- 1Guangdong Key Laboratory of Mental Health and Cognitive Science, Ministry of Education Key Laboratory of Brain Cognition and Educational Science, Centre for Studies of Psychological Applications, School of Psychology, South China Normal University, Guangzhou, China
- 2Faculty of Medicine, McGill University, Montreal, QC, Canada
- 3Center for Public Health Initiatives, University of Pennsylvania, Philadelphia, PA, United States
Background: People with prior experience of severe trauma may be particularly vulnerable in the face of the COVID-19 pandemic. However, little is known about mental health problems among prior trauma survivors during the pandemic outbreak.
Methods: A total of 362 Wenchuan earthquake survivors were assessed using Patient Health Questionnaire, Generalized Anxiety Disorder Scale, as well as Multidimensional Scale of Perceived Social Support, as part of an online survey between February 3 and 10, 2020.
Results: Our results showed that 6.6 and 4.7% of the participants experienced depression and anxiety during the COVID-19 outbreak, respectively. Perceived social support was negatively associated with depressive and anxiety symptoms. Earthquake exposure has no direct effect on current depressive and anxiety symptoms, but it would moderate the direct relationship between perceived social support and psychological symptoms.
Conclusions: Our findings suggested that trauma exposure may lead to salutogenic outcomes. The protective effect of perceived social support on psychological symptoms was greater in people with a higher level of trauma exposure than in a lower one.
Background
Numerous studies have shown that the COVID-19 pandemic leads to the development of mental health problems in public (1, 2). For some special groups, such as psychiatric patients (3), frontline healthcare workers (4), and even patients infected with COVID-19 (5), their mental health is even more likely to be affected by the pandemic. However, little attention has been paid to the mental health of another high-risk group during the pandemic: survivors of prior trauma.
Theoretically, prior trauma exposure and subsequent posttraumatic stress (PTS) symptoms may intensify one's vulnerability when facing additional stressors. By draining one's resources (6, 7) and coping capacity, trauma exposure and PTS symptoms heighten one's sensitivity to stress (8, 9). One late study in a sample of 976 adults indicated that history of trauma exposure and resultant PTS were associated with an elevated risk for psychological distress following COVID-19 (10). This finding leads us to suspect that whether individuals who experienced natural disaster (e.g., earthquake) could have greater risks of poor mental health during the COVID-19 pandemic.
Considered as an important disaster preparedness resource, social support is linked to better mental health outcomes for survivors after disasters (11). More specifically, it has been proposed that stronger social support can predict better mental health functioning (12, 13), enhance resilience to stress, and help protect against developing trauma-related psychopathology (14). Meanwhile, people who give and receive social support before the occurrence of disasters are significantly less likely to develop mental health problems (e.g., depressive symptoms) during the post-disaster time compared to those without support (15).
On the other hand, perceived social support is distinct from received social support, which is a better predictor of mental health and support utilization than other measures (16). People suffering from a greater degree of disaster-related traumatic stressors are more likely to seek and receive greater amount of actual support, which consists of a significant indirect path to reduce distress. Greater received support predicted greater perceived support over time, and greater perceived support in turn predicted greater reductions in distress over time, although perceived support tends to decrease over time (17–21). Furthermore, the level of perceived social support was negatively impacted by disaster-related stressors as well as subsequent life stressors in the aftermath of disasters (22). Accordingly, what about prior trauma survivors' perceived social support while facing a subsequent traumatic events such as the COVID-19 pandemic?
In the light of the foregoing discussion, we conducted the present study to examine the level of perceived social support and the prevalence of mental health problems among Wenchuan earthquake (2008) survivors during the COVID-19 outbreak. Three specific objectives were as follows: (a) to investigate depression and anxiety prevalence rates among 362 earthquake survivors during the pandemic outbreak; (b) to examine the effect of perceived social support in relation to depression and anxiety; and (c) to explore the differences in the relationship between perceived social support and mental health among survivors who suffer from different levels of earthquake exposure severity. It was hypothesized that perceived social support would be negatively associated with depression/anxiety. Earthquake exposure severity would moderate the direct association between perceived social support and mental health. Specifically, people suffering from greater degree of earthquake exposure are more likely to perceive greater social support, leading to fewer mental health problems.
