Working Towards a Treat-to-Target Protocol in Juvenile Proliferative Lupus Nephritis – A Survey of Pediatric Rheumatologists and Nephrologists in Germany and Austria
- 1Department of Pediatrics, RWTH Aachen University Hospital, Aachen, Germany
- 2Department of Pediatrics, Medizinische Fakultät Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany
- 3Department of Pediatric Rheumatology, Alder Hey Children’s NHS Foundation Trust Hospital, Liverpool, United Kingdom
- 4Department of Women’s and Children’s Health, Institute of Life Course and Medical Sciences, University of Liverpool, Liverpool, United Kingdom
- 5Universitätsmedizin Hamburg, Kinder- und Jugendklinik, Hamburg, Germany
- 6Department of Pediatrics, Kinderkrankenhaus Amsterdamer Strasse, Cologne, Germany
- 7Department of Pediatrics, Pediatric Rheumatology, Medizinische Universität Innsbruck, Innsbruck, and Danube Private University, Krems an der Donau, Austria
- 8Clinic for Pediatrics III, University Hospital Essen, Essen, Germany
- 9Department of Pediatric Rheumatology, Clementine Kinderhospital, Frankfurt, Germany
- 10Center for Pediatric Rheumatology, Olgahospital, Stuttgart, Germany
- 11German Rheumatism Research Center, Leibniz Institute, Berlin, and Charité Universitätsmedizin Berlin, Pediatric Pneumology, Immunology and Critical Care Medicine and SPZ (Center for Chronically Sick Children), Berlin, Germany
- 12Department of Pediatric Rheumatology and Immunology, University Hospital, Münster, Germany
- 13Department of Pediatrics I, University Children’s Hospital, Heidelberg, Germany
- 14Division of Pediatric Nephrology, Children’s and Adolescents’ Hospital, University Hospital of Cologne, Faculty of Medicine, University of Cologne, Cologne, Germany
- 15Clementine Kinderhospital Frankfurt, Frankfurt, Germany
- 16Department of Pediatric Gastroenterology, Nephrology and Metabolic Diseases, Charité Universitätsmedizin Berlin, Berlin, Germany
- 17Division of Pediatric Nephrology, Olgahospital, Klinikum Stuttgart, Stuttgart, Germany
- 18Division of Pediatric Diabetology/Endocrinology, University Hospital Magdeburg, Magdeburg, Germany
- 19Clinic of Pediatrics and Adolescent Medicine, University Medical Center Göttingen, Göttingen, Germany
- 20Department of Pediatric Kidney, Liver and Metabolic Diseases, Hannover Medical School, Hanover, Germany
Background: To describe treatment practices for juvenile proliferative lupus nephritis (LN) class III and IV of pediatric rheumatologists and nephrologists in Germany and Austria in preparation for a treat-to-target treatment protocol in LN.
Methods: Survey study by members of the Society for Pediatric and Adolescent Rheumatology (GKJR) and the German Society for Pediatric Nephrology (GPN) on diagnostics and (concomitant) therapy of LN.
Results: Fifty-eight physicians completed the survey. Overall, there was a considerable heterogeneity regarding the suggested diagnostics and management of juvenile proliferative LN. Increased urinary protein excretion, either assessed by 24 h urine collection or spot urine (protein-creatinine ratio), and reduced estimated glomerular filtration rate were specified as important parameters for indication of kidney biopsy to diagnose proliferative LN and monitoring of therapy. Corticosteroids were generally proposed for induction and maintenance therapy, most often in conjunction with either mycophenolate mofetil (MMF) or cyclophosphamide (CP) as steroid-sparing immunosuppressants. MMF was clearly preferred over CP for induction therapy of LN class III, whereas CP and MMF were equally proposed for LN class IV. MMF was most often recommended for maintenance therapy in conjunction with oral corticosteroids and continued for at least 3 years and 1 year, respectively, after remission. Hydroxychloroquine was widely accepted as a concomitant measure followed by renin-angiotensin system inhibitors in cases of arterial hypertension and/or proteinuria.
Conclusion: The majority of pediatric rheumatologists and nephrologists in Germany and Austria propose the use of corticosteroids, most often in combination with either MMF or CP, for treatment of proliferative LN in children. The considerable heterogeneity of responses supports the need for a treat-to-target protocol for juvenile proliferative LN between pediatric rheumatologists and nephrologists.
Introduction
Lupus nephritis (LN) is a substantial cause of morbidity and mortality among patients with systemic lupus erythematosus (SLE). Within 10 years of an initial SLE diagnosis, 5–20% of patients with LN develop end-stage kidney disease (1). In up to 20% of all SLE patients, the onset of the disease occurs in childhood or adolescence (2). By contrast to adults, 50 to 60% of patients with juvenile onset SLE will develop lupus nephritis (3–6).
In German registries [National Pediatric Rheumatologic Database and German Lupus Nephritis Registry of the German Society for Pediatric Nephrology (GPN)], approximately 20 patients with LN per year are newly documented (with the possibility of underrepresentation due to the level of awareness of the registries) (7). The small number of cases distributed over several centers hampers a standardized procedure for this difficult-to-treat disease.
To improve long-term outcomes in children and adolescents with rheumatic diseases, the definition and evaluation of therapeutic strategies (treat-to-target, T2T) is an important tool (8). To develop these tools, the PRO-KIND initiative (Projekte zur Klassifikation, Überwachung und Therapie in der Kinderrheumatologie/Projects on classification, monitoring and therapy in pediatric rheumatology) within the Commission of the Society for Pediatric and Adolescent Rheumatology (Gesellschaft für Kinder- und Jugendrheumatologie, GKJR) was founded in 2015. Their task is to develop T2T protocols for the most prevalent pediatric rheumatic diseases in Germany, some of which have been published (9–15). In 2019, the initiative received funding from the Joint Federal Committee (Gemeinsamer Bundesausschuss, GBA) to evaluate the practicability and effectiveness of these protocols. To achieve this aim, 500 patients with new-onset rheumatic diseases will be recruited in a register study and treatment of these patients will be prospectively followed for 12 months. The register is currently recruiting patients until September 2022.
For SLE and specifically for LN, there is currently no T2T therapy protocol, while consensus treatment plans (CTPs) of the Childhood Arthritis and Rheumatology Research Alliance (CARRA) and the Single Hub and Access point for pediatric Rheumatology in Europe (SHARE) initiative’s recommendations are available (16, 17). Therefore, the development of an agreed consensus treatment protocol between pediatric rheumatologists and nephrologists is a key goal. To develop such a protocol, the PRO-KIND SLE working group evolved and conducted a survey together with the SLE working group of the GPN. This survey addressed current diagnosis and treatment of patients with proliferative LN in Germany and Austria on the basis of different case vignettes. The survey was distributed via the mailing lists of GKJR and GPN, and 58 German-speaking pediatric rheumatologists and nephrologists completed this survey and the data is presented here.
Materials and Methods
Survey
A survey (Supplementary Appendix) was developed by the PRO-KIND SLE working group and representatives of the GPN. The survey consisted of 25 closed and open-ended questions. Questions (a combination of Likert scale, multiple choice, and open comments) included:
– The respondent’s field of activity and type of workplace, as well as their age group
– Whether the respondents are currently treating patients with SLE or how many they have treated in their career so far
– The description of patients with LN WHO class III or IV and further detailed questions on
∘ Diagnostics,
∘ Indication for kidney biopsy in SLE patients,
∘ Activity assessment of SLE,
∘ Therapy for proliferative LN class III or IV,
∘ Definition of response to therapy in LN and,
∘ Concomitant therapies and preventive measures in SLE or LN.
In August 2016, the survey link was mailed to pediatric rheumatologists and nephrologists via the mailing lists of GKJR and GPN. Responses were collected via SurveyMonkey®; a follow-up message was sent out once to encourage survey completion after a few weeks. Data collection was closed in January 2017.
Analysis
Percentages and mean values were determined from the Likert scale and multiple-choice question responses. Rating averages were calculated by adding up the score results of the Likert scale and dividing it by the number of respondents. Open-ended comments were analyzed.
