- 1National Clinical Research Center for Mental Disorders, Department of Psychiatry, The Second Xiangya Hospital of Central South University, Changsha, China
- 2Shanghai Key Laboratory of Forensic Medicine, Key Laboratory of Forensic Science, Ministry of Justice China, Shanghai Forensic Service Platform, Academy of Forensic Science, Shanghai, China
- 3Health Management Center, Health Management Research Center of Central South University, The Third Xiangya Hospital, Central South University, Changsha, China
- 4Dongguan Mental Health Center, Dongguan, China
Objective: Adolescents and young adults are susceptible to high-risk behaviors such as self-harm and suicide. However, the impact of childhood maltreatment on suicide attempts in adolescents and young adults with first episode of depression remains unclear. This study examined the association between suicide attempts and childhood maltreatment among adolescents and young adults with first depressive episodes.
Methods: A total of 181 adolescents and young adults with first depressive episodes were included. The Child Trauma Questionnaire (CTQ), Beck Anxiety Inventory (BAI), and Patient Health Questionnaire-2 (PHQ-2) were used to assess childhood maltreatment and the severity of anxiety and depressive symptoms, respectively. The suicide item in the MINI-International Neuropsychiatric Interview (M.I.N.I.) 5.0 was used to assess the suicide attempts. Logistic regression analyses were used to explore the associated factors of suicide attempts.
Results: The prevalence of SA in the total sample was 31.5% (95% CI = 24.9–38.1%). Multivariate logistic regression analyses revealed that the diagnosis of bipolar disorder (OR = 2.18, 95% CI = 1.07–4.40), smoking (OR = 2.64, 95% CI = 1.10–6.37), anxiety symptoms (OR = 1.05, 95% CI = 1.02–1.08), and childhood maltreatment (OR = 1.04, 95% CI = 1.01–1.07) were potential associated factors of SA. In addition, anxiety symptoms had a mediating effect on the relationship between childhood maltreatment and SA.
Conclusion: Adolescents and young adults with first depressive episodes and having experiences of childhood maltreatment are at a high risk of suicide. The severity of anxiety symptoms may mediate the relation between childhood maltreatment and suicide attempts in this group of patients.
Introduction
Suicide attempt (SA), one of the major suicidal behaviors, is defined as an act of self-injuring with the intention of ending one's own life (1). Around 703,000 people die from suicide worldwide, each year. Suicide is a leading cause of death among young people aged 15–24 years and suicide attempts are considerably high among children and adolescents aged 12–17 years (2, 3). The prevalence of SA among Chinese adolescents ranges from 0.94 to 9.01%, with an overall prevalence of 2.94% (95% CI = 2.53–3.41%) (4).
Mental disorders, such as major depressive disorder (MDD) and bipolar disorder (BP), could increase the risk of suicide behaviors in adolescents and young adults (5–7). A meta-analysis found that MDD and BP were the most common diagnoses among youths with SA (8, 9). The risk of SA is five times higher in adolescents with MDD than in the general population (10). The lifetime prevalence of SA in younger BP patients (14.7%, 95% CI = 5.9–20.0%) (11) was significantly higher than those without psychiatric disorders (0.8%, 95% CI = 0.7–0.9%) (12). For patients with BP, suicide behaviors were predominantly present during depressive episodes (13), especially during the first depressive episode (14).
Apart from the negative outcomes of physical injury and the increased risk of completed suicide, SA could worsen patients' general well-being and increase their utilization of health services and the economic burden (15). Understanding the associates of SA could benefit the development of effective prevention strategies for adolescents and young adults with MDD and BP.
Childhood maltreatment, including abuse (i.e., physical, sexual, and emotional abuse) and neglect (i.e., physical and emotional neglect), often has negative and long-term adverse effects on individuals' mental health (16–18). Increasing evidence shows that childhood maltreatment is closely related to the following self-harm and suicide behaviors including suicide attempts. Such phenomenon has also been confirmed among patients with MDD and BP (19, 20). For example, childhood maltreatment, such as physical abuse and emotional neglect, could increase the risk of subsequent SA among patients with MDD and BP (21, 22). Several theories have been raised to explain the path from childhood maltreatment to SA. For instance, childhood maltreatment can disturb developmental processes associated with strengthening of emotional regulation and relevant interpersonal skills and increased impulsivity and neuroticism. These disturbances may lower the threshold of suicidal behavior in individuals to experience stressful events. And the reduction in long-term social support associated with childhood maltreatment also increases the risk of suicide attempts (23). Previous studies majorly examined the association between SA and childhood maltreatment among adults with MDD and BP (22, 24). However, limited studies have discussed this relationship among adolescents and young adults. Besides, the existing studies are majorly conducted in Western populations, which may limit their generalization among other racial groups including China (20).
Considering that childhood maltreatment may lead to SA among patients with MDD and BP and suicide behaviors are most likely presented in their first depressive episode (14, 25), we conducted this study to examine the relationship between childhood maltreatment and SA among adolescents and young adults with first depressive episodes. Antidepressants, such as buprenorphine (26) and ketamine (27) and cognitive behavioral therapy (CBT) can reduce self-harming behaviors in depressed patients (28, 29). For antidepressants, which can increase 5-HT neurotransmission and 5-HT1A autoreceptor sensitivity, release hopelessness feelings and reduce depression, achieve the effect of reducing suicide-related behavior (30). For CBT, aims to change feelings of negativity and behaviors into positive thoughts and behaviors to redress adverse cognitive and decrease negative emotional affects (31). Therefore, we targeted on psychiatric treatment -naive patients first depressive episode in this study to avoid the impact of psychiatric medication and psychotherapy on suicide behaviors. For both patients and clinical practitioners, this study will try to verify the understanding on the impact of childhood maltreatment experience by using a purer sample and strengthen the evidence of intervening childhood maltreatment at an early age.
In addition, studies among healthy adults suggested that negative emotion, such as depression and anxiety, may mediate the association between childhood maltreatment and suicide behaviors (32–34). Such association is still under discussed among patients with depression. Therefore, we further explored the mediation effect of depressive and anxiety symptoms between childhood maltreatment and SA in our studied population.
Materials and Methods
Participants
This cross-sectional study is part of Youth Depression Cohort (XiangyYa) study (YDC-XY), which was conducted from January 1, 2018, to December 31, 2019, at the outpatient department of the Second Xiangya Hospital of Central South University, China. Patients who visited the hospital because of their first depressive episode were consecutively recruited if they fulfilled the following criteria: (1) aged between 14 and 24, (2) experiencing their first depressive episode, (3) diagnosed with MDD or BP according to the Diagnostic and Statistical Manual of Mental Disorders-V (DSM-V), and (4) received no psychiatric treatment (including antipsychotic drugs and psychotherapy) in the past 3 months. The exclusion criteria were as follows: (1) comorbid with neurological conditions or substance dependence and (2) participating in other clinical trials.
Measurements
Sociodemographic and clinical data were collected, including age, gender, education year, marital status, nationality, occupation, history of smoking, drinking, drug use, family history of psychiatric disorders and parents' marital status. Drug use history was assessed using a dichotomous item: “In your lifetime, have you ever used any of the following drugs (according to the MINI-International Neuropsychiatric Interview, M.I.N.I)?.” Smoking and drinking history was assessed using two dichotomous items: “Have you ever smoked?” and “Have you ever consumed alcohol?.” SA was assessed using the item of M.I.N. I: “In the past month did you attempt suicide?.”
The Child Trauma Questionnaire (CTQ) (35), a 28-item self-report instrument, was used to assess the experience of abuse and neglect in childhood and adolescence. The scale was first developed by Bernstein in 1998 and has been widely used. Its Chinese version has been validated in both adolescents and adults (36). The CTQ assesses childhood maltreatment from five aspects, including emotional neglect, emotional abuse, physical neglect, physical abuse, and sexual abuse. Each subscale consists of five five-point items, with each item rated from “1” (not at all) to “5” (very often). The scores of each subscale were the summation of all loaded item scores and ranged from 5 to 25, while the total score of the CTQ was the summation of all subscale scores and ranged from 25 to 125.
The Beck Anxiety Inventory (BAI) (37) was used to assess the anxiety symptoms. It is a self-rating scale consisting of 21 four-point items with each item rated from “0” (not at all) to “3” (severely), and the total score of the scale ranged from 0 to 63, with a higher total score indicating more severe anxiety symptoms. The Chinese version of the BAI was found to have satisfactory reliability and validity in adolescents and adults (38).
The Chinese version of the Patient Health Questionnaire-9 has been widely used in research and clinical practice to screen depressive symptoms (39). The Patient Health Questionnaire-2 (PHQ-2) (40) is a short version of the PHQ-9 and has been found to have equal psychometric properties compared to the PHQ-9 for depressive symptom screening (41). The two items of the PHQ-2 were rated from “0” (none at all) to “3” (almost every day), and the total score of the scale ranged from 0 to 6.
Procedures
The continuous sampling method was applied. All patients who were first time visit the psychiatric outpatient services because of depression invited to participate in the survey. After obtaining written informed consent from the participants, a face-to-face interview was conducted to reconfirm the psychiatric diagnosis by a senior psychiatrist using a structured diagnostic tool, the M.I.N.I according to the DSM-V. Then all participants were asked complete all measurements mentioned above. According to patients' response to the item “In the past month did you attempt suicide?” in M.I.N.I, patients were recognized as having “suicide attempts” if they answer “yes” and as having “no suicide attempts” if “no.”
Statistical Analysis
The SPSS 24.0 software was used for all statistical analyses. The two-independent sample t-tests and chi-square tests were used to compare the socio-demographic and clinical data between patients with and without SA, as appropriate. Multiple logistic regressions were performed to examine the independent variables associated with SA. Variables with p < 0.10 in univariate analyses were entered into the regression model as independent variables. In addition, the association between the total score of the BAI and CTQ was tested using Pearson's correlation coefficient. Mediation analysis was conducted using the PROCESS v3. 3 to examine the extent to which potential mediators may explain the relationship between childhood maltreatment and SA. Potential mediators were selected based on the results of the multiple logistic regression. The significance level was set as p < 0.05 (two sides).
Ethical Approval and Informed Consent
This study was approved by the ethics committee of The Second Xiangya Hospital of Central South University. All patients signed written informed consent.
Results
A total of 181 adolescents and young adults with first depressive episodes met the eligibility criteria and were included. Among them, 31.5% (95% CI = 24.9–38.1%) (n = 57) reported SA. The sociodemographic and clinical data are shown in Table 1. The majority of the patients were female (75.1%). The mean age of the patients was 18.6 ± 2.3 years, while the mean years of education was 12.2 ± 2.3 years. A total of 115 (63.5%) patients were diagnosed with MDD, while the remaining 66 (36.5%) patients were diagnosed with BP.
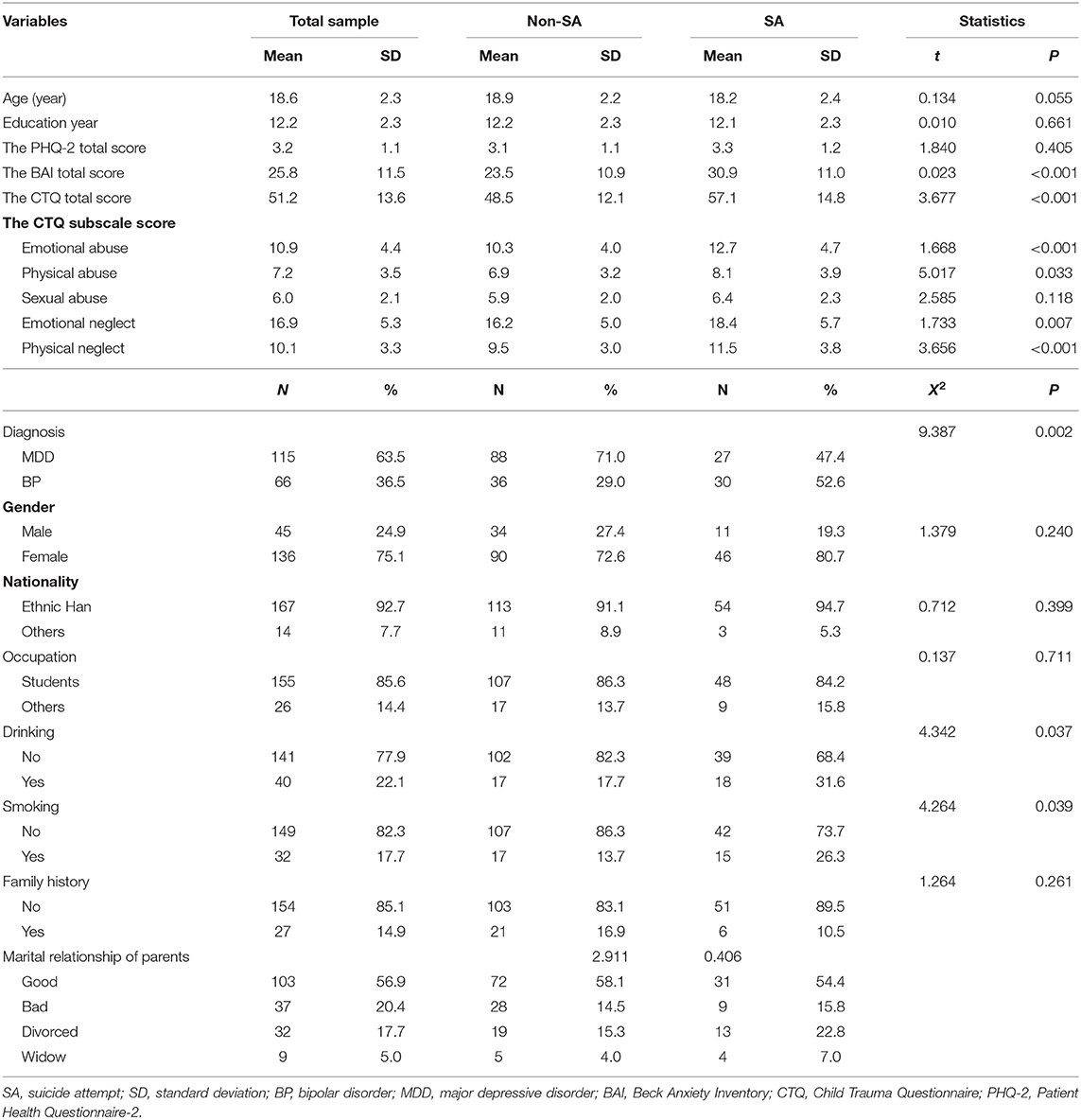
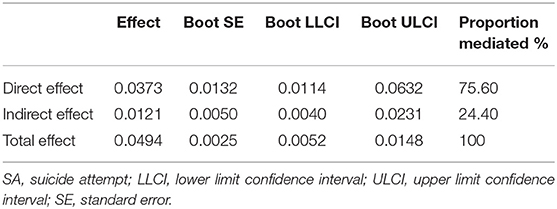
Table 1. Sociodemographic and clinical characteristics among adolescents and young adults with first depressive episode.
Patients with SA were more likely to have a diagnosis of BP (52.6 vs. 29.0%, p = 0.002), drink (31.6 vs. 17.7%, p < 0.050), smoke (26.3 vs. 13.7%, p < 0.050), and present with more severe anxiety symptoms (30.9 ± 11.0 vs. 23.5 ± 10.9, p < 0.001) than those without. Compared to patients without SA, patients with SA experienced significantly more severe emotional abuse (12.7 ± 4.7 vs. 10.3 ± 4.0, p < 0.001), physical abuse (8.1 ± 3.9 vs. 6.9 ± 3.2, p = 0.033), emotional neglect (18.4 ± 5.7 vs. 16.2 ± 5.0, p < 0.001), physical neglect (11.5 ± 3.8 vs. 9.5 ± 3.0, p < 0.001), and overall childhood maltreatment (57.1 ± 14.8 vs. 48.5 ± 12.1, p < 0.001). There was no significant difference in the PHQ-2 total score between patients with and without SA (3.3 ± 1.2 vs. 3.1 ± 1.1, p = 0.405) (Table 1).
A multiple logistic regression model revealed that the diagnosis of BP [odds ratio (OR) =2.18, 95% CI = 1.07–4.40], smoking (OR = 2.63, 95% CI = 1.10–6.37), severity of anxiety symptoms (OR = 1.05, 95% CI = 1.02–1.08), and childhood maltreatment (OR = 1.04, 95% CI = 1.01–1.07) were significantly and positively associated with SA (Table 2). There was a significant positive association between the severity of anxiety symptoms and overall childhood maltreatment (r = 0.201, p < 0.001).
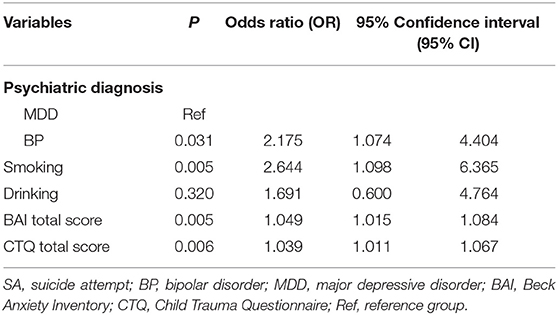
Table 2. Multiple logistic regression model assessing variables associated with SAs among adolescents and young adults with first depressive episode.
The mediation analysis revealed that anxiety symptoms mediated the relationship between childhood maltreatment and SA [coefficient (indirect) =0.01, standard error (SE) =0.005, 95% CI = 0.004–0.023] and explained 24.40% of the total effect (Figure 1, Table 3).
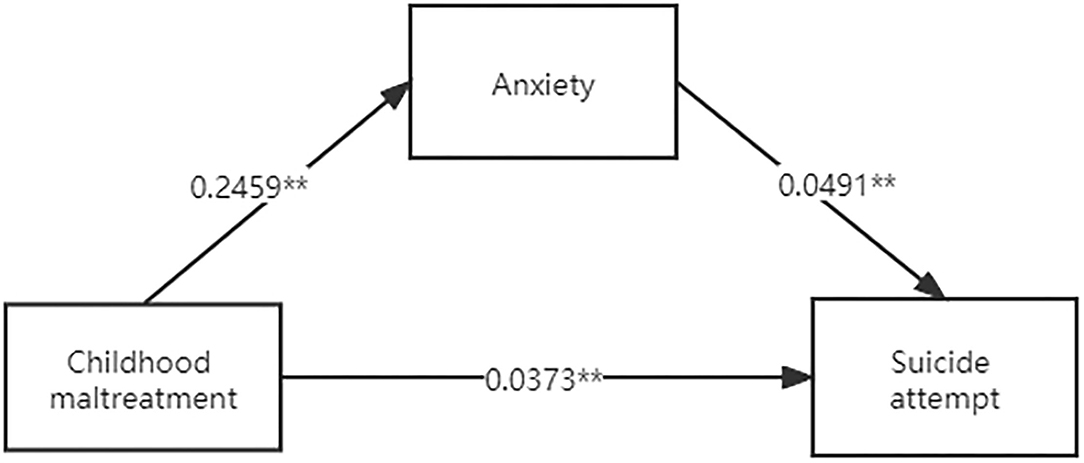
Figure 1. The mediation effect of anxiety on the relationship between childhood maltreatment and SA. **P < 0.01.
Discussion
This study found that 31.5% of treatment-naïve adolescents and young adults with first depressive episodes had SA, which was higher than one previous study about the first-episode and drug naïve patients with MDD with a prevalence of 19.9% (42). Several possible reasons may contribute to this discrepancy. On the one hand, the patients in this study were untreated adolescents and young adults in the first episode of depression and acute episode, those who had severe depressive symptoms. On the other hand, our study recruited clinical psychiatric outpatients, those who had more severe depressive symptoms than those surveyed in the community. Adolescents and young adults are the most common age groups for first mood disorders (43, 44), such as MDD and BP. These people are not mature in terms of cognitive structure, emotional structure and rationality. When an adverse stressful event or major environmental change cannot be dealt with, it is possible they may decide to commit suicide to end the current pain and escape the existing situation (45).
One of the important findings of this study is that patients with SA experienced more childhood maltreatment than those without SA. Previous studies also found a similar association between childhood maltreatment and SA among general adolescents and adults (21, 46). Patients experiencing childhood maltreatment often have negative family environments, such as a lack of shelter and safe living conditions, which can prevent the patients from developing appropriate emotional regulation and stress coping skills (47). As a result, they may impulsively react to stressful life events and even present suicidal behaviors. Emotional trauma may negatively affect the development of the hypothalamus-pituitary-adrenal axis (HPA axis) in growth and progression, and alteration of the function of the HPA axis was found to have an impact on individuals' biological, emotional, behavioral, and cognitive responses to stressful events (48–52), which were related to suicidal behaviors.
Another important finding of this study is that anxiety symptoms were found to mediate the relationship between childhood maltreatment and SA among adolescents and young adults with first depressive episodes, which is consistent with previous studies (53). These results have been confirmed in previous studies (54–56), which found an independent association between SA and anxiety symptoms in adolescents. Anxiety can also predict the occurrence of SA (57). Behavioral avoidance, one clinical feature of anxiety, often leads to social isolation, reduced quality of life, and impaired functioning, all of which are related to an increased risk of suicide (58, 59). Relevant studies have shown that the influence of childhood maltreatment on SA is indirectly affected by psychological factors (34). This suggests that anxiety should be the treatment target in the prevention strategies of SA in depressed adolescents and young adults.
Furthermore, this study found that young patients with BP were more likely to have SA than those with MDD, which is consistent with previous findings (8, 60). For example, in a study of people hospitalized after SA, 28 percent were diagnosed with MDD and 39 percent with BP (61). In an 18-month follow-up cohort of patients with BP and MDD, 19.9% of those with BP and 9.5% of those with MDD attempted suicide (62). The possible reasons for the relatively higher risk of SA in patients with BP compared to their counterparts with MDD may be that they have more severe depressive symptoms during their depressive episodes (60), more difficulties of treatment, more impulsivity, and a higher risk of comorbidity of anxiety (63) than patients with MDD.
The strengths of the present study include the large sample size of treatment-naïve adolescents and young adults with first depressive episodes. In addition, the study examined the association between SA and childhood maltreatment among adolescents and young adults with MDD and BP, and discussed the association between childhood maltreatment and suicide behaviors among patients with depression. However, several methodological limitations should be considered. First, as a cross-sectional study, a causal relationship between SA and associated factors could not be generated. Second, some potential factors associated with SA, such as residential type and socioeconomic state (15, 64), were not examined. Third, the single-site study design could limit the generalization of the results. Forth, young patients with MDD may convert to BP during the progression of the disease, which may bias the estimation of the prevalence of SA in patients with each disorder. Fifth, although PHQ-2 has been proved to have equal psychometric properties compared to the PHQ-9 for depressive symptom screening, only using 2 items for depressive symptom screening may influence the identification of other depressive symptoms and the results of this study. Sixth, although we studied a pure sample that was treatment-naïve and with a first depressive episode, the acute illness phase may increase the risk of suicide behaviors in this population, which may potentially bias the results. Finally, some potential associated factors, such as smoking and drinking, were not included in the mediation model.
Conclusion
This study found that treatment-naive adolescents and young adults with first depressive episodes were at a high risk of SA. Patients with SA were more likely to have experiences of childhood maltreatment and present more severe anxiety symptoms than those without SA. Anxiety symptoms may mediate the relationship between childhood maltreatment and SAs. Considering the severe negative outcomes of SA, it is essential to develop prevention strategies for SA among depressed adolescents and young adults. Alleviating anxiety may be an effective way to reduce the risk of suicide in this group of patients.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Second Xiangya Hospital of Central South University. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
HC, SZ, and JZ: conceived and designed the study. PL, JL, XCh, HG, CL, and XL: participated in the acquisition of data. HC: analyzed the data and drafted the manuscript. WL, XCa, JZ, and XW: revised the manuscript. All authors read and approved the final manuscript.
Funding
This study was supported in part by grants from the National Natural Science Foundation of China (82071543, JZ, PI), the Natural Science Foundation of Hunan (2019JJ40424, Jiansong Zhou, PI), the Health Committee of Hunan (202103091470, JZ, PI), the Hunan Province Innovation Province Construction Project (2019SK2334, XW and JZ, Co-PI), and Clinical medical technology innovation guidance project of Hunan (2020SK53415, JZ, PI).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors are grateful to the participants and their families for contributing to this research.
References
1. Klonsky ED, May AM, Saffer BY. Suicide, suicide attempts, and suicidal ideation. Annu Rev Clin Psychol. (2016) 12:307–30. doi: 10.1146/annurev-clinpsy-021815-093204
2. Hawton K, Hill NTM, Gould M, John A, Lascelles K, Robinson J. Clustering of suicides in children and adolescents. Lancet Child Adolesc Health. (2020) 4:58–67. doi: 10.1016/S2352-4642(19)30335-9
4. Hu J, Dong Y, Chen X, Liu Y, Ma D, Liu X, et al. Prevalence of suicide attempts among Chinese adolescents: a meta-analysis of cross-sectional studies. Compr Psychiatry. (2015) 61:78–89. doi: 10.1016/j.comppsych.2015.05.001
5. Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. (2008) 192:98–105. doi: 10.1192/bjp.bp.107.040113
6. Hawton K, Saunders KEA, O'Connor RC. Self-harm and suicide in adolescents. Lancet. (2012) 379:2373–82. doi: 10.1016/S0140-6736(12)60322-5
7. Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the national comorbidity survey replication adolescent supplement. JAMA Psychiatry. (2013) 70:300–10. doi: 10.1001/2013.jamapsychiatry.55
8. De Crescenzo F, Serra G, Maisto F, Uchida M, Woodworth H, Casini MP, et al. Suicide attempts in juvenile bipolar versus major depressive disorders: systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. (2017) 56:825–31 e3. doi: 10.1016/j.jaac.2017.07.783
9. Hakim Shooshtari M, Malakouti SK, Panaghi L, Mohseni S, Mansouri N, Rahimi Movaghar A. Factors associated with suicidal attempts in Iran: a systematic review. Iran J Psychiatry Behav Sci. (2016) 10:e948. doi: 10.17795/ijpbs-948
10. Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Mol Psychiatry. (2010) 15:868–76. doi: 10.1038/mp.2009.29
11. Hauser M, Galling B, Correll CU. Suicidal ideation and suicide attempts in children and adolescents with bipolar disorder: a systematic review of prevalence and incidence rates, correlates, and targeted interventions. Bipolar Disord. (2013) 15:507–23. doi: 10.1111/bdi.12094
12. Cao XL, Zhong BL, Xiang YT, Ungvari GS, Lai KY, Chiu HF, et al. Prevalence of suicidal ideation and suicide attempts in the general population of China: a meta-analysis. Int J Psychiatry Med. (2015) 49:296–308. doi: 10.1177/0091217415589306
13. Beglyankin NI, Burygina LA, Levin ME, Bardenshteyn LM. [Clinical features of depressive episode with onset in adolescence and the risk of bipolar depression]. Zh Nevrol Psikhiatr Im S Korsakova. (2019) 119:22–7. doi: 10.17116/jnevro20191191222
14. Cremaschi L, Dell'Osso B, Vismara M, Dobrea C, Buoli M, Ketter TA, et al. Onset polarity in bipolar disorder: a strong association between first depressive episode and suicide attempts. J Affect Disord. (2017) 209:182–7. doi: 10.1016/j.jad.2016.11.043
15. Dávila Cervantes CA, Luna Contreras M. Suicide attempt in teenagers: associated factors. Rev Chil Pediatr. (2019) 90:606–16. doi: 10.32641/rchped.v90i6.1012
16. Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. (2009) 373:68–81. doi: 10.1016/S0140-6736(08)61706-7
17. Fumagalli F, Molteni R, Racagni G, Riva MA. Stress during development: impact on neuroplasticity and relevance to psychopathology. Prog Neurobiol. (2007) 81:197–217. doi: 10.1016/j.pneurobio.2007.01.002
18. Lara MA, Navarrete L, Nieto L, Le HN. Childhood abuse increases the risk of depressive and anxiety symptoms and history of suicidal behavior in Mexican pregnant women. Braz J Psychiatry. (2015) 37:203–10. doi: 10.1590/1516-4446-2014-1479
19. Angelakis I, Austin JL, Gooding P. Association of childhood maltreatment with suicide behaviors among young people: a systematic review and meta-analysis. JAMA Netw Open. (2020) 3:e2012563. doi: 10.1001/jamanetworkopen.2020.12563
20. Polanco-Roman L, Alvarez K, Corbeil T, Scorza P, Wall M, Gould MS, et al. Association of childhood adversities with suicide ideation and attempts in Puerto Rican young adults. JAMA Psychiatry. (2021) 78:896–902. doi: 10.1001/jamapsychiatry.2021.0480
21. Hadland SE, Wood E, Dong H, Marshall BDL, Kerr T, Montaner JS, et al. Suicide attempts and childhood maltreatment among street youth: a prospective cohort study. Pediatrics. (2015) 136:440–9. doi: 10.1542/peds.2015-1108
22. Adiguzel V, Ozdemir N, Sahin SK. Childhood traumas in euthymic bipolar disorder patients in Eastern Turkey and its relations with suicide risk and aggression. Nord J Psychiatry. (2019) 73:490–6. doi: 10.1080/08039488.2019.1655589
23. Hoertel N, Franco S, Wall MM, Oquendo MA, Wang S, Limosin F, et al. Childhood maltreatment and risk of suicide attempt: a nationally representative study. J Clin Psychiatry. (2015) 76:916–23. doi: 10.4088/JCP.14m09420
24. Duarte D, Belzeaux R, Etain B, Greenway KT, Rancourt E, Correa H, et al. Childhood-maltreatment subtypes in bipolar patients with suicidal behavior: systematic review and meta-analysis. Braz J Psychiatry. (2020) 42:558–67. doi: 10.1590/1516-4446-2019-0592
25. Li XY, Tabarak S, Su XR, Qin Z, Chai Y, Zhang S, et al. Identifying clinical risk factors correlate with suicide attempts in patients with first episode major depressive disorder. J Affect Disord. (2021) 295:264–70. doi: 10.1016/j.jad.2021.08.028
26. Yovell Y, Bar G, Mashiah M, Baruch Y, Briskman I, Asherov J, et al. Ultra-low-dose buprenorphine as a time-limited treatment for severe suicidal ideation: a randomized controlled trial. Am J Psychiatry. (2016) 173:491–8. doi: 10.1176/appi.ajp.2015.15040535
27. Grunebaum MF, Galfalvy HC, Choo TH, Keilp JG, Moitra VK, Parris MS, et al. Ketamine for rapid reduction of suicidal thoughts in major depression: a midazolam-controlled randomized clinical trial. Am J Psychiatry. (2018) 175:327–35. doi: 10.1176/appi.ajp.2017.17060647
28. Shu Y, Kuang L, Huang Q, He L. Fractional amplitude of low-frequency fluctuation (fALFF) alterations in young depressed patients with suicide attempts after cognitive behavioral therapy and antidepressant medication cotherapy: a resting-state fMRI study. J Affect Disord. (2020) 276:822–8. doi: 10.1016/j.jad.2020.07.038
29. Gøtzsche PC, Gøtzsche PK. Cognitive behavioural therapy halves the risk of repeated suicide attempts: systematic review. J R Soc Med. (2017) 110:404–10. doi: 10.1177/0141076817731904
30. Mahar I, Bambico FR, Mechawar N, Nobrega JN. Stress, serotonin, and hippocampal neurogenesis in relation to depression and antidepressant effects. Neurosci Biobehav Rev. (2014) 38:173–92. doi: 10.1016/j.neubiorev.2013.11.009
31. Afrasiabifar A, Hosseini N, Haghgoo A. The effects of Group Cognitive Behavior Therapy (GCBT) on suicidal thoughts in patients with major depression. (2018) 16:228–35. doi: 10.5742/MEWFM.2018.93293
32. Lee MA. Emotional abuse in childhood and suicidality: the mediating roles of re-victimization and depressive symptoms in adulthood. Child Abuse Negl. (2015) 44:130–9. doi: 10.1016/j.chiabu.2015.03.016
33. Bahk YC, Jang SK, Choi KH, Lee SH. The relationship between childhood trauma and suicidal ideation: role of maltreatment and potential mediators. Psychiatry Investig. (2017) 14:37–43. doi: 10.4306/pi.2017.14.1.37
34. Obikane E, Shinozaki T, Takagi D, Kawakami N. Impact of childhood abuse on suicide-related behavior: analysis using marginal structural models. J Affect Disord. (2018) 234:224–30. doi: 10.1016/j.jad.2018.02.034
35. Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/S0145-2134(02)00541-0
36. Zhao XF, Zhang YL, Li LF, Zhou YF. Evaluation on reliability and validity of Chinese version of childhood trauma questionnaire. Chin J Clin Rehabil. (2005) 9:209–11.
37. Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. (1988) 56:893–7. doi: 10.1037/0022-006X.56.6.893
38. Zheng JR, Huang ZR, Huang JJ, zhuang XQ, Wang DB, Zheng SY, et al. A study of psychometric properties, normative scores and factor structure of beck anxiety inventory Chinese version. Chin J Clin Psychol. (2002) 10:4–6.
39. Tsai FJ, Huang YH, Liu HC, Huang KY, Huang YH, Liu SI. Patient health questionnaire for school-based depression screening among Chinese adolescents. Pediatrics. (2014) 133:e402–9. doi: 10.1542/peds.2013-0204
40. Kroenke K, Spitzer RL, Williams JB. The patient health questionnaire-2: validity of a two-item depression screener. Med Care. (2003) 41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C
41. Mitchell AJ, Yadegarfar M, Gill J, Stubbs B. Case finding and screening clinical utility of the Patient Health Questionnaire (PHQ-9 and PHQ-2) for depression in primary care: a diagnostic meta-analysis of 40 studies. BJPsych Open. (2016) 2:127–38. doi: 10.1192/bjpo.bp.115.001685
42. Shen Y, Wei Y, Yang XN, Zhang G, Du X, Jia Q, et al. Psychotic symptoms in first-episode and drug naive patients with major depressive disorder: Prevalence and related clinical factors. Depress Anxiety. (2020) 37:793–800. doi: 10.1002/da.23026
43. Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustün TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. (2007) 20:359–64. doi: 10.1097/YCO.0b013e32816ebc8c
44. Beesdo-Baum K, Knappe S, Asselmann E, Zimmermann P, Bruckl T, Hofler M, et al. The 'Early Developmental Stages of Psychopathology (EDSP) study': a 20-year review of methods and findings. Soc Psychiatry Psychiatr Epidemiol. (2015) 50:851–66. doi: 10.1007/s00127-015-1062-x
45. Beautrais AL. Suicide and serious suicide attempts in youth: a multiple-group comparison study. Am J Psychiatry. (2003) 160:1093–9. doi: 10.1176/appi.ajp.160.6.1093
46. Dias de Mattos Souza L, Lopez Molina M, Azevedo da Silva R, Jansen K. History of childhood trauma as risk factors to suicide risk in major depression. Psychiatry Res. (2016) 246:612–6. doi: 10.1016/j.psychres.2016.11.002
47. Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry. (2010) 197:378–85. doi: 10.1192/bjp.bp.110.080499
48. Carpenter LL, Tyrka AR, Ross NS, Khoury L, Anderson GM, Price LH. Effect of childhood emotional abuse and age on cortisol responsivity in adulthood. Biol Psychiatry. (2009) 66:69–75. doi: 10.1016/j.biopsych.2009.02.030
49. Jokinen J, Carlborg A, Martensson B, Forslund K, Nordstrom AL, Nordstrom P. DST non-suppression predicts suicide after attempted suicide. Psychiatry Res. (2007) 150:297–303. doi: 10.1016/j.psychres.2006.12.001
50. Kuhlman KR, Geiss EG, Vargas I, Lopez-Duran NL. Differential associations between childhood trauma subtypes and adolescent HPA-axis functioning. Psychoneuroendocrinology. (2015) 54:103–14. doi: 10.1016/j.psyneuen.2015.01.020
51. Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. (2009) 10:434–45. doi: 10.1038/nrn2639
52. Mann JJ, Currier D, Stanley B, Oquendo MA, Amsel LV, Ellis SP. Can biological tests assist prediction of suicide in mood disorders? Int J Neuropsychopharmacol. (2006) 9:465–74. doi: 10.1017/S1461145705005687
53. Sachs-Ericsson N, Corsentino E, Rushing NC, Sheffler J. Early childhood abuse and late-life suicidal ideation. Aging Ment Health. (2013) 17:489–94. doi: 10.1080/13607863.2012.758236
54. Jenkins R, Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, et al. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health surveys. PLoS Med. (2009) 6:e1000123. doi: 10.1371/journal.pmed.1000123
55. Yen CF, Lai CY, Ko CH, Liu TL, Tang TC, Wu YY, et al. The associations between suicidal ideation and attempt and anxiety symptoms and the demographic, psychological, and social moderators in Taiwanese adolescents. Arch Suicide Res. (2014) 18:104–16. doi: 10.1080/13811118.2013.824826
56. Tanabe S, Terao T, Shiotsuki I, Kanehisa M, Ishii K, Shigemitsu O, et al. Anxious temperament as a risk factor of suicide attempt. Compr Psychiatry. (2016) 68:72–7. doi: 10.1016/j.comppsych.2016.04.001
57. Bentley KH, Franklin JC, Ribeiro JD, Kleiman EM, Fox KR, Nock MK. Anxiety and its disorders as risk factors for suicidal thoughts and behaviors: a meta-analytic review. Clin Psychol Rev. (2016) 43:30–46. doi: 10.1016/j.cpr.2015.11.008
58. Kaplan MS, McFarland BH, Huguet N, Newsom JT. Physical illness, functional limitations, and suicide risk: a population-based study. Am J Orthopsychiatry. (2007) 77:56–60. doi: 10.1037/0002-9432.77.1.56
59. Kanwar A, Malik S, Prokop LJ, Sim LA, Feldstein D, Wang Z, et al. The association between anxiety disorders and suicidal behaviors: a systematic review and meta-analysis. Depress Anxiety. (2013) 30:917–29. doi: 10.1002/da.22074
60. Michaels MS, Balthrop T, Pulido A, Rudd MD, Joiner TE. Is the higher number of suicide attempts in bipolar disorder vs. major depressive disorder attributable to illness severity? Arch Suicide Res. (2017) 22:46–56. doi: 10.1080/13811118.2017.1319308
61. Raja M, Azzoni A. Suicide attempts: differences between unipolar and bipolar patients and among groups with different lethality risk. J Affect Disord. (2004) 82:437–42. doi: 10.1016/j.jad.2004.02.001
62. Holma KM, Haukka J, Suominen K, Valtonen HM, Mantere O, Melartin TK, et al. Differences in incidence of suicide attempts between bipolar I and II disorders and major depressive disorder. Bipolar Disord. (2014) 16:652–61. doi: 10.1111/bdi.12195
63. Bellani M, Hatch JP, Nicoletti MA, Ertola AE, Zunta-Soares G, Swann AC, et al. Does anxiety increase impulsivity in patients with bipolar disorder or major depressive disorder? J Psychiatr Res. (2012) 46:616–21. doi: 10.1016/j.jpsychires.2012.01.016
Keywords: suicide attempt, first depressive episode, anxiety, adolescents, childhood maltreatment
Citation: Chen H, Li W, Cao X, Liu P, Liu J, Chen X, Luo C, Liang X, Guo H, Zhong S, Wang X and Zhou J (2021) The Association Between Suicide Attempts, Anxiety, and Childhood Maltreatment Among Adolescents and Young Adults With First Depressive Episodes. Front. Psychiatry 12:745470. doi: 10.3389/fpsyt.2021.745470
Received: 22 July 2021; Accepted: 24 November 2021;
Published: 17 December 2021.
Edited by:
Kevin G. Bath, Brown University, United StatesReviewed by:
Omneya Ibrahim, Suez Canal University, EgyptBao-Liang Zhong, Wuhan Mental Health Center, China
Min Hyuk Kim, Yonsei University, South Korea
Copyright © 2021 Chen, Li, Cao, Liu, Liu, Chen, Luo, Liang, Guo, Zhong, Wang and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiansong Zhou, zhoujs2003@csu.edu.cn
 Hui Chen
Hui Chen Wen Li
Wen Li Xia Cao
Xia Cao Peiqu Liu1
Peiqu Liu1 Xiaoping Wang
Xiaoping Wang Jiansong Zhou
Jiansong Zhou