Methods
Participants and Procedure
The 8.0-magnitude earthquake occurred on May 12, 2008, in Wenchuan county of Sichuan province, which has been the strongest earthquake over the past 50 years in China. The earthquake was devastating: 69,197 died, 374,176 were injured, and 18,222 were missing. Meanwhile, at least 4.8 million residents were left homeless due to their houses being destroyed by the earthquake. Fan et al. conducted a longitudinal study of mental health among adolescent survivors exposed to the Wenchuan earthquake in May 2008 (23). A total of 1,573 Wenchuan earthquake survivors completed assessments of mental health at 6 months after the earthquake (sampling time: November 2008) (23). Among these participants, 410 completed the web-based survey during the COVID-19 outbreak (sampling time: from February 3 to 10, 2020), and the response rate was 26.1%. To control the quality of the survey responses, exclusion criteria included was that “missing information >25%” and “response time <5 min.” Finally, 362 participants were included in the subsequent analyses. The chi-square test and t-test were used to compare the participants who participated in the web-based survey during the COVID-19 outbreak with those whose did not in major variables at baseline. There was no significant difference in age (t = −1.05, p = 0.292) and earthquake exposure (t = −0.79, p = 0.431) between these two groups. Men were less likely to participate (χ2 = 15.90, p < 0.001), mainly because they were more likely to drop out at school age. Among participants, 93.6% (N = 339) of the survivors lived in Sichuan Province during the survey period, which was a low infection risk area with <1,000 cumulative confirmed cases during the COVID-19 outbreak (24).
Researchers sent the informed consent and a specific web link or quick response (QR) code to participants through their contact information (e.g., QQ, WeChat, or SMS). Participants completed the online survey by clicking the questionnaire link or scanning the QR code of the questionnaire with mobile phones. This study was entirely voluntary; interested participants needed to sign an electronic informed consent form before the survey and could quit at any time. The ethics board of the South China Normal University (SCNU-PSY-2020-01-001) examined and approved the project. Participants were also provided psychological counseling from the School of Psychology, South China Normal University. If needed, participants can also assess free online psychological counseling service (“Xin-Qing”Hotline) from the School of Psychology of South China Normal University.
Measures
Sample Characteristics and Trauma Exposure
Sample characteristics included sex, age, marital status, family income, history of mental and physical illness, history of smoking, and alcohol use.
The main two trauma exposures in this study are Wenchuan earthquake and COVID-19 pandemic-related factors. Earthquake exposure was assessed using four items (25): I1: death, injury, and/or missing of family members; I2: house damage; I3: property loss; I4: witness or hearing of tragic scenes. Each item was rated on a five-point Likert scale with 1 representing the lowest level of exposure and five representing the highest. Summing up scores on all items generates a total score, indicating overall severity of earthquake exposure.
Pandemic-related factors were assessed using three questions: Q1: Are there confirmed or suspected cases in your community or village? (1 = yes, 0 = no); Q2: Do you have relatives or friends who have been infected with COVID-19? (1 = yes, 0 = no); and Q3: How much time are you exposed to news and information about COVID-19 on social media? (1 = <1 h/day, 2 = 1–2 h/day, 3 = >3 h/day).
Perceived Social Support
The Multidimensional Scale of Perceived Social Support (MSPSS) was used to assess participants' perceived social support (26). It consisted of 12 items addressing the following three domains: family, friends, and significant others. Each item was scored on a 7-point scale ranging from 1 (very strongly disagree) to 7 (very strongly agree), with a range of 12–84. A higher total score indicated greater level of perceived social support. Degree of social support can be determined by the following cuto? scores: 12–48 low social support, 49–68 moderate social support, and 69–84 high social support. The Chinese version of MSPSS was reported to have good reliability and validity (27). It also had satisfactory internal consistency in this study (Cronbach' α = 0.95).
Depressive Symptoms
The 9-item Patient Health Questionnaire (PHQ-9) was used to assess participants' depressive symptoms over the past 2 weeks (28). Each item was answered on a 3-point Likert scale (0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day), with higher scores indicating higher levels of depressive symptoms. The cutoff point of 10 was usually used for demonstrating clinically significant depression (29). The Chinese version of PHQ-9 has been reported to have good reliability and validity in the Chinese sample (30). In the current sample, Cronbach's α for PHQ-9 was 0.89.
Anxiety Symptoms
The 7-item Generalized Anxiety Disorder (GAD-7) was used to measure participants' anxiety symptoms over the past 2 weeks (31). Responders should provide a response for each item using a 6-point scale ranging from 0 (not at all) to 3 (nearly every day). Summing up scores on all items would generate a total score indicating the overall severity of anxiety symptoms. A preliminary study suggested that a cutoff score of 10 is the optimal threshold to indicate clinical level of anxiety (32). The scale of the Chinese version has demonstrated satisfactory psychometric properties in the Chinese population (33). In the present study, GAD-7 also demonstrated high internal consistency, with the Cronbach's α being 0.93.
Data Analyses
All statistical analyses were conducted using SPSS, version 23.0, and p < 0.05 were considered statistically significant for all two-tailed tests. Descriptive statistics were calculated for sample characteristics, pandemic-related factors, and earthquake exposure. To assess the differences between levels of perceived social support in relation to PHQ-9 and GAD-7, χ2-test and one-way ANOVA were used, as appropriate. Pearson correlations were examined among earthquake exposure, MSPSS, PHQ-9, and GAD-7. Meanwhile, PROCESS was used to examine the mediation hypotheses, with 5,000 iterations to estimate the effect size of models (34). Harman's one-factor test was conducted to examine common method variance before regression analysis (35). The moderation effect was tested: MSPSS score was entered as the predictor, earthquake exposure was entered as the moderator, and PHQ-9 or GAD-7 score was entered as the outcome. Simple slopes were calculated for high, medium, and low levels of earthquake exposure (using the mean score and cutoffs either one standard deviation above or below the mean), to determine the level at which perceived social support starts to have a significant correlation with earthquake exposure. Sample characteristics and pandemic-related factors were also included in the current analyses as covariates.