Case Vignette
A 15-year-old previously healthy girl with a suspected diagnosis of SLE meeting 7 of 11 American College of Rheumatology (ACR) classification criteria (18) (malar rash, photosensitivity, oral ulcers, renal disorder, hematologic disorder, positive ANA titer, and immunologic disorder) was presented in a case vignette once with LN class III and once with LN class IV. Based on this case vignette, questions regarding further diagnostic and therapeutic procedures were queried in the survey (see Supplementary Appendix for full survey).
Results
Respondent Demographics
Of all pediatric rheumatologists (n = 129) and nephrologists (n = 315) contacted, a total of 58 responded and 42 fully completed the survey, resulting in a response rate of 13 and 9.5%, respectively. Most respondents (n = 25) belong to the age group of 41–50 years, the others belong to the age groups 51–60 years (n = 19), 31–40 years (n = 8) and >60 years (n = 6), respectively (Figure 1A).
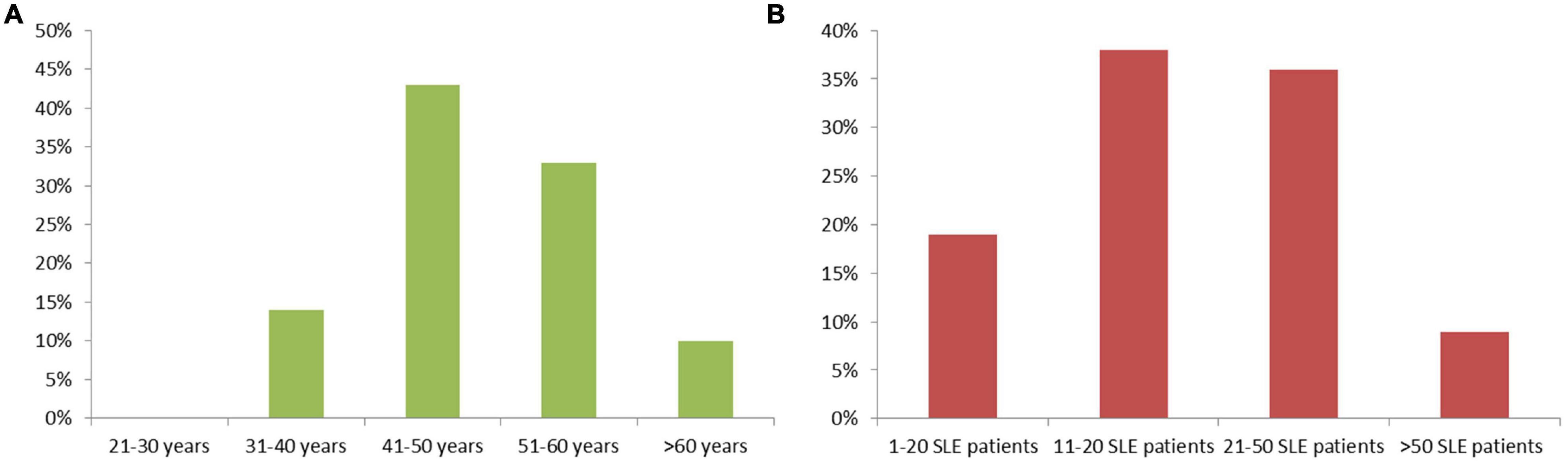
Figure 1. (A) Age distribution of survey respondents, and (B) numbers of SLE patients treated by each survey respondent.
The participants were mostly pediatric rheumatologists (60%), followed by pediatric nephrologists (35%) and general pediatricians (5%). More than half (54%) work at a university hospital, 44% at a non-university hospital, and one participant in a general pediatric practice.
Of the participants 38% have cared for 11–20 SLE patients in their career to date, while 36% have cared for 21–50 SLE patients, 19% have treated 1–10 and 7% have treated more than 50 SLE patients (Figure 1B).
Diagnostics
The vast majority of survey respondents (91%) would involve a pediatric nephrologist in the initial diagnosis and treatment planning of a patient with LN; other disciplines involved by the majority are ophthalmologists and cardiologists (see Table 1). 55% of respondents would suggest consulting a pediatric rheumatologist, which suggests that, depending on the presentation of the patient, pediatric rheumatologists are less frequently involved in the initial diagnosis and treatment planning.
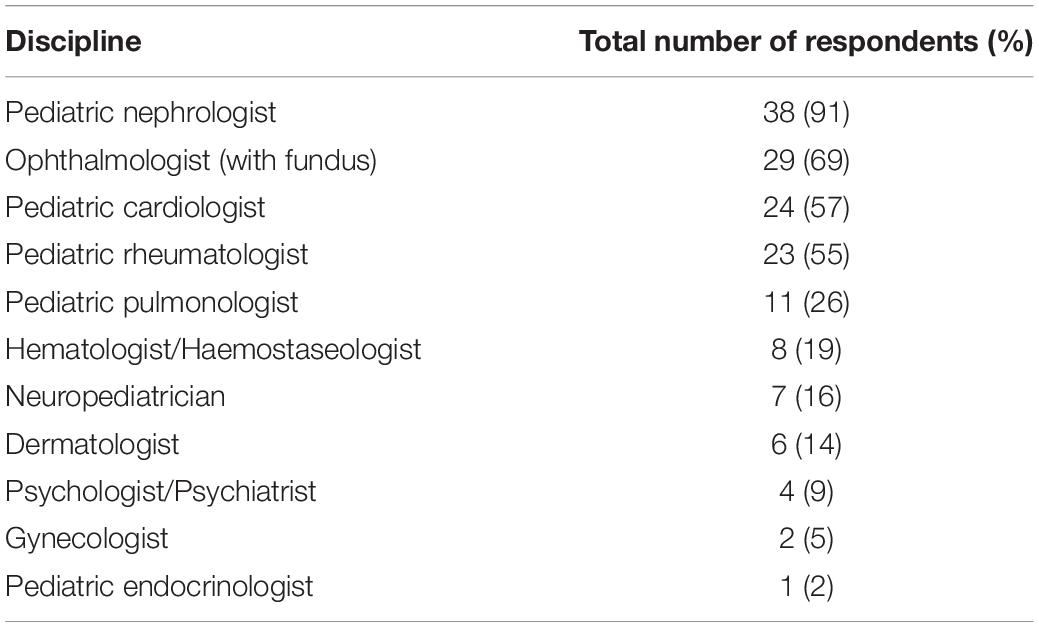
Table 1. Consultants involved in the diagnosis and treatment planning of an SLE patient with suspected LN.
When assessing the extent of LN, protein excretion in 24 h collection urine (>300 mg/m2 and 24 h or ≥0.5 g per 24 h) was rated as most essential, above the protein-creatinine ratio in spot urine (>0.2 g/g or >20 mg/mmol). However, several other parameters, e.g., dip-stick protein, and serum creatinine were also considered helpful (see Table 2).
