors, but outcomes of interest were depression, anxiety, and/or sleep quality (15, 16). Thus, investigation of associations between suicide-related behaviors and multiple lifestyle behaviors is required. To carry out timely and effective prevention strategies before suicide-related behaviors emerge, it is important to identify relevant multiple modifiable lifestyle factors associated with suicidal tendencies. Therefore, the aim of this study was to examine the prevalence of lifestyle behaviors and suicidal outcomes and the association between them in a nationally representative sample of adolescents from the USA.
Methods
Study Design and Participants
Data was retrieved from a project entitled the “Youth Risk Behavior Surveillance System (YRBS).” This biennially conducted project was designed by the Centre for Disease Control (CDC), USA, to track how risk behaviors change over time among high-school students. The YRBS survey was approved by the Institutional Review Board of the CDC. The sampling process consisted of three stages through which 9-12 grade students (14-18 years of age) from regular public school, parochial, and other non-public schools across the USA were approached for participation. The first-stage sampling frame comprised 1,257 primary sampling units (PSUs). The 1,257 PSUs were categorized into 16 strata. Among the 1,257 PSUs, 54 were sampled with probability proportional to overall school enrollment size for that PSU. For the second-stage sampling, secondary sampling units (SSUs) were defined as a physical school with grades 9–12 or a school created by combining nearby schools to provide all four grades. From the 54 PSUs, 162 SSUs were sampled with probability proportional to school enrollment size. To provide adequate coverage of students in small schools, an additional 15 small SSUs were selected from a subsample of 15 PSUs from the 54 PSU sample. These 177 SSUs corresponded to 184 physical schools. The third stage of sampling comprised random sampling of one or two classrooms in each of grades 9–12 from either a required subject (e.g., English or social studies) or a required period (e.g., homeroom or second period). All students in sampled classes were eligible to participate. Schools, classes, and students who refused to participate were not replaced in the sampling design. Data collected in 2019 included 13,872 participants from 136 schools invited to participate in the survey. Of these, 13,677 provided valid data for the final analysis. The overall response rate of the 2019 YRBS survey was 60.3%, calculated by multiplying school response rate (75.1%) with the student response rate (80.3%). Weighting for non-response and oversampling of minority students was carried out for each participant based on gender, ethnicity, and grade. A weight based on student sex, race/ethnicity, and grade was applied to each record to adjust for school and student non-response and oversampling of black and Hispanic students. The overall weights were scaled so that the weighted count of students equals the total sample size, and the weighted proportions of students in each grade match the national population proportions. Therefore, weighted estimates are nationally representative of all students in grades 9–12 attending U.S. public and private schools. The detailed sampling strategy is described in a previous study (17).
YRBS Procedures
The YRBS survey was conducted at the targeted schools where informed consent was obtained and the legal guardian or parents signed the consent form. The participants were asked to respond to the computer-scannable questionnaire with assistance of trained data collectors. All procedures of the survey were designed based on the personal privacy protection, encouraging anonymous and voluntary participation, and all the study participants were informed about the research aims and given instructions prior to the formal survey.
Measures
Independent Variables (Lifestyle Behaviors)
In the current study, physical activity (including muscle strengthening exercise, sport team participation), television viewing, video [or computer games] use, sleep duration, physical education, fruit intake, vegetable intake, milk consumption, eating breakfast, and substance use (including current alcohol use and smoking) were included as independent variables. The details of measures used to assess lifestyle behaviors are available in Supplementary Table 1.
Outcome Variables (Suicide-Related Behaviors)
Three suicide-related behaviors (i.e., considered attempting suicide, planned suicide, and attempted suicide) were included in the current study. Considered attempting suicide was asked through a question with dichotomous answer (yes or no): “During the past 12 months, did you ever seriously consider attempting suicide?”; planned suicide was confirmed through the question (with yes or no responses): “During the past 12 months, did you make a plan about how you would attempt suicide?”; and attempted suicide was confirmed from the question “During the past 12 months, how many times did you actually attempt suicide?” with responses ranging from 0 to 6 or more times. For attempted suicide, study participants answering 0 times were considered as no suicide attempt.
Control Variables (Demographic Factors)
Study participants reported their demographic characteristics, including sex (female or male), age (ranging from ≤12 to ≥18 years), grade (from 9th to 12th), race (white, African American, Hispanic/Latino or all other races). Likewise, participants self-reported their height (feet and inches) and weight (pounds) on a paper-based questionnaire, which were used to calculate body mass index so that overweight or obesity status could be determined. All these variables were considered as confounding variables during statistical analysis.
Statistical Analysis
Following the YRBS protocol, all the statistical analysis were performed after taking the complex sampling design into account to estimate nationally representative results of included variables. Missing data were not imputed. The statistical analysis was performed using SPSS v26.0. All the variables were treated as categorical ones; thus, descriptive statistics (percentage, %) were calculated to report the characteristics of the study sample (Supplementary Table 1). The weighted percentage of each variable was also reported with 95% confidence interval. Binary logistic regression was utilized to assess associations of lifestyle behaviors with suicidal outcomes while controlling for sex, age, grade, race, overweight and obesity. In the models, those reporting no for the outcome variable were considered the reference group, whereas the reference group for each independent variable was as follows: sufficient physical activity (yes), television watching hours (≤2 h per day), played video or computer games or used a computer (≤2 h per day), sleep duration was >8 h per night (yes), physical education attendance for at least 1 day (yes), muscle strengthening exercise for at least three times a week (yes), participation in team sports for at least one team (yes), do not eat fruit (no), not eat vegetable (no), do not eat breakfast (no), do not drink milk (no), currently use alcohol (no), and currently smoking (no). The odds ratios with 95%CI were calculated to assess the associations of lifestyle behaviors with the suicidal outcomes. The above statistical analysis was performed using the Complex Sample Module of the SPSS. Statistical significance was set as p < 0.05.
Results
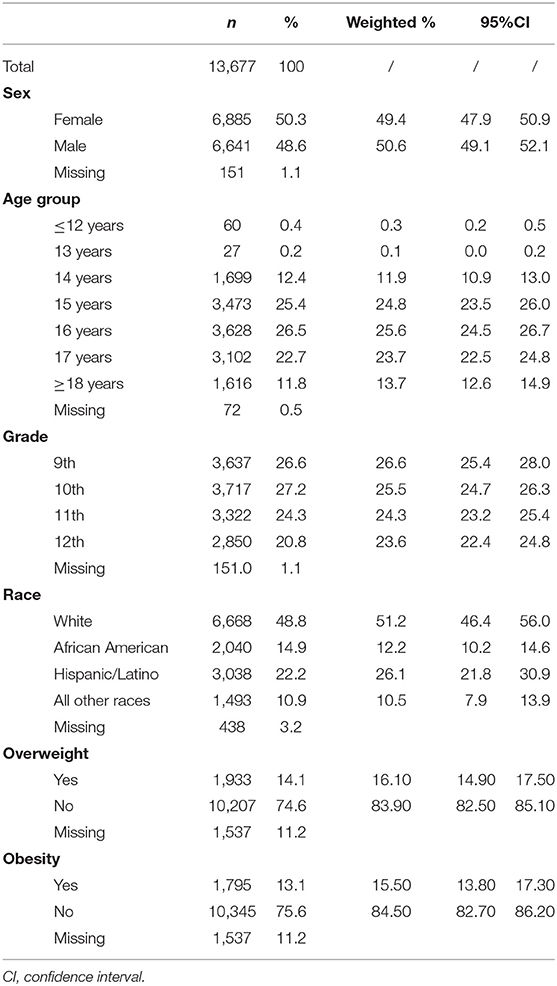
Participant characteristics are shown in Table 1. Of the 13,677 participants, 50.3% were female. The age range 15-17 years made up the majority of the participants (74.6%). The proportions of 9th, 10th, 11th, and 12th grade students were 26.6, 27.2, 24.3, and 20.8%, respectively. The proportion of White was highest across all the race groups (48.8%). The prevalence of overweight (14.4%) and obesity (13.1%) were relatively equal.
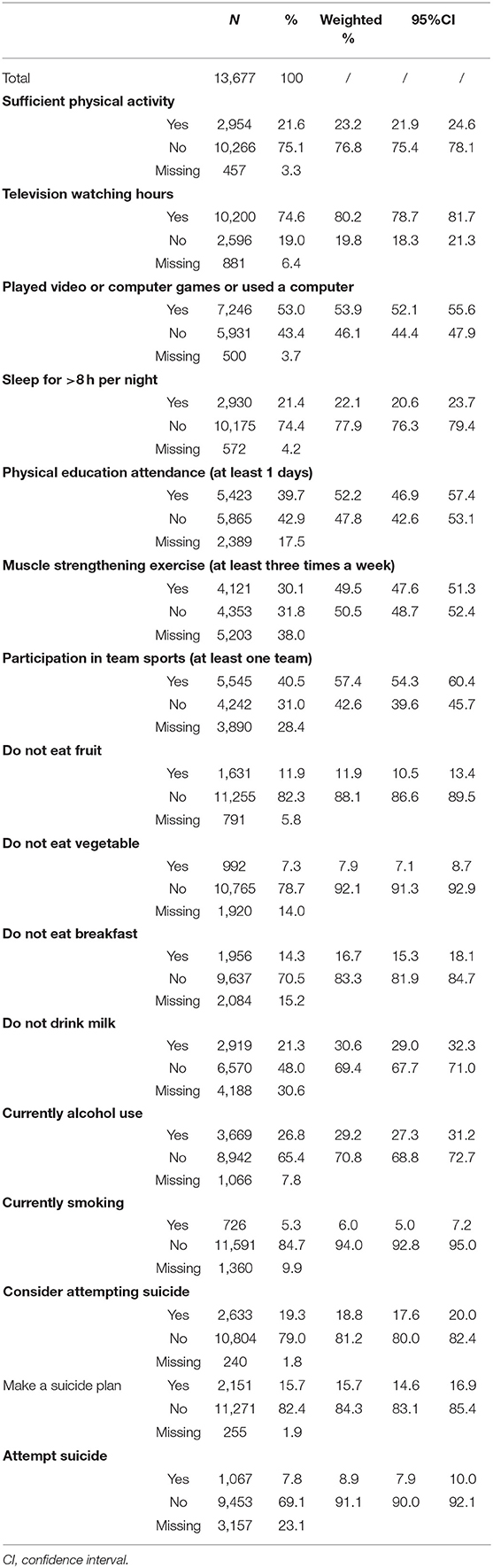
Weighted results of lifestyle behaviors are presented in Table 2. Only 21.6% of the participants reached the sufficient level of physical activity. Television viewing and use of video/computer games for <2 h per day accounted for 74.6 and 53.0% of the participants, respectively. Only 21.4 % of the participants slept for >8 h per night. Attendance of physical education for at least 1 day was reported by 39.7% participants. Moreover, 30.1% of the participants engaged for >3 days in muscle strengthening exercise. Over two-fifths of the participants participated in at least one sport team. The prevalence of participants who did not eat/drink fruit, vegetable, breakfast and milk were 11.9, 7.3, 14.3, and 21.3%, respectively. Current alcohol use was reported by 26.8% of participants and current smoking by 5.3%.
Table 3 presents information on the associations of lifestyles behaviors with each outcome: consider attempting suicide, make a suicide plan and attempt suicide. Significant results were only observed in terms of video/computer games, sleep duration, sport team participation, eating/drinking behaviors (breakfast, alcohol use, and smoking). Specifically, participants who played video/computer games for ≥2 h were more likely to report considering a suicide attempt (OR = 1.55, 95%CI: 1.30-1.85). Daily sleep duration of ≤8 h was positively associated with considering a suicide attempt (OR = 1.99, 95%CI: 1.62-2.43). In addition, participants who did not engage in any sport team were more likely to report considering a suicide attempt (OR = 1.50, 95%CI: 1.24-1.81). Further, participants with an eating habit of no breakfast, current alcohol use and smoking habit had higher odds for considering a suicide attempt. Similar associations were found for other outcomes (i.e., suicidal plan and attempt suicide).
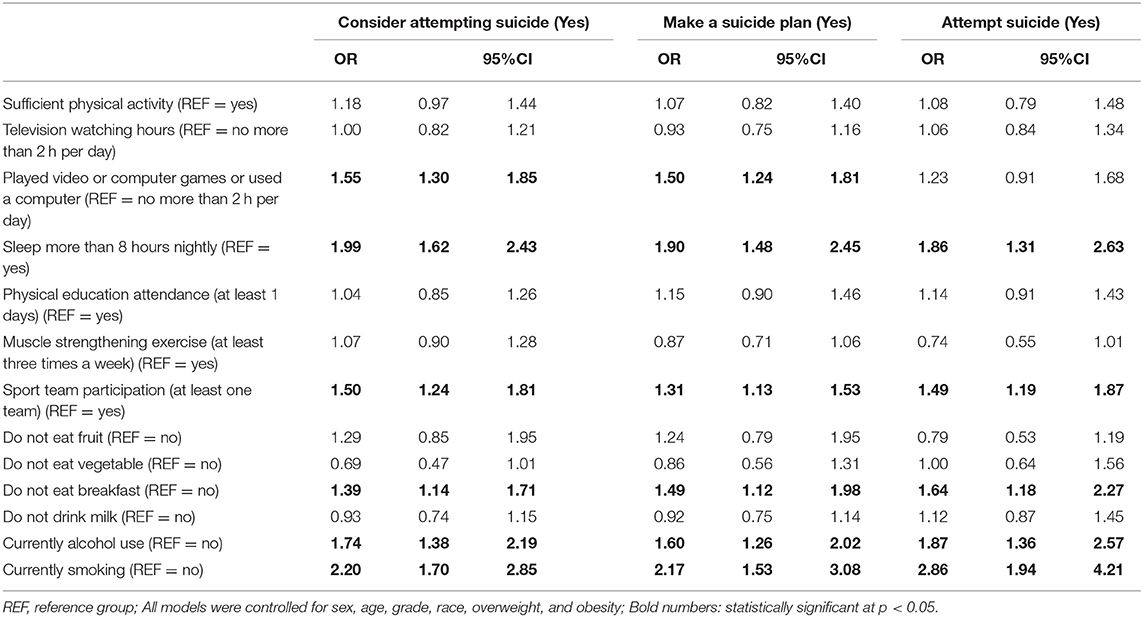
Table 3. Factors associated with suicide-related behaviors (consider attempting suicide, make a suicide plan and attempt suicide).
Discussion
The current study was designed to investigate the prevalence and lifestyle correlates of suicide-related behaviors, which include suicidal consideration, suicidal plan, and suicidal attempt, using a nationally representative sample of US adolescents. The findings of the current study show that spending time on video or computer games (>2 h per day), insufficient nocturnal sleep (<8 h per day), and sport team participation (<1 team) were positively associated with higher risks of three suicide-related behaviors in adolescents, while sufficient PA was not correlated with suicide-related behaviors. Moreover, no eating/drinking behaviors but eating breakfast was negatively associated with suicide-related behaviors. Excessive substance use (alcohol and smoking use) were risk factors of suicide-related behaviors in adolescents.
To investigate the potential factors that influence suicide-related behaviors, most previous studies have examined only a few lifestyle behaviors (e.g., physical activity, sleep) (8, 18), and have not yet examined others. As such, previous research may offer limited results. In fact, suicide-related behavior is influenced by a multiplicity of risk factors (19), such as physical inactivity, poor sleep (20), sedentary behavior (7), substance abuse (21), and poor diet (11). It is, thus, essential to take these lifestyle factors together to investigate their relationship with suicide-related behaviors. Therefore, our study included additional factors such as participation in team sport, physical education attendance, and muscle strengthening exercise in relation to the suicide-related behaviors. Interestingly, the findings of our study showed that there were no significant associations of physical activity, television watching hours, physical education attendance, muscle strengthening exercise, and diet (e.g., eat fruit, eat vegetables, and drink milk) with suicide-related behavior. One plausible reason for this may be a combination of including other lifestyle behaviors and controlling for personal factors/potential confounders, which in turn attenuates the associations of physical activity, television watching hours, physical education attendance, muscle strengthening exercise and diet behaviors with suicide-related behaviors.
With respect to sleep, our finding was consistent with a previous study (22) which found that insufficient sleep was associated with a higher risk of suicide-related behaviors (e.g., consider suicide, and attempt suicide) among adolescents. One recent cross-sectional study showed a higher risk of suicide-related behaviors in those with insufficient sleep than those without sleep problems (21). It is possible that insufficient sleep may cause a decrease in the frontal lobe function and diminish the executive functions, which form a common pathway to the suicidal tendency in adolescents (23). Besides, insufficient sleep duration may result from poor sleep quality, which in turn is associated with suicide-related behaviors (24). Although sleep interventions have been proposed as potential prevention of suicide risk (25), the underlying mechanisms linking insufficient sleep and suicide-related behaviors among adolescents are still unclear, especially the underlying physiological pathways. Of note, the study could not determine the direction of the association between insufficient sleep and suicide outcomes. An alternative explanation for the significant association found in this study may be that those with suicidal ideas have been affected by negative emotions, which might have disturbed the sleep (26) and lead to insufficient sleep.
It is very common for modern teenagers to use electronic devices. Most students use electronic devices to access the internet and play games. The negative effects caused by improper use of electronic products have attracted many researchers' interest, who have found that playing games can result in psychological problems, which eventually leads to suicide-related behaviors among adolescents (27, 28). For instance, Rostad et al. found that excessive media use is associated with an increased risk of suicide-related behaviors among high school students (29). Overall, our findings have added to existing knowledge, indicating an association between the screen-based risk factors (watching videos, computer games, or computer use) and suicide-related behaviors. As the direction could not be determined in this study, prospective studies are needed to examine the relationships between screen-based behaviors and suicide-related behaviors.
The protective effects of sport participation on suicide-related behaviors have been indicated in the previous literature. Participation in team sports (at least one team) was associated with a lower risk of suicide-related behaviors in the present study, as observed in previous studies on adolescents (30, 31). The mechanism by which participation in sports reduces the risk of the three suicide-related behaviors is not yet clear. However, it could be argued that adolescents who engage in the sport can have chances to establish positive social relationships with participants of the activity (32). Adolescents with strong social support generally show higher resilience, less hopelessness, and a lower risk of suicide (30). As team sports participation has been one of the relatively prevalent forms of PA among adolescents in the USA, encouraging their participation in team sports is a feasible approach to reduce suicide-related behaviors. However, as this data was based on adolescents from the USA, future research should examine the associations between team sports participation and suicide-related behaviors in adolescents from other countries. Interestingly, the current study found that no association between PA and suicide-related behaviors in adolescents, which is inconsistent with previous studies using data from prior YRBS surveys (9, 33). A possible reason for this finding is that several lifestyle behaviors examined in the current study offset the independent effect of PA on suicide-related behaviors in adolescents.
Compared with eating breakfast, not eating breakfast was positively associated with a higher risk of suicide-related behaviors in adolescents. This finding indicates that eating breakfast might play a role in reducing the risks of suicide-related behaviors and ideation in adolescents. Although the existing literature has fewer studies on the role of breakfast on suicide-related behaviors, the association between not eating breakfast and higher risks for suicide-related behaviors and ideation can still be supported by the limited evidence (9, 34). A possible mechanism linking breakfast consumption with suicide-related behaviors is the positive effect of breakfast consumption on mood. Not eating breakfast is associated with poorer emotions, such as depression (35, 36) or anxiety (36–38), both of which are contributing factors for suicide-related behaviors and ideation in adolescents. Nevertheless, owing to the cross-sectional nature of this study, it is also possible that those with suicidal ideations or attempts may already have been affected by their negative emotions or other life difficulties, so they had low appetite and did not want to eat breakfast.
Current alcohol use and current smoking were two positive correlates of suicide-related behaviors in adolescents in this study. Thus, restricting access for adolescents to alcohol and cigarettes is recommended. Previous studies have suggested that alcohol use and smoking are associated with higher risks for suicide-related behaviors (39). Our research findings were that adolescents with current alcohol use had a greater likelihood of suicidal attempt, plans, and ideation, which agrees with previous evidence. It is well-established that excessive alcohol use is associated with dysfunction of the neuroendocrine system, which subsequently increases the risk for suicide-related behaviors in the general population (39). Concerning the association between smoking and suicide-related behaviors, a few previous studies reported findings similar to the current study. For example, a study of adolescents in Nepal found that smoking was associated with suicidal attempts (40). Similarly, cross-sectional evidence indicated that more smoking was associated with suicidal ideation (41), a suicidal plan (42), and suicidal attempts among Korean adolescents (43). In a meta-analysis, the authors found that smoking is associated with an increased risk of suicide-related behaviors and ideation (44). There are plausible explanations for the associations between smoking and suicide-related behaviors. One is that smokers have pre-existing conditions that result in higher risks for suicide, alternatively that smoking causes adverse conditions that probably lead to the development of suicidal tendency (45). However, these explanations remain untested. It could also be argued that individuals with suicide-related behaviors (e.g., suicide ideation) may be more likely to engage in drinking or smoking behaviors. While the direction of the association between cigarette smoking and suicide-related behaviors remains unclear, it has been argued that the co-occurance deserves attention (46). From the perspective of public health, the possibility that the use of alcohol and / or cigarettes may contribute to suicide-related behaviors suggests that policies reducing adolescents' exposure to alcohol and cigarette products are needed.
Study Strengths and Limitations
The current study has two strengths. The first one is that we used a nationally representative sample of adolescents, which can increase the generalizability of research findings. Second, we included several lifestyle factors to assess the associations between lifestyle behaviors and suicidal outcomes, after controlling for multiple demographic factors, in order to determine the specific role of each behavior in affecting suicidal tendencies. However, some study limitations should be mentioned. One weakness is that the YRBS survey has a cross-sectional study design, which prevents the possibility of establishing a causal association. Moreover, the use of self-reported measures can be subject to reporting and recall bias due to social desirability. Furthermore, owing to the standardized measurement protocol, each variable in our study was assessed by a single item and the measures may be negatively impacted owing to limited validity and reliability.
Practical Implications
The current study has practical implications guiding suicide-related interventions. Our results indicate the potential importance of lifestyle behaviors for prevention of suicide. This calls for the need to raise public health awareness on promoting healthy lifestyle behaviors of adolescents. The results of our study may also specifically stress the role of changing lifestyle behaviors in preventing suicide. For example, discouraging substance use (including alcoholism and smoking) may be an effective approach to reduce suicide ideation and behavior. Similarly, from the perspective of changing movement behaviors, reducing time for games (video or computer) and encouraging activity through team sports are two potential ways to decrease the risk of suicide-related behaviors. Collectively, considering that the current study did not use a causal inference approach to identify the aforementioned associations, addressing suicide-related behaviors through improving their lifestyle is a potential way that needs more examination.
Conclusion
This study suggests that optimal lifestyle behaviors may have an essential role in preventing suicidal behavior and ideation in adolescents. For example, limiting time for video or computer use, encouraging adequate sleep duration, sport team participation, regular breakfast consumption, and avoiding substance use might be protective factors against suicide-related behaviors. Owing to the study design, longitudinal studies are needed in the future to determine the specific effect of multiple lifestyle factors on reducing the risk of suicide-related behaviors in adolescents.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found at: The data presented in this study are available on request from https://www.cdc.gov/healthyyouth/data/yrbs/index.htm (accessed on July, 23 2021).
Ethics Statement
YRBS survey was approved by the Institutional Review Board of the Centre for Disease Control (CDC), USA. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
XL and GC: conceptualization. XL: methodology, formal analysis, investigation, and writing—original draft preparation. GC and S-TC: validation. YS: resources, supervision, and project administration. All authors: writing—review and editing.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.766972/full#supplementary-material
References
1. Suicide (2021). Available online at: www.who.int/news-room/fact-sheets/detail/suicide (accessed July 23, 2021).
2. Curtin CC, Warner M, Hedegaard H. Increase in suicide in the United States, 1999–2014. NCHS Data Brief. (2016) 23:2021. Available online at: https://www.cdc.gov/nchs/products/databriefs/db241.htm
3. Shepard DS, Gurewich D, Lwin AK, Reed GA, Jr., Silverman MM. Suicide and suicidal attempts in the United States: costs and policy implications. Suicide Life Threat Behav. (2016) 46:352–62. doi: 10.1111/sltb.12225
4. O'Connor RC, Nock MK. The psychology of suicidal behaviour. Lancet Psychiatry. (2014) 1:73–85. doi: 10.1016/S2215-0366(14)70222-6
5. Ati NAL, Paraswati MD, Windarwati HD. What are the risk factors and protective factors of suicidal behavior in adolescents? A systematic review. J Child Adolesc Psychiatr Nurs. (2021) 34:7–18. doi: 10.1111/jcap.12295
6. Wasserman D, Carli V, Iosue M, Javed A, Herrman H. Suicide prevention in childhood and adolescence: a narrative review of current knowledge on risk and protective factors and effectiveness of interventions. Asia Pac Psychiatry. (2021) 13:e12452. doi: 10.1111/appy.12452
7. Vancampfort D, Hallgren M, Firth J, Rosenbaum S, Schuch FB, Mugisha J, et al. Physical activity and suicidal ideation: a systematic review and meta-analysis. J Affect Disord. (2018) 225:438–48. doi: 10.1016/j.jad.2017.08.070
8. Chen ST, Guo T, Yu Q, Stubbs B, Clark C, Zhang Z, et al. Active school travel is associated with fewer suicide attempts among adolescents from low-and middle-income countries. Int J Clin Health Psychol. (2021) 21:100202. doi: 10.1016/j.ijchp.2020.11.001
9. Michael SL, Lowry R, Merlo C, Cooper AC, Hyde ET, McKeon R. Physical activity, sedentary, and dietary behaviors associated with indicators of mental health and suicide risk. Prevent Med Rep. (2020) 19:101153. doi: 10.1016/j.pmedr.2020.101153
10. Silva AFD, Júnior C, Hinnig PF, Lima LRA, Silva DAS. Suicidal behaviors and sedentary lifestyles among adolescents: A cross-sectional epidemiological study in Latin American and Caribbean countries. Clinics. (2020) 75:e2015. doi: 10.6061/clinics/2020/e2015
11. Bryant ZJ. Association of dietary intake with suicidal ideation or suicide attempts in adolescents. (2018) 23:2021. Available online at: https://scholarworks.waldenu.edu/dissertations/5681/
12. Bossarte RM, Swahn MH. The associations between early alcohol use and suicide attempts among adolescents with a history of major depression. Addict Behav. (2011) 36:532–5. doi: 10.1016/j.addbeh.2010.12.031
13. Darvishi N, Farhadi M, Haghtalab T, Poorolajal J. Alcohol-related risk of suicidal ideation, suicide attempt, and completed suicide: a meta-analysis. PLoS ONE. (2015) 10:e0126870. doi: 10.1371/journal.pone.0126870
14. Peltzer K, Pengpid S. Lifestyle and mental health among school-going adolescents in Namibia. J Psychol Africa. (2017) 27:69–73. doi: 10.1080/14330237.2016.1268293
15. Maenhout L, Peuters C, Cardon G, Compernolle S, Crombez G, DeSmet A. The association of healthy lifestyle behaviors with mental health indicators among adolescents of different family affluence in Belgium. BMC Public Health. (2020) 20:958. doi: 10.1186/s12889-020-09102-9
16. Zhu Y, Yu X, Wu Y, Shi C, Zhang A, Jiang R, et al. Association of depression and unhealthy lifestyle behaviors in chinese patients with acute coronary syndromes. J Cardiopulm Rehabil Prev. (2019) 39:E1–5. doi: 10.1097/HCR.0000000000000384
17. Redfield RR, B. R., Greenspan A, Kent CK, Leahy MA, Martinroe JC, et al. Youth Risk Behavior Surveillance System (YRBSS). (2019). Available online at: www.cdc.gov/healthyyouth/data/yrbs/index.htm (accessed July 23, 2021).
18. Baiden P, Tadeo SK, Tonui BC, Seastrunk JD, Boateng GO. Association between insufficient sleep and suicidal ideation among adolescents. Psychiatry Res. (2020) 287:112579. doi: 10.1016/j.psychres.2019.112579
19. Chiu HY, Lee HC, Chen PY, Lai YF, Tu YK. Associations between sleep duration and suicidality in adolescents: a systematic review and dose-response meta-analysis. Sleep Med Rev. (2018) 42:119–26. doi: 10.1016/j.smrv.2018.07.003
20. Lee YJ, Cho SJ, Cho IH, Kim SJ. Insufficient sleep and suicidality in adolescents. Sleep. (2012) 35:455–60. doi: 10.5665/sleep.1722
21. Schilling EA, Aseltine RH Jr., Glanovsky JL, James A, Jacobs D. Adolescent alcohol use, suicidal ideation, suicide attempts. J Adolesc Health. (2009) 44:335–41. doi: 10.1016/j.jadohealth.2008.08.006
22. Gao C, Sun Y, Zhang F, Zhou F, Dong C, Ke Z, et al. Prevalence and correlates of lifestyle behavior, anxiety and depression in Chinese college freshman: a cross-sectional survey. Int J Nurs Sci. (2021) 8:347–53. doi: 10.1016/j.ijnss.2021.05.013
23. Perlis ML, Grandner MA, Chakravorty S, Bernert RA, Brown GK, Thase ME. Suicide and sleep: Is it a bad thing to be awake when reason sleeps? Sleep Med Rev. (2016) 29:101–7. doi: 10.1016/j.smrv.2015.10.003
24. Chan NY, Zhang J, Tsang CC, Li AM, Chan JWY, Wing YK, et al. The associations of insomnia symptoms and chronotype with daytime sleepiness, mood symptoms and suicide risk in adolescents. Sleep Med. (2020) 74:124–31. doi: 10.1016/j.sleep.2020.05.035
25. Blake MJ, Allen NB. Prevention of internalizing disorders and suicide via adolescent sleep interventions. Curr Opin Psychol. (2020) 34:37–42. doi: 10.1016/j.copsyc.2019.08.027
26. Gijzen MWM, Rasing SPA, Creemers DHM, Smit F, Engels R, De Beurs D. Suicide ideation as a symptom of adolescent depression. A network analysis. J Affect Disord. (2021) 278:68–77. doi: 10.1016/j.jad.2020.09.029
27. Franklin JC, Huang X, Bastidas D. Virtual reality suicide: development of a translational approach for studying suicide causes. Behav Res Ther. (2019) 120:103360. doi: 10.1016/j.brat.2018.12.013
28. Twenge JM, Joiner TE, Rogers ML, Martin GN. Increases in depressive symptoms, suicide-related outcomes, and suicide rates among U.S. Adolescents after 2010 and links to increased new media screen Time. Clin Psychol Sci. (2018) 6:3–17. doi: 10.1177/2167702617723376
29. Rostad WL, Basile KC, Clayton HB. Association among television and computer/video game use, victimization, and suicide risk among U.S. High School Students. J Interpers Viol. (2021) 36:2282–2305. doi: 10.1177/0886260518760020
30. Lester D. Participation in sports activities and suicidal behaviour: a risk or a protective factor? Int J Sport Exer Psychol. (2017) 15:103–8. doi: 10.1080/1612197X.2015.1073340
31. Unger JB. Physical activity, participation in team sports, and risk of suicidal behavior in adolescents. Am J Health Promot. (1997) 12:90–3. doi: 10.4278/0890-1171-12.2.90
32. Taliaferro LA, Eisenberg ME, Johnson KE, Nelson TF, Neumark-Sztainer D. Sport participation during adolescence and suicide ideation and attempts. Int J Adolesc Med Health. (2011) 23:3–10. doi: 10.1515/ijamh.2011.002
33. Sibold J, Edwards E, Murray-Close D, Hudziak JJ. Physical activity, sadness, and suicidality in bullied US adolescents. J Am Acad Child Adolesc Psychiatry. (2015) 54:808–15. doi: 10.1016/j.jaac.2015.06.019
34. Xiao Y, Romanelli M, Lindsey MA. A latent class analysis of health lifestyles and suicidal behaviors among US adolescents. J Affect Disord. (2019) 255:116–26. doi: 10.1016/j.jad.2019.05.031
35. Lee SA, Park E-C, Ju YJ, Lee TH, Han E, Kim TH, et al. Breakfast consumption and depressive mood: a focus on socioeconomic status. Appetite. (2017) 114:313–9. doi: 10.1016/j.appet.2017.04.007
36. Lien L. Is breakfast consumption related to mental distress and academic performance in adolescents? Public Health Nutr. (2007) 10:422–8. doi: 10.1017/S1368980007258550
37. Ferrer-Cascales R, Sánchez-SanSegundo M, Ruiz-Robledillo N, Albaladejo-Blázquez N, Laguna-Pérez A, Zaragoza-Martí A. Eat or skip breakfast? The important role of breakfast quality for health-related quality of life, stress and depression in Spanish adolescents. Int J Environ Res Public Health. (2018) 15:1781. doi: 10.3390/ijerph15081781
38. Khalid S, Williams CM, Reynolds SA. Is there an association between diet and depression in children and adolescents? A systematic review. Br J Nutr. (2016) 116:2097–108. doi: 10.1017/S0007114516004359
39. Pompili M, Serafini G, Innamorati M, Dominici G, Ferracuti S, Kotzalidis GD, et al. Suicidal behavior and alcohol abuse. Int J Environ Res Public Health. (2010) 7:1392–431. doi: 10.3390/ijerph7041392
40. Pandey AR, Bista B, Dhungana RR, Aryal KK, Chalise B, Dhimal M. Factors associated with suicidal ideation and suicidal attempts among adolescent students in Nepal: findings from Global School-based Students Health Survey. PLos ONE. (2019) 14:e0210383. doi: 10.1371/journal.pone.0210383
41. Kim HW, Kim YK, Paik JY, Hong CB, Lee K, Park J, et al. The relationship between smoking and suicidal behavior in Korean adolescents: 12th Korea Youth Risk Behavior web-based survey. Korean J Health Promot. (2017) 17:219–33. doi: 10.15384/kjhp.2017.17.4.219
42. Han MA, Kim KS, Ryu SY, Kang MG, Park J. Associations between smoking and alcohol drinking and suicidal behavior in Korean adolescents: Korea Youth Behavioral Risk Factor Surveillance, 2006. Prev Med. (2009) 49:248–52. doi: 10.1016/j.ypmed.2009.06.014
43. Cho MS. Use of alcohol, tobacco, and caffeine and suicide attempts: findings from a nationally representative cross-sectional study. J Prim Care Commun Health. (2020) 11:2150132720913720. doi: 10.1177/2150132720913720
44. Poorolajal J, Darvishi N. Smoking and suicide: a meta-analysis. PLoS ONE. (2016) 11:e0156348. doi: 10.1371/journal.pone.0156348
45. Hughes JR. Smoking and suicide: a brief overview. Drug Alcohol Depend. (2008) 98:169–78. doi: 10.1016/j.drugalcdep.2008.06.003
Keywords: lifestyle, behaviors, suicide, adolescents, the Youth Risk Behavior Surveillance System Survey
Citation: Li X, Chi G, Taylor A, Chen S-T, Memon AR, Zhang Y, Song Y, Li J, Luo X and Zou L (2021) Lifestyle Behaviors and Suicide-Related Behaviors in Adolescents: Cross-Sectional Study Using the 2019 YRBS Data. Front. Public Health 9:766972. doi: 10.3389/fpubh.2021.766972
Received: 30 August 2021; Accepted: 12 October 2021;
Published: 19 November 2021.
Edited by:
Yuka Kotozaki, Iwate Medical University, JapanReviewed by:
Catalina Sau Man Ng, The Education University of Hong Kong, Hong Kong SAR, ChinaSiddharth Sarkar, All India Institute of Medical Sciences, India
Copyright © 2021 Li, Chi, Taylor, Chen, Memon, Zhang, Song, Li, Luo and Zou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yagang Song, ygsong1990@163.com
 Xiaozhi Li1
Xiaozhi Li1 Alyx Taylor
Alyx Taylor Si-Tong Chen
Si-Tong Chen Aamir R. Memon
Aamir R. Memon Yanjie Zhang
Yanjie Zhang Yagang Song
Yagang Song Jinming Li
Jinming Li Liye Zou
Liye Zou