- 1Neuroscience Graduate Program, McMaster University, Hamilton, ON, Canada
- 2Department of Psychiatry and Behavioral Neurosciences, McMaster University, Hamilton, ON, Canada
- 3Anxiety Treatment and Research Clinic, St. Joseph's Healthcare Hamilton, Hamilton, ON, Canada
- 4Department of Psychiatry, University of Western, London, ON, Canada
- 5Homewood Research Institute, Guelph, ON, Canada
- 6Imaging Division, Lawson Health Research Institute, London, ON, Canada
- 7Department of Neuroscience, Western University, London, ON, Canada
- 8Veterans Affairs Canada, Ottawa, ON, Canada
- 9Department of Psychiatry, University of Ottawa, Ottawa, ON, Canada
- 10Centre of Excellence on Post-Traumatic Stress Disorder, Ottawa, ON, Canada
- 11University of Ottawa Institute of Mental Health Research at the Royal, Ottawa, ON, Canada
- 12Homewood Health Centre, Guelph, ON, Canada
- 13Mental Health and Addictions Program, St. Joseph's Healthcare, Hamilton, ON, Canada
The COVID-19 pandemic has resulted in a still-unfolding series of novel, potentially traumatic moral and ethical challenges that place many healthcare workers at risk of developing moral injury. Moral injury is a type of psychological response that may arise when one transgresses or witnesses another transgress deeply held moral values, or when one feels that an individual or institution that has a duty to provide care has failed to do so. Despite knowledge of this widespread exposure, to date, empirical data are scarce as to how to prevent and, where necessary, treat COVID-19-related moral injury in healthcare workers. Given the relation between moral injury and post-traumatic stress disorder (PTSD), we point here to social and interpersonal factors as critical moderators of PTSD symptomology and consider how this knowledge may translate to interventions for COVID-19-related moral injury. Specifically, we first review alterations in social cognitive functioning observed among individuals with PTSD that may give rise to interpersonal difficulties. Drawing on Nietlisbach and Maercker's 2009 work on interpersonal factors relevant to survivors of trauma with PTSD, we then review the role of perceived social support, social acknowledgment and social exclusion in relation to potential areas of targeted intervention for COVID-19-related moral injury in healthcare workers. Finally, building on existing literature (e.g., Phoenix Australia—Centre for Posttraumatic Mental Health and the Canadian Centre of Excellence—PTSD, 2020) we conclude with individual and organizational considerations to bolster against the development of moral injury in healthcare workers during the pandemic.
Introduction
Healthcare workers around the globe are facing a series of novel, potentially traumatic moral and ethical challenges during the COVID-19 pandemic. In interviews with Canadian healthcare workers that our research group has been conducting throughout 2021, for example, healthcare workers have recounted repeatedly struggling with how wrong it feels to helplessly witness the deterioration of human life when caring for critically ill COVID-positive patients (see Figure 1 for a sample vignette of healthcare workers' experiences with moral injury). Exposure to such events has the potential to place healthcare workers at an elevated risk for moral injury. Moral injury is a form of psychological response that may arise when one transgresses, or witnesses another transgress, deeply held moral values, or when one feels that an individual or institution that has a duty to provide care has failed to do so (1, 2). Moral injury is associated with negative mental health outcomes, such as incapacitating feelings of guilt and shame (3) and elevated symptoms of anxiety (4, 5), depression (6–8), post-traumatic stress disorder (PTSD) (4, 5, 9–12) and suicidality (12–14). Despite widespread exposure during the COVID-19 pandemic, limited empirical data renders it unclear at present how best to prevent and, where necessary, treat moral injury in healthcare workers during the pandemic, particularly among those who go on to develop full-blown mental illness as a result of this exposure.
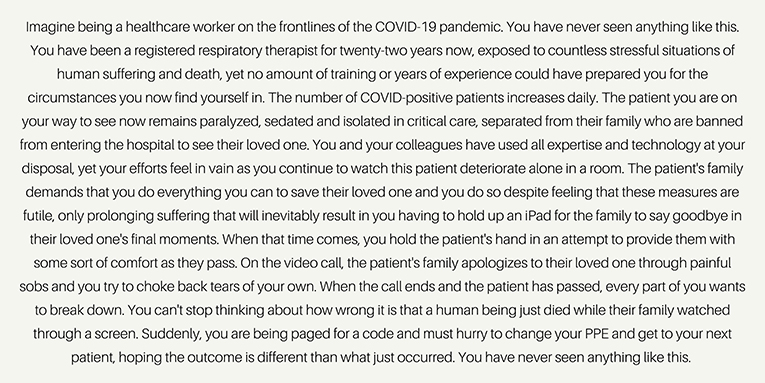
Figure 1. In an ongoing study in our research group, healthcare workers from across Canada have described various events which may be experienced as morally injurious. This vignette provides a summary of the types of events we have heard about from Canadian respiratory therapists early in the Spring of 2021. Participants recounted instances of having to perform care that was perceived to be futile, feeling helpless when caring for critically-ill COVID-positive patients and being at the beside of dying COVID-positive patients in place of their family members, who were prohibited from entering the hospital due to COVID restrictions. Additional stressors compacting upon these potentially morally injurious events included having no time to process events, rushing to change PPE and a high patient caseload.
A growing body of literature points to a relation between moral injury and PTSD (reviewed below), suggesting that knowledge in the field of PTSD may translate well to prevention of and intervention for moral injury. Here, an understanding of alterations in social cognitive functioning (e.g., empathy, moral reasoning, theory of mind) associated with PTSD (15) may assist in better elucidating the role of interpersonal factors (e.g., social support, acknowledgment and exclusion) in moderating PTSD symptomology (16). These disruptions are of particular concern where an overwhelming body of evidence points to social support as a consistently strong predictor of who develops PTSD following trauma exposure (17–22), such as the exposures associated with the current pandemic.
Given evidence pointing toward the role of interpersonal factors in moderating symptoms of PTSD, along with the relation between PTSD and moral injury, we suggest here that an interpersonally-focused approach may serve as a useful starting point for prevention, early intervention, and treatment strategies for COVID-19-related moral injury in healthcare workers. Accordingly, the purpose of the present narrative review is to illustrate the potential utility of an interpersonally-focused approach focusing on the role of perceived social support, social acknowledgment and social exclusion as key targets in understanding and mitigating COVID-19-related moral injury in healthcare workers. In this synthesis of the relevant literature, we first review social cognitive impairments previously observed in PTSD that may be associated with interpersonal difficulties. We next consider Nietlisbach and Maercker's (16) landmark review of the role of social support, social acknowledgment and social exclusion in the development and maintenance of PTSD symptoms and consider these factors in relation to moral injury among healthcare workers during the COVID-19 pandemic. Finally, we summarize individual and organizational considerations for bolstering against the development of moral injury among healthcare workers during and after the pandemic.
Moral Injury in Healthcare Workers
Moral Injury and Moral Distress
The potentially traumatic moral and ethical challenges that healthcare workers face in their occupation were first addressed in the moral distress literature. Moral distress has been conceptualized as the psychological distress that arises when a healthcare worker is prevented, by personal or institutional constraints, from doing what they believe to be right (e.g., witnessing the deterioration of patient care due to institutional factors or a lack of communication) (23, 24). Moral distress is associated with poor self-esteem, low job satisfaction, burnout and intention to leave one's position or profession (23–25). Relatedly, moral injury, as reviewed above, has been defined as a type of psychological response to trauma that may arise from exposure to a single or several potentially morally injurious events (PMIEs): rarely occurring, abnormally stressing, high-stakes situations with limited time for decision making (3, 26). Although a concrete definition has yet to be established, Litz et al. (10) contend that PMIEs can take several forms, including acting in ways that contravene moral values (i.e., acts of commission), failing to prevent events that transgress moral values (i.e., acts of omission), or witnessing someone else fail to act in line with moral values (10). Following this definition, PMIEs may be discussed as perpetration- and/or betrayal-based, where an individual holds perceived responsibility for a PMIE (e.g., by acting or failing to act), or has witnessed/been affected by the actions or inactions of others, respectively (11). Morally injurious outcomes will vary on an individual basis according to the codes of moral conduct in one's culture and one's personal values, yet the sequelae of moral injury, as reported in a recent integrative review, often include widespread effects in psychological/behavioral, social, religious/spiritual and biological domains (11). Following Litz and Kerig's heuristic continuum of moral injury (2), moral distress and moral injury may differ in frequency and event magnitude, where moral distress, although harmful, is believed to be less severe in degree of psychological impact when compared to moral injury (2). Due to its origin in the military literature, empirical research on healthcare workers' experiences with moral injury is limited in comparison to research on moral distress among this population. Indeed, in a recent scoping review, Cartolovni et al. (27) identified just seven articles examining moral injury among healthcare workers. Given the unique moral and ethical challenges present in the healthcare arena, exacerbated further by the COVID-19 pandemic, research in this area appears to be accelerating, with some researchers using moral injury and moral distress as interchangeable terms in healthcare during the COVID-19 pandemic (28).
COVID-19-Related Moral Injury in Healthcare Workers
Healthcare workers may be at an elevated risk for moral injury during the COVID-19 pandemic as they are more likely to be exposed to PMIEs at this time than, for example, civilians. Possible PMIEs discussed within the healthcare context during COVID-19 include having to take potentially life-saving resources from one patient in an attempt to save another patient's life, exposing individuals to the coronavirus because of failure in the screening process, witnessing healthcare managers poorly ration life-saving resources, or witnessing people living life unbothered outside of the hospital (26, 29). Indeed, preliminary findings from ongoing research in our group have revealed that Canadian respiratory therapists experienced intubating and proning patients over 90 years of age and “holding an infant while he passed away because COVID rules would not allow his mother in the room” as PMIEs. Critically, as the pandemic persists, moral injury and other mental health concerns are expected to remain, if not increase. Hines et al. (30) reported that healthcare workers in the United States showed stable symptoms of moral injury across the first 3 months of the pandemic (i.e., March to July 2020), occurring at levels similar to reports from military veterans upon return from deployment (31). Similarly to military populations, moral injury in healthcare workers during the pandemic has been associated with anxiety, depression, PTSD and suicidal ideation (32). Some caution is warranted in the interpretation of these findings, however, as moral injury is a relatively recent concept in the healthcare context and, to date, the clinical and research communities have not identified a highly-reliable, psychometrically-validated measurement tool for common use in this population.
Notably, as moral injury has been related to psychological/behavioral, social, religious/spiritual and biological harm (11), outcomes of moral injury among healthcare workers performing their duties during the COVID-19 pandemic may also vary across these domains. For example, in the case of a respiratory therapist comforting a dying infant in place of his mother, the respiratory therapist may experience impairing moral emotions of guilt, shame, anger or betrayal. The distress associated with this experience may, in turn, lead the respiratory therapist to withdraw from others, question prior beliefs of the world as a just place or experience a spiritual/existential crisis (11). Exposure to this event may be associated with physical manifestations such as decreased sensitivity to pain or stress-related illnesses, such as arthritis and PTSD, as found in prior research on outcomes of exposure to PMIEs (33, 34). Furthermore, exposure to these types of events may be associated with a sense of being “dirty” or shameful, thus contributing to a sense of being undeserving. Relatedly, such feelings of being “undeserving” have been recounted by healthcare workers in our research group's ongoing interviews during the COVID-19 pandemic where healthcare workers have shared that these feelings have limited their efforts to seek appropriate physical or mental healthcare and/or take breaks and rest periods from the healthcare environment.
Moral Injury and PTSD
Moral injury and PTSD are currently thought to be associated yet distinct concepts based on symptomology and etiology (9, 11). Both moral injury and PTSD are stressor-linked problems where the outcome is identified after evidence of a prolonged emotional response from exposure to a potentially traumatic or morally injurious event (2). To date, whereas PTSD is considered a mental disorder, moral injury is not (5, 35). There is some evidence to suggest, however, that moral injury and PTSD are associated by symptomology. Based on research with military service members, Litz et al. (10) developed a conceptual model of moral injury that accounts for intersecting symptoms of PTSD and moral injury. In this model, individuals who experience distress over a moral transgression and hold global, internal and stable (i.e., not context dependent, specific to the individual and enduring) attributions about the event are posited to experience enduring shame, guilt and anxiety, which may influence the individual to socially withdraw. With social withdrawal comes failure to encounter experiences with important members of one's community that may otherwise have provided alternative attributions that cultivate self-forgiveness. Here, Litz et al. (10) contend that the path following internal moral conflict, withdrawal and self-condemnation resembles PTSD symptomology. Indeed, chronic intrusions of the morally transgressive event, avoidance behaviors, numbing, self-harming or self-handicapping and demoralization are expected here and, critically, are also classic experiences indicative of PTSD (10, 36).
Conversely, Bryan et al. (12) found evidence of distinct symptom profiles between moral injury and PTSD in a sample of American military personnel. In this study, the PTSD symptom profile included an exaggerated startle reflex, memory loss, flashbacks, nightmares and insomnia, whereas the moral injury symptom profile included guilt, shame, anger, anhedonia and social alienation (12). A distinction between moral injury and PTSD is further supported by etiology, where PTSD has been defined as a response after exposure to direct or indirect life threat or sexual violence (9), but such criteria is not necessary for PMIEs, which are characterized by moral transgressions or betrayal from leadership (10). Furthermore, Currier et al. (33) highlighted how the function of symptoms consistent between PTSD and moral injury may be related to different motivations in some cases. For example, whereas some individuals with PTSD may engage in avoidance behaviors related to fear and safety concerns, some individuals with moral injury may engage in avoidance behaviors motivated by shame and a perception that they may morally contaminate others (33). Although further research on the relationship between moral injury and PTSD is needed, they are currently thought of as associated yet distinct traumatic responses (9, 11).
Given the relation between moral injury and PTSD, it has been suggested that some evidenced-based psychotherapies for PTSD may prove useful in treating moral injury (9, 37). Here, the majority of research and clinical work centred on the treatment of moral injury focuses primarily on military populations (38–41). For example, prolonged exposure therapy and cognitive processing therapy for PTSD have been proposed for treating moral injury in military samples (35, 38, 42). Murray and Ehlers (35), however, recently discussed the use of cognitive therapy for PTSD (CT-PTSD) for moral injury-related PTSD (i.e., PTSD related to traumatic events including a PMIE), providing a case outline and example of the use of CT-PTSD in a healthcare population. As treatment for moral injury continues to be explored, it will be essential that PTSD treatments be strategically adapted to target symptoms specific to moral injury [e.g., dissonance that arises from the discrepancy between moral beliefs and perpetrations/witnessed events, impairing guilt and shame; (10, 12)].
Social Cognition and PTSD
Alterations in social cognitive functioning have been documented among survivors of trauma who went on to develop a diagnosis of PTSD (15–17, 43–45). Nietlisbach and Maercker (16) previously reviewed evidence for a relation between PTSD and impairments in social cognition and associated interpersonal factors (e.g., social support, acknowledgment and exclusion). Social cognition has been defined as “the ability to use, encode and store information about others that we gain from social interactions” (40). Specifically, social cognition is the coordination of several modes of cognition (e.g., attention, perception, interpretation and processing) in a social context that allows one to perceive and interpret social cues to direct their behavior (41, 46). There are four classic domains of social cognition, namely, theory of mind (ToM), social perception, affective empathy and social behavior (15). ToM refers to the ability to draw on knowledge of how the mind works and of social rules to understand the mental states and beliefs of others (15). ToM can be subdivided into a cognitive component (i.e., what others are thinking) and an affective component (i.e., what others are feeling) (15). Social perception is a domain of social cognition concerned with the ability to recognize and perceive emotional stimuli such as facial expressions, body language or prosody, whereas affective empathy refers to one's emotional response to social situations (15). Finally, social behavior refers to the ways in which an individual conducts themselves in a social context. Alterations in any one of ToM, social perception or affective empathy may lead to deficits in social behavior where an individual displays aggression or socially withdraws (15).
A recently published systematic review of social cognition in PTSD found that social cognition is altered in individuals with PTSD as they display significant impairments in predicting the internal states of others, alterations in perceiving basic emotions and disturbances in empathy (15). In a study investigating emotion recognition and ToM among military police officers exposed to trauma, Mazza et al. (17) found that those with PTSD, in comparison to their counterparts without PTSD, showed deficits in ToM on a task where they were instructed to identify the emotions of a protagonist in a short story. Poljac et al. (44) examined emotion recognition in PTSD patients and controls when viewing video clips of an individual displaying basic emotions. The PTSD group displayed reduced accuracy and sensitivity to facial expressions of fear and sadness in comparison to controls (44). Relatedly, Parlar et al. (47) examined empathic responding among women with PTSD related to childhood trauma. Results of this investigation revealed altered empathic responding in this population, such that women with PTSD showed impairments in identifying the perspective of others when compared to healthy controls (47). Interestingly, however, women with PTSD in this study reported greater levels of personal distress than controls when learning about the negative experiences of others (47). Nazarov et al. (43) examined moral reasoning among women with PTSD related to chronic abuse in childhood and found evidence of altered moral reasoning among these women in comparison to healthy, matched controls. Participants in this study were presented with complex moral situations and were asked to provide a response and justification for their decisions to these dilemmas. The results of this investigation revealed that women with PTSD related to chronic childhood abuse were less likely than controls to approve of utilitarian decisions if the decision involved personally inflicting direct physical harm driven by concern over feelings of guilt and shame associated with these actions (43). Finally, Sherman et al. (45) examined veteran's perceptions of the impact that PTSD had on their parenting, on their children and on the parent-child relationship. More than half of the sample scored above the cut-off on the reactivity subscale of the Parenting Scale, suggestive of alterations in social behavior related to PTSD (45). Cumulatively, the evidence on deficits in key domains of social cognition (i.e., ToM, social perception, affective empathy and social behavior) among individuals with PTSD are related to outcomes of poor quality of life (15). This evidence warrants, in part, the necessity of interpersonally-focused interventions for survivors of trauma with PTSD.
Here, we explore the utility of a social cognitive approach to understanding, mitigating and treating moral injury in healthcare workers during the COVID-19 pandemic. While not intended to be a stand-alone approach to treatment of moral injury in the healthcare population, this perspective may prove useful to the development and implementation of prevention, early intervention and targeted intervention strategies surrounding moral injury in this vital workforce. In a study investigating the relation between moral injury and PTSD among a sample of U.S. National Guard personnel, Bryan et al. (12) noted that a social-cognitive perspective may be a useful approach to understanding moral injury. Social cognitive theory accounts for different types of emotions: natural and manufactured (12, 42). Natural emotions include fear, anxiety and sadness as they are natural responses to direct trauma exposure. By contrast, manufactured emotions are those that arise from an individual's processing and interpretation of events as opposed to the event itself and include feelings of guilt and shame (12, 42). Targeting healthcare workers' interpretation and processing of events during the pandemic, thus, may be one mechanism through which to buffer against the deleterious impacts of guilt and shame related to moral injury. As interpersonal factors such as social support, acknowledgment and inclusion are mediators of PTSD symptom development and maintenance (16), we argue further that an interpersonally-focused approach to moral injury may prove a useful starting point to address COVID-19-related moral injury among healthcare workers.
Importantly, evidence-based treatments for PTSD should always be provided where necessary. The International Society for Traumatic Stress Studies offers guidelines for the prevention and treatment of PTSD, including the use of cognitive behavioral therapy and eye movement desensitization and reprocessing (48). Beyond evidence-based treatments for PTSD that may be adapted for moral injury, a social cognitive approach may be promising, while in need of future study. Notably, this approach relies heavily on a top-down, cognitively oriented approach to the treatment of moral injury. We wish to be clear here that we believe such approaches may, in some cases, require augmentation with more bottom-up therapies that target raw emotion and alterations in somatosensory processes that are also characteristic of PTSD [please see Harricharan et al. (39) for a recent review] (49). An additional caveat to the discussion that follows is that the targeted treatment approach described does not distinguish between dissociative and non-dissociative presentations of PTSD (50–52). Such work, focusing on neuroscientifically-guided approaches to restoration of lower-brain based alterations in emotional processing and somatosensory integration [e.g., deep-brain re-orienting; (53, 54)] as potential augmentative treatments for moral injury are on-going in our research group, as are efforts to develop therapeutic approaches for the treatment of moral injury that distinguish between the dissociative and non-dissociative presentations of PTSD. Lloyd et al. (83) recently demonstrated alterations in top-down control of emotional affect among military and paramilitary personnel with PTSD. Specifically, participants with PTSD described a “nauseating and painful, like an internal gnawing sensation (p. 601)” when recalling morally injurious events, which was thought to be linked to increased activation of the posterior insula and its connections to the viscera. The authors postulated that unpleasant visceral sensations aroused when recalling morally injurious events may, in turn, lead to increased activation of modulating brain areas such as the dorsolateral prefrontal cortex, or the central executive network, in an effort to control excessive bottom-up activity evoked from recalling morally injurious events (83). Critically, over-modulation of excessive bottom-up affect is a pattern of neural activation consistent with dissociation (82, 83). Social support, for example, may then be an important factor in processing morally injurious events as treatments focused on bottom-up affective processes and bodily sensation may encourage pro-social, attachment-based, interpersonal relationships and in turn alleviate interfering symptoms, including heightened arousal and dissociation. Further evidence is required, however, to verify the veracity of this claim and at present, it is imperative that healthcare workers receive access to evidence-based approaches to treat PTSD that, where necessary, may be augmented by evidence-informed approaches for residual symptoms in treatment-refractory cases.
An Interpersonally-Focused Approach to Moral Injury
With limited empirical data on moral injury in healthcare workers in general and during COVID-19 specifically, we look here to interpersonal factors known to influence the development and maintenance of PTSD symptoms (e.g., social support, acknowledgment and exclusion) as a starting point for potential prevention and treatment strategies. Notably, this interpersonally-focused approach to moral injury is in keeping with evidence from healthcare workers' experiences during the SARS crisis (55). Here, social support and social rejection/isolation were reported to be associated with the psychological impact that the crisis had on healthcare workers (55). Marjanovic et al. (56) found that poor organizational support was associated with avoidance and anger among nurses, a finding similar to that of Tam et al. (57) who reported that poor “team spirit” and administrators not hearing healthcare workers' feedback were associated with poor mental health (55). Similarly, Chen et al. (58) found that nurses who reported greater family support were at a lower risk of mental health problems (55). Koh et al. (59) reported increased work stress and workload among healthcare workers on the frontlines of the SARS crisis in Singapore, with many experiencing social stigmatization and ostracism from family members due to their occupation (55). Drawing on this pre-pandemic evidence in combination with Nietlisbach and Maercker's (16) work on interpersonal factors relevant to survivors of trauma with PTSD, we now provide a review of the role of perceived social support, social acknowledgment and social exclusion in relation to potential areas of targeted intervention for COVID-19-related moral injury in healthcare workers.
Perceived Social Support
Social Support and PTSD
Social support is a psychological construct referring to the emotional and instrumental care provided by those close in one's social circle, such as family or close friends (16). Whereas, seeking social support to deal with traumatic stress is a protective factor against PTSD (18), a perceived lack of social support is strongly associated with increased PTSD symptoms (60). The role of social support in mediating PTSD has been reported among many populations, including war veterans (19), survivors of childhood sexual abuse (20), survivors of violent crime (61) and nurses (21). Cieslak (19) investigated the role of perceived social support and self-efficacy in veterans' adaptations to distress. The results of this investigation revealed that greater received and perceived social support predicted high coping self-efficacy, which in turn predicted lower post-traumatic stress and depression symptom severity (19). Kerasiotis and Motta (21) investigated PTSD symptoms among nurses and found that nurses reported high levels of anxiety but did not reach clinically significant levels of PTSD, depression and dissociation. Here, social support was inferred to help nurses cope with work-related stressors (21). Finally, in a study investigating the specific types of perceived social support that mediated PTSD development in female survivors of childhood sexual abuse, self-esteem support was defined as “others' communications indicating that the abused individual is valued” (20) and was the type of social support that specifically mediated PTSD development in the sample. It is critical to acknowledge that while social support is a strong moderator of PTSD symptom development and maintenance, PTSD characteristically undermines relationships and support networks (62) as discussed above, making social relationships a key target for PTSD intervention. Moreover, PTSD is highly associated with disruptions in childhood attachment (47, 63, 64), rendering it potentially more difficult to form and sustain interpersonal relationships into adulthood.
Social support is thought to influence the cognitive appraisals of traumatic events in survivors of trauma. Specifically, social support may influence how one attributes their role in the traumatic event and their beliefs about the world (65). Cohen and Wills' (66) well-cited stress-buffering model posits that social support is a protective factor against the deleterious effects of trauma exposure as it increases one's perceived ability to cope with trauma and reduces negative appraisals of the traumatic event (22). In a study investigating social constraints, post-traumatic cognitions and PTSD among recent survivors of trauma, those who reported more social constraints (i.e., feeling unsupported, misunderstood or alienated when seeking support) reported more negative post-traumatic cognitions (67). Further, both social constraints and negative post-traumatic cognitions were related to a greater number of PTSD symptoms in this sample (67). These findings are in keeping with decades of research on the role of social support following exposure to trauma where a lack of social support continues to be a strong risk factor for developing PTSD (18, 22, 68). Further, individuals with strong social support are likely to recover faster than those who lack support (68). Indeed, in a recent meta-analytic review, Zalta et al. (22) examined the magnitude of the relation between social support and PTSD symptom severity, reporting a medium effect size across 148 cross-sectional studies and 38 longitudinal studies. The results supported the notion that greater levels of social support and lower levels of negative social reactions are related to lower levels of PTSD symptom severity (22).
Though not fully understood, the relation between social support and resilience documented in neurobiological literature may represent, in part, the mechanism through which social support moderates PTSD symptoms. The noradrenergic and hypothalamic-pituitary-adrenocortical (HPA) systems are implicated in both stress and resilience. Individuals with PTSD display dysregulated noradrenergic systems that fail to terminate the stress response after exposure to stressful stimuli (62). Individuals who report low social support display physiological and neuroendocrine responses, such as increased heart rate and blood pressure, that are indicative of a heightened reactivity to stress (69). Conversely, stress resilience is associated with the ability to keep the HPA and noradrenergic systems stable during exposure to stressful stimuli and terminated when the stimuli are no longer present (69). Social support is thought to influence both biological and environmental susceptibility to stress by acting on the HPA and noradrenergic systems, encouraging resilience (69, 70). As such, on a neurobiological level, social support may be a key factor in mediating the stress response as it promotes resilience.
Relatedly, the neurohormone oxytocin also plays a key role in stress regulation where social contact impacts the HPA axis to release oxytocin and in turn reduce stress (71–77). Indeed, studies using animal models have demonstrated that social contact is associated with oxytocin release (75–77). Furthermore, oxytocin release during or just after exposure to stressful events has been shown to regulate the HPA axis through the corticotropin-releasing factor (72, 78). Oxytocin's affinity for reducing PTSD symptoms may be related, in part, to its critical role in social bonding as oxytocin is known as the neurohormonal substrate of human affiliations, including parental, romantic and filial social bonds (79). For example, oxytocin release is implicated in maternal-infant social bonds such that oxytocin levels early in pregnancy and postpartum were related to maternal bonding behaviors such as positive affect, attachment-related thoughts and frequency of attending to the infant (80). Indeed, in a study investigating the therapeutic potential of intranasal oxytocin administration as a preventative measure for PTSD symptoms, Frijling et al. (81) found that repeated oxytocin administration reduced the development of PTSD symptoms among individuals who were recently trauma exposed. Furthermore, oxytocin has been shown to cause long-term depression of the amygdala, regulating the amygdala's sensitivity to aversive social stimuli (74). As such, the relation between social support and PTSD symptom severity may be explained, in part, due to the release of oxytocin, which is critical for social bonding and regulates the HPA axis along with subcortical structures critical to the stress response [see Lanius et al. (82) for a detailed review of the neurobiology of PTSD, including its dissociative subtype].
Healthcare Workers and Social Support During COVID-19
Research on healthcare workers' perceived social support during the pandemic is limited yet provides evidence that social support is critical for mental health and well-being. Indeed, in a systematic review of quantitative studies investigating psychological resilience, coping behaviors and social support in nurses during the pandemic (84), only seven studies explored the relation between social support and mental health outcomes, where greater perceived social support yielded a reduction in burnout (84, 85) and explained variance in psychological distress (84, 86). Using qualitative interviews, Brophy et al. (87) explored Canadian healthcare workers' experiences during the initial months of the pandemic, reporting that a perceived lack of support from employers affected healthcare workers' sense of well-being (e.g., a co-worker being sent to care for a suspected COVID-19 patient without PPE). Similarly, Xiao et al. (88) explored the impact of social support on sleep quality and functioning in a sample of Chinese healthcare workers providing medical care during the pandemic. Social support not only decreased anxiety and stress, but also increased self-efficacy in this sample (88). Finally, Labrague and De los Santos (89) examined the role of resilience, social support and organizational support on COVID-19-related anxiety among nurses working on the frontlines in the Philippines. Here, whereas social support was defined as assistance and protection offered by colleagues, managers, friends and family, organizational support was defined as the degree to which resources, reinforcement, communication and encouragement were offered to an individual by their organization (89). Both social and organizational support significantly predicted COVID-19-related anxiety among this sample, such that greater degrees of these supports were associated with lower degrees of anxiety (89).
In recent surveys of healthcare workers' needs during the pandemic, healthcare workers have highlighted their desire for social support. For example, Shanafelt et al. (90) asked healthcare workers about their main concerns during the pandemic, their needs from leaders and their perspectives on tangible supports. Healthcare workers' requests were summarized as follows: hear me, protect me, prepare me, support me and care for me. Healthcare workers desire clear assurance from their leaders that they, along with their families, will be supported emotionally, physically and socially while working on the frontlines on the pandemic (90). Specifically, healthcare workers shared a desire for their expert perspectives to be included in decision making, for their risk of infection to be mitigated, for appropriate training to treat critically ill patients, for support in dealing with extreme work hours and distress and for practical support such as food and childcare aid should they be infected (90). This call for support was echoed in a recent review by Heber et al. (91) who reported that public safety personnel (PSP) who, like healthcare workers, face novel stressors while working during the pandemic (e.g., greater risk of infection compared to civilians), may benefit from consistent support offered in the form of specialized mental health and preparedness training, frequent and transparent communication, strong leadership and team building, assistance in navigating quarantine and focus on self-care.
Altogether, social support mediates PTSD symptoms in a range of populations, perhaps through influencing cognitive appraisals of events by survivors of trauma (i.e., buffering patterns of common emotional response to trauma, enhancing feelings of connectedness) and likely enhancing resiliency on a neurobiological level [i.e., increasing the availability of neurohormones associated with stress reduction, in turn, regulating the HPA axis and critical subcortical structures associated with trauma and stress; (63–65, 67, 69, 70, 84). Given the relation between moral injury and PTSD symptoms and emerging mental health data suggesting that social support is important for decreasing healthcare workers' anxiety and stress during pandemic situations, targeting perceived social support is one means by which organizations and individuals may mediate the morally injurious outcomes for healthcare workers exposed to PMIEs during the COVID-19 pandemic. This may be accomplished by creating Communities of Practice where healthcare workers may gather in person and/or virtually to discuss shared concerns and coping mechanisms, or by ensuring that healthcare workers have regular breaks to spend with family members or creating “buddy systems.” Similarly, the need for efforts to retain a healthcare workforce that is increasingly considering leaving the profession given experiences throughout the pandemic (92, 93) combined with our own preliminary qualitative findings that healthcare workers demonstrate more concern for team members and family members than themselves, we suggest that efforts to retain healthcare staff and to promote workplace wellness focus, to an extent, on teams and team well-being. Strengthening these connections by highlighting social cohesion with team members may facilitate retention and promote post-traumatic growth. These efforts may also focus on the identity of the healthcare worker as a helping professional and serve as a reminder of why the healthcare worker entered the field in the first place.
Perceived Social Acknowledgment
Social Acknowledgment and PTSD
Social acknowledgment involves receiving appreciation and positive reactions from the wider social environment in recognition of the difficult situation experienced by individuals exposed to trauma (16). The social environment may include colleagues, neighbors, authorities, clergy and the media (94). Social acknowledgment differs from social support as the former measures the degree to which one feels recognized and understood as a survivor of trauma and the latter emphasizes emotional or instrumental care (95).
Poor social acknowledgment (i.e., receiving disapproval and a lack of recognition as a survivor of trauma) is associated with greater severity of PTSD (95). For example, in a study examining PTSD symptom trajectories for Red Cross volunteers in Indonesia who responded to a large earthquake, those in the chronic PTSD trajectory reported lower perceived social acknowledgment compared to those in the resilient trajectory (96). Furthermore, a lack of social acknowledgment predicted increased PTSD symptomology in a longitudinal study on predictors of PTSD recovery in survivors of crime (97). In a study investigating trauma and PTSD symptomatology in German developmental aid workers, some participants reported that experiencing general disapproval from others was associated with more severe intrusive thoughts about the traumatic event and increased hyperarousal (94). Finally, a study on PTSD symptom severity, disclosure attitudes and social acknowledgment among Chinese and German survivors of crime found that, although PTSD symptom severity differed cross-culturally, disclosure attitudes and social acknowledgment predicted PTSD severity in both groups where a reluctance to disclose and a perceived lack of social acknowledgment predicted greater PTSD severity (97).
One mechanism through which social acknowledgment may mediate PTSD symptom development and maintenance is similar to that of social support, namely, post-traumatic cognitions. Post-traumatic cognitions are recognized as strong predictors of PTSD (97). Whereas, a strong sense of social acknowledgment may help survivors of trauma affirm positive cognitions that a traumatic experience has damaged, poor social acknowledgment may foster negative self- and other-focused cognitions (95). Indeed, Mueller et al. (97) found that perceived social acknowledgment was negatively associated with post-traumatic cognitions in a sample of 86 survivors of crime.
Here, it is critical to note evidence of altered patterns of response to emotions among individuals with PTSD that may pose as a barrier to the reception of social acknowledgment. For example, Nazarov et al. (98) found evidence for altered comprehension of affective prosody among women with PTSD related to chronic child abuse. Women in this study were asked to recognize angry, fearful, sad and happy emotions on a computer-based task and also asked to identify if the emotions portrayed in consecutive excerpts were the same or different. Nazarov et al. (98) found that women with PTSD took longer to identify all emotions except for those portraying anger in comparison to healthy controls. Interestingly, women with PTSD who experienced dissociative symptoms were more likely to be less accurate in discriminating between consecutive emotional presentations (98). Further, greater severity of childhood trauma was related to poorer accuracy in discrimination as well as slower recognition of emotions (98). Consistent with the altered patterns of emotional response demonstrated by Nazarov et al. (98), alterations in ToM, emotional recognition, empathic reasoning, moral reasoning and social behavior have been demonstrated among individuals with PTSD, as described above (15, 17, 43–45). As such, altered patterns of emotional response in PTSD must be considered when evaluating interventions targeting social acknowledgment.
Healthcare Workers and Social Acknowledgment During COVID-19
Research on healthcare workers' perceived social acknowledgment during the pandemic is limited, with the majority of work instead focused heavily on social support from familiar others, such as co-workers. A small number of studies, however, have explored healthcare workers perceptions surrounding a lack of recognition for their efforts during the COVID-19 pandemic. For example, some healthcare workers have described feeling abandoned by political leaders and have attributed inadequate staffing and PPE during the pandemic to political leaders' poor response to their needs during the crisis (26, 99). Relatedly, in a recent systematic review and meta-synthesis on frontline healthcare workers' experiences during pandemics and epidemics (e.g., COVID-19, SARS, MERS, Ebola), Billings et al. (100) reported that workers felt abandoned and betrayed by organizations when they did not received promised financial renumeration for their service and sacrifice on the frontlines. Kröger (26) stated further that healthcare workers may perceive an inconsistent world outside of the hospital when witnessing people carelessly ignoring safety measures. Despite window decorations in homes and businesses thanking healthcare workers for their service, healthcare workers may perceive the non-chalance of people in their communities as a lack of recognition for their sacrifice on the frontlines. Finally, Cai et al. (99) investigated the psychological impact and coping strategies of healthcare workers in China and found that recognition from management and the government was associated with psychological benefit. Preliminary findings from our research groups' ongoing interviews with healthcare workers throughout 2021 corroborate the perceived lack of recognition discussed in the literature where nurses discussed feeling underappreciated at the beginning of the pandemic when financial renumeration for their service was smaller in proportion to that offered to some first responders. Unsurprisingly, we also heard from some healthcare workers that they felt abandoned and described a lack of recognition from the community when protests against masks and vaccines were held outside the hospital.
As social acknowledgment plays a role in the development and maintenance of PTSD symptoms in various trauma-exposed groups, it is imperative that healthcare workers perceive that they are recognized and understood as survivors of trauma during the COVID-19 pandemic. This perception may influence positive post-traumatic cognitions that may ameliorate moral injury as a response to COVID-19-related-PMIEs. Indeed, in outlining how healthcare workers desire strong leadership to support them during the pandemic, Shanafelt et al. (90) note the critical role of leadership asking healthcare workers about their concerns and acknowledging their requests. Despite potentially being constrained from providing answers, leadership must demonstrate that healthcare workers' service is acknowledged and appreciated (90). This call for strong leadership was echoed by Jetly et al. (1) who discussed key qualities of effective leadership in the military that may prove useful for leaders attending to COVID-19-related moral injury in healthcare workers. Jetly et al. (1) propose that effective leadership listens to the concerns of subordinates, are positive yet not overly optimistic, respect their subordinates' values, recognize that the risk of COVID-19 infection is not evenly distributed as frontline workers are the most vulnerable at this time, care about those whom they lead and accept the blame for team failures while attributing success to their team members.
Perceived Social Exclusion
Social Exclusion and PTSD
Social exclusion is an act of ostracism related to stigmatization where one is rejected and isolated from a group (16). Humans have an inherent need for relationships with others that is disturbed in situations of social exclusion (101). Social exclusion may lead to feelings of isolation as if one were no longer viewed as a part of society (16). When ostracized, survivors of trauma may perceive themselves as less-human and believe that they are perceived to be less-human by the perpetrator of their ostracism (101). Social exclusion or ostracism can lead to physiological changes, such as cardiovascular issues or increased cortisol levels and psychological issues, including negative emotions of anger, sadness and shame (102, 103).
Individuals suffering from PTSD and other mental illnesses are often victims of social exclusion in the form of stereotyping and stigmatization (104). For example, among East-African conflict survivors, stigmatization was associated with an increased likelihood of PTSD after exposure to trauma (105). Wesselmann et al. (103) investigated the relation between perceived ostracism (i.e., “being ignored and excluded”) and post-traumatic stress among military veterans and found that perceived ostracism was related to post-traumatic stress symptoms, anxiety and psychological distress. Further, perceived ostracism explained variance in post-traumatic stress symptoms apart from theoretically relevant variables (i.e., deployment stress and social support) (103). In a study investigating the effects of social exclusion between individuals with PTSD and control participants, those with PTSD reported greater perceived social exclusion than control participants in an experimental manipulation of inclusion and exclusion (106), perhaps underscoring evidence of impaired social cognition among individuals with PTSD. Finally, among female adolescents exposed to war-related trauma, those who experienced sexual violence reported increased stigmatization (i.e., feeling treated worse than others, being insulted, rejected and excluded from family or community) (107). Further, stigmatization explained symptoms of depression and post-traumatic stress more so than did the direct impact of sexual violence in this sample (107).
Healthcare Workers and Social Exclusion During COVID-19
Healthcare workers may perceive themselves to be socially excluded during the pandemic. In acknowledgment of the stigmatization that healthcare workers may experience by their communities during disease outbreaks, Taylor et al. (108) conducted a North American study evaluating non-healthcare workers' attitudes toward healthcare workers serving during COVID-19 and found that more than one quarter of respondents believed that healthcare workers should be subject to severe restrictions, including isolation from communities and families. Further, one-third of the respondents reported avoiding healthcare workers due to fear of infection (108). Indeed, Kröger (26) highlighted how healthcare workers have been prohibited from certain public spaces including bringing their children to school and Shimizu and Lin (109) recounted instances of defamation against healthcare workers in Japan during the pandemic. Individuals affected by COVID-19 in Japan have experienced societal rejection, discrimination and stigmatization and since healthcare workers are at a high risk of infection due to contact with COVID-19 patients, they are more likely to suffer from social exclusion (110). Reports indicate that Japanese healthcare workers have been victims of discrimination and abuse outside of work as the public treats them as “germs” (109). Healthcare workers in Japan have also been denied access to public transportation and their families have fallen victim to discrimination as well (109). In Canada, a national news organization reported on two nurses' experiences of facing criticism for crossing the border to provide care at a hospital in Detroit. The nurses described being blamed for bringing COVID cases into their city as they worked to be a part of the solution by caring for COVID-19 patients (111). Furthermore, Dye et al. (112) conducted a survey of healthcare workers' experiences of COVID-19-related bullying and stigma with participants from across 173 countries, reporting that healthcare workers were experiencing social exclusion during the pandemic, especially in communities affected by the intersection of racism, violence and police involvement (112).
In sum, social exclusion violates the inherent human need for relationships, consequently generating physiological and psychological disturbances. The effects of social exclusion in the form of stigmatization have been documented among various populations such as war veterans (103), survivors of sexual violence (107) and survivors of conflict (105). Our research group is currently preparing a scoping review on healthcare workers' and public safety personnel's exposure to PMIEs and distressing experiences during the pandemic. Here, we identified a need for further investigation of the verbal and physical abuse that healthcare workers have experienced in order to understand the context and severity of such exposures globally. As social exclusion is implicated in the development and maintenance of PTSD symptoms, targeting healthcare workers' perceptions of social exclusion may be an effective strategy to prevent and treat COVID-19-related moral injury.
Discussion
In Litz et al.'s (10) conceptual model of moral injury, it is clear that an individual's social world is expected to mediate their response to PMIEs. Indeed, this model postulates that the degree of dissonance an individual initially experiences post-PMIE will be moderated by others' reactions. In addition, stable, internal and global attributions may be countered when an individual has others in their environment to offer interpretations of events that lead to self-forgiveness rather than self-condemnation (10). Targeting perceived social support, acknowledgment and inclusion may be an opportunity for PMIE-exposed healthcare workers to reconcile dissonant cognitions of their beliefs about the world and their experiences. Here, this targeted approach may aid the individual in processing intense moral emotions and deter them from social withdrawal, which may otherwise manifest into symptoms of moral injury such as self-condemnation, overwhelming shame, guilt, anger, anhedonia and/or PTSD symptoms. For example, social exclusion may play a critical role in how healthcare workers evaluate themselves after experiencing perpetration-based PMIEs during the COVID-19 pandemic. In interviews our research group has conducted with healthcare workers throughout 2021, healthcare workers have described excessive guilt when not able to attend to patients quickly enough due to changing out of and into PPE. If an individual in this situation is subsequently ostracized from colleagues or receives condemning information from close individuals in their life regarding their actions, these reactions may strengthen beliefs such as “I am a bad person” and “I am responsible for the patient's death”, contributing to the sequalae of moral injury postulated by Litz et al. (10).
Relatedly, social support and acknowledgment may not only be factors that mediate morally injurious outcomes among those who are exposed to PMIEs, but may also inherently constitute PMIEs for some healthcare workers during the pandemic. For example, in a recent review of frontline healthcare workers' perspectives on working during pandemics and epidemics (e.g., COVID-19, SARS, Ebola), Billings et al. (100) discussed how healthcare workers valued support from their organizations and perceived the organization to have “an institutional duty to provide staff with sufficient protection to work safely” (pg. 10). Healthcare workers may feel betrayed by their organization when they are sent to care for COVID-19 patients without appropriate PPE (87) or when they feel unheard by leaders (91) who establish procedures and policy with which workers do not agree. Finally, actions or inactions that communicate to healthcare workers that their efforts on the frontlines are not recognized or appreciated [e.g., lack of inclusion in financial compensation; (100)] may constitute betrayal-based PMIEs for some healthcare workers. Thus, healthcare organizations must carefully consider the ways in which their operations may betray their employees in addition to recognizing that, as a trusted authority to their healthcare workers, they have the ability and responsibility to support workers and mitigate the effects of moral injury through means of social support and acknowledgment.
An important consideration in translating research on interpersonal factors in PTSD to moral injury, however, is that moral injury by definition may involve witnessing morally transgressive acts and/or an individual enacting the moral harm themselves. Thus, the utility of addressing social support, acknowledgment and exclusion in moral injury may need to be strategically implemented to accommodate for both personally transgressed and witnessed PMIEs, which has not been explored in the PTSD literature. This tailored approach will mimic research that has adapted traditional PTSD treatments to better suit the experience of those with moral injury (11, 35). With this consideration, it is necessary for future studies to continue to investigate the boundaries between moral injury and PTSD as well as the ways in which a social cognitive model can inform treatment interventions.
An interpersonally-focused approach to understanding and mitigating moral injury in healthcare workers during COVID-19 is consistent with a recent call for moral injury treatments to move beyond psychotherapy and include an affirmative community effort (11). This approach must include both individual and organization considerations that take into account the unqiue indiviudal in their specific social environement. Indeed, Billings et al. (100) highlighted the importance of the social environment when reviewing the experiences of frontline healthcare workers affected by stigma and discrimination in their communities. Here, healthcare workers reported feeling supported by their orgnizations at times (e.g., when communication was clear, when buddy systems were established between expereinced and new staff) and unsupported at other times (e.g., when staff safety was not a clear priority, when they felt coerced to caring for infected paitents). Below, we synthesize and disucss ciritical considerations for bolstering against the deliterious imapcts of moral injury in healthcare workers at both the indiviudal and organizaiton level.
Individual Considerations
In line with the recommendations made in the recent Moral Injury Guide prepared by the Centre of Excellence on PTSD (113), we offer the following individual level considerations to buffer against the deleterious impacts of moral injury for healthcare workers during the COVID-19 pandemic.
At the individual level, it is important to consider risk and resilience factors that may affect one's likelihood of developing moral injury after exposure to a PMIE. Williamson et al. (114) highlighted risk factors for moral injury in the military, which may be pertinent to healthcare workers during the pandemic, including loss of life to a vulnerable person (e.g., elderly, children), perception of leaders not taking responsibility for events or being unsupportive, staff feeling unprepared for the emotional or psychological impacts of decisions, concurrent exposure to other traumatic events and a lack of social support after exposure to a PMIE. Furthermore, our research group has shown that emotional abuse during childhood (115, 116) and emotional regulation (116) are critical factors related to moral injury. Battaglia et al. (115) examined the relation between childhood abuse and moral injury among members of the Canadian Armed Forces (CAF) and found that emotional abuse in childhood may increase the likelihood of moral injury among adults in the CAF (115). Further, Roth and colleagues (116) demonstrated that exposure to adverse childhood experiences was associated with both moral injury and trauma-related symptoms among PSP, but emotion regulation skills buffered moral injury (116). Thus, whereas healthcare workers who are survivors of childhood trauma may be at an elevated risk for moral injury, those with strong emotion regulation skills may have the necessary resilience to buffer against the development of moral injury.
Healthcare workers who identify with a minority group (e.g., gender, sexual orientation, or racial/ethnic group) may also be at an elevated risk for moral injury during the pandemic due to the compacting nature of minority stress (i.e., stress associated with discrimination or marginalization) with COVID-19-related stressors. The Centre of Excellence on PTSD's moral injury guide (113) highlighted that racialized individuals are at a higher risk of COVID-19 exposure, infection and severe outcomes due to racial disparities in income and poverty. Further, racialized healthcare workers may deal with stressors related to systemic racism in addition to the stressors associated with providing care during COVID-19. For example, racialized healthcare workers may experience racism from patients and colleagues, may witness colleagues make racist comments about patients, may feel compelled to protect racialized patients from racism, may face skepticism about their training and competence, may experience belittlement of their speech, appearance, religion or cultural practices and may be called upon to educate others about systemic racism (113). As a result, racialized healthcare workers may be at an increased risk of experiencing distress and moral injury during the pandemic in comparison to their non-racialized counterparts. It is vital to acknowledge the unique stressors that healthcare workers who identify with minority groups may face in relation to discrimination and marginalization and consider these impacts when developing interventions for COVID-19-related moral injury.
Based on Heber at al.'s (91) recommendations for PSP to support themselves during COVID-19, healthcare workers may benefit from taking time to practice self-care in the form of healthy coping and seeking connections and help. For example, frontline workers should prioritize sleep, nutrition, hydration and exercise, stress management, relaxation, maintaining/establishing routines, connecting with friends, family and co-workers and seeking informal and formal supports as needed (91). These individual recommendations were echoed in the Centre of Excellence on PTSD's guide to moral injury (113), which additionally recommends that healthcare workers gain education about moral stressors, moral injury, relaxation therapy and mindfulness or meditation to reduce stress.
Organizational Considerations
Cohen and Wills' (66) stress-buffering model contends that a specific match between trauma and the subsequent social support is necessary for social support to reduce the harmful psychological responses associated with trauma exposure. Thus, in the context of COVID-19, healthcare organizations must play a critical role in supporting healthcare workers to buffer against moral injury as their workers look to leadership for guidance in these unprecedent times. In line with the recommendations made in the recent Moral Injury Guide prepared by the Centre of Excellence on PTSD (113), we offer the following organizational level considerations for leaders to consider in an effort to buffer against the deleterious impacts of PMIE exposure and moral injury as an outcome for healthcare workers during the COVID-19 pandemic. Recommendations for organizations to support healthcare workers include: offering clear, positive yet realistic information; establishing peer support networks among healthcare workers where team cohesion is emphasized; time and space to rest and discuss experiences; encouraging self-forgiveness and re-integration of moral transgressions into one's moral code; honest discussions about the moral requirements of working during a pandemic; leaders taking responsibility to ensure that staff are prepared for the emotional consequences of their work and are aware of vicarious traumatization and relevant coping strategies; peer support teams to provide psychological first aid; encouraging staff to utilize employee assistance programs, chaplaincy, or other levels of support; intentionally expressing gratitude to frontline workers; offering accessible professional resources; rotating staff between high and low stress roles; optimizing the work environment for appropriate breaks; educating healthcare workers on PMIEs and the possible morally injurious outcomes that may be experienced after exposure (e.g., overwhelming moral emotions of anger, guilt, shame betrayal; self-condemnation, anhedonia, social withdrawal), encouraging self-assessments for risks of moral injury and formal screening for PTSD, as well as receiving evidenced-based treatment, if required (113, 117–121). Critically, some healthcare workers may show signs of distress, yet deny or lack insight into these difficulties and refuse help (122). Healthcare workers involved in previous pandemics and epidemics did not fully voice their needs or seek supports until after the peak of the crisis (100). As such, it is essential that orgnaizations continiously offer and encourage staff to prioritize their mental health during and beyond the COVID-19 pandemic, even in the absence of explicit requests for this support.
Limitations
While a thorough search of the literature was conducted in preparing this review, it must be acknowledged that the present review is limited by its narrative structure, which inherently is unsystematic and is consequently associated with bias. The purpose of this review was to synthesize literature on different topics (e.g., social cognition, PTSD, moral injury) to present the notion of an interpersonally-focused approach to COVID-19-related moral injury in healthcare workers. Though it has limitations, a narrative review was the most appropriate type of review for this work (123). The present review is additionally limited by the paucity of empirical research surrounding moral injury in healthcare workers and a lack of consensus on moral injury as a clinical phenomenon. As moral injury has historically been situated in the military context, there remains a need for research on the types of events that may be experienced by healthcare workers as PMIEs, as well as the outcomes associated with these exposures, to better characterize healthcare workers' experiences and arrive at a definition for moral injury in this population. Future research should consider a systematic review of the literature on moral injury in healthcare workers as data becomes available to reduce bias and synthesize knowledge on moral injury in this population.
Conclusion
In summary, many healthcare workers have faced morally and ethically challenging situations throughout the COVID-19 pandemic that place them at an elevated risk for moral injury. The relation between moral injury and PTSD, although not fully understood, suggests that the two are related yet distinct responses to trauma. Alterations in social cognitive functioning that may contribute to interpersonal difficulties in PTSD render interpersonal factors such as social support, acknowledgment and exclusion important in moderating PTSD symptomology. Existing research on the interpersonal factors that moderate PTSD symptom development and maintenance, then, may prove to be a useful starting point for preventing and, where necessary, treating moral injury in healthcare workers during the COVID-19 pandemic. We urge researchers and clinicians to consider carefully a social cognitive and interpersonal lens in relation to ongoing research on moral injury in healthcare workers during the COVID-19 pandemic and beyond. Healthcare organizations should follow the available recommendations to support healthcare workers at this time to bolster against moral injury.
Author Contributions
AD'A: conceptualization, writing (original draft), review, and editing. KR and RM: conceptualization and review and editing. RL, AH, PS, AM, HS, CO'C, FH, and SR: review and editing. MM and RL: conceptualization, writing, review and editing, and funding acquisition. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by research grants from the Veteran's Affairs Canada supported Centre of Excellence on PTSD, Defense Canada, and the Canadian Institute of Health Research (grant number: MVP-171647) to MM and RL, along with a generous donation from Homewood Health Incorporated to Homewood Research Institute. MM was supported by the Homewood Chair in Mental Health and Trauma at McMaster University. RL was supported by the Harris-Woodman Chair in Psyche and Trauma at Western University of Canada.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors would like to acknowledge that healthcare workers around the globe have placed themselves and their families at great risk during this time and also like to thank frontline healthcare workers and staff for their heroic efforts and sacrifices in providing care to those in need during the COVID-19 pandemic.
References
1. Jetly R, Vermetten E, Easterbrook B, Lanius R, McKinnon M. Going to “war”: Military approach as the antidote to defeating COVID-19. Military Behav Health. (2020) 8:243–7. doi: 10.1080/21635781.2020.1765911
2. Litz BT, Kerig PK. Introduction to the special issue on moral injury: Conceptual challenges, methodological issues, and clinical applications. J Traumatic Stress. (2019) 32:341–9. doi: 10.1002/jts.22405
3. Nazarov A, Jetly R, McNeely H, Kiang M, Lanius R, McKinnon MC. Role of morality in the experience of guilt and shame within the armed forces. Acta Psychiatria Scand. (2015) 132:4–19. doi: 10.1111/acps.12406
4. Protopopescu A, Boyd JE, O'Connor C, Rhind SG, Jetly R, Lanius RA, et al. Examining the associations among moral injury, difficulties with emotion regulation, and symptoms of PTSD, depression, anxiety, and stress among Canadian military members and Veterans: A preliminary study. J Military Veteran Family Health. (2021) 7:71–80. doi: 10.3138/jmvfh-2020-0036
5. Williamson V, Stevelink SAM, Greenberg N. Occupational moral injury and mental health: Systematic review and meta-analysis. Br J Psychiatry. (2018) 212:339–46. doi: 10.1192/bjp.2018.55
6. Currier JM, Holland JM, Malott J. Moral injury, meaning making, and mental health in returning veterans. J Clin Psychol. (2015) 71:229–40. doi: 10.1002/jclp.22134
7. Drescher KD, Foy DW, Kelly C, Leshner A, Schutz K, Litz B, et al. An exploration of the viability and usefulness of the construct of moral injury in war veterans. Traumatology. (2011) 17:8–13. doi: 10.1177/1534765610395615
8. Ray TN, Hunsanger JA, Nagy SM, Pickett SM. Potentially morally injurious events and depression symptoms among a trauma-exposed sample: Examining the roles of interpersonal needs and emotion dysregulation. Stress Health. (2021) 37:151–61. doi: 10.1002/smi.2981
9. Barnes HA, Hurley RA, Taber KH. Moral injury and PTSD: Often co-occurring yet mechanistically different. J Neuropsychiatry Clin Neurosci. (2019) 31:A4–103. doi: 10.1176/appi.neuropsych.19020036
10. Litz BT, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, et al. Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clin Psychol Rev. (2009) 29:695–706. doi: 10.1016/j.cpr.2009.07.003
11. Griffin BJ, Purcell N, Burkman K, Litz BT, Bryan CJ, Schmitz M, et al. Moral injury: An integrative review. J Traumatic Stress. (2019) 32:350–62. doi: 10.1002/jts.22362
12. Bryan CJ, Bryan AO, Roberge E, Leifker FR, Rozek DC. Moral injury, posttraumatic stress disorder, and suicidal behavior among National Guard personnel. Psychol Trauma. (2018) 10:36–45. doi: 10.1037/tra0000290
13. Kopacz MS, Ames D, Koenig HG. It's time to talk about physician burnout and moral injury. Lancet Psychiatry. (2019) 6:e28. doi: 10.1016/S2215-0366(19)30385-2
14. Levi-Belz Y, Dichter N, Zerach G. Moral injury and suicide ideation among Israeli combat veterans: The contribution of self-forgiveness and perceived social support. J Interpersonal Violence. (2020) 37:NP1031-NP1057. doi: 10.1177/0886260520920865
15. Couette M, Mouchabac S, Bourla A, Nuss P, Ferreri F. Social cognition in post-traumatic stress disorder: A systematic review. Br J Clin Psychol. (2020) 59:117–38. doi: 10.1111/bjc.12238
16. Nietlisbach G, Maercker A. Social cognition and interpersonal impairments in trauma survivors with PTSD. Journal of Aggression Maltreatment and Trauma. (2009) 18:382–402. doi: 10.1080/10926770902881489
17. Mazza M, Giusti L, Albanese A, Mariano M, Pino MC, Roncone R. Social cognition disorders in military police officers affected by posttraumatic stress disorder after the attack of An-Nasiriyah in Iraq 2006. Psychiatry Res. (2012) 198:248–52. doi: 10.1016/j.psychres.2011.11.027
18. Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychol Bull. (2003) 129:52–73. doi: 10.1037/0033-2909.129.1.52
19. Cieslak R, Shoji K, Luszczynska A, Taylor S, Rogala A, Benight CC. Secondary trauma self-efficacy: Concept and its measurement. Psych Assessment. (2013) 25:917–28. doi: 10.1037/a0032687
20. Hyman O. Perceived social support and secondary traumatic stress symptoms in emergency responders. J Traumaitc Stress. (2004) 17:149–56. doi: 10.1023/B:JOTS.0000022621.27014.0e
21. Kerasiotis B, Motta RW. Assessment of PTSD symptoms in emergency room, intensive care unit, and general floor nurses. Int J Emergency Mental Health. (2004) 6:121–33.
22. Zalta AK, Tirone V, Orlowska D, Blais RK, Lofgreen A, Klassen B, et al. Examining moderators of the relationship between social support and self-reported PTSD symptoms: A meta-analysis. Psychol Bull. (2021) 147:33–54. doi: 10.1037/bul0000316
23. Hamric AB. Empirical research on moral distress: Issues, challenges, and opportunities. HEC Forum. (2012) 24:39–49. doi: 10.1007/s10730-012-9177-x
24. Whitehead PB, Herbertson RK, Hamric AB, Epstein EG, Fisher JM. Moral distress among healthcare professionals: Report of an institution-wide survey. J Nursing Scholarship. (2015) 47:117–25. doi: 10.1111/jnu.12115
25. Epstein EG, Whitehead PB, Prompahakul C, Thacker LR, Hamric AB. Enhancing understanding of moral distress: The Measure of Moral Distress for Health Care Professionals. AJOB Empir Bioeth. (2019) 10:113–24. doi: 10.1080/23294515.2019.1586008
26. Kröger C. Shattered social identity and moral injuries: Work-related conditions in health care professionals during the COVID-19 pandemic. Psychol Trauma. (2020) 12:S156–8. doi: 10.1037/tra0000715
27. Cartolovni A, Stolt M, Scott PA, Suhonen R. Moral injury in healthcare professionals: A scoping review and discussion. Nurs Ethics. (2021) 28:590–602. doi: 10.1177/0969733020966776
28. Hossain F, Clatty A. Self-care strategies in response to nurses' moral injury during COVID-19 pandemic. Nurs Ethics. (2021) 28:23–32. doi: 10.1177/0969733020961825
29. Borges LM, Barnes SM, Farnsworth JK, Bahraini NH, Brenner LA. A commentary on moral injury among health care providers during the COVID-19 pandemic. Psychol Trauma. (2020) 12:S138–40. doi: 10.1037/tra0000698
30. Hines SE, Chin KH, Glick DR, Wickwire EM. Trends in moral injury, distress, and resilience factors among healthcare workers at the beginning of the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:488. doi: 10.3390/ijerph18020488
31. Hines SE, Chin KH, Levine AR, Wickwire EM. Initiation of a survey of healthcare worker distress and moral injury at the onset of the COVID-19 surge. Am J Ind Med. (2020) 63:830–3. doi: 10.1002/ajim.23157
32. Amsalem D, Lazarov A, Markowitz JC, Naiman A, Smith TE, Dixon LB, et al. Psychiatric symptoms and moral injury among US healthcare workers in the COVID-19 era. BMC Psychiatry. (2021) 21:546. doi: 10.1186/s12888-021-03565-9
33. Currier JM, Farnsworth JK, Drescher KD, McDermott RC, Sims BM, Albright DL. Development and evaluation of the expressions of moral injury scale-military version. Clin Psychol Psychotherapy. (2018) 25:474–88. doi: 10.1002/cpp.2170
34. Currier JM, Drescher KD, Nieuwsma J. Addressing Moral Injury in Clinical Practice. Washington, DC: American Psychological Association (2021). doi: 10.1037/0000204-000
35. Murray H, Ehlers A. Cognitive therapy for moral injury in post-traumatic stress disorder. Cogn Behav Ther. (2021) 14:e8. doi: 10.1017/S1754470X21000040
36. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed. Virgina: American Psychiatric Publishing (2013).
37. Maguen S, Burkman K. Combat-related killing: Expanding evidence-based treatments for PTSD. Cognit Behav Practice. (2013) 20:476–9. doi: 10.1016/j.cbpra.2013.05.003
38. Steenkamp MM, Nash WP, Lebowitz L, Litz BT. How best to treat deployment-related guilt and shame: Commentary on Smith, Duax, and Rauch. Cognit Behav Practice. (2013) 20:471–5. doi: 10.1016/j.cbpra.2013.05.002
39. Harricharan S, McKinnon MC, Lanius RA. How processing of sensory information from the internal and external worlds shape the perception and engagement with the world in the aftermath of trauma: Implications for PTSD. Front Neurosci. (2021) 15:360. doi: 10.3389/fnins.2021.625490
40. McKinnon MC, Boyd JE, Frewen PA, Lanius UF, Jetly R, Richardson JD, et al. A review of the relation between dissociation, memory, executive functioning and social cognition in military members and civilians with neuropsychiatric conditions. Neuropsychologia. (2016) 90:210–34. doi: 10.1016/j.neuropsychologia.2016.07.017
41. Sharp C, Fonagy P, Allen JG. Posttraumatic stress disorder: A social-cognitive perspective. Clin Psychol Sci Practice. (2012) 19:229–40. doi: 10.1111/cpsp.12002
42. Resick PA, Monson CM, Chard KM. Cognitive Processing Therapy: Veteran/Military Version. Washington, DC: Department of Veterans Affairs (2007). doi: 10.1037/e514742018-001
43. Nazarov A, Walaszczyk V, Frewen P, Oremus C, Lanius R, McKinnon MC. Moral reasoning in women with posttraumatic stress disorder related to childhood abuse. Eur J Psychotraumatol. (2016) 7:1. doi: 10.3402/ejpt.v7.31028
44. Poljac E, Montagne B, de Haan EHF. Reduced recognition of fear and sadness in post-traumatic stress disorder. Cortex. (2011) 47:974–80. doi: 10.1016/j.cortex.2010.10.002
45. Sherman MD, Smith JLG, Larsen JL, Gewirtz A. Veterans' perceptions of the impact of PTSD on their parenting and children. Psychol Serv. (2016) 13:401–10. doi: 10.1037/ser0000101
46. Kandalaft MR, Didehbani N, Cullum CM, Krawczyk DC, Allen TT, Tamminga CA, et al. The Wechsler ACS Social Perception Subtest: A preliminary comparison with other measures of social cognition. J Psychoeduc Assessment. (2012) 30:455–65. doi: 10.1177/0734282912436411
47. Parlar M, Frewen P, Nazarov A, Oremus C, MacQueen G, Lanius R, et al. Alterations in empathic responding among women with posttraumatic stress disorder associated with childhood trauma. Brain Behav. (2014) 4:381–9. doi: 10.1002/brb3.215
48. Bisson JI, Berliner L, Cloitre M, Forbes D, Jensen TK, Lewis C, et al. The international society for trauamtic stress studies new guidelines for the prevention and treatment of posttraumatic stress disorder: methodology and development process. J Trauma Stress. (2019) 32:475–83. doi: 10.1002/jts.22421
49. Ogden P, Pain C, Fisher J. A sensorimotor approach to the treatment of trauma and dissociation. Psychiatr Clin North Am. (2006) 19:263–79. doi: 10.1016/j.psc.2005.10.012
50. Brand BL, Schielke HJ, Schiavone F, Lanius R. Finding Solid Ground: Overcoming Obstacles in Trauma Treatment. Oxford: Oxford University Press (2020).
51. Schielke HJ, Brand BL, Lanius RA. The Finding Solid Ground Program Workbook: Overcoming Obstacles in Trauma Recovery. Oxford: Oxford University Press (2020).
52. Dalenberg CJ, Brand BL, Loewenstein RJ, Frewen PA, Spiegel D. Inviting scientific discourse on traumatic dissociation: Progress made and obstacles to further resolution. Psychol Inj Law. (2020) 13:135–54. doi: 10.1007/s12207-020-09376-9
53. Lanius UF, Paulsen SP, Corrigan FM. Neurobiology and Treatment of Traumatic Dissociation. New York, NY: Springer (2014). doi: 10.1891/9780826106322
54. Corrigan F, Grand D. Brainspotting: Recruiting the midbrain for accessing and healing sensorimotor memories of traumatic activation. Med Hypotheses. (2013) 80:759–66. doi: 10.1016/j.mehy.2013.03.005
55. Brooks SK, Dunn R, Amlôt R, Rubin GJ, Greenberg N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J Occupational Environ Med. (2018) 60:248–57. doi: 10.1097/JOM.0000000000001235
56. Marjanovic Z, Greenglass ER, Coffey S. The relevance of psychosocial variables and working conditions in predicting nurses' coping strategies during the SARS crisis: An online questionnaire survey. Int J Nursing Stud. (2007) 44:991–8. doi: 10.1016/j.ijnurstu.2006.02.012
57. Tam CWC, Pang EPF, Lam LCW, Chiu HFK. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: Stress and psychological impact among frontline healthcare workers. Psychol Med. (2004) 34:1197–204. doi: 10.1017/S0033291704002247
58. Chen CS, Wu HY, Yang P, Yen CF. Psychological distress of nurses in Taiwan who worked during the outbreak of SARS. Psychiatric Serv. (2005) 76:76–9. doi: 10.1176/appi.ps.56.1.76
59. Koh D, Meng KL, Sin EC, Soo MK, Qian F, Ng V, et al. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore: What can we learn? Med Care. (2005) 43:676–82. doi: 10.1097/01.mlr.0000167181.36730.cc
60. Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. (2000) 68:748–66. doi: 10.1037/0022-006X.68.5.748
61. Andrews B, Brewin CR, Rose S. Gender, social support, and PTSD in victims of violent crime. J Traumatic Stress. (2003) 16:421–7. doi: 10.1023/A:1024478305142
62. Yehuda R, Hoge CW, McFarlane AC, Vermetten E, Lanius RA, Nievergelt CM, et al. Post-traumatic stress disorder. Nat Rev Dis Primers. (2015) 1:15057. doi: 10.1038/nrdp.2015.57
63. Breidenstine AS, Bailey LO, Zeanah CH, Larrieu JA. Attachment and trauma in early childhood: A review. J Child Adolesc Trauma. (2011) 4:274–90. doi: 10.1080/19361521.2011.609155
64. O'Connor M, Elklit A. Attachment styles, traumatic events, and PTSD: A cross-sectional investigation of adult attachment and trauma. Attach Human Dev. (2008) 10:59–71. doi: 10.1080/14616730701868597
65. Woodward MJ, Eddinger J, Henschel A V., Dodson TS, Tran HN, Beck JG. Social support, posttraumatic cognitions, and PTSD: The influence of family, friends, and a close other in an interpersonal and non-interpersonal trauma group. J Anxiety Disord. (2015) 35:60–7. doi: 10.1016/j.janxdis.2015.09.002
66. Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. (1985) 98:310–57. doi: 10.1037/0033-2909.98.2.310
67. Belsher BE, Ruzek JI, Bongar B, Cordova MJ. Social constraints, posttraumatic cognitions, and posttraumatic stress disorder in treatment-seeking trauma survivors: Evidence for a social-cognitive processing model. Psychol Trauma. (2012) 4:386–91. doi: 10.1037/a0024362
68. Olff M. Bonding after trauma: On the role of social support and the oxytocin system in traumatic stress. Eur J Psychotraumatol. (2012) 3:18597. doi: 10.3402/ejpt.v3i0.18597
69. Ozbay F, Johnson DC, Dimoulas E, Morgan CA, Charney D, Southwick S. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry. (2007) 4:35–40.
70. Sippel LM, Pietrzak RH, Charney DS, Mayes LC, Southwick SM. How does social support enhance resilience in the trauma-exposed individual? Ecol Soc. (2015) 20:4. doi: 10.5751/ES-07832-200410
71. Olff M, Frijling JL, Kubzansky LD, Bradley B, Ellenbogen MA, Cardoso C, et al. The role of oxytocin in social bonding, stress regulation and mental health: An update on the moderating effects of context and interindividual differences. Psychoneuroendocrinology. (2013) 38:1883–94. doi: 10.1016/j.psyneuen.2013.06.019
72. Neumann ID. Chapter 12 Involvement of the brain oxytocin system in stress coping: interactions with the hypothalamo-pituitary-adrenal axis. Progress Brain Res. (2002) 139:147–62. doi: 10.1016/S0079-6123(02)39014-9
73. Bartz JA, Hollander E. The neuroscience of affiliation: Forging links between basic and clinical research on neuropeptides and social behavior. Hormones Behav. (2006) 50:518–28. doi: 10.1016/j.yhbeh.2006.06.018
74. Feldman R. What is resilience: an affiliative neuroscience approach. World Psychiatry. (2020) 19:132–50. doi: 10.1002/wps.20729
75. Seltzer LJ, Ziegler TE, Pollak SD. Social vocalizations can release oxytocin in humans. Proc Biol Sci. (2010) 277:2661–6. doi: 10.1098/rspb.2010.0567
76. Smith AS, Wang Z. Hypothalamic oxytocin mediates social buffering of the stress response. Biol Psychiatry. (2013) 76:281–8. doi: 10.1016/j.biopsych.2013.09.017
77. Hostinar CE, Sullivan RM, Gunnar MR. Psychobiological mechanisms underlying the social buffering of the hypothalamic-pituitary-adrenocortical axis: A review of animal models and human studies across development. Psychol Bull. (2014) 140:256–82. doi: 10.1037/a0032671
78. Winter J, Jurek B. The interplay between oxytocin and the CRF system: Regulation of the stress response. Cell Tissue Res. (2019) 375:85–91. doi: 10.1007/s00441-018-2866-2
79. Feldman R. Oxytocin and social affiliation in humans. Hormones Behav. (2012) 61:380–91. doi: 10.1016/j.yhbeh.2012.01.008
80. Feldman R, Weller A, Zagoory-Sharon O, Levine A. Evidence for a neuroendocrinological foundation of human affiliation: Plasma oxytocin levels across pregnancy and the postpartum period predict mother-infant bonding. Psychol Sci. (2007) 18:965–70. doi: 10.1111/j.1467-9280.2007.02010.x
81. Frijling JL. Preventing PTSD with oxytocin: Effects of oxytocin administration on fear neurocircuitry and PTSD symptom development in recently trauma-exposed individuals. Eur J Psychotraumatol. (2017) 8:1. doi: 10.1080/20008198.2017.1302652
82. Lanius RA, Boyd JE, McKinnon MC, Nicholson AA, Frewen P, Vermetten E, et al. A review of the neurobiological basis of trauma-related dissociation and its relation to cannabinoid- and opioid-mediated stress response: A transdiagnostic, translational approach. Curr Psychiatry Rep. (2018) 20:118. doi: 10.1007/s11920-018-0983-y
83. Lloyd CS, Nicholson AA, Densmore M, Théberge J, Neufeld RW, Jetly R, et al. Shame on the brain: Neural correlates of moral injury event recall in posttraumatic stress disorder. Depression Anixety. (2020) 38:596–605. doi: 10.1002/da.23128
84. Labrague LJ. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: A systematic review of quantitative studies. J Nursing Manage. (2021) 29:1893–905. doi: 10.1111/jonm.13336
85. Giusti EM, Pedroli E, D'Aniello GE, Stramba Badiale C, Pietrabissa G, Manna C, et al. The psychological impact of the COVID-19 outbreak on health professionals: A cross-sectional study. Front Psychol. (2020) 11:1684. doi: 10.3389/fpsyg.2020.01684
86. Nie A, Su X, Zhang S, Guan W, Li J. Psychological impact of COVID-19 outbreak on frontline nurses: A cross-sectional survey study. J Clin Nursing. (2020) 29:4217–26. doi: 10.1111/jocn.15454
87. Brophy JT, Keith MM, Hurley M, McArthur JE. Sacrificed: Ontario healthcare workers in the time of COVID-19. New Solut. (2020) 30:267–81. doi: 10.1177/1048291120974358
88. Xiao H, Zhang Y, Kong BCD D, Li ABCG S, Yang N. The effects of social support on sleep quality of medical staff treating patients with Coronavirus in China. Med Sci Monitor. (2020) 26:e923549. doi: 10.12659/MSM.923549
89. Labrague LJ, De los Santos JAA. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. J Nursing Manage. (2020) 28:1653–61. doi: 10.1111/jonm.13121
90. Shanafelt T, Ripp J, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. J Am Med Assoc. (2020) 323:2133–4. doi: 10.1001/jama.2020.5893
91. Heber A, Testa V, Smith-MacDonald L, Brémault-Phillips S, Carleton N. Rapid response to COVID-19: Addressing challenges and increasing the mental readiness of public safety personnel. Health Promotion Dis Prevention Canada. (2020) 40:350–5. doi: 10.24095/hpcdp.40.11/12.04
92. Sat SÖ, Akbaş P, Sözbir SY. Nurses' exposure to violence and their professional commitment during the COVID-19 pandemic. J Clin Nursing. (2021) 30:2036–47. doi: 10.1111/jocn.15760
93. Zhang SX, Chen J, Jahanshahi AA, Alvarez-Risco A, Dai H, Li J, et al. Succumbing to the COVID-19 pandemic-Healthcare workers not satisfied and intend to leave their jobs. Int J Mental Health Addiction. (2021) 7:1–10. doi: 10.1007/s11469-020-00418-6
94. Jones B, Müller J, Maercker A. Trauma and posttraumatic reactions in German development aid workers: Prevalences and relationship to social acknolwedgement. Int J Soc Psychiatry. (2006) 52:91–100. doi: 10.1177/0020764006061248
95. Woodhouse S, Brown R, Ayers S. A social model of posttraumatic stress disorder: Interpersonal trauma, attachment, group identification, disclosure, social acknowledgement, and negative cognitions. J Theoretical Soc Psychol. (2018) 2:35–48. doi: 10.1002/jts5.17
96. Thormar SB, Sijbrandij M, Gersons BPR, Van de Schoot R, Juen B, Karlsson T, et al. PTSD symptom trajectories in disaster volunteers: The role of self-efficacy, social acknowledgement, and tasks carried out. J Trauma Stress. (2016) 29:17–25. doi: 10.1002/jts.22073
97. Mueller J, Moergeli H, Maercker A. Disclosure and social acknowledgement as predictors of recovery from posttraumatic stress: A longitudinal study in crime victims. Canad J Psychiatry. (2008) 53:160–8. doi: 10.1177/070674370805300306
98. Nazarov A, Frewen P, Oremus C, Schellenberg EG, Mckinnon MC, Lanius R. Comprehension of affective prosody in women with post-traumatic stress disorder related to childhood abuse. Acta Psychiatria Scand. (2015) 131:342–9. doi: 10.1111/acps.12364
99. Cai H, Tu B, Ma J, Chen L, Fu L, Jiang Y, et al. Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of Coronavirus disease 2019 (COVID-19) in Hubei, China. Med Sci Monitor. (2020) 26:e924171. doi: 10.12659/MSM.924171
100. Billings J, Ching BCF, Gkofa V, Greene T, Bloomfield M. Experiences of frontline healthcare workers and their views about support during COVID-19 and previous pandemics: a systematic review and qualitative meta-synthesis. BMC Health Serv Res. (2021) 21:923. doi: 10.1186/s12913-021-06917-z
101. Bastian B, Haslam N. Excluded from humanity: The dehumanizing effects of social ostracism. J Experi Soc Psych. (2010) 46:107–13. doi: 10.1016/j.jesp.2009.06.022
102. Iffland B, Sansen LM, Catani C, Neuner F, Zentner M, Rauthmann JF. Rapid heartbeat, but dry palms: reactions of heart rate and skin conductance levels to social rejection. Front Psychiatry. (2014) 5:956. doi: 10.3389/fpsyg.2014.00956
103. Wesselmann ED, Ispas D, Olson MD, Swerdlik ME, Caudle NM. Does perceived ostracism contribute to mental health concerns among veterans who have been deployed? PLoS ONE. (2018) 13:e0208438. doi: 10.1371/journal.pone.0208438
104. Hipes C, Gemoets D. Stigmatization of war veterans with Posttraumatic Stress Disorder (PTSD): Stereotyping and social distance findings. Soc Mental Health. (2019) 9:243–58. doi: 10.1177/2156869318801889
105. Schneider A, Conrad D, Pfeiffer A, Elbert T, Kolassa I-T, Wilker S. Stigmatization is associated with increased PTSD risk after traumatic stress and diminished likelihood of spontaneous remission-A study with East-African conflict survivors. Front Psychiatry. (2018) 9:423. doi: 10.3389/fpsyt.2018.00423
106. Nietlisbach G, Maercker A. Effects of social exclusion in trauma survivors with Posttraumatic Stress Disorder. Psychol Trauma. (2009) 1:323–31. doi: 10.1037/a0017832
107. Verelst A, De Schryver M, De Haene L, Broekaert E, Derluyn I. The mediating role of stigmatization in the mental health of adolescent victims of sexual violence in Eastern Congo. Child Abuse Neglect. (2014) 38:1139–46. doi: 10.1016/j.chiabu.2014.04.003
108. Taylor S, Landry CA, Rachor GS, Paluszek MM, Asmundson GJG. Fear and avoidance of healthcare workers: An important, under-recognized form of stigmatization during the COVID-19 pandemic. J Anxiety Disord. (2020) 75:102289. doi: 10.1016/j.janxdis.2020.102289
109. Shimizu K, Lin L. Defamation against healthcare workers during COVID-19 pandemic. Int J Health Policy Manage. (2020). doi: 10.34172/ijhpm.2020.184. [Epub ahead of print].
110. Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin Neurosci. (2020) 74:281–2. doi: 10.1111/pcn.12988
111. CTV News. “You Can't be Pointing the Finger”: Windsor Nurses Feel Ostracized for Working in Detroit. (2020). Available online at: https://windsor.ctvnews.ca/you-can-t-be-pointing-the-finger-windsor-nurses-feel-ostracized-for-working-in-detroit-1.4879450
112. Dye TD, Alcantara L, Siddiqi S, Barbosu M, Sharma S, Panko T, et al. Risk of COVID-19-related bullying, harassment and stigma among healthcare workers: An analytical cross-sectional global study. BMJ Open. (2020) 10:e046620. doi: 10.1136/bmjopen-2020-046620
113. Phoenix Australia - Centre for Posttraumatic Mental Health the Canadian Centre of Excellence - PTSD. Moral Stress Amongst Healthcare Workers During COVID-19: A Guide to Moral Injury. Phoenix Australia - Centre for Posttraumatic Mental Health and the Canadian Centre of Excellence - PTSD (2020).
114. Williamson V, Greenberg N, Murphy D. Impact of moral injury on the lives of UK military veterans: A pilot study. BMJ Military Health. (2020) 166:302–6. doi: 10.1136/jramc-2019-001243
115. Battaglia AM, Protopopescu A, Boyd JE, Lloyd C, Jetly R, O'Connor C, et al. The relation between adverse childhood experiences and moral injury in the Canadian Armed Forces. Eur J Psychotraumatol. (2019) 10:1. doi: 10.1080/20008198.2018.1546084
116. Roth SL, Andrews K, Protopopescu A, Lloyd C, O'Connor C, Losier BJ, et al. Mental health symptoms in Public Safety Personnel: Examining the effects of adverse childhood experiences and moral injury. Child Abuse Negl. (2022) 123:105394. doi: 10.1016/j.chiabu.2021.105394
117. Wu AW, Connors C, Everly GS. COVID-19: Peer support and crisis communication strategies to promote institutional resilience. Ann Internal Med. (2020) 172:822–3. doi: 10.7326/M20-1236
118. Kok N, Hoedemaekers A, van der Hoeven H, Zegers M, van Gurp J. Recognizing and supporting morally injured ICU professionals during the COVID-19 pandemic. Intensive Care Med. (2020) 46:1653–4. doi: 10.1007/s00134-020-06121-3
119. Selman LE, Chao D, Sowden R, Marshall S, Chamberlain C, Koffman J. Bereavement support on the frontline of COVID-19: Recommendations for hospital clinicians. J Pain Symptom Manage. (2020) 60:E81–6. doi: 10.1016/j.jpainsymman.2020.04.024
120. Tracy DK, Tarn M, Eldridge R, Cooke J, Calder JDFF, Greenberg N. What should be done to support the mental health of healthcare staff treating COVID-19 patients? Br J Psychiatry. (2020) 217:537–9. doi: 10.1192/bjp.2020.109
121. Roycroft M, Wilkes D, Pattani S, Fleming S, Olsson-Brown A. Limiting moral injury in healthcare professionals during the COVID-19 pandemic. Occup Med. (2020) 5:312–4. doi: 10.1093/occmed/kqaa087
122. Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:E15–6. doi: 10.1016/S2215-0366(20)30078-X
Keywords: moral injury, post-traumatic stress disorder, healthcare workers, COVID-19, interpersonal factors, social cognition
Citation: D'Alessandro AM, Ritchie K, McCabe RE, Lanius RA, Heber A, Smith P, Malain A, Schielke H, O'Connor C, Hosseiny F, Rodrigues S and McKinnon MC (2022) Healthcare Workers and COVID-19-Related Moral Injury: An Interpersonally-Focused Approach Informed by PTSD. Front. Psychiatry 12:784523. doi: 10.3389/fpsyt.2021.784523
Received: 28 September 2021; Accepted: 29 December 2021;
Published: 14 February 2022.
Edited by:
Rosalba Morese, University of Italian Switzerland, SwitzerlandReviewed by:
Agata Benfante, University of Turin, ItalyHannah Murray, University of Oxford, United Kingdom
Copyright © 2022 D'Alessandro, Ritchie, McCabe, Lanius, Heber, Smith, Malain, Schielke, O'Connor, Hosseiny, Rodrigues and McKinnon. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Margaret C. McKinnon, mckinno@mcmaster.ca
 Andrea M. D'Alessandro
Andrea M. D'Alessandro Kimberly Ritchie2
Kimberly Ritchie2 Ruth A. Lanius
Ruth A. Lanius Charlene O'Connor
Charlene O'Connor Sara Rodrigues
Sara Rodrigues Margaret C. McKinnon
Margaret C. McKinnon