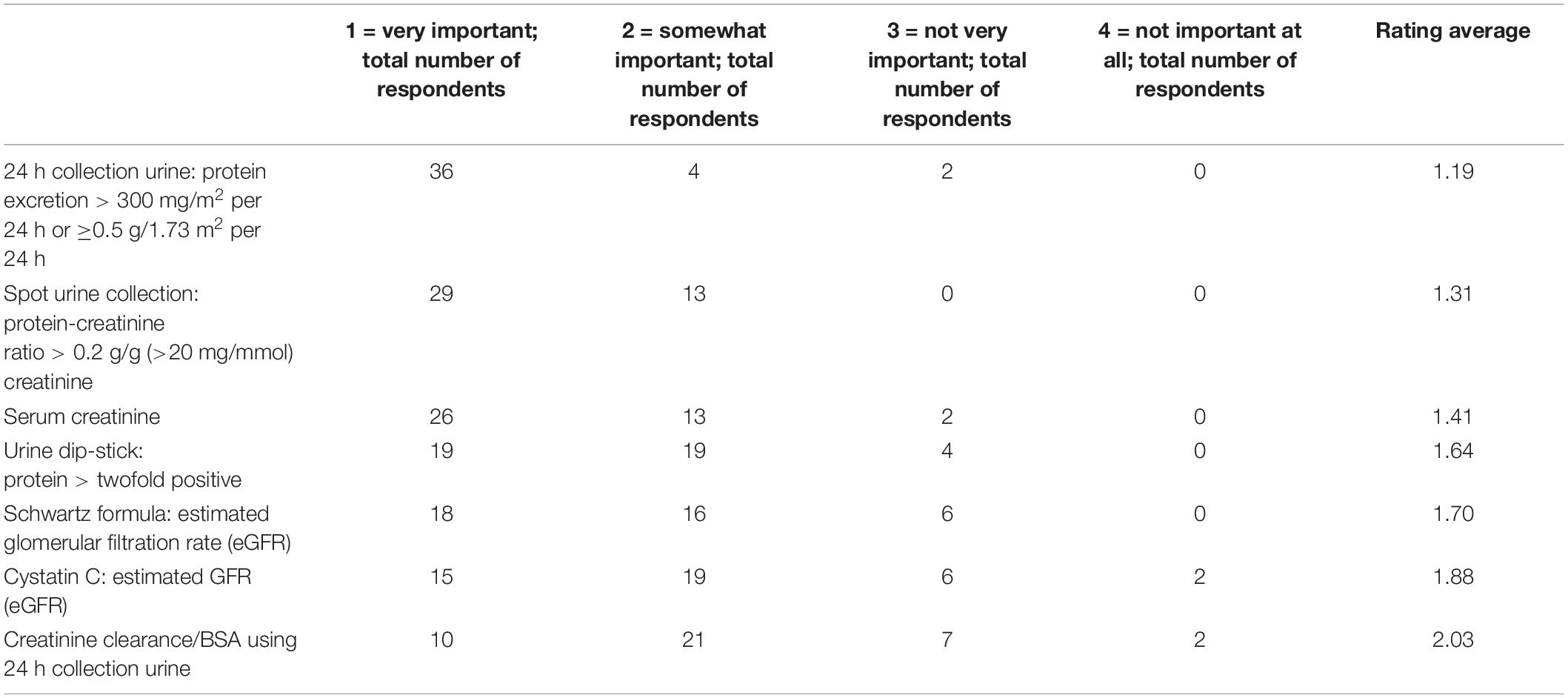
Table 2. Laboratory parameters in terms of their importance in assessing the extent of LN (answers by Likert scale: 1 = very important, 2 = somewhat important, 3 = not very important, 4 = not important at all; with rating average of respondents).
Kidney Biopsy for Diagnosis of Lupus Nephritis
According to the majority of the respondents (98%), the decision to perform a kidney biopsy is made on the basis of relevant pathological urine and kidney findings. A pathologic urine finding requiring kidney biopsy was agreed upon by 100% (n = 42) of respondents for nephrotic-range proteinuria [>1 g/m2 per 24 h or protein-creatinine ratio > 2 g/g creatinine (>200 mg/mmol)], 98% (n = 41) for rapidly progressive proteinuria, 62% (n = 26) for pathologic urine status (e.g., >5 erythrocytes/high power field and/or detection of RBC casts) with mild-moderate proteinuria (≤1 g/m2 per 24 h or protein-creatinine ratio 0.2–2 g/g creatinine or 20–200 mg/mmol), 48% for mild-moderate proteinuria with normal urine status, and 24% for pathologic urine status without mild-moderate proteinuria. Pediatric nephrologists tended to propose more frequently isolated mild-moderate proteinuria as an indicator for kidney biopsy as compared to rheumatologists (60 vs. 45%). Parameters also considered important for the indication of a kidney biopsy are listed in Table 3, including reduced eGFR < 60 ml/min per 1.73 m2 and an increase in serum creatinine. By contrast, highly elevated double-stranded DNA antibodies alone and patients’ ethnicity were considered not very important.
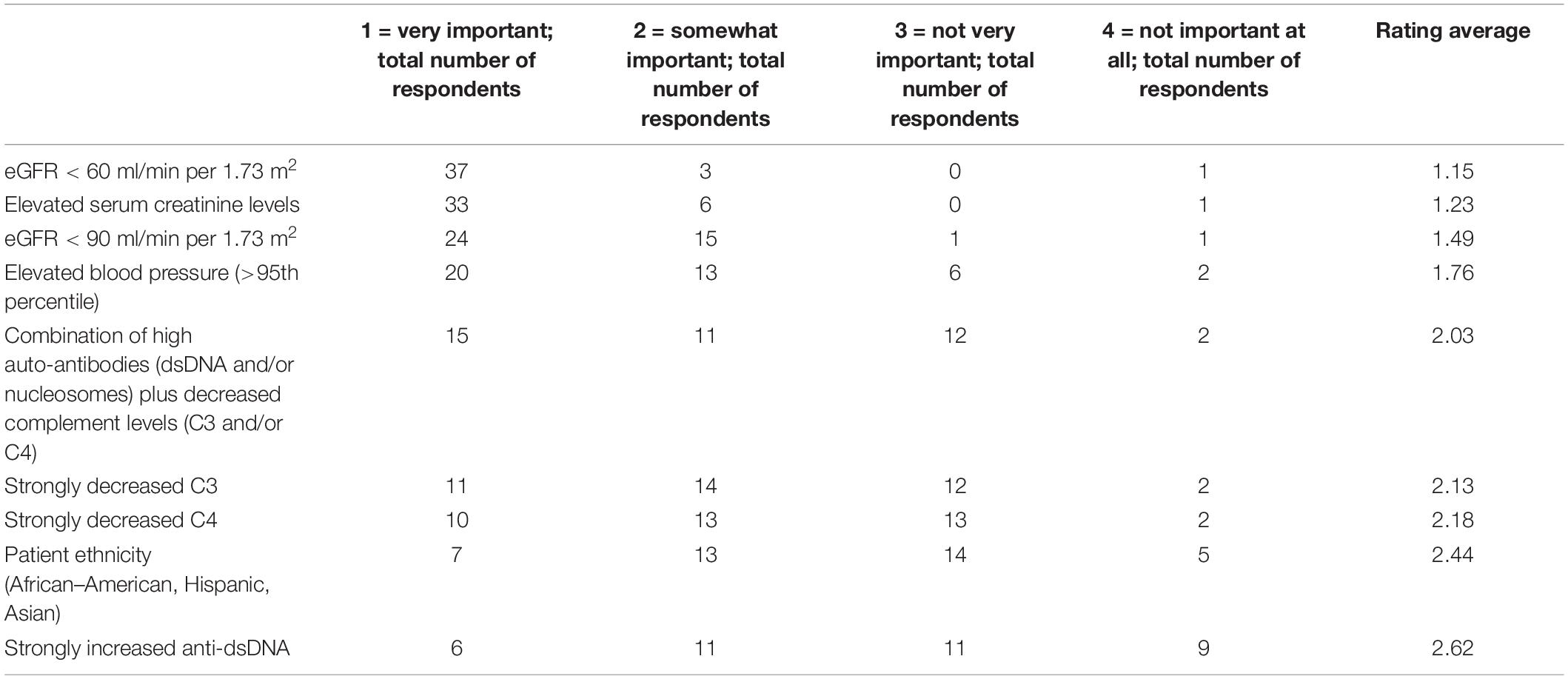
Table 3. Other relevant parameters for the indication of a kidney biopsy (answers by Likert scale: 1 = very important, 2 = somewhat important, 3 = not very important, 4 = not important at all; with rating average of respondents).
Activity Assessment of Systemic Lupus Erythematosus
To monitor SLE activity, more than 90% of respondents suggest the use of the Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) as a validated tool; further, Physician Global Assessment (76%), Parent/Patient Global Assessment (64%), and Childhood Health Assessment Questionnaire (C-HAQ) (52%) were considered relevant. Other tools such as Simple Measure of Impact of Lupus Erythematosus in Youngsters (SMILEY), which is not available in German, and European Consensus Lupus Activity Measurement (ECLAM) (10% each) and British Isles Lupus Assessment Group (BILAG) index (5%) were considered less relevant.
Therapy for Systemic Lupus Erythematosus With Proliferative Lupus Nephritis Class III
As the answers on therapy schemes were a combination of Likert scale, multiple choice, and open comments, the different dosing regimens are displayed in the Supplementary Appendix. Only significant differences are described, otherwise no clear preference for the proposed dosing regimens were seen.
The hypothetical patient with LN outlined in the case vignette, presented with proteinuria 500 mg/m2 and protein-creatinine ratio 0.8 g/g creatinine (90 mg/mmol), erythrocyte cylinder Erys: 10/high power field, eGFR: 110 ml/min per 1.73 m2 and blood pressure at the 75th percentile.
For induction therapy for the SLE patient with LN class III, as outlined in the case vignette, 54% (n = 22) of respondents opted for the combination of intravenous and oral corticosteroid therapy (Table 4), and similar numbers suggest mainly intravenous (n = 10) or mainly oral (n = 9) therapy.
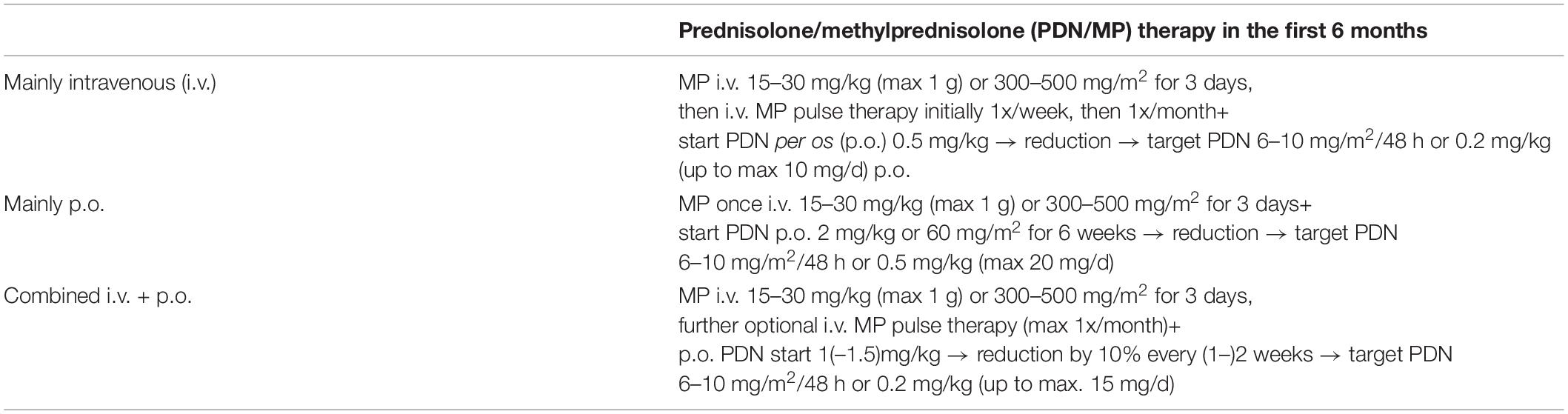
Table 4. Suggested corticosteroid induction therapies for proliferative lupus nephritis class III or IV (adapted from Refs. 17, 63).
For non-steroidal immunosuppressive therapy (NSI), 74% respondents (n = 31) suggest initiation of therapy with mycophenolate mofetil (MMF) at a dosage of 1000–1200 mg/m2 per day, with either a maximum of 3 g (n = 15) or 2 g per day (n = 16). The lower MMF dosage was more frequently proposed by pediatric rheumatologists compared to nephrologists (50 vs. 27%). Other suggested additional immunosuppressants (multiple answers possible, see Supplementary Appendix for dosing regimens) were cyclophosphamide (CP) [n = 7 (17%), with no clear preference for the preferred dosage], azathioprine (AZA), and rituximab (RTX) (n = 3 each). Another 3 respondents indicated that they would not use any other immunosuppression in addition to corticosteroid therapy. In the open-ended comments, hydroxychloroquine (HCQ) was mentioned as an immunomodulatory. This concomitant drug for SLE was not part of the selection, as it is not specifically for the treatment of LN. Primary therapy with cyclosporin A (CsA) was not suggested by any respondent.
For maintenance therapy after achieving disease inactivity and after at least 6 months, 39% (n = 16) of respondents opted to discontinue corticosteroid therapy upon complete remission of the nephritis (based on normalization of proteinuria and eGFR) and 61% (n = 25) decided to continue corticosteroid therapy for at least one more year. There was no clear consensus for PDN dosing in maintenance therapy, with half of the subgroup opting for 5–7.5 mg per day (or 0.15–0.2 mg/kg per day). BSA adjusted corticosteroid dosing was preferred by pediatric nephrologists, whereas rheumatologists preferred dosing according to body weight. For further immunosuppression in the context of maintenance therapy, most respondents (n = 24, 57%) suggested MMF (with a dosage of 1000–1200 mg/kg per day, max. 2 g per day). 8 respondents (20%) would prefer therapy with AZA, 3 (8%) with RTX (with no clear preference for the proposed dosing regimens), and 2 (5%) with CsA.
In case of non-response to induction therapy in LN class III, 5% of respondents (n = 2) suggest continuing the basic medication and only increase PDN p.o. or MP i.v. dose. By contrast, the remaining 95% of respondents (n = 39) would add an immunosuppressive drug, depending on the previous therapy, in addition to corticosteroids. In general (multiple answers possible), 16 respondents (32%) suggested CP, another 16 respondents (32%) suggested MMF (see Supplementary Appendix for suggested dosage regimens, no clear preference emerged among respondents), 11 (22%) suggested RTX, and 7 (14%) CsA. Two respondents proposed plasmapheresis and one immunoadsorption. In the open comments, therapy with ofatumumab (alone or in combination with MMF) was suggested twice.
Therapy for Systemic Lupus Erythematosus With Proliferative Lupus Nephritis Class IV
The hypothetical patient with LN outlined in the case vignette presented with prognostically unfavorable risk factors: histology with LN WHO class IV and 50% crescent formation, proteinuria 1.5 g/m2 per day and urinary protein-creatinine ratio 2.1 g/g creatinine (237 mg/mmol), erythrocyte cylinder 10/high power field, eGFR 72 ml/min per 1.73 m2, blood pressure 97th percentile.
For induction therapy, 67% of respondents (n = 28) would opt for a combined i.v. and p.o. corticosteroid therapy and 33% (n = 14) for oral therapy only. For additional immunosuppression (multiple answers possible), a similar number of respondents suggested the use of CP (n = 23, 40%), including 3 in combination with other immunosuppressants and MMF (n = 24, 41%). Other immunosuppressants or therapies suggested were RTX (n = 8, 14%), CsA (n = 1, 2%), MTX (n = 1, 2%), and plasmapheresis (n = 1, 2%).
For maintenance therapy after achieving disease inactivity and after at least 6 months, 82% (n = 31) proposed continuation of corticosteroid therapy for at least one more year. Unlike in LN class III, most respondents (n = 16, 42%) suggested a dose of 5–7.5 mg per day (or 0.15–0.2 mg/kg/d), 18% (n = 7) of respondents opted to discontinue corticosteroid therapy following complete clinical remission of nephritis. Furthermore, most respondents suggest MMF (n = 34, 69%) for maintenance therapy (multiple answers possible) and others suggest RTX (n = 6, 12%), AZA (n = 6, 12%), CsA (n = 3, 6%), and CP (n = 1, 2%).
In case of non-response to induction therapy, most respondents (n = 37, 97%) opt for an extension of the basic therapy beyond the increase of the corticosteroid dose, depending on previous therapy. This most often included (multiple answers possible) RTX (n = 21), followed by CP (n = 17), MMF (n = 11), CsA (n = 6), AZA (n = 3), plasmapheresis (n = 6), and immunoadsorption (n = 3). In the open comments, therapy with ofatumumab (alone or in combination with MMF) was indicated twice, as well as therapy with intravenous immunoglobulin (IVIG) (n = 1) and tacrolimus (n = 1) and combinations of immunosuppressants, e.g., MPN + RTX + MMF + CsA or RTX + MMF.
Definition of Response to Therapy in Lupus Nephritis
Parameters most frequently considered relevant for assessing a satisfactory response to LN therapy were either the urinary protein-creatinine ratio in a spot urine, or 24 h protein excretion and normalization of eGFR (>90 ml/min per 1.73 m2). However, normalization of urine sediment and normalization of serum complement C3 were also considered important decision tools (see Table 5).
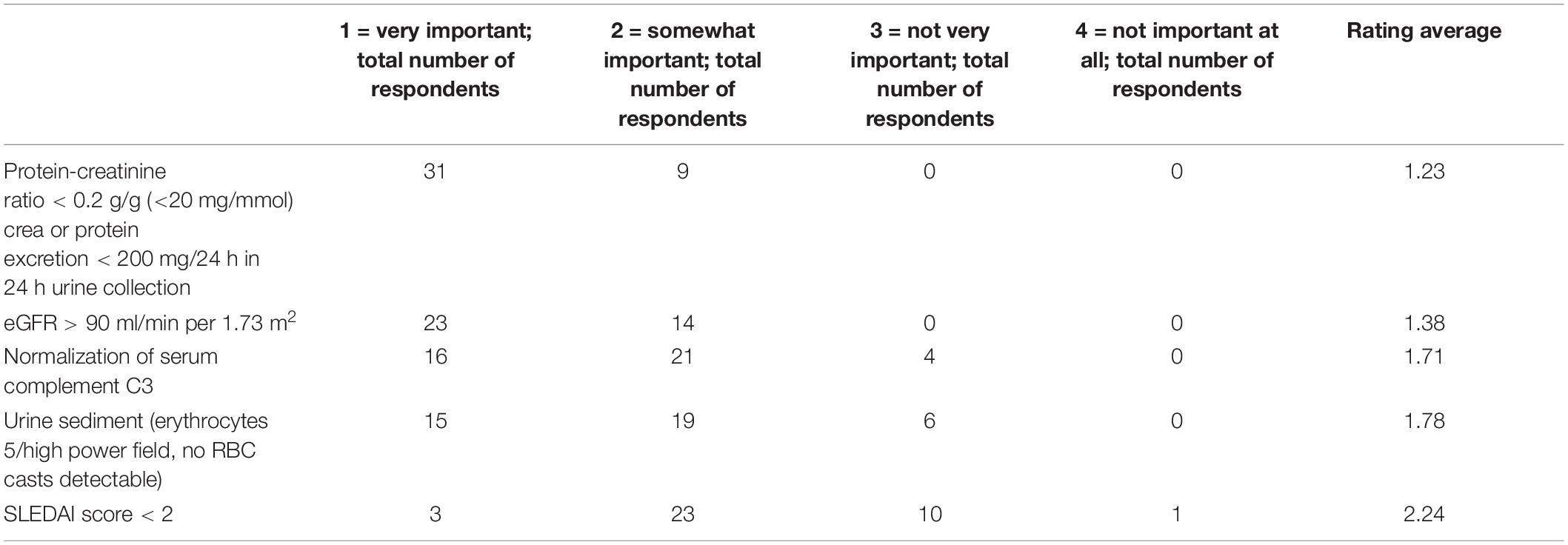
Table 5. Suggested criteria in assessing remission in lupus nephritis (answers by Likert scale: 1 = very important, 2 = somewhat important, 3 = not very important, 4 = not important at all; with rating average of respondents).
As shown in Table 5, remission was defined by the following criteria: protein-creatinine ratio <0.2 g/g creatinine (<20 mg/mmol), eGFR > 90 ml/min per 1.73 m2, and SLEDAI score < 2. Time acceptable to achieve remission was selected by participants.
In case of LN class III, 71% (n = 29) of participants considered an interval of 8–12 weeks until remission, following induction therapy, as acceptable. Seven% of respondents considered an interval of 24 weeks as acceptable, while 5% would expect a therapeutic response after only 2 weeks, or 17% after 4 weeks, following induction therapy.
In cases of LN class IV, 49% (n = 20) of respondents considered a period of 8–12 weeks until reaching a therapeutic response (see Table 5) to be acceptable, whereas 5% would require this after only 2 weeks, or 34% after 4 weeks, following induction therapy, and 10% stated the acceptable interval until response to be 24 weeks and 2% even 52 weeks.
In case of a satisfactory treatment response, most respondents (64%, n = 27) suggest continuing immunosuppressive therapy for at least 3 years, whereas 10% (n = 4) suggest stopping treatment after 1 year and 26% (n = 11) suggest continuing for more than 3 years. Pediatric nephrologists proposed longer treatment durations.
Table 6 shows different scenarios for repeat kidney biopsies. Respondents saw different indications, but most would rather perform a repeat kidney biopsy in the event of a suspected recurrence of nephritis. Other reasons included persistence of proteinuria for over one year on maintenance therapy, partial response after 6–12 months, or after 3–4 months in case of non-response at the end of induction therapy.
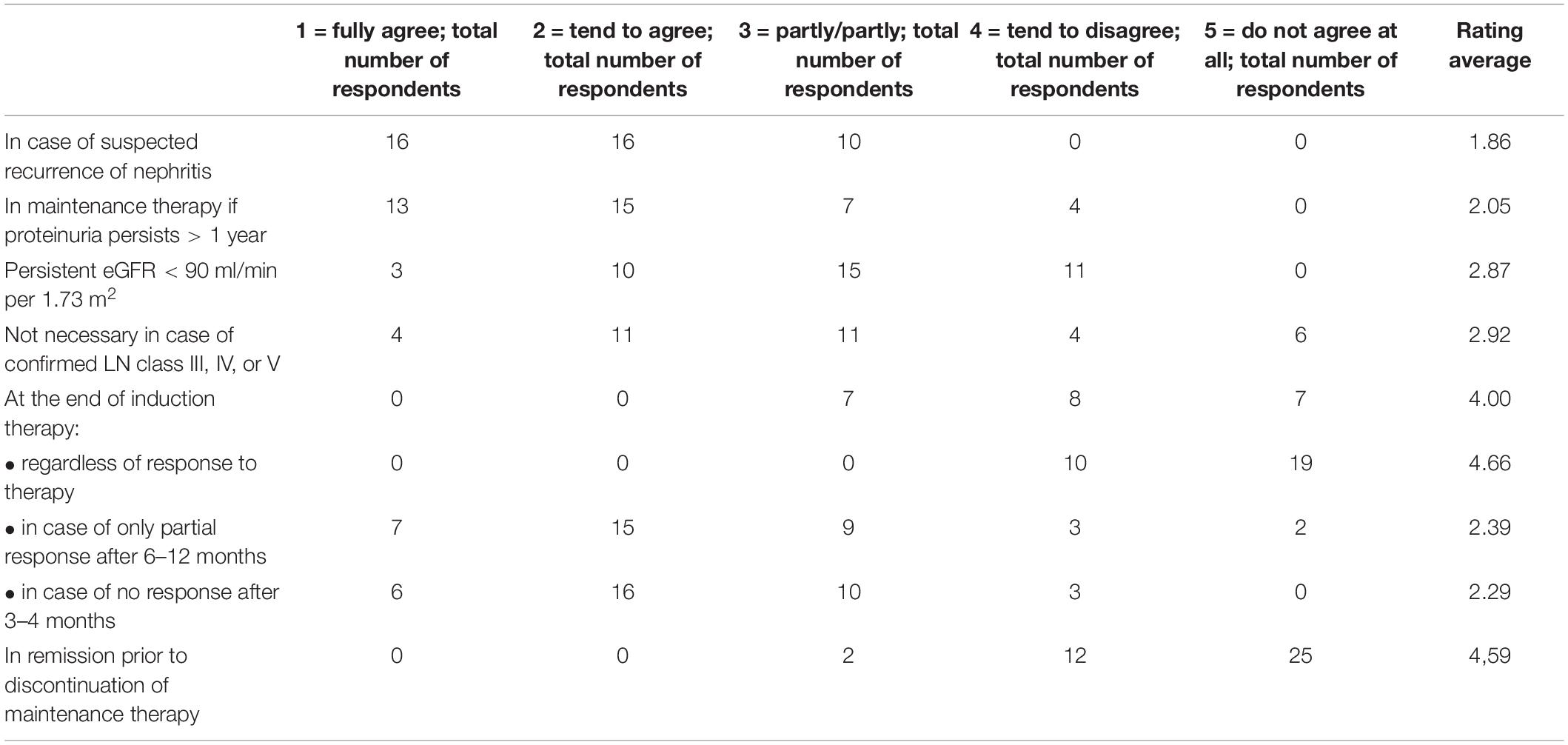
Table 6. Indications for repeat kidney biopsy during follow-up of lupus nephritis (answers by Likert scale: 1 = fully agree, 2 = tend to agree, 3 = partly/partly, 4 = tend to disagree, 5 = do not agree; with rating average of respondents).
Concomitant Therapy and Preventive Measures for Lupus Nephritis
There was general agreement that patients should receive HCQ as a concomitant therapy for LN (Table 7). Other important measures included therapy with an angiotensin-converting enzyme (ACE) inhibitor or angiotensin II (ATII) receptor antagonist in cases of arterial hypertension and/or proteinuria, followed by gonadotropin releasing hormone (GnRH) analogs or fertility preservation, prior to therapy with CP, prescription of progestogen (especially in antiphospholipid syndrome), vitamin D substitution and the implementation of vaccinations and infection prophylaxes.
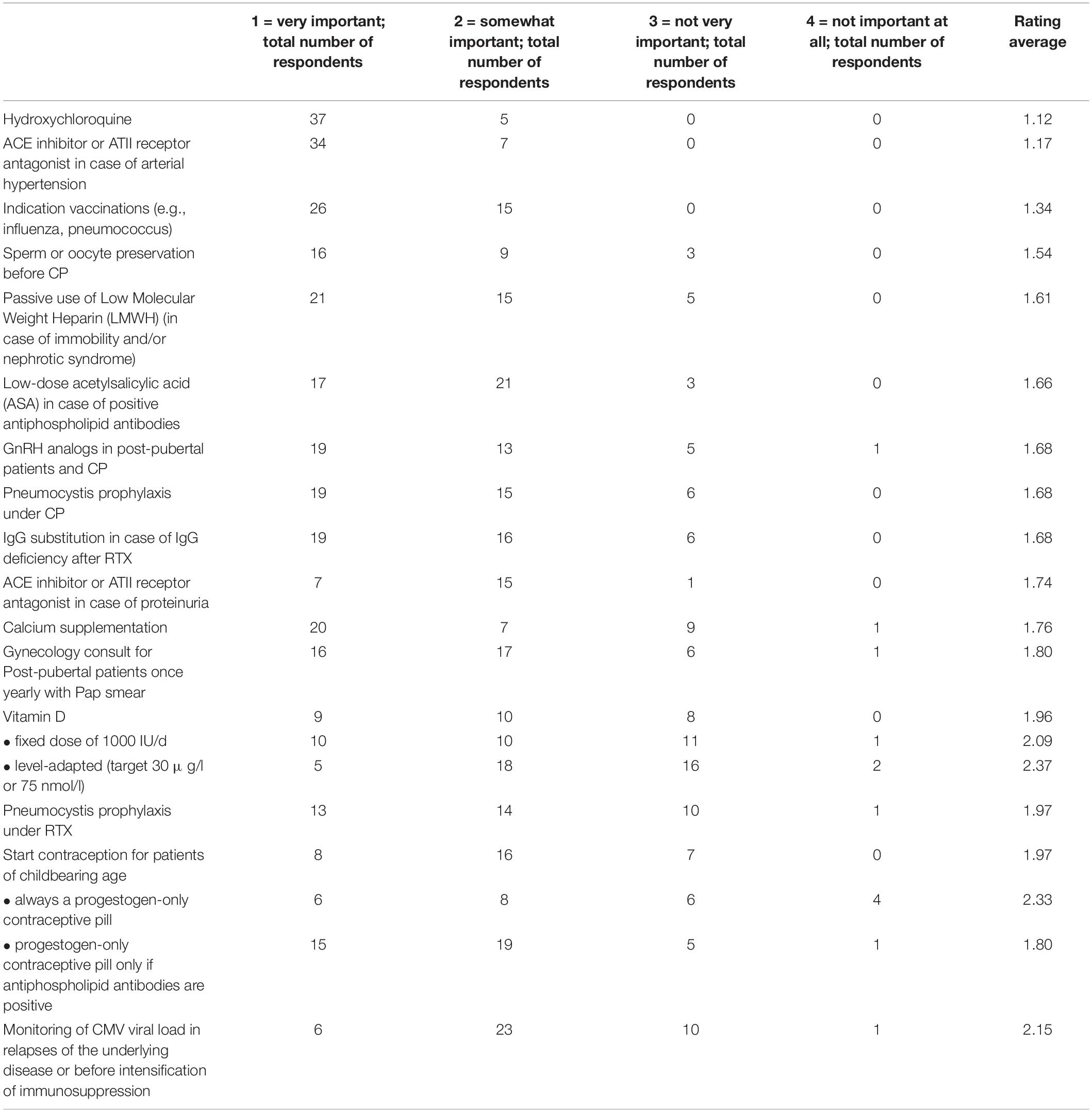
Table 7. Useful concomitant therapies or preventive measures in patients with lupus nephritis (answers by Likert scale: 1 = very important, 2 = somewhat important, 3 = not very important, 4 = not important at all; with rating average of respondents).
Discussion
This study provides new insights into treatment practices of pediatric subspecialists caring for patients with proliferative LN class III and IV in Germany and Austria. As early diagnosis and prompt treatment of LN can improve long-term renal survival (19), the two working groups (PRO-KIND SLE working group and the GPN SLE working group) have the following common goal: to develop consensus protocols for clinical practice with clearly defined treatment goals including timelines for achieving these goals.
The principle of T2T has been successfully introduced for several rheumatic diseases including juvenile idiopathic arthritis, recently published (10–15). Identifying appropriate therapeutic targets and translation of these targets into clinical practice will lead to improved care for patients and, subsequently, to a better outcome (20). International and German consensus treatment recommendations for LN in children are available (16, 17, 21, 22), but lack a T2T approach.
Overall, the answers to the survey questions reflect a large heterogeneity in the management of juvenile proliferative LN in Germany and Austria, supporting the need to design T2T strategies which should be consented by the relevant subspecialties caring for SLE patients.
Rheumatologists participating in this survey are more likely to involve a nephrologist in the diagnosis and treatment planning of an SLE patient with suspected LN than vice versa, while international recommendations emphasize the inclusion of both disciplines (16, 21). That only 55% consult a rheumatologist might also be partly due to the fact that the majority of respondents are themselves pediatric rheumatologists. Since isolated lupus nephritis is a very rare condition (23–25) and SLE is a multisystem disease, interdisciplinary collaboration is important and worthy of support, to which the joint establishment of a treatment protocol could contribute.
When assessing the extent of LN, protein excretion in 24 h collection urine (>300 mg/m2 per 24 h or ≥0.5 g per 24 h) and protein-creatinine ratio (>0.2 g/g creatinine or >20 mg/mmol) in spot urine collection were evaluated as key parameters. Recently, Smith et al. did not find significance of proteinuria in differentiating SLE patients with and without development of LN longitudinally (26). However, proteinuria is generally noted in patients with juvenile proliferative LN (7) and remains an important tool for detecting subclinical renal involvement in SLE (16). In our survey, serum creatinine and eGFR were also assessed as important parameters in evaluating the extent of LN. It is worth mentioning, that these two parameters failed to discriminate between patients with and without LN in the United Kingdom JSLE Cohort Study (26).
The definition of therapeutic targets is obviously a core element of the T2T approach. To date, the literature does not offer a uniform definition of complete remission in LN. The Joint European League Against Rheumatism and European Renal Association-European Dialysis and Transplant Association (EULAR/ERA-EDTA) recommendations define proteinuria as <0.5 g/24 h and normal or near normal (within 10% of normal eGFR if previously abnormal) eGFR as complete response (CR), and this definition has also been adopted by the SHARE Initiative (16, 27). In our survey, respondents also rated the increase of eGFR to >90 ml/min/m2 as a very important target for remission, as well as protein excretion in 24 h urine collection < 200 mg/24 h, which is somewhat stricter than the above recommendations. Furthermore, normalization of serum complement C3 is also an important decision tool to define CR to the respondents, while it has been shown to have modest specificity for active LN (28). On the other hand, in a recent British cohort, C3 levels at baseline were a significant predictor for subsequent LN development (26). In summary, targets in the management of LN need to be defined and should be the subject of consensus findings.
When renal involvement is suspected in patients with SLE, kidney biopsy is the widely accepted gold standard (16, 29). In our survey, respondents stipulated that nephrotic-range or rapidly progressing proteinuria were important indicators for kidney biopsy, reflecting the consensus in adult SLE (27, 30–32). The fact that respondents of this survey failed to rate ethnicity as an important parameter in the indication for kidney biopsy, is in discordance with the literature: African Americans, East Asians, and Hispanics with SLE are more likely to develop LN than are SLE patients of European descent (33, 34). This result may reflect the historically lower prevalence of these ethnicities in Germany and Austria and the lack of awareness of this risk factor. Many pediatric nephrologists and rheumatologists continue to follow ACR recommendations when deciding on the necessity of a kidney biopsy (17, 35).
For induction therapy of proliferative LN, our survey suggests that the use of corticosteroids is mandatory, with respondents preferring combined intravenous and oral administration. The majority of participants suggested maintaining PDN treatment for at least one year, but consider discontinuation thereafter, in order to avoid long-term side effects (36). However, there was no consensus on optimal dose and duration of PDN treatment in children in order to balance efficacy and side effects. A recent study conducted by the GPN in children with LN class III or IV, showed corticosteroid toxicity in 42% and growth failure in 78% of children in the first year of treatment (7). Therefore, a consensus for optimal corticosteroid dosing is of utmost importance.
Mycophenolate mofetil was clearly preferred over CP for induction therapy, in addition to corticosteroids in patients with LN class III. By contrast, CP (0.5 g/m2/month for 6 months) and MMF were rated equally for induction treatment of LN class IV. This approach is supported by recent registries and cohort studies suggesting the comparability of MMF and CP in induction therapy for proliferative LN in children, although no difference between MMF and CP with respect to treatment-associated side effects was noted with a follow-up of maximum 13 months (7, 37, 38). The use of high-dose intravenous CP (0.5–0.75 g/m2 monthly for 6 months) was recommended to be reserved for adult patients with proliferative LN class III/IV showing unfavorable clinical (nephritic urine sediment and impaired renal function with an eGFR between 25 and 80 ml/min/1.73 m2), or histologic (crescents or necrosis in >25% of glomeruli) prognostic factors (21). Of note, there was no consensus on the MMF dosage regimen to be used during induction treatment with half each of the participants proposing 2 and 3 g, respectively. The latter was more frequently proposed by pediatric nephrologists and is in line with recent guidelines for treatment of proliferative LN in adults (21).
Most physicians considered an interval of 12 weeks as acceptable to assess treatment response, which is in agreement with a survey of North American pediatric nephrologists and rheumatologists (39). This timeline may be rather optimistic, as recent registry data showed that 25 and 17% of German patients with juvenile LN class III/IV receiving induction treatment with corticosteroids in combination with either MMF of CP showed persistent proteinuria after 3 and 6 months, respectively (7). Again, consensus on timelines for treatment targets need to be better defined. This is important, as it will guide physicians toward switching to second-line treatments.
In case of non-response to induction therapy, most respondents opt for a switch of medication beyond the increase of the corticosteroid dose, depending on previous therapy. This most often included RTX (preferred by 8% among nephrologists vs. 25% among rheumatologists) (39), followed by CP, MMF, and CsA, whereas other measures such as plasmapheresis and immunoadsorption were rarely proposed. This reflects what is currently recommended for adult patients with proliferative LN in case of treatment failure or partial response only, i.e., switching to MMF, a calcineurin inhibitor, intravenous CP or RTX (21, 40–49).
Mycophenolate mofetil was most often recommended for maintenance therapy in LN class III/IV, in conjunction with oral corticosteroids, whereas AZA or CsA were rarely suggested, which is in line with recommendations for adults with proliferative LN (21, 49).
As for concomitant therapies and preventive measures in childhood LN, results of our survey echo the published data, that pediatric SLE patients should all be treated with HCQ (50). As there is evidence in adult SLE patients that ACE inhibitors or ATII receptor antagonist have a protective effect on the kidneys in case of proteinuria (51, 52), its use is recommended in children with LN and proteinuria (16), a view widely shared by respondents of this survey. In addition, respondents of this survey confirm the importance of using inhibitors of the renin-angiotensin system in arterial hypertension, as documented in international recommendations (53).
The question of fertility preservation in therapy with CP is particularly relevant in adolescent patients. Low-dose intravenous CP does not seem to impact ovarian reserve as measured by anti-Mullerian hormone (54) and the SHARE initiative did not include recommendations for fertility preservation (16). Still, the occurrence of premature ovarian failure (POF) and the risk of permanent sterility in young men the with CP exposure is a rare but serious event (55, 56). In addition to the CP dose limitation that appears to minimize the risk of fertility reduction (57), the combined use of GnRH analogs with CP therapy was shown to be associated with a significant reduction of POF among premenopausal women with SLE, suggesting that the addition of GnRH analog can be a strategy to prevent POF among premenopausal women (58). In addition to endorsing this measure, participants of the survey also consider sperm or oocyte preservation before CP to be useful which, of course, must be discussed individually with each patient (59).
It was shown that low-dose ASA may be beneficial in the primary prophylaxis of cardiovascular (CV) events in SLE patients (60, 61). Considering the general increased risk for a CV event in SLE patients (62) and especially with positive antiphospholipid antibodies, a low-dose acetylsalicylic acid (ASA) therapy in case of positive antiphospholipid antibodies can be considered useful, as suggested by our respondents and also in the literature (50).
The limitations of our study are low participation/response rates (which is not unusual for an online survey distributed via mail) and which may be related to the treatment of LN being primarily in highly specialized centers. However, LN in children and adolescents is a rare condition. Therefore, the number of rheumatologists and nephrologists treating children with LN is also low and likely only those felt consequently addressed to answer the survey. In addition, there is a possible selection bias in only addressing members of the mailing lists of GKJR and GPN. We realize that the definitions of treatment response and failure need to be more clearly delineated. Finally, the role of adherence and therapeutic drug monitoring to optimize treatment with MMF, and the use of “multitarget therapy” (i.e., MMF in combination with a calcineurin inhibitor) for induction of LN were not included in this survey, as these measures have only recently gained attention. The same accounts for new therapeutic options, such as belimumab, which has been approved as an add-on therapy for adult SLE patients with LN in Germany since 2021. In this 2017 survey, belimumab was not yet considered as a treatment option, but which may gain importance in childhood LN therapy.
Several additional aspects should be discussed when treating children and adolescents with LN, such as treatment adherence (possibly promoting intravenous drug administration), the issue of growth (corticosteroid dose limitation), fertility, necessitating CP dose limitation, as well as the psychosocial aspects, such as schooling and socialization with peers. In a study conducted by the GPN in children with LN class III or IV, 80% of patients had drug-related complications in the first year of treatment, including glucocorticoid toxicity in 42% of children and growth retardation in 78% (7).
In conclusion, our survey reveals that the majority of German and Austrian pediatric rheumatologists and nephrologists would use corticosteroids, most often in combination with either MMF or CP for induction treatment of juvenile proliferative LN. Minimization of steroid-exposure remains a major challenge in these children and adolescents, asking for well-designed clinical trials to define the optimal dosage and duration of corticosteroid treatment. The considerable heterogeneity of responses highlights the need for a treat-to-target protocol (T2T) between pediatric rheumatologists and nephrologists. This goal is to be achieved, among other measures, through interdisciplinary cooperation in consensus conferences followed by either controlled or register studies, in which the value of the T2T protocols is tested.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
CS, FS, CMH, CH, and KT designed the survey. KM, JB, UN, AH, TK, NW, BT, LW, and DH revised the survey design. CS, KT, and KV were involved in interpretation of the data and analyzed the data. KV drafted the manuscript. KT, CMH, BT, FS, and DH substantively revised the manuscript. All authors critically revised the manuscript and approved the final draft.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would especially like to thank all respondents of the survey for their participation.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.851998/full#supplementary-material
Abbreviations
ACE, angiotensin-converting enzyme; ACR, American College of Rheumatology; ASA, acetylsalicylic acid; ATII, angiotensin II; AZA, azathioprine; BILAG, British Isles Lupus Assessment Group index; BSA, Body Surface Area; CARRA, Childhood Arthritis and Rheumatology Research Alliance; C-HAQ, Childhood Health Assessment Questionnaire; CP, cyclophosphamide; CR, complete response; CsA, cyclosporin A; CTP, consensus treatment plan; CV, cardiovascular; ECLAM, European Consensus Lupus Activity Measurement; eGFR, estimated glomerular filtration rate; ERA-EDTA, European Renal Association-European Dialysis and Transplant Association; EULAR, Joint European League Against Rheumatism; GKJR, Society for Pediatric and Adolescent Rheumatology; GnRH, gonadotropin releasing hormone; GPN, German Society for Pediatric Nephrology; HCQ, hydroxychloroquine; IVIG, intravenous immunoglobulin; LMWH, low molecular weight heparin; LN, lupus nephritis; MMF, mycophenolate mofetil; MP, methylprednisolone; NSI, non-steroidal immunosuppression; PDN, prednisolone; POF, premature ovarian failure; PRO-KIND, Projekte zur Klassifikation, Überwachung und Therapie in der Kinderrheumatologie/Projects on classification, monitoring and therapy in pediatric rheumatology; RBC casts, Red Blood Cell casts; RTX, rituximab; SHARE, Single Hub and Access point for pediatric Rheumatology in Europe; SLE, systemic lupus erythematosus; SLEDAI-2K, Systemic Lupus Erythematosus Disease Activity Index 2000; SMILEY, Simple Measure of Impact of Lupus Erythematosus in Youngsters; T2T, treat-to-target; TAC, tacrolimus.
References
1. Anders HJ, Saxena R, Zhao MH, Parodis I, Salmon JE, Mohan C. Lupus nephritis. Nat Rev Dis Primers. (2020) 6:7.
2. Smith EMD, Lythgoe H, Midgley A, Beresford MW, Hedrich CM. Juvenile-onset systemic lupus erythematosus: update on clinical presentation, pathophysiology and treatment options. Clin Immunol. (2019) 209:108274. doi: 10.1016/j.clim.2019.108274
3. Bader-Meunier B, Armengaud JB, Haddad E, Salomon R, Deschênes G, Koné-Paut I, et al. Initial presentation of childhood-onset systemic lupus erythematosus: a French multicenter study. J Pediatr. (2005) 146:648–53. doi: 10.1016/j.jpeds.2004.12.045
4. Font J, Cervera R, Espinosa G, Pallarés L, Ramos-Casals M, Jiménez S, et al. Systemic lupus erythematosus (SLE) in childhood: analysis of clinical and immunological findings in 34 patients and comparison with SLE characteristics in adults. Ann Rheum Dis. (1998) 57:456–9. doi: 10.1136/ard.57.8.456
5. Ramírez Gómez LA, Uribe Uribe O, Osio Uribe O, Grisales Romero H, Cardiel MH, Wojdyla D, et al. Childhood systemic lupus erythematosus in Latin America. The GLADEL experience in 230 children. Lupus. (2008) 17:596–604. doi: 10.1177/0961203307088006
6. Watson L, Leone V, Pilkington C, Tullus K, Rangaraj S, McDonagh JE, et al. Disease activity, severity, and damage in the UK juvenile-onset systemic lupus erythematosus cohort. Arthritis Rheum. (2012) 64:2356–65. doi: 10.1002/art.34410
7. Suhlrie A, Hennies I, Gellermann J, Büscher A, Hoyer P, Waldegger S, et al. Twelve-month outcome in juvenile proliferative lupus nephritis: results of the German registry study. Pediatr Nephrol. (2020) 35:1235–46. doi: 10.1007/s00467-020-04501-x
8. Ravelli A, Consolaro A, Horneff G, Laxer RM, Lovell DJ, Wulffraat NM, et al. Treating juvenile idiopathic arthritis to target: recommendations of an international task force. Ann Rheum Dis. (2018) 77:819–28. doi: 10.1136/annrheumdis-2018-213030
9. Horneff G. Protokolle zur klassifikation, überwachung und therapie in der kinderrheumatologie (PRO-KIND). Arthritis Rheum. (2021) 41:276–85. doi: 10.1055/a-1516-0459
10. Hansmann S, Lainka E, Horneff G, Holzinger D, Rieber N, Jansson AF, et al. Consensus protocols for the diagnosis and management of the hereditary autoinflammatory syndromes CAPS, TRAPS and MKD/HIDS: a German PRO-KIND initiative. Pediatr Rheumatol Online J. (2020) 18:17. doi: 10.1186/s12969-020-0409-3
11. Horneff G, Klein A, Ganser G, Sailer-Höck M, Günther A, Foeldvari I, et al. Protocols on classification, monitoring and therapy in children’s rheumatology (PRO-KIND): results of the working group polyarticular juvenile idiopathic arthritis. Pediatr Rheumatol Online J. (2017) 15:78. doi: 10.1186/s12969-017-0206-9
12. Hinze CH, Holzinger D, Lainka E, Haas JP, Speth F, Kallinich T, et al. Practice and consensus-based strategies in diagnosing and managing systemic juvenile idiopathic arthritis in Germany. Pediatr Rheumatol Online J. (2018) 16:7. doi: 10.1186/s12969-018-0224-2
13. Hospach A, Trauzeddel R, Windschall D, Kekow M, Hardt S, Küster R-M, et al. Protokolle zur klassifikation, überwachung und therapie in der kinderrheumatologie (PRO-KIND): enthesitis-assoziierte arthritis. ergebnisse der arbeitsgruppe enthesitis-assoziierte arthritis in der GKJR-kommission PRO-KIND. Arthritis Rheum. (2018) 38:132–40. doi: 10.1055/s-0038-1649293
14. Schwarz T, Oommen PT, Windschall D, Weissbarth-Riedel E, Trauzeddel R, Grote V, et al. Protokolle zur klassifikation, überwachung und therapie in der kinderrheumatologie (PRO-KIND): chronisch nicht-bakterielle osteomyelitis (CNO). Arthritis Rheum. (2018) 38:282–8. doi: 10.1055/s-0038-1669796
15. Hinze CH, Oommen PT, Dressler F, Urban A, Weller-Heinemann F, Speth F, et al. Development of practice and consensus-based strategies including a treat-to-target approach for the management of moderate and severe juvenile dermatomyositis in Germany and Austria. Pediatr Rheumatol Online J. (2018) 16:40. doi: 10.1186/s12969-018-0257-6
16. Groot N, de Graeff N, Marks SD, Brogan P, Avcin T, Bader-Meunier B, et al. European evidence-based recommendations for the diagnosis and treatment of childhood-onset lupus nephritis: the SHARE initiative. Ann Rheum Dis. (2017) 76:1965–73. doi: 10.1136/annrheumdis-2017-211898
17. Mina R, von Scheven E, Ardoin SP, Eberhard BA, Punaro M, Ilowite N, et al. Consensus treatment plans for induction therapy of newly diagnosed proliferative lupus nephritis in juvenile systemic lupus erythematosus. Arthritis Care Res. (2012) 64:375–83. doi: 10.1002/acr.21558
18. Hochberg MC. Updating the American college of rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. (1997) 40:1725. doi: 10.1002/art.1780400928
19. Esdaile JM, Joseph L, MacKenzie T, Kashgarian M, Hayslett JP. The benefit of early treatment with immunosuppressive agents in lupus nephritis. J Rheumatol. (1994) 21:2046–51.
20. van Vollenhoven RF, Mosca M, Bertsias G, Isenberg D, Kuhn A, Lerstrøm K, et al. Treat-to-target in systemic lupus erythematosus: recommendations from an international task force. Ann Rheum Dis. (2014) 73:958–67. doi: 10.1136/annrheumdis-2013-205139
21. Fanouriakis A, Kostopoulou M, Cheema K, Anders HJ, Aