- 1Institute of Nephrology, Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 2Department of Urology, Shuguang Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 3The National Clinical Research Center for Metabolic Diseases, Department of Metabolism and Endocrinology, The Second Xiangya Hospital, Central South University, Changsha, Hunan, China
- 4Department of Anorectal Surgery, Shuguang Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 5Anorectal Disease Institute of Shuguang Hospital, Shanghai, China
Background: Accumulating evidence suggests that traditional Chinese medicine (TCM) has significant effects on reducing 24-h urinary protein (24-h UPRO) and improves renal function indices. The current level of evidence-based medicine is still not enough due to the limitation of clinical center size and sample size.
Objective: We aimed to update the current evidence on the efficacy of TCM in the treatment of diabetic kidney disease (DKD).
Methods: PubMed, Embase, the Cochrane Library, and SinoMed were searched to identify randomized controlled trials (RCTs) comparing the clinical efficacy of TCM combined with Western medicine with that of Western medicine alone for the treatment of DKD. The main outcome measure was 24-h UPRO. The secondary outcomes were serum creatinine (Scr), blood urea nitrogen (BUN), glycosylated hemoglobin (HbA1c), fasting blood glucose (FBG), total cholesterol (TC), and triglyceride (TG). Meta-analyses were performed using random-effects models. The revised Cochrane risk-of-bias tool was used to assess the risk of bias.
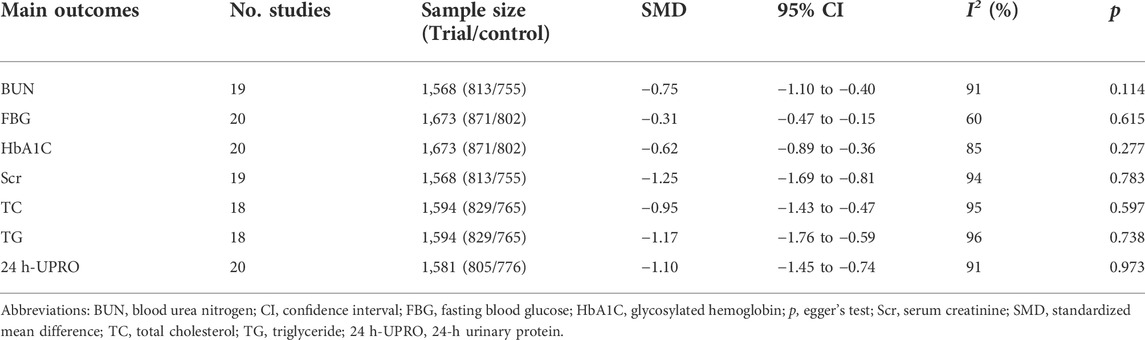
Results: A total of 44 RCTs with 3,730 participants were included. The summary estimates showed that compared with Western medicine alone, TCM combined with Western medicine significantly improved 24-h UPRO [standardized mean difference (SMD) −1.10, 95% confidence interval (CI) −1.45 to −0.74]. Moreover, TCM combined with Western medicine significantly reduced the levels of other renal function indices, including Scr (SMD −1.25, 95% CI: −1.69 to −0.81) and BUN (SMD −0.75, 95% CI: −1.10 to −0.40). TCM combined with Western medicine also showed greater benefits in reducing the levels of FBG (SMD −0.31, 95% CI: −0.47 to −0.15) and HbA1c (SMD −0.62, 95% CI: −0.89 to −0.36) in patients with DKD. In addition, superior effects on the lipid profile were noted in the TCM combined with Western medicine group in terms of TG (SMD −1.17, 95% CI: −1.76 to −0.59) and TC (SMD −0.95, 95% CI: −1.43 to −0.47). The risk of bias could have resulted from selective reports, unclear randomization methods, unblinded assignments, and some missing data.
Conclusion: The results of this meta-analysis suggest that TCM combined with Western medicine has significant effects on reducing 24-h UPRO and improves renal function indices and lipid profiles compared with Western medicine alone for DKD. However, the results should be interpreted with caution due to the risk of bias of the included trials.
Systematic Review Registration: [https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=213199], identifier [CRD: 42020213199].
1 Introduction
Globally, more than five million people die each year because they do not have access to critical treatment for kidney disease, and chronic kidney disease (CKD) is expected to be the fifth leading cause of death in the world by 2040. Approximately 30%–50% of the end-stage renal disease (ESRD) cases in the world are caused by diabetic kidney disease (DKD) (Ruiz-Ortega et al., 2020; Bakris et al., 2021). DKD has become the leading cause of ESRD in middle-aged and elderly individuals in China, and it is increasing worldwide at an alarming rate (KDOQI, 2007; Bourassa-Moreau et al., 2020). It is estimated that by 2035, the number of DKD patients will exceed 350 million (Gheith et al., 2016). The first symptom of DKD is microalbuminuria; with the progression of the disease, renal function continues to be impaired, and continuous microalbuminuria develops to massive albuminuria and eventually develops into ESRD (Afkarian et al., 2016; Chen et al., 2017; Wang et al., 2019). Proteinuria is the main independent risk factor for the progression of DKD (Hemmelgarn et al., 2010). At present, the treatment for reducing albuminuria in modern medicine is to administer drugs to control blood sugar and lower blood pressure (Emdin et al., 2015; Unger et al., 2020), including renin angiotensin aldosterone system (RAAS) blockers (Viberti et al., 1994; Haller et al., 2011; Unger et al., 2020), on the basis of lifestyle intervention (Perl et al., 2017; American Diabetes Association, 2019a). Drugs that can lower blood sugar and may reduce urinary protein to protect renal function include glucose cotransporter 2 inhibitors (SGLT2is) (Garofalo et al., 2019; Jardine et al., 2019; Heerspink et al., 2020), glucagon-like peptide-1 (GLP-1) receptor agonists (Marso et al., 2016; Mann et al., 2017; Muskiet et al., 2018; Pratley et al., 2019), and dipeptidyl peptidase (DPP)-4 inhibitors (Cornel et al., 2016; Groop et al., 2017; Mosenzon et al., 2017). However, the above methods cannot control the proteinuria of all patients with DKD.
In recent years, the field of traditional Chinese medicine (TCM) has represented a vast untapped resource for modern medicine. Researchers have begun to recognize TCM as a potential source of new drug candidates (Li and Zhang, 2008; Hu et al., 2017; Du et al., 2018). TCM acts on multiple targets through different signaling pathways to delay the progression of diseases (Gene Ontology Consortium, 2015). A large number of randomized controlled trials (RCTs) have shown that TCM combined with Western medicine in the treatment of DKD can better reduce urinary protein excretion and protect renal function (Tu et al., 2015; Wen et al., 2017). Mahuang Fuzi Shenzhuo decoction can enhance podocyte autophagy, inhibit the activation of the Wnt/β-Catenin signaling pathway stimulated by high glucose, and help to reduce podocyte injury in rats with DKD (Dai et al., 2020). The TCM capsule for replenishing qi and nourishing yins could significantly reduce the 24-h urinary albumin and the expression of CD34 and CD144 in the kidneys of DKD model rats and improve the pathological changes in glomerular hypertrophy, mesenteric matrix thickening, mesenteric thickening, and nodular hyperplasia (Zhou et al., 2019).
However, the current level of evidence-based medicine is still not enough due to the limitation of clinical center size and sample size. The evaluation and comparison of various treatment methods are not sufficient, and to the best of our knowledge, there is no comprehensive evaluation of the clinical efficacy of TCM combined with Western medicine [angiotensin-converting–enzyme inhibitor (ACEI)/angiotensin II receptor blocker (ARB)] in the treatment of DKD proteinuria under the guidance of different treatment methods.
The purpose of this meta-analysis is to provide a sufficient basis for the clinical application of TCM combined with Western medicine. We hope that the results of the study will provide clinicians with the best choice for the treatment of DKD proteinuria and provide them with a research direction.
2 Methods
This systematic review was guided by the recommendations for performing systematic reviews in the Cochrane Handbook, and the reporting was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. The review protocol was registered with PROSPERO before commencement (CRD: 42020213199).
2.1 Information sources and searches
Two independent reviewers searched through major databases, including PubMed, EMBASE, the Cochrane Library and Chinese Bio-Medical, from their initiation through March 2020 and updated in December 2021 using the detailed search strategy and specific terms [(traditional Chinese medicine or herbal medicine or Chinese herbal drug) and (diabetic kidney disease or diabetic nephropathy or diabetic nephrosclerosis or diabetic glomerulosclerosis) and (randomized controlled trial or controlled clinical trial or randomized or placebo)], which were searched as free text words and as MeSH/Entree terms. Supplementary Material shows the detailed search strategy for each database. In addition, the references of the retrieved trials and previous related systematic reviews were also manually reviewed to identify potential missing eligible trials.
2.2 Study selection and eligibility criteria
Original studies were reviewed, and data abstraction was conducted by two independent authors (XL and YX). A group discussion was carried out for any discrepancies during this step until consensus was achieved. A senior author (ZM) was consulted to obtain a confirming suggestion. When necessary, we contacted the corresponding authors of the original studies for detailed information.
Studies were considered appropriate and were included in the analysis if they satisfied the following established inclusion criteria.
(1) Adult participants aged at least 18 years were diagnosed with DKD or clinical DKD according to its diagnostic (Alicic et al., 2017; Anders et al., 2018) and staging criteria established by American Diabetes Association in 2020 the National Kidney Foundation Disease Outcomes Quality Initiative (KDOQI) guidelines36 and Mogensen staging (Mogensen et al., 1983). No restrictions were applied on the age, sex, ethnicity, region or economic status of the included participants.
(2) Patients in the treatment group were treated with TCM combined with Western medicine, while patients in the control group were treated with Western medicine alone. The treatment dose, duration and frequency were not limited. In addition, patients in both groups received the same routine treatment, including the integrated management of blood pressure and nutrition, as recommended by the clinical practice guidelines for chronic kidney disease (American Diabetes Association, 2019a), (American Diabetes Association, 2019b). Patients with nondiabetic proteinuria who had ESRD or who received renal replacement therapy were excluded from the study.
(3) Western medicine alone was used as a common comparator for this meta-analysis.
(4) Trials were included that evaluated at least one of the following outcomes. We selected 24-h urinary protein (24-UPRO) as the primary outcome measure because it was one of the major measurements used to diagnose CKD and other kidney diseases and was also commonly reported as the primary outcome in the literature. The secondary outcomes included protein and renal function indicators [including serum creatinine (Scr) and blood urea nitrogen (BUN)], fasting blood glucose (FBG), glycosylated hemoglobin (HbA1c), triglyceride (TG), and total cholesterol (TC).
(5) RCTs were included regardless of blinding. We did not apply date and language restrictions.
2.3 Data collection and quality assessment
For each trial, the following details concerning the PICOS characteristics were abstracted: first author, year of publication, patient age, sample size, interventions, and chief outcome indicators obtained from the study.
Two authors independently assessed the risk of bias for each RCT according to the recommendation criteria of the Cochrane Handbook for Systematic Reviews of Interventions (Cumpston et al., 2019). There were seven domains that were evaluated, including random sequence generation, allocation concealment, blinding methods (including investigators, participants, and outcome assessment), attrition bias, reporting bias and other sources of bias. Each potential source of bias was evaluated at three levels: high, low or unclear bias. Any disagreements between the two authors were resolved through discussion.
2.4 Data synthesis and analysis
All statistical analyses were carried out with Review Manager Software (version 5.3, Cochrane Community, UK). We used continuous variables in this meta-analysis to pool the effect estimates [standardized mean difference (SMD)] using the generic inverse variance method. All analyses were performed using a more conservative random‐effects model. Leave-one-out sensitivity analysis was applied to assess the stability of the overall effect estimates. The intertrial heterogeneity was assessed with I‐square and chi‐square tests, with I2 > 50% indicating significant heterogeneity. For the main outcome, we also conducted subgroup analyses to explore the potential sources of heterogeneity based on the baseline characteristics of the included RCTs. Publication bias was tested by funnel plots and Egger’s test when the number of included studies was more than 10 for the studied outcome. A value of p < 0.05 was considered statistically significant.
3 Results
3.1 Study selection
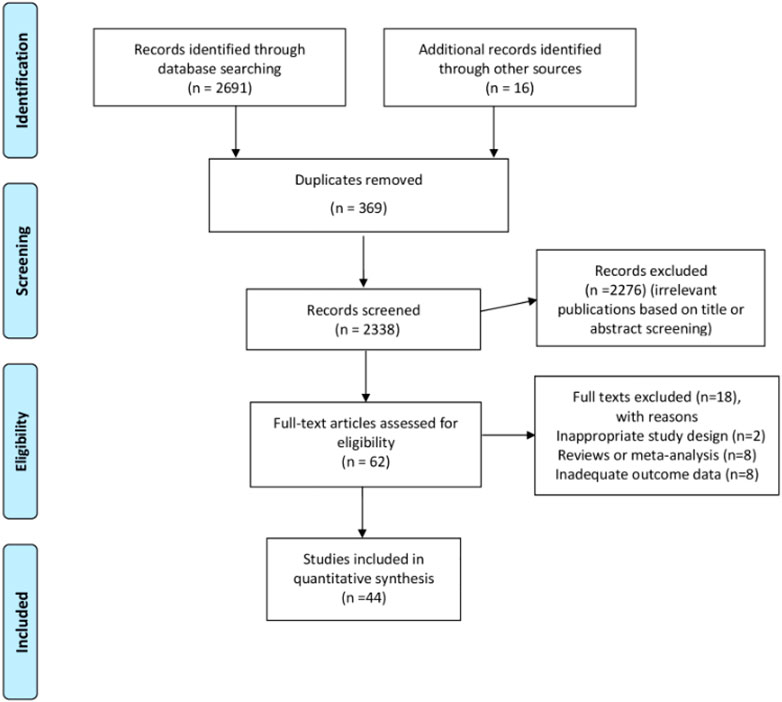
We present the flowchart of the literature search process in Figure 1. In summary, a total of 2,707 records were identified from the initial literature search. Our primary search strategy from the four major databases yielded 2,691 articles, including 265 records in PubMed, 409 records in Embase, 345 records in the Cochrane Library and 1,672 records in Chinese Bio-Medical. Moreover, 16 records were added through a manual reference search of related systematic reviews and original studies. EndNote X7 software was used to remove duplicate records, and 62 records remained for full-text review after we further removed unrelated records through title and abstract screening. During the process, 1,184 records were excluded due to studies being irrelevant to the effects of TCM on proteinuria in DKD patients. We carefully conducted the full-text review of the remaining 62 articles. Of these, 18 studies were excluded for multiple reasons, and 44 RCTs including 3,730 participants were finally included in the meta-analysis for the evaluation of TCM combined with Western medicine in the treatment of proteinuria in patients with DKD.
3.2 Study characteristics
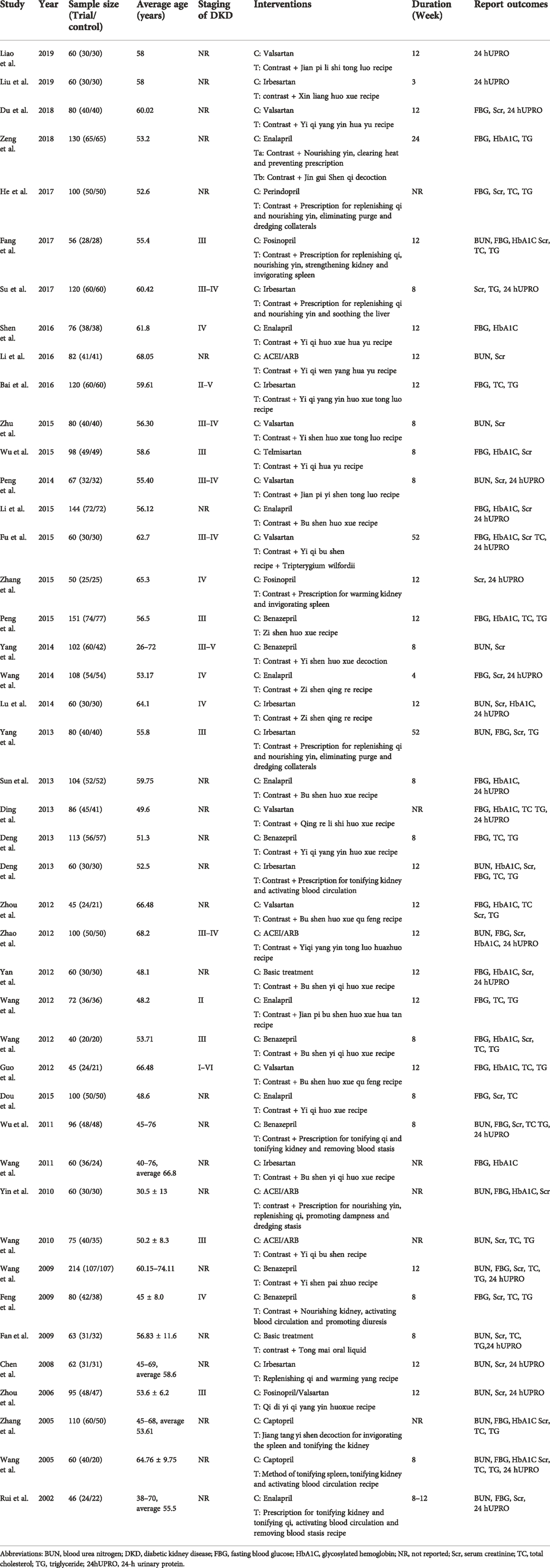
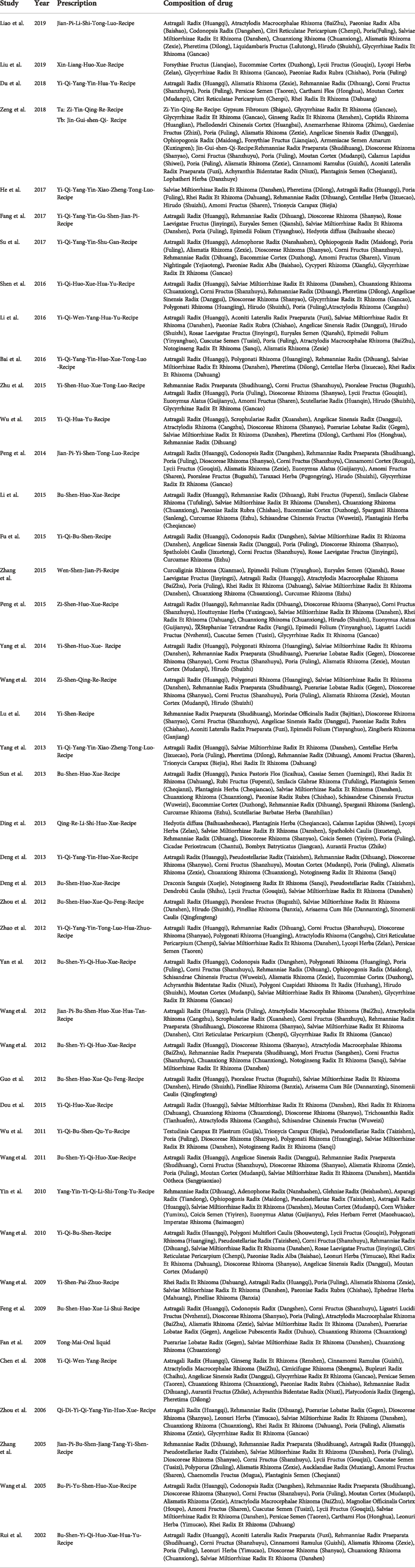
All 44 RCTs [39-83] included in this study investigated TCM combined with Western medicine in the treatment of proteinuria. All the articles were sourced from Chinese publications, and the trials were all conducted in China between 2012 and 2019. Overall, the combined patient sample size was 203, ranging from 45 to 214. The basic characteristics of the trial patients and controls as well as the interventions of the 44 eligible studies are displayed in Table 1. Summary results of the outcome measures are shown in Table 2. Studies of composition of prescription are displayed in Table 3.
3.3 Quality assessment (Risk of bias)
A summary of the risk of bias of the 44 RCTs is shown in Supplementary Figure S1. Two of the seven domains (allocation concealment and blinding methods) based on the Cochrane tool were rated as high risk of bias. Other limitations were identified as unclear risk of random sequence generation (54.5%), binding of outcome assessment (97.7%), and selective reporting (68.2%).
3.4 Outcomes
3.4.1 Primary outcome
3.4.1.1 24-h UPRO
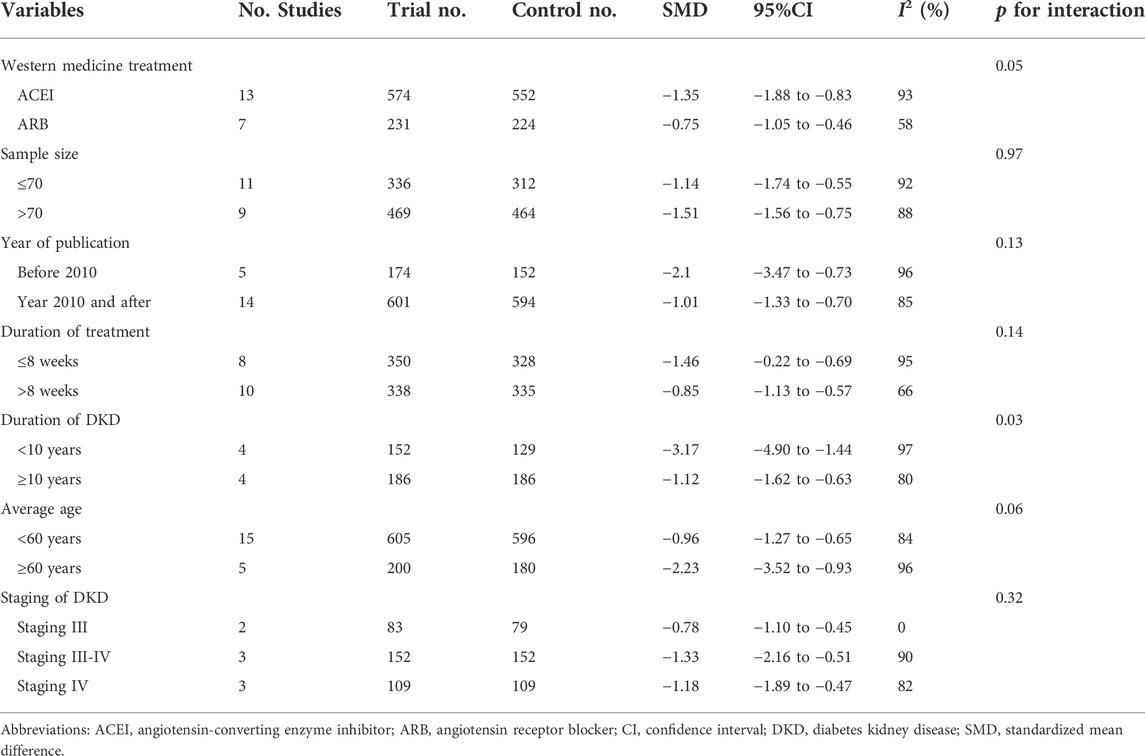
A summary of the effect estimate of the primary outcome is presented in Figure 2. In our analysis, TCM combined with Western medicine showed a greater improvement in the reduction of 24-h UPRO than Western medicine alone, with an SMD of −1.10 [95% confidence interval (CI) −1.45 to −0.74; n = 20 studies].
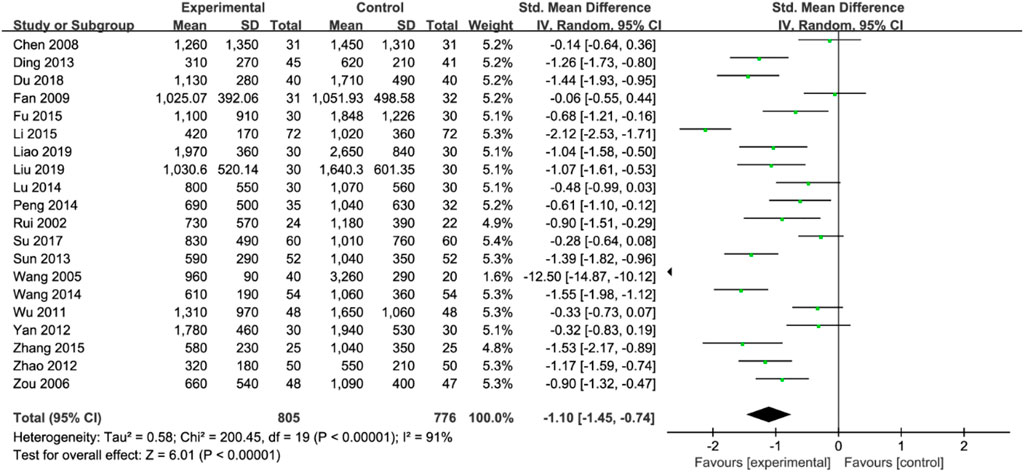
FIGURE 2. Forest plot for meta-analysis of the effect of TCM combined with Western medicine on 24-h urinary protein.
However, high interstudy heterogeneity was noted (I2 = 91%). We tried to investigate the potential sources of heterogeneity through subgroup analyses stratified by Western medicine intervention measures, study sample size, year of publication, treatment duration, duration of DKD, mean patient age and staging of DKD. The effect estimates of all the subgroups were consistent with the primary effect estimate, indicating that the result of the meta-analysis of the primary outcome was robust. Moreover, the I2 values for most of the subgroups were slightly or moderately reduced (Table 4), inferring that the stratified factors might be potential sources of heterogeneity. No publication bias was noted from the general inspection of funnel plot symmetry (Figure 3) and Egger’s test (p = 0.973).
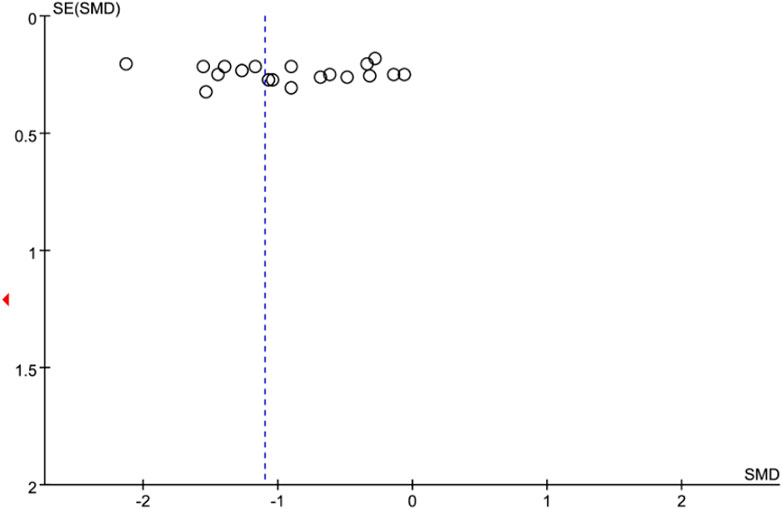
FIGURE 3. Funnel plot for meta-analysis of the effect of TCM combined with Western medicine on 24-h urinary protein.
3.4.2 Secondary outcomes
3.4.2.1 Fasting blood glucose
FBG levels were reported by 20 studies, with 871 participants in the interventional (TCM combined with Western medicine) group and 802 participants in the control (Western medicine alone) group. TCM combined with Western medicine significantly reduced the FBG level more than Western medicine alone [SMD: −0.31 (95% CI: −0.47 to −0.15)]. Subgroup analysis indicated that compared with that in patients treated with the control intervention, the FBG level was more significantly reduced in those with a longer course of treatment (>8 weeks) [SMD: −0.45 (95% CI: −0.68 to −0.22)] than in those with a shorter course of treatment (≤8 weeks) and in those with an older average age (≥60 years) [SMD −0.34 (95% CI: −0.54 to −0.14)] than in those with a younger average age (<60 years) (Supplementary Table S1).
3.4.2.2 Glycosylated hemoglobin
The HbA1c level was reported by 20 studies with 871 participants in the interventional group and 802 participants in the control group. Overall, the HbA1c level was significantly lower in the interventional group than in the control group [SMD: −0.62 (95% CI, −0.89 to −0.36)]. In the subgroup analysis, HbA1c levels were significantly lower in the interventional group among different subgroups stratified by baseline characteristics (Supplementary Table S2). However, there was no significant difference between the subgroups.
3.4.2.3 Serum creatinine
The Scr level was reported by 19 studies with 813 participants in the interventional group and 755 participants in the control group. Compared to the control group, the interventional group had a significantly lower Scr level [SMD −1.25 (95% CI: −1.69 to −0.81)]. In the subgroup analysis, the Scr level was significantly lower in those with a shorter duration of DKD (≤10 years) [SMD −2.81 (95% CI: −4.08 to −1.54)] than in those with a longer duration of DKD (>10 years) and in those with a younger average age (≤70 years) [SMD −0.92 (95% CI: −1.61 to −0.23)] than in those with an older average age (>70 years) (Supplementary Table S3).
3.4.2.4 Blood urea nitrogen
The BUN level was reported by four studies with 813 participants in the investigational group and 755 participants in the control group. The investigational group had a significantly higher BUN level than the control group [SMD −0.75 (95% CI: −1.10, −0.40)]. In the subgroup analysis, the BUN level was significantly lower in those with a shorter duration of DKD (<10 years) [SMD −1.30 (95% CI: −2.15 to −0.46)] than in those with a longer duration of DKD (≥10 years) and in those with an older average age (≥60 years) [SMD −1.44 (95% CI: −2.47 to −0.41)] than in those with a younger average age (<60 years) (Supplementary Table S4).
3.4.2.5 Total cholesterol
The TC level was reported by 18 studies with 829 participants in the interventional group and 765 participants in the control group. Compared to the control group, the interventional group had significantly lower TC levels [SMD −0.95 (95% CI: −1.43 to −0.47)]. In the subgroup analysis, the TC level was significantly lower in those with a longer duration of DKD (>5 years) [SMD −1.79 (95% CI: −2.57 to −1.02)] than in those with a shorter duration of DKD (≤5 years) and in those with an older average age (≥60 years) [SMD −1.36 (95% CI: −3.37 to −0.64)] than in those with a younger average age (<60 years) (Supplementary Table S5).
3.4.2.6 Triglyceride
TG was reported by 18 studies with 829 participants in the interventional group and 765 participants in the control group. Compared to the control group, the interventional group had a significantly lower TG level [SMD −1.17 (95% CI: −1.76 to −0.59)]. Subgroup analysis showed that compared with the control group, for the interventional group, the TG level was significantly lower for trials with larger sample sizes (>70) [SMD −1.41 (95% CI: −2.17 to −0.64)] than for trials with smaller sample sizes (p < 0.001) (Supplementary Table S6).
4 Discussion
4.1 Principal findings
This meta-analysis found that compared to Western medicine alone, traditional Chinese medicine (TCM) combined with Western medicine yielded significantly better clinical efficacy in the treatment of proteinuria in patients with diabetic kidney disease (DKD).
The 24-h urinary protein (24-h UPRO) level was significantly more improved in the intervention group than in the control group. Moreover, the levels of fasting blood glucose (FBG), glycosylated hemoglobin (HbA1c), blood urea nitrogen (BUN), total cholesterol (TC) and triglyceride (TG) were also generally more improved with the intervention of TCM combined with Western medicine.
4.2 Potential mechanisms
The potential mechanisms of TCM in the treatment of DKD and albuminuria are not clear. In recent years, under the guidance of the unique theoretical system of TCM, we found in clinical practice that TCM could alleviate the clinical symptoms related to DKD and improve renal function. Animal experiments have shown that astragaloside IV can relieve proteinuria and glomerulosclerosis in streptozotocin (STZ)-induced DKD mice, inhibit podocyte apoptosis, restore damaged autophagy, block autophagy or AMPK activation, and block the effect of astragaloside IV, suggesting that astragaloside IV partially delays the progression of DKD through AMPK-mediated autophagy induction (Du et al., 2018). Mangiferin is a natural xanthone extracted from Anemarrhena and other plants, and recent studies have shown that mangiferin can delay the progression of DKD in STZ-induced DKD rats and protect podocytes (Wang et al., 2018). Berberine is an extract of Coptis chinensis and Phellodendron Phellodendri that has the pharmacological effects such as reducing blood glucose and lipid levels and anti-inflammatory effects (Jin F. et al., 2017; Jin Y. et al., 2017; Sun et al., 2018). Adzuki bean extract has been reported to reduce the level of plasma glutathione and block the expression of heme oxygenase superoxide dismutase 1 and p47phox protein in DKD rats, which is consistent with the improvement of renal dysfunction and glucose metabolism disorder (Sato et al., 2016). Abelmoschus Manihot is an extract of okra that shows a nephroprotective effect by improving podocytosis and alleviating renal pathological changes in type 2 diabetic rats (Kim et al., 2018). It has received increasing attention in the treatment of DKD.
In the treatment of CKD with Western medicine, some commonly used drugs (such as hormones and immunosuppressants) are toxic, which may cause severe side effects and can affect patient quality of life during the treatment. The application of TCM combined with Western medicine according to the syndrome differentiation has been proved to not only increase the curative effect, prevent the rebound phenomenon, but also reduce the side effects such as Cushing syndrome, mental symptoms, and infection.
4.3 Implications
This meta-analysis found that compared to Western medicine alone, TCM combined with Western medicine has significant effects on reducing 24-h UPRO and improves renal function indices and lipid profiles compared with Western medicine alone for DKD. The results of the study will provide clinicians with the best choice for the treatment of DKD proteinuria and provide them with a research direction. The use of TCM combined with Western medicine in the treatment of DKD may improve the therapeutic effect.
4.4 Comparisons with previous reports
Some of the findings of this meta-analysis are in line with the findings of a previously published meta-analysis, which mainly focused on the effects of single herbs or specific formulations. Ren et al. (2019) investigated the clinical efficacy of Tripterygium wilfordii polyglycosides in the treatment of stage IV DKD and found that Tripterygium wilfordii polyglycosides could induce a significant decrease in albuminuria and Scr and increase in albumin. Based on 21 RCTs, it was found that Tripterygium wilfordii polyglycosides combined with ARB was superior to ACEI in reducing 24-h proteinuria. A recently published article regarding the Liuwei Dihuang Pill in the treatment of proteinuria in DKD showed that compared with TCM placebo, Liuwei Dihuang Pill had a better clinical effect in patients with DKD, but there was no significant difference in the HbA1c level (Ren et al., 2019). Though the results indicated that the effects of FBG and HbA1c examined in the study had great heterogeneity, the data suggested that the interventions of different prescriptions might be the reason for the heterogeneity, suggesting that different prescriptions had different effects on patients with DKD.
4.5 Strengths and limitations
Our study has several strengths. Firstly, this is the largest and most comprehensive pooled analysis regarding this topic which may provide high level evidence on the efficacy of TCM combined with Western medicine in the treatment of DKD. Secondly, we enumerated the compositions of each prescription for each trial so that the between-prescription differences could be more transparent (Table 4). Thirdly, compared with single prescriptions of TCM, this study included all the prescriptions of TCM for the treatment of DKD under the guidance of different principles of TCM treatment, which provides a more objective and comprehensive evaluation of TCM combined with Western medicine in the treatment of proteinuria in DKD patients. In addition, it is well known that instead of analyzing a single component of TCM, since each TCM contains a variety of compounds, it is better to analyze the whole TCM; for example, Astragalus membranaceus contains triterpene saponins, flavonoids, polysaccharides, and other components (Liu et al., 2020; Salehi et al., 2020; Guo et al., 2021). Thus, this study conducted a more comprehensive evaluation of the effects of TCM prescriptions at the multicomponent, multitarget and multipathway levels, which provided broadened new ideas for the treatment of proteinuria in DKD patients. Finally, the current systematic review involved the six most frequently assessed outcome indicators with the largest combined sample size. We also conducted multiple subgroup analyses to investigate the sources of heterogeneity and the robustness of the findings on the therapeutic effect of TCM on proteinuria and other serum indicators, providing high-level evidence for TCM combined with Western medicine in the treatment of DKD.
However, our study still has several limitations. Firstly, several trials included in our meta-analysis had a relatively small sample size, making some subgroup analyses less robust. Secondly, 17 of the included trials had a short follow-up period (<12 weeks), and the long-term effects of TCM on renal function and clinical outcomes should be further investigated in the future. Thirdly, more than half of the included trials did not provide details of the randomization and allocation procedures, so the impact of potential selection bias is unclear. Fourthly, since most of the participants in the trials were middle-aged and elderly individuals, the renal protective effect of TCM on young people and those with advanced kidney disease is still uncertain. In the included trials, the form of TCM used was a multicomponent TCM prescription developed according to the clinical experience with classic prescriptions or of famous TCM experts. At present, the drug-drug interactions and the detailed components of these TCM prescriptions are not clear. Fifthly, we did not test the side effects of TCM, which will be further focused on in our future studies. Finally, though we investigated the potential sources of heterogeneity through multiple subgroup analyses, the heterogeneity remained high. The difference in TCM composition could be one of the sources of heterogeneity.
This study has potential risk of bias in several aspects. Firstly, according to the risk of bias assessment of the included trials, we found that most of the trials had an obvious risk of bias in allocation concealment and blinding methods. Secondly, due to the lack of sufficient data, we only evaluated the overall clinical efficacy of TCM in the treatment of DKD, while not the effect of specific chemical components of TCM on DKD. Finally, the difference in observation time between trials might also influence the results. However, the results of multiple subgroup analyses and sensitivity analysis confirmed the robustness of the pooled estimates.
5 Conclusion
Based on this systematic review and meta-analysis of large sample size RCTs, we found that TCM combined with Western medicine has significant effects on reducing 24-h UPRO and improves renal function indices and lipid profiles compared with Western medicine alone for DKD. However, the results should be interpreted with caution due to the high heterogeneity and risk of bias of the included trials. This study also provides a theoretical basis for potential prescription selection and dispensing for further research. In the future, we propose that larger, well-designed, multicenter RCTs with long-term follow-up should be carried out to further confirm the long-term efficacy and safety of TCM in the treatment of DKD.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
Conceptualization: ZM, XL, and XY. Data curation: ZM, XL, MG, XZ, YX, and YZ. Formal analysis: ZM and XL, Funding acquisition: ZM and XY. Investigation: MG, YX, YZ, ZX, and XY. Methodology: ZM, MG, XZ, YX, ZX, and XY. Project administration: YX, Resources: MG, YX, and ZZ. Software: ZM and XL, Supervision: ZM and XY. Validation: ZM, MG, XZ, YX, YZ, ZX, ZZ, and XY. Visualization: MG and ZX. Writing—original draft: ZM and XL. Writing—review and editing: ZM and XL.
Funding
This work was supported by special funds for clinical research projects arranged by municipal finance in the budget of the Shanghai Shenkang Hospital Development Center (Project Number SHDC12019123) (to XY), the National Natural Science Foundation of China (grant no. 81774112 to ZM).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2022.1009571/full#supplementary-material
Abbreviations
ACEI, angiotensin-converting–enzyme inhibitor; ARB, angiotensin II receptor blocker; BUN, blood urea nitrogen; CI, confidence interval; CKD, chronic kidney disease; DKD, diabetic kidney disease; DPP, dipeptidyl peptidase; ESRD, end-stage renal disease; FBG, fasting blood glucose; GLP-1, glucagon-like peptide-1; HbA1c, glycosylated hemoglobin; KDOQI, National kidney foundation disease outcomes quality initiative; PRISMA, preferred reporting items for systematic reviews and meta-analyses; RAAS, renin angiotensin aldosterone system; RCTs, randomised controlled trials; Scr, serum creatinine; SGLT2is, glucose cotransporter 2 inhibitors; SMD, standardized mean difference; STZ, streptozotocin; TC, total cholesterol; TCM, traditional Chinese medicine; TG, triglyceride; 24-h UPRO, 24-h urinary protein.
References
Afkarian, M., Zelnick, L. R., Hall, Y. N., Heagerty, P. J., Tuttle, K., Weiss, N. S., et al. (2016). Clinical manifestations of kidney disease among US adults with diabetes, 1988-2014. Jama 316 (6), 602–610. doi:10.1001/jama.2016.10924
Alicic, R. Z., Rooney, M. T., and Tuttle, K. R. (2017). Diabetic kidney disease: Challenges, progress, and possibilities. Clin. J. Am. Soc. Nephrol. 12 (12), 2032–2045. doi:10.2215/CJN.11491116
American Diabetes Association (2019b). 16. Diabetes advocacy: Standards of medical care in diabetes-2019. Diabetes Care 42 (1), S182–S183. doi:10.2337/dc19-S016
American Diabetes Association (2019a). 5. Lifestyle management: Standards of medical care in diabetes-2019. Diabetes Care 42 (1), S46–s60. doi:10.2337/dc19-S005
Anders, H-J., Huber, T. B., Isermann, B., and Schiffer, M. (2018). CKD in diabetes: Diabetic kidney disease versus nondiabetic kidney disease. Nat. Rev. Nephrol. 14 (6), 361–377. doi:10.1038/s41581-018-0001-y
Bakris, G., Agarwal, R., and Filippatos, G.FIDELIO-DKD Study Group (2021). Finerenone and chronic kidney disease outcomes in type 2 diabetes. N. Engl. J. Med. 384 (11), e42. doi:10.1056/NEJMc2036175
Baoming, W., Shaoxia, L., and Wei, Z. (2010). Yi qi huo xue tonifying teratment of diabetie NePhroPathy clinical study of microalbuminuria. J. Pract. traditional Chin. Med. Intern. Med. 24 (09), 73–74. doi:10.3969/j.issn.1671-7813.2010.09.40
Binbin, D., Zhangzhi, Z., and Baoling, L. (2018). Clinical observation of Qi-yin-nourishing and Blood-stasis-resolving decoction combined with valsartan capsules on early diabetic nephropathy. Hebei Tradit. Chin. Med. 40 (05), 721–725+9. 10.3969.
Bourassa-Moreau, E., Versteeg, A., Moskven, E., Charest-Morin, R., Flexman, A., Ailon, T., et al. (2020). Sarcopenia, but not frailty, predicts early mortality and adverse events after emergent surgery for metastatic disease of the spine. Spine J. 20 (1), 22–31. doi:10.1016/j.spinee.2019.08.012
Chen, C., Wang, C., Hu, C., Han, Y., Zhao, L., Zhu, X., et al. (2017). Normoalbuminuric diabetic kidney disease. Front. Med. 11 (3), 310–318. doi:10.1007/s11684-017-0542-7
Chenghai, Z., Wenchao, Y., Ran, N., Hongyan, C., and Yongjia, L. (2012). Clinical observation on the treatment of diabetic nephropathy by replenishing qi, nourishing yin, dredging collaterals and resolving turbid. Beijing Tradit. Chin. Med. 31 (03), 207–210. 10.16025.
Cornel, J. H., Bakris, G. L., Stevens, S. R., Alvarsson, M., Bax, W. A., Chuang, L. M., et al. (2016). Effect of sitagliptin on kidney function and respective cardiovascular outcomes in type 2 diabetes: Outcomes from TECOS. Diabetes Care 39 (12), 2304–2310. doi:10.2337/dc16-1415
Cumpston, M., Li, T., Page, M. J., Chandler, J., Welch, V. A., Higgins, J. P., et al. (2019). Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for systematic reviews of interventions. Cochrane Database Syst. Rev. 10, Ed000142. doi:10.1002/14651858.Ed000142
Dai, H., Liu, F., Qiu, X., Liu, W., Dong, Z., Jia, Y., et al. (2020). Alleviation by mahuang fuzi and Shenzhuo decoction in high glucose-induced podocyte injury by inhibiting the activation of wnt/β-catenin signaling pathway, resulting in activation of podocyte autophagy. Evid. Based. Complement. Altern. Med. 2020, 7809427. doi:10.1155/2020/7809427
H. Dongying (Editor) (2017). “Effect of yiqi yangyin xiaozhuo tongluo traditional Chinese medicine combined with western medicine on urinary microalbumin in early diabetic nephropathy,” The fifth world congress on integrated traditional Chinese and western medicine in 2017 (Guangdong, China: Guangzhou).
Dou, X., Wu, J., Han, L., Yu, S., and Hu, R. (2012). The therapeutic effects of Yiqihouxue herb on the diabetic kidney disease. Shanxi Med. J. 41 (5), 3.
Du, N., Xu, Z., Gao, M., Liu, P., Sun, B., and Cao, X. (2018). Combination of Ginsenoside Rg1 and Astragaloside IV reduces oxidative stress and inhibits TGF-β1/Smads signaling cascade on renal fibrosis in rats with diabetic nephropathy. Drug Des. devel. Ther. 12, 3517–3524. doi:10.2147/dddt.S171286
Emdin, C. A., Rahimi, K., Neal, B., Callender, T., Perkovic, V., and Patel, A. (2015). Blood pressure lowering in type 2 diabetes: A systematic review and meta-analysis. Jama 313 (6), 603–615. doi:10.1001/jama.2014.18574
Fang, L., Jiangming, L., Aisheng, W., Weihua, M., Meiling, L., Xiaoxia, L., et al. (2014). Clinical study on warming kidney and nourishing yin in the treatment of type 2 diabetic nephropathy with deficiency of both yin and Yang. New tradit. Chin. Med. 46 (10), 95–97. 10.13457.
Fangting, W. (2011). Observation on the efficacy of tonifying qi and tonifying kidney and removing blood stasis in treating 48 cases of diabetic nephropathy. New tradit. Chin. Med. 43 (07), 32–33. 10.13457.
Garofalo, C., Borrelli, S., Liberti, M. E., Andreucci, M., Conte, G., Minutolo, R., et al. (2019). SGLT2 inhibitors: Nephroprotective efficacy and side effects. Med. Kaunas. 55 (6), E268. doi:10.3390/medicina55060268
Gene Ontology Consortium (2015). Gene Ontology Consortium: Going forward. Nucleic Acids Res. 43, D1049–D1056. doi:10.1093/nar/gku1179
Gheith, O., Farouk, N., Nampoory, N., Halim, M., and Al-Otaibi, T. (2016). Diabetic kidney disease: World wide difference of prevalence and risk factors. J. Nephropharmacol. 5 (1), 49–56.
Groop, P. H., Cooper, M. E., Perkovic, V., Hocher, B., Kanasaki, K., Haneda, M., et al. (2017). Linagliptin and its effects on hyperglycaemia and albuminuria in patients with type 2 diabetes and renal dysfunction: The randomized MARLINA-t2d trial. Diabetes Obes. Metab. 19 (11), 1610–1619. doi:10.1111/dom.13041
Guizhen, M., and Bailong, C. (2009). Clinical observation on the treatment of early diabetic nephropathy with jianpi bushen huoxue huatan method. Mod. distance Educ. traditional Chin. Med. China 7 (10), 101–102. 1672-2779 (2009) -10-0101-02. doi:10.3969/j.issn.1672-2779.2009.10.080
Guo, J. C., Pan, H. C., Yeh, B. Y., Lu, Y. C., Chen, J. L., Yang, C. W., et al. (2021). Associations between using Chinese herbal medicine and long-term outcome among pre-dialysis diabetic nephropathy patients: A retrospective population-based cohort study. Front. Pharmacol. 12, 616522. doi:10.3389/fphar.2021.616522
Haller, H., Ito, S., Izzo, J. L., Januszewicz, A., Katayama, S., Menne, J., et al. (2011). Olmesartan for the delay or prevention of microalbuminuria in type 2 diabetes. N. Engl. J. Med. 364 (10), 907–917. doi:10.1056/NEJMoa1007994
Heerspink, H. J. L., Stefánsson, B. V., Correa-Rotter, R., Chertow, G. M., Greene, T., Hou, F. F., et al. (2020). Dapagliflozin in patients with chronic kidney disease. N. Engl. J. Med. 383 (15), 1436–1446. doi:10.1056/NEJMoa2024816
Hemmelgarn, B. R., Manns, B. J., Lloyd, A., James, M. T., Klarenbach, S., Quinn, R. R., et al. (2010). Relation between kidney function, proteinuria, and adverse outcomes. Jama 303 (5), 423–429. doi:10.1001/jama.2010.39
Hu, J., Liu, S., Liu, W., Zhang, H., Chen, J., and Shang, H. (2017). Establishing an evaluation mode with multiple primary outcomes based on combination of diseases and symptoms in TCM clinical trials. Ann. Transl. Med. 5 (21), 420. doi:10.21037/atm.2017.06.06
Huafu, W., Yiping, Y., Zhihong, G., Xiaoru, Z., and Huiqin, X. (2014). Observation on the therapeutic effect of nourishing yin and clearing heat on patients with diabetic nephropathy. Strait Pharm. 26 (06), 110–112. doi:10.11655/zgywylc2014.07.003
Huawei, G., Jiajun, Z., and Liqun, H. (2012). Clinical observation on the effect of kidney-replenishing blood-promoting and pathogenic wind dispelling recipein the treatment of diabetic nephropathyin the stage of IV and V of spleen and kidney qi deficiencywith phlegm and blood stasis intermingled syndrome. Liaoning J. traditional Chin. Med. 39 (12), 2411–2413. 10.13192.
Huiping, C., and Xin, M. (2008). The curative effect observation of diabetic nephropathy treated with yiqiwenyang treatment. Chin. J. traditional Chin. Med. 26 (12), 2732–2734. 10.13193.
Jardine, M. J., Mahaffey, K. W., and Perkovic, V. (2019). Canagliflozin and renal outcomes in diabetic nephropathy. N. Engl. J. Med. 381 (11), 1089–1090. doi:10.1056/NEJMc1909687
Jiajie, F., Bin, Z., Jiazhen, Y., Liming, M., and Xiaoxia, C. (2015). A randomized controlled trial of the combination of yiqibushen decoction with Tripterygium glycosides and valsartan for the treatment of spleen and kidney deficiency type diabetic nephropathy. Chin. J. Nephrop. Integr. traditional Chin. West. Med. 16 (10), 881–883.
Jiajun, Z., and Huawei, G. (2012). Clinical effects of kidney-invigorating, blood-promoting and wind-dispelling therapy on diabetic nephropathy in IV and V stages and its influence on MCP-1. J. Shanghai Univ. traditional Chin. Med. 26 (02), 42–45. 10.16306.
Jian Wen, F. (2009). Curative effect observation to inciting the kidney blood and water circulation to treat diabetes nephrosis 42 cases. J. Zhejiang Univ. traditional Chin. Med. 33 (01), 61–63. 10.16466.
Jin, F., Zhihong, J., Guoyan, Z., and Zhiguang, Z. (2017). Clinical research of supplementing qi and nourishing yin, soliding kidney and invigorating the spleen for the treatment of early diabetic nephropathy. Chin. J. basic traditional Chin. Med. 23 (05), 659–661.
Jin, Y., Liu, S., Ma, Q., Xiao, D., and Chen, L. (2017). Berberine enhances the AMPK activation and autophagy and mitigates high glucose-induced apoptosis of mouse podocytes. Eur. J. Pharmacol. 794, 106–114. doi:10.1016/j.ejphar.2016.11.037
Kai, D. (2013). Clinical study on the method of clearing heat, promoting dampness and activating blood circulation in the treatment of diabetic nephropathy in stage III and IV. Inn. Mong. Tradit. Chin. Med. 32 (19), 50–52. 10.16040.
KDOQI (2007). KDOQI clinical practice guidelines and clinical practice recommendations for diabetes and chronic kidney disease. Am. J. Kidney Dis. 49(2):S12–S154. doi:10.1053/j.ajkd.2006.12.005
Kim, H., Dusabimana, T., Kim, S. R., Je, J., Jeong, K., Kang, M. C., et al. (2018). Supplementation of abelmoschus manihot ameliorates diabetic nephropathy and hepatic steatosis by activating autophagy in mice. Nutrients 10 (11), E1703. doi:10.3390/nu10111703
Li, X. J., and Zhang, H. Y. (2008). Western healers in traditional Chinese medicine. EMBO Rep. 9 (2), 112–113. doi:10.1038/sj.embor.7401166
Lihong, Z., JianHua, Z., and Pingfu, L. (2006). Clinical observation on qidi yiqi yangyin huoxue recipe in treating diabetic nephropathy at stage III clinical observation on qidi yiqi yangyin huoxue recipe in treating diabetic nephropathy at stage III and IV. Chin. J. Integr. traditional Chin. West. Med. 11, 1023–1026. doi:10.3321/j.issn:1003-5370.2006.11.017
Lin, Z. (2015). Clinical research of yishen huoxue tongluo yin in the treatment of diabetic nephropathy. J. traditional Chin. Med. 30 (07), 967–968. 10.16368.
Liu, Y. L., Zhang, Q. Z., Wang, Y. R., Fu, L. N., Han, J. S., Zhang, J., et al. (2020). Astragaloside IV improves high-fat diet-induced hepatic steatosis in nonalcoholic fatty liver disease rats by regulating inflammatory factors level via TLR4/NF-κB signaling pathway. Front. Pharmacol. 11, 605064. doi:10.3389/fphar.2020.605064
Lu, B., Jianghua, Z., Jinsheng, Z., Liwei, T., and Beibei, H. (2016). Effect of yiqi yangyin huoxue tongluo fang on blood glucose, lipid metabolism and blood rheology of of DN patients. Hebei J. traditional Chin. Med. 31 (03), 9–11. 10.16370.
Lushi, S., and Ping, C. (2016). Clinical curative effect observation and influence on quality of life of Supplementing Qi nourishing Yin and liver soothing methods in the treatment of diabetic nephropathy. J. Mod. Integr. traditional Chin. West. Med. 25 (26), 2867–2870. 10.3969.
Mann, J. F. E., Ørsted, D. D., Brown-Frandsen, K., Marso, S. P., Poulter, N. R., Rasmussen, S., et al. (2017). Liraglutide and renal outcomes in type 2 diabetes. N. Engl. J. Med. 377 (9), 839–848. doi:10.1056/NEJMoa1616011
Marso, S. P., Bain, S. C., Consoli, A., Eliaschewitz, F. G., Jódar, E., Leiter, L. A., et al. (2016). Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N. Engl. J. Med. 375 (19), 1834–1844. doi:10.1056/NEJMoa1607141
Mingli, Y., Xinghua, H., and Xiaojuan, H. (2014). Observation on therapeutic effect of yishen huoxue decoction on diabetic nephropathy with deficiency of both qi and yin and blood stasis syndrome. Shaanxi Tradit. Chin. Med. 35 (04), 408–410. 10.3969.
Mogensen, C. E., Christensen, C. K., and Vittinghus, E. (1983). The stages in diabetic renal disease. With emphasis on the stage of incipient diabetic nephropathy. Diabetes 32, 64–78. doi:10.2337/diab.32.2.s64
Mosenzon, O., Leibowitz, G., Bhatt, D. L., Cahn, A., Hirshberg, B., Wei, C., et al. (2017). Effect of saxagliptin on renal outcomes in the SAVOR-TIMI 53 trial. Diabetes Care 40 (1), 69–76. doi:10.2337/dc16-0621
Muskiet, M. H. A., Tonneijck, L., Huang, Y., Liu, M., Saremi, A., Heerspink, H. J. L., et al. (2018). Lixisenatide and renal outcomes in patients with type 2 diabetes and acute coronary syndrome: An exploratory analysis of the ELIXA randomised, placebo-controlled trial. Lancet. Diabetes Endocrinol. 6 (11), 859–869. doi:10.1016/s2213-8587(18)30268-7
Perl, J., Karaboyas, A., Morgenstern, H., Sen, A., Rayner, H. C., Vanholder, R. C., et al. (2017). Association between changes in quality of life and mortality in hemodialysis patients: Results from the DOPPS. Nephrol. Dial. Transpl. 32 (3), 521–527. doi:10.1093/ndt/gfw233
Ping, F., Haiying, Y., Yongjun, Z., and Nizhi, Y. (2009). Clinical study of the cinise medicine benefiting vital energy and promoting blood in treating the diabetic nephropathy with qi deficiency and blood stasis syndrome. Emerg. traditional Chin. Med. 18 (03), 367–369.
Pratley, R., Amod, A., Hoff, S. T., Kadowaki, T., Lingvay, I., Nauck, M., et al. (2019). Oral semaglutide versus subcutaneous liraglutide and placebo in type 2 diabetes (PIONEER 4): A randomised, double-blind, phase 3a trial. Lancet 394 (10192), 39–50. doi:10.1016/s0140-6736(19)31271-1
Ren, D., Zuo, C., and Xu, G. (2019). Clinical efficacy and safety of Tripterygium wilfordii hook in the treatment of diabetic kidney disease stage IV: A meta-analysis of randomized controlled trials. Med. Baltim. 98 (11), e14604. doi:10.1097/md.0000000000014604
Ruiz-Ortega, M., Rodrigues-Diez, R. R., Lavoz, C., and Rayego-Mateos, S. (2020). Special issue "diabetic nephropathy: Diagnosis, prevention and treatment. J. Clin. Med. 9 (3), E813. doi:10.3390/jcm9030813
Salehi, B., Carneiro, J. N. P., Rocha, J. E., Coutinho, H. D. M., Morais Braga, M. F. B., Sharifi-Rad, J., et al. (2020). Astragalus species: Insights on its chemical composition toward pharmacological applications. Phytotherapy Res. 35, 2445–2476. doi:10.1002/ptr.6974
Sato, S., Kataoka, S., Kimura, A., and Mukai, Y. (2016). Azuki bean (Vigna angularis) extract reduces oxidative stress and stimulates autophagy in the kidneys of streptozotocin-induced early diabetic rats. Can. J. Physiol. Pharmacol. 94 (12), 1298–1303. doi:10.1139/cjpp-2015-0540
Shulei, P. (2015). Clinical observation on the treatment of Diabetic Nephropathy with the method of invigorating the spleen and toni. Emerg. traditional Chin. Med. 24 (09), 1664–1665. 10.3969.
Shunyou, D., Ping, F., Zheng, Z., XiaoYan, C., and Yuyu, T. (2013). Clinical effect of nourishing kidney and activating blood circulation combined with irbesartan on early diabetic nephropathy. Chin. J. Gerontology 33 (01), 371005–399202. doi:10.3969/j.issn.1005-9202.2013.01.016
Sun, Y., Xia, M., Yan, H., Han, Y., Zhang, F., Hu, Z., et al. (2018). Berberine attenuates hepatic steatosis and enhances energy expenditure in mice by inducing autophagy and fibroblast growth factor 21. Br. J. Pharmacol. 175 (2), 374–387. doi:10.1111/bph.14079
Tang, Y. J., and Haiwen, D. (2012). Observation on the efficacy of Bushen Yiqi Huoxue recipe in the treatment of early diabetic nephropathy. Sichuan Tradit. Chin. Med. 30 (09), 94–95.
Tao, P., Li, P., Qingmei, T., Li, L., Jiping, L., Zhenyu, L., et al. (2015). Ziyin huoxue fang for qi- yin asthenia and blood stasis type of diabetic nephropathy with stage III. J. traditional Chin. Med. 30 (01), 32–34. 10.16368.
Ting, Z., Yanbin, G., and Wenming, Y. (2015). Wenshen jianpi and huayu tongluo methods in treating clinical-stage diabetic nephropathy. Chin. J. Exp. Prescr. 21 (20), 200–203. 10.13422.
Tu, X., Ye, X., Xie, C., Chen, J., Wang, F., and Zhong, S. (2015). Combination therapy with Chinese medicine and ACEI/ARB for the management of diabetic nephropathy: The promise in research fragments. Curr. Vasc. Pharmacol. 13 (4), 526–539. doi:10.2174/1570161112666141014153410
Tujinjun, S., Shaomin, H., and Hailing, F. (2016). Clinical observation of yiqi huoxue huayu tongluo herbs in the treatment of stage IV diabetic nephropathy. Bethune Med. J. 14 (03), 323–325. 10.16485.
Unger, T., Borghi, C., Charchar, F., Khan, N. A., Poulter, N. R., Prabhakaran, D., et al. (2020). 2020 International Society of Hypertension global hypertension practice guidelines. J. Hypertens. 38 (6), 982–1004. doi:10.1097/hjh.0000000000002453
Viberti, G., Mogensen, C. E., Groop, L. C., and Pauls, J. F. (1994). Effect of captopril on progression to clinical proteinuria in patients with insulin-dependent diabetes mellitus and microalbuminuria. European Microalbuminuria Captopril Study Group. JAMA J. Am. Med. Assoc. 271 (4), 275–279. doi:10.1001/jama.271.4.275
Wang, L., Wang, Y. H., Zhang, X. H., Yang, X. L., Wei, H. L., An, Z. C., et al. (2019). Effectiveness comparisons of traditional Chinese medicine on treating diabetic nephropathy proteinuria: A systematic review and meta-analysis. Med. Baltim. 98 (43), e17495. doi:10.1097/md.0000000000017495
Wang, X., Gao, L., Lin, H., Song, J., Wang, J., Yin, Y., et al. (2018). Mangiferin prevents diabetic nephropathy progression and protects podocyte function via autophagy in diabetic rat glomeruli. Eur. J. Pharmacol. 824, 170–178. doi:10.1016/j.ejphar.2018.02.009
Weihua, L., and Weihua, R. (2015). Analysis of clinical efficacy of enalapril combined with tonifying the kidney and promoting blood circulation method on diabetic nephropathy. Chin. J. basic Med. traditional Chin. Med. 21 (08), 980–981+4.
Wen, Y., Yan, M., Zhang, B., and Li, P. (2017). Chinese medicine for diabetic kidney disease in China. Nephrology 22, 50–55. doi:10.1111/nep.13149
Wenlong, Z. (2005). Clinical observation on 60 cases of diabetic nephropathy treated with the method of invigorating spleen and tonifying kidney. Emerg. traditional Chin. Med. 2005 (10), 946–947. doi:10.3969/j.issn.1004-745X.2005.10.018
Xiao, L., and Jinsong, C. (2019). Clinical observation of invigorating spleen, promoting dampness and dredging collaterals in the treatment of diabetic nephropathy proteinuria. latest Med. Inf. Abstr. World 19 (28), 167–168. 10.19613.
Xiaochun, N., Weijie, J., Xuguang, Z., and Xiaohong, Z. (2019). Clinical study on Zhibai Dihuang Pills combined with irbesartan in treatment of diabetic nephropathy. Mod. Med. Clin. 34 (05), 1488–1491. 10.7501.
Xiaoguang, W., Dacheng, W., and Qihua, Z. (2005). Effect of tonifying spleen, tonifying kidney in review 23 and activating blood circulation on lipid metabolism and TXA_2/PGI_2 balance in elderly patients with clinical diabetic nephropathy. Beijing Tradit. Chin. Med. 2005 (02), 70–73. doi:10.3969/j.issn.1674-1307.2005.02.002
Xiaomin, D., and Chaofeng, G. (2013). Clinical application of yiqi yangyin huoxue recipe in the treatment of early diabetic nephropathy with deficiency of both qi and yin and blood stasis. Glob. Tradit. Chin. Med. 6 (09), 661–664. 10.3969.
Xingmin, W., Kexiao, S., Haifeng, J., Liwei, L., and Feng, L. (2011). Clinical observation of irbesartan combined with Bushen Yiqi Huoxue decoction in the treatment of 36 cases of early diabetic nephropathy. Sci. Technol. traditional Chin. Med. 18 (03), 232–233. doi:10.3969/j.issn.1005-7072.2011.03.039
Xiuxia, W., Yaping, Z., and YuZhong, W. (2009). Clinical study of Yishen Paizhuo decoction combined with benazepril in the treatment of Diabetic Nephropathy. Liaoning J. traditional Chin. Med. 36 (06), 986–988.
Xuemin, W. (2015). Effect of Chinese medicine yiqi huayu on the cell factor levels of early diabetic nephropathy. J. traditional Chin. Med. 30 (09), 1270–1272. 10.16368.
Xufeng, L., Shujin, W., Hong, Z., Guohong, L., Jia, F., Hua, Y., et al. (2018). Effects of xin xue huoxue recipe on urinary protein and related factors in diabetic nephropathy. World tradit. Chin. Med. 13 (06), 1436–1438+43. 10.3969.
Yan, W., Ping, H., Mingjie, F., Zhenghua, X., Junzhou, F., and Zhixin, L. (2012). Analysis of clinical effects on Chinese medicine of strengthening spleen and tonifying kidney and invigoration blood in the treatment of early type II diabetic nephropathy. China Med. Her. 9 (05), 99–101+3. doi:10.3969/j.issn.1673-7210.2012.05.044
Yani, H., and Lirong, L. (2016). Blood pressure management for patients with diabetic nephropathy. Chin. Electron. J. Nephrop. Res. 5 (04), 152–154. doi:10.3877/cma.j.issn.2095-3216.2016.04.002
Yi, S., and Mianzhi, Z. (2013). Treatment of clinical-stage diabetic nephropathy with therapy of tonifying kidney and activating blood. J. Beijing Univ. traditional Chin. Med. 36 (05), 353–356. 10.3969.
Yirong, R. (2002). Observation on the efficacy of tonifying kidney, replenishing qi, activating blood circulation and removing blood stasis combined with enalapril in the treatment of diabetic nephropathy. Shenzhen J. Integr. traditional Chin. West. Med. 2002 (12), 40–41. 10.16458.
Yupeng, L. (2016). Observation on the clinical effect of invigorating qi and warming Yang for removing blood stasis method in the treatment of diabetic nephropathy. Bright Tradit. Chin. Med. 31 (23), 3455–3457. 10.3969.
Zhenxiang, Y., Lizhong, G., and Miaowen, J. (2010). Replenish yin nourishi QI eliminate wetness tongyu method treatment of diabetic nephropathy. J. Pract. traditional Chin. Med. Intern. Med. 24 (09), 75–76. doi:10.3969/j.issn.1671-7813.2010.09.41
Zhou, X., Xu, C., Wang, K., Chu, Q., Dong, C., Wu, C., et al. (2019). Effect of traditional Chinese medicine for replenishing qi, nourishing yin and activating blood on renal Notch/Hes1 signaling in rats with diabetic nephropathy. Nan Fang. Yi Ke Da Xue Xue Bao 39 (7), 855–860. doi:10.12122/j.issn.1673-4254.2019.07.17
Keywords: traditional Chinese medicine, diabetic kidney disease (DKD), pooled analysis, randomized controlled trials (RCT), clinical efficacy
Citation: Liu X, Ge M, Zhai X, Xiao Y, Zhang Y, Xu Z, Zhou Z, Mei Z and Yang X (2022) Traditional Chinese medicine for the treatment of diabetic kidney disease: A study-level pooled analysis of 44 randomized controlled trials. Front. Pharmacol. 13:1009571. doi: 10.3389/fphar.2022.1009571
Received: 02 August 2022; Accepted: 26 September 2022;
Published: 13 October 2022.
Edited by:
Jaw-Wen Chen, Taipei Veterans General Hospital, TaiwanReviewed by:
Bin Deng, Huazhong University of Science and Technology, ChinaPing Fu, Sichuan University, China
Shih-Jie Chou, Taipei Veterans General Hospital, Taiwan
Copyright © 2022 Liu, Ge, Zhai, Xiao, Zhang, Xu, Zhou, Mei and Yang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zubing Mei, herrmayor@126.com; Xuejun Yang, yangxuejun@shutcm.edu.cn
†These authors share first authorship
 Xuele Liu
Xuele Liu Minyao Ge2†
Minyao Ge2† Yang Xiao
Yang Xiao Zhiguang Zhou
Zhiguang Zhou Zubing Mei
Zubing Mei Xuejun Yang
Xuejun Yang