Results
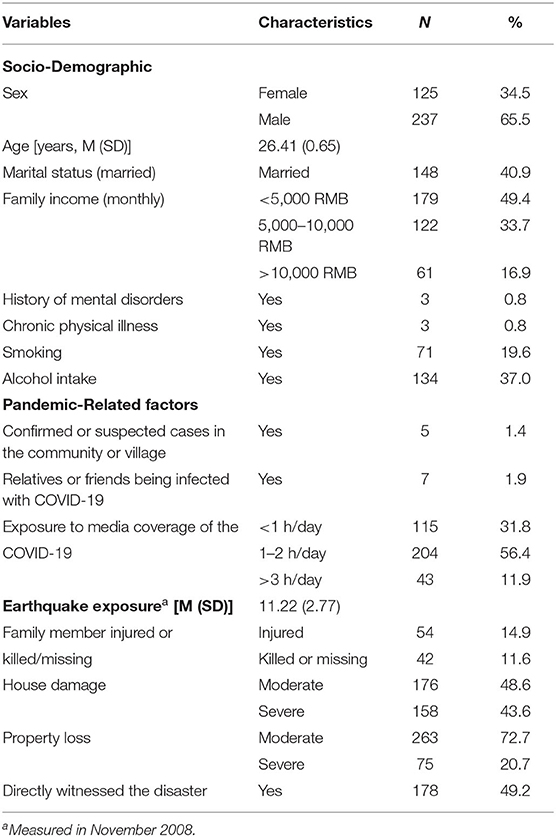
This sample consisted of 362 Wenchuan earthquake survivors, 125 men and 237 women. Their age ranged from 25 to 28 years old, with the average age of 26.41 (SD = 0.65) years; 1.4% participants lived in the community or village with confirmed or suspected cases, and 1.9% reported that their relatives or friends have been infected with COVID-19. Other sample characteristics and trauma exposure are listed in Table 1.
Of the 362 participants, 24 (6.6%) had depression, with a mean PHQ-9 score of 3.01 (SD = 3.87). A total of 17 (4.7%) were shown to be positive for anxiety, with a mean GAD-7 score of 2.20 (SD = 3.29). In terms of perceived social support, only 14.4% (N = 52) had a low level, while 42.5% (N = 154) had a high level. The mean score of MSPSS was 63.98 (SD = 12.10).
Demographic characteristics along with the outcomes of interest were presented in Table 2, stratified by different levels of perceived social support. Compared to low perceived social support, participants who perceived a high level of social support were reported to have lower PHQ-9 and GAD-7 scores, as well as significantly lower proportion of depression and anxiety. Correlation analysis further showed MSPSS scores being negatively associated with PHQ-9 (r = −0.41, p < 0.001) and GAD-7 (r = −0.37, p < 0.001) scores. In addition, earthquake exposure was not associated with MSPSS (r = −0.07, p = 0.177), PHQ-9 (r =0.07, p = 0.186), and GAD-7 (r =0.06, p = 0.282) scores.
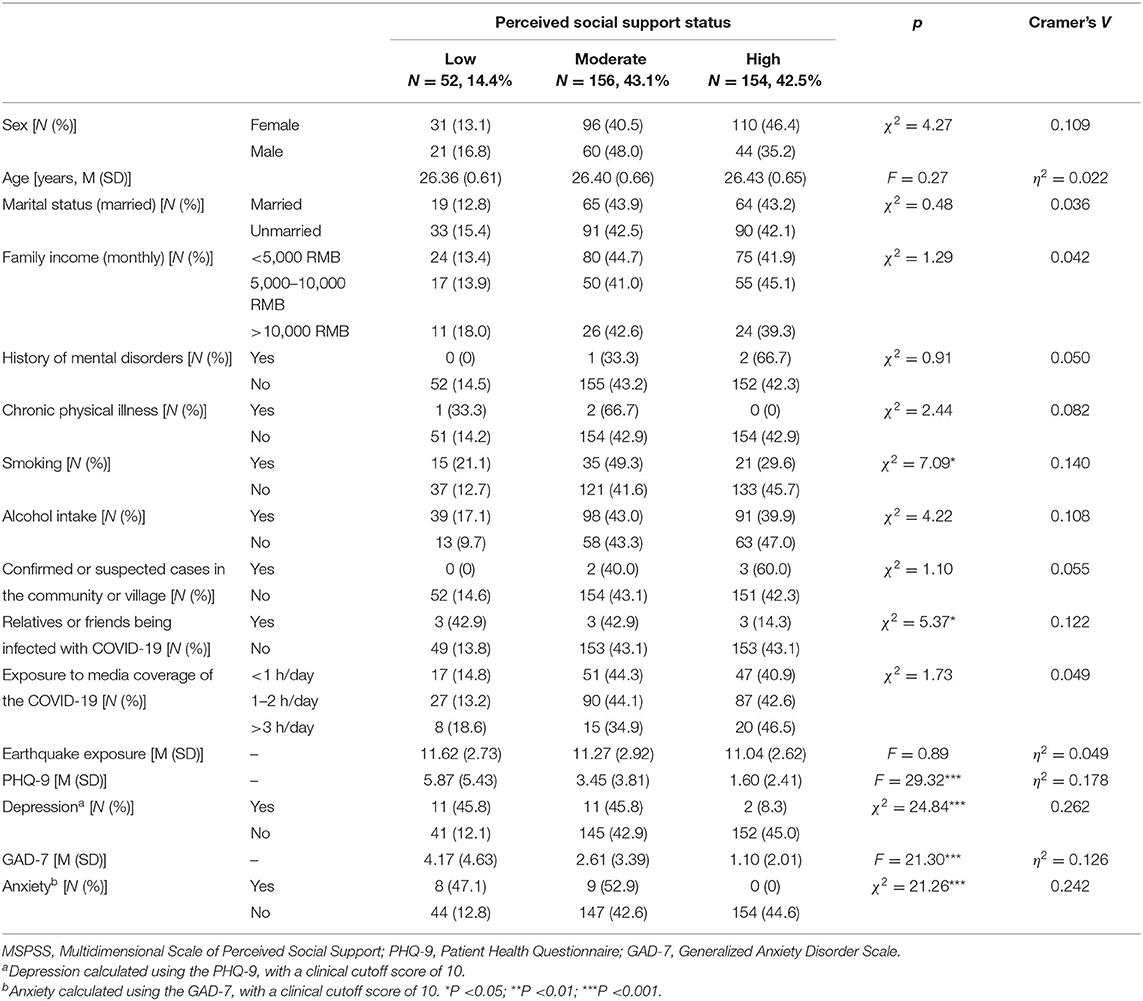
Table 2. Characteristics of participants enrolled to the study according to perceived social support status.
As shown in Table 3, the moderation model with PHQ-9 score as outcome was significant with F(14, 347) = 7.40, p < 0.001, accounting for 23.0% of the total variance. Perceived social support had a negative main effect on depressive symptoms (b = −0.40, SE = 0.05, 95% CI = −0.49, −0.30). While earthquake exposure did not directly affect depressive symptoms (b = 0.05, SE = 0.05, 95% CI = −0.05,0.14), it moderated the relationship between perceived social support and depressive symptoms, b = −0.14, SE = 0.05, 95% CI = −0.24, −0.04, indicating that the indirect effect of perceived social support on depressive symptoms significantly differed at various levels of earthquake exposure. With simple slope analyses, a significant negative relationship between perceived social support and depressive symptoms was found at low (b = −0.28, SE = 0.06, 95% CI = −0.41, 0.16), moderate (b = −0.38, SE = 0.05, 95% CI = −0.48, −0.29), and high levels of earthquake exposure (b = −0.54, SE = 0.07, 95% CI = −0.67, −0.40) (see Figure 1A).
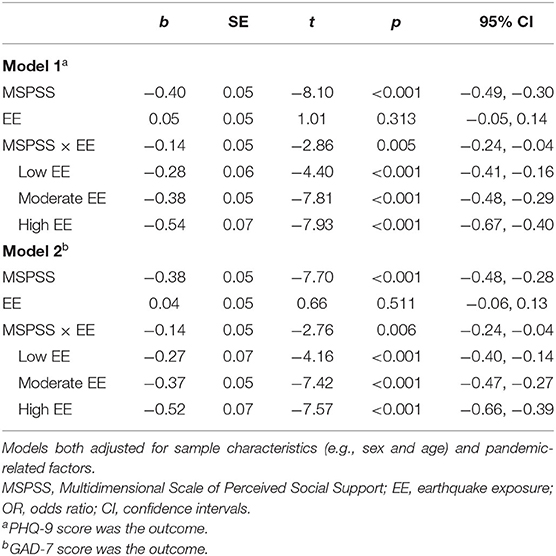
Table 3. Regression coefficients from analyses of moderating effect of earthquake exposure on the relationship between perceived social support and mental health status.
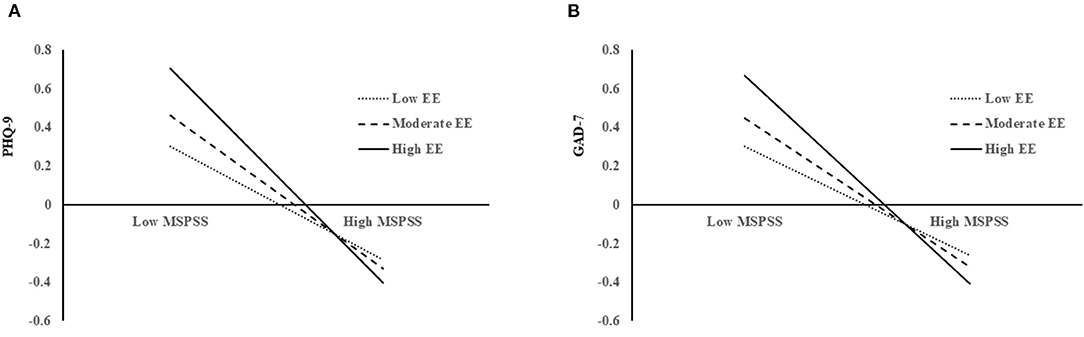
Figure 1. Simple slope analyses. (A) The interaction between perceived social support and depression as moderated by earthquake exposure and shows that perceived social support was negatively associated with depression better with higher earthquake exposure. (B) The interaction between perceived social support and anxiety as moderated by earthquake exposure and shows that perceived social support was negatively associated with anxiety better with higher earthquake exposure. MSPSS, Multidimensional Scale of Perceived Social Support; EE, earthquake exposure; PHQ-9, Patient Health Questionnaire; GAD-7, Generalized Anxiety Disorder Scale.
The moderation model with GAD-7 score as the outcome was also significant with F(14, 347) = 6.40, p < 0.001, accounting for 20.5% of the total variance. Similar to the results of depressive symptoms, earthquake exposure moderates the relationship between perceived social support and anxiety symptoms (b = −0.14, SE = 0.05, 95% CI = −0.24, −0.14). Simple slope analyses also found a significantly positive relationship between perceived social support and anxiety symptoms at low (b = −0.27, SE = 0.07, 95% CI = −0.40, −0.14), moderate (b = −0.37, SE = 0.05, 95% CI = −0.47, −0.27), and high (b = −0.37, SE = 0.07, 95% CI = −0.66, −0.39) level of earthquake exposure (see Figure 1B). These findings indicated that earthquake exposure is a moderator of perceived social support and mental health among earthquake survivors during the COVID-19 outbreak.
Discussion
To our best knowledge, this was the first study to examine the mental health status of prior natural disaster survivors during the COVID-19 outbreak. Our findings suggested that earthquake survivors did not confer any increase in the prevalence of depression and anxiety during the outbreak phase of the pandemic. Meanwhile, higher prior earthquake exposure experience strengthens the protective effect of individual's perceived social support.
This study found that only 6.6% of the participants reported having depression and 4.7% reported having anxiety. In order to understand the meaning of our results, they are compared with data of the same type (the PHQ-9/GAD-7 cutoff of 10 or higher) on national and international surveys during the pandemic outbreak. Based on previous research, depression and anxiety rate in the current sample was lower than that of a similar study measuring Chinese adult citizens (12% depression, 7.1% anxiety) between February 9 and 20, 2020 (36). Several web-based studies found that the percentage of Chinese general public with depression was 13.6% between February 11 and 16, 2020 (37), and anxiety rate was 22.6% between January 31 and February 2, 2020 (38). Meanwhile, the general population from Jordan reported 32.1% depression and 22.8% anxiety between March 22 and 28, 2020 (39). Ettman et al. observed that the prevalence rate of depression was 27.8% in U.S. general adults during the COVID-19 outbreak (March 31–April 13, 2020) (40). Compared to these studies that have taken place in a similar phase of the outbreak, lower levels of depression and anxiety symptoms were observed in earthquake survivors.
Our study also found a higher level of perceived social support in earthquake survivors when compared to that of general college students in China during the same period (February 3–10, 2020). Our results showed that perceived social support of the present sample (mean score = 63.98, SD = 12.10) was higher than the level of college students (mean score = 59.8, SD = 11.7) living in the moderate-risk (Guangdong Province) and low-risk aeras (Jiangxi Province) (41). In the current sample, 42.5% of participants could be classified into the high social support group (scores from 69 to 84), which seemed to be significantly higher than the rate in the Lebanese public (20.8%) during the outbreak of COVID-19 with a consistent demarcation (42). Earthquake survivors having higher perceived social support in our study may be due to the solid financial and emotional support from both the government and the civilians in China (43), such as house reconstruction and better healthcare. In addition, perceived social support was observed to have a significant negative association with anxiety and depression. Higher levels of perceived social support were related to lower level of depression and anxiety outcomes, which was in line with previous literature (42, 44). It has been proposed that such social support could predict better mental health functioning and be regarded as a protective factor against the onset of new mental health problems (12, 45). More specifically, social support could also enhance resilience to stress and reduce the development of trauma-related psychopathology (14).
Interestingly, prior earthquake exposure did not exhibit a direct effect on current depressive and anxiety symptoms, but it moderated the relationship between perceived social support and psychological symptoms. The effect of perceived social support on depression or anxiety significantly differed at varying levels of prior earthquake exposure. Specifically, social support had a stronger protective effect on mental health among survivors who had greater earthquake exposure. Although scholars proposed that trauma was a vital risk factor for individuals' mental health issues (46), prior trauma exposure might also have salutogenic effects. Recent evidence found that people with high trauma exposure were more likely to experience posttraumatic growth (PTG) (47), which denoted the tendency to report a positive transformation in the aftermath of a trauma exposure (48). Scrutinizing the empirical literature also found that participants with higher PTSD symptoms were more likely to grow from the impact of the trauma (49, 50). Theoretically, PTG might indicate perceived change rather than reflect actual growth (51). It could also be understood as a motivated positive illusion that served a protective function (52). We speculated that these improved personal resources and qualities [e.g., resilience (53)] that precipitated from past adversities acted as active protective factors that could be set in motion as one facing adversities again (e.g., COVID-19 pandemic).
Finally, several limitations must be considered. First, the present study was conducted on a sample of trauma survivors who experienced the 2008 Wenchuan earthquake. Before the disaster, they were both students of junior and senior school (Grades 7–12). Therefore, generalizations of our findings to sufferers of other traumatic experiences or of different age groups need to be done with caution. Second, there was a high attrition rate in the present study, which may lead to affect the accuracy of results. The time interval between the two surveys was more than 11 years, resulting in a high attrition rate. Although no significant differences were found for earthquake exposure between participants who followed up and those lost to follow-up, the results need to be interpreted with caution. Third, depression and anxiety variables relied on self-report questionnaires, which might cause potential reporting bias in the data collection. Meanwhile, other important factors that might affect the study findings, such as PTG or actual support, were not examined. In addition, depression and anxiety among the current sample needed to be further assessed longitudinally. Mental healthcare should still be provided to those prior trauma survivors at risk in the aftermath of the pandemic.
Conclusion
In conclusion, this study described the unique contribution of prior trauma exposure in explaining trauma-related symptoms among earthquake survivors during the COVID-19 outbreak. Earthquake survivors seemed to perceive higher levels of social support and exhibit lower mental health problems. They might also have a faster decline in mental health problems if they have been involved in greater prior trauma.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Board of the South China Normal University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
DW, FF, and XL: conceptualization. DW: methodology, formal analysis, and writing—original draft. DW, JC, YC, SH, and CW: data curation. SZ, FF, and XL: writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
The present study was funded by the National Natural Science Foundation of China (Grant No. 31871129); Research on the Processes and Repair of Psychological Trauma in Youth, Project of Key Institute of Humanities and Social Sciences, MOE (Grant No. 16JJD190001); Guangdong Province Universities and Colleges Pearl River Scholar Funded Scheme (GDUPS 2016); and Graduate Research and Innovation Project of School of Psychology, South China Normal University (PSY-SCNU202017).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to show their great gratitude to all participants and related workers in this study for their participation.
References
1. Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. (2021) 28:91–8. doi: 10.1016/j.jad.2020.11.117
2. Cenat JM, Blais-Rochette C, Kokou-Kpolou CK, Noorishad PG, Mukunzi JN, McIntee SE, et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. (2021) 295:113599. doi: 10.1016/j.psychres.2020.113599
3. Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. (2020) 87:100–6. doi: 10.1016/j.bbi.2020.04.069
4. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
5. Mazza MG, De Lorenzo R, Conte C, Poletti S, Vai B, Bollettini I, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun. (2020) 89:594–600. doi: 10.1016/j.bbi.2020.07.037
6. Hobfoll SE. The influence of culture, community, and the nested-self in the stress process: advancing conservation of resources theory. Appl Psychol. (2001) 50:337–70. doi: 10.1111/1464-0597.00062
7. Hobfoll SE. Social and psychological resources and adaptation. Rev Gen Psychol. (2002) 6:307–24. doi: 10.1037/1089-2680.6.4.307
8. Resnick HS, Yehuda R, Pitman RK, Foy DW. Effect of previous trauma on acute plasma cortisol level following rape. Am J Psychiatry. (1995) 152:1675–7. doi: 10.1176/ajp.152.11.1675
9. Yehuda R, Kahana B, Schmeidler J, Southwick SM, Wilson S, Giller EL. Impact of cumulative lifetime trauma and recent stress on current posttraumatic stress disorder symptoms in holocaust survivors. Am J Psychiatry. (1995) 152:1815–8. doi: 10.1176/ajp.152.12.1815
10. Lahav Y. Psychological distress related to COVID-19 - The contribution of continuous traumatic stress. J Affect Disord. (2020) 277:129–37. doi: 10.1016/j.jad.2020.07.141
11. Shang F, Kaniasty K, Cowlishaw S, Wade D, Ma H, Forbes D. Social support following a natural disaster: a longitudinal study of survivors of the 2013 lushan earthquake in China. Psychiatry Res. (2019) 273:641–6. doi: 10.1016/j.psychres.2019.01.085
12. Harandi TF, Taghinasab MM, Nayeri TD. The correlation of social support with mental health: a meta-analysis. Electron Physician. (2017) 9:5212–22. doi: 10.19082/5212
13. De Silva MJ, McKenzie K, Harpham T, Huttly SR. Social capital and mental illness: a systematic review. J Epidemiol Community Health. (2005) 59:619–27. doi: 10.1136/jech.2004.029678
14. Ozbay F, Johnson DC, Dimoulas E, Morgan CA, Charney D, Southwick S. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry. (2007) 4:35–40.
15. Sasaki Y, Aida J, Tsuji T, Koyama S, Tsuboya T, Saito T, et al. Pre-disaster social support is protective for onset of post-disaster depression: prospective study from the great east Japan earthquake & tsunami. Sci Rep. (2019) 9:19427. doi: 10.1038/s41598-019-55953-7
16. Wethington E, Kessler RC. Perceived support, received support, and adjustment to stressful life events. J Health Soc Behav. (1986) 27:78–89. doi: 10.2307/2136504
17. Kaniasty K, Norris FH. Help-seeking comfort and receiving social support: the role of ethnicity and context of need. Am J Community Psychol. (2000) 28:545–81. doi: 10.1023/A:1005192616058
18. Kaniasty K, Norris FH. In search of altruistic community: patterns of social support mobilization following Hurricane Hugo. Am J Community Psychol. (1995) 23:447–77. doi: 10.1007/BF02506964
19. Kaniasty K, Norris FH. A test of the social support deterioration model in the context of natural disaster. J Pers Soc Psychol. (1993) 64:395–408. doi: 10.1037/0022-3514.64.3.395
20. Norris FH, Baker CK, Murphy AD, Kaniasty K. Social support mobilization and deterioration after Mexico's 1999 flood: effects of context, gender, and time. Am J Community Psychol. (2005) 36:15–28. doi: 10.1007/s10464-005-6230-9
21. Norris FH, Kaniasty K. Received and perceived social support in times of stress: a test of the social support deterioration deterrence model. J Pers Soc Psychol. (1996) 71:498–511. doi: 10.1037/0022-3514.71.3.498
22. La Greca AM, Silverman WK, Lai B, Jaccard J. Hurricane-related exposure experiences and stressors, other life events, and social support: concurrent and prospective impact on children's persistent posttraumatic stress symptoms. J Consult Clin Psychol. (2010) 78:794–805. doi: 10.1037/a0020775
23. Fan F, Zhou Y, Mo L, Zhang W, Xie J, Liu X. Cohort profile: the Wenchuan earthquake adolescent health cohort study. Int J Epidemiol. (2017) 46:27–8. doi: 10.1093/ije/dyw013
24. WHO. Coronavirus Disease (COVID-2019) Situation Reports 2020. WHO (2020). Available online at: https://www.who.int/emergencies/diseases/novelcoronavirus-2019/situation-reports.
25. Geng F, Zhou Y, Liang Y, Fan F. A longitudinal study of recurrent experience of earthquake and mental health problems among Chinese adolescents. Front Psychol. (2018) 9:1259. doi: 10.3389/fpsyg.2018.01259
26. Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. (1990) 55:610–7. doi: 10.1207/s15327752jpa5503&4_17
27. Zhou K, Li H, Wei X, Yin J, Liang P, Zhang H, et al. Reliability and validity of the multidimensional scale of perceived social support in Chinese mainland patients with methadone maintenance treatment. Compr Psychiatry. (2015) 60:182–8. doi: 10.1016/j.comppsych.2015.03.007
28. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
29. Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the patient health questionnaire (PHQ-9): a meta-analysis. CMAJ. (2012) 184:E191–6. doi: 10.1503/cmaj.110829
30. Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2014) 36:539–44. doi: 10.1016/j.genhosppsych.2014.05.021
31. Spitzer RL, Kroenke K, Williams JBW, Lwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
32. Lowe B, Decker O, Muller S, Brahler E, Schellberg D, Herzog W, et al. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care. (2008) 46:266–74. doi: 10.1097/MLR.0b013e318160d093
33. Tong X, An D, Mcgonigal A, Park SDZ. Validation of the generalized anxiety disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res. (2016) 120:31–6. doi: 10.1016/j.eplepsyres.2015.11.019
34. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, New York, NY: Guilford Press (2013).
35. Johnson RE, Rosen CC, Djurdjevic E. Assessing the impact of common method variance on higher order multidimensional constructs. J Appl Psychol. (2011) 96:744–61. doi: 10.1037/a0021504
36. Ren Z, Zhou Y, Liu Y. The psychological burden experienced by Chinese citizens during the COVID-19 outbreak: prevalence and determinants. BMC Public Health. (2020) 20:1617. doi: 10.1186/s12889-020-09723-0
37. Zhang W, Yang X, Zhao J, Yang F, Jia Y, Cui C, et al. Depression and psychological-behavioral responses among the general public in china during the early stages of the COVID-19 pandemic: survey study. J Med Internet Res. (2020) 22:e22227. doi: 10.2196/22227
38. Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE. (2020) 15:e231924. doi: 10.2139/ssrn.3541120
39. Naser AY, Dahmash EZ, Al-Rousan R, Alwafi H, Alrawashdeh HM, Ghoul I, et al. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: a cross-sectional study. Brain Behav. (2020) 10:e1730. doi: 10.1002/brb3.1730
40. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in us adults before and during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2019686. doi: 10.1001/jamanetworkopen.2020.19686
41. Ma Z, Zhao J, Li Y, Chen D, Wang T, Zhang Z, et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol Psychiatr Sci. (2020) 29:e181. doi: 10.1017/S2045796020000931
42. Grey I, Arora T, Thomas J, Saneh A, Tohme P, Abi-Habib R. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res. (2020) 293:113452. doi: 10.1016/j.psychres.2020.113452
43. Fan F, Long K, Zhou Y, Zheng Y, Liu X. Longitudinal trajectories of post-traumatic stress disorder symptoms among adolescents after the Wenchuan earthquake in China. Psychol Med. (2015) 45:2885–96. doi: 10.1017/S0033291715000884
44. Scardera S, Perret LC, Ouellet-Morin I, Gariepy G, Juster RP, Boivin M, et al. Association of social support during adolescence with depression, anxiety, and suicidal ideation in young adults. JAMA Netw Open. (2020) 3:e2027491. doi: 10.1001/jamanetworkopen.2020.27491
45. Wang J, Mann F, Lloyd-Evans B, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. (2018) 18:156. doi: 10.1186/s12888-018-1736-5
46. Hollifield M, Warner TD, Lian N, Krakow B, Jenkins JH, Kesler J, et al. Measuring trauma and health status in refugees: a critical review. JAMA. (2002) 288:611–21. doi: 10.1001/jama.288.5.611
47. Schneider S, Rasul R, Liu B, Corry D, Lieberman-Cribbin W, Watson A, et al. Examining posttraumatic growth and mental health difficulties in the aftermath of hurricane sandy. Psychol Trauma. (2019) 11:127–36. doi: 10.1037/tra0000400
48. Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress. (1996) 9:455–71. doi: 10.1002/jts.2490090305
49. Liu AN, Wang LL, Li HP, Gong J, Liu XH. Correlation between posttraumatic growth and posttraumatic stress disorder symptoms based on Pearson correlation coefficient: a meta-analysis. J Nerv Ment Dis. (2017) 205:380–9. doi: 10.1097/NMD.0000000000000605
50. Lowe SR, Manove EE, Rhodes JE. Posttraumatic stress and posttraumatic growth among low-income mothers who survived Hurricane Katrina. J Consult Clin Psychol. (2013) 81:877–89. doi: 10.1037/a0033252
51. Frazier P, Tennen H, Gavian M, Park C, Tomich P, Tashiro T. Does self-reported posttraumatic growth reflect genuine positive change? Psychol Sci. (2009) 20:912–9. doi: 10.1111/j.1467-9280.2009.02381.x
52. McFarland C, Alvaro C. The impact of motivation on temporal comparisons: coping with traumatic events by perceiving personal growth. J Pers Soc Psychol. (2000) 79:327–43. doi: 10.1037/0022-3514.79.3.327
Keywords: perceived social support, depression, anxiety, trauma exposure, COVID-19
Citation: Wang D, Zhai S, Chen J, Chen Y, Hua S, Wang C, Fan F and Liu X (2022) A Positive Legacy of Trauma? The Role of Perceived Social Support on Mental Health Among Earthquake Survivors During the COVID-19 Outbreak. Front. Psychiatry 13:845929. doi: 10.3389/fpsyt.2022.845929
Received: 30 December 2021; Accepted: 28 February 2022;
Published: 27 April 2022.
Edited by:
Xenia Gonda, Semmelweis University, HungaryReviewed by:
Shi-Bin Wang, Guangdong Mental Health Center, ChinaLiuhua Ying, Zhejiang Sci-Tech University, China
Copyright © 2022 Wang, Zhai, Chen, Chen, Hua, Wang, Fan and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fang Fan, fangfan@scnu.edu.cn
 Dongfang Wang
Dongfang Wang Shuyi Zhai2
Shuyi Zhai2 Fang Fan
Fang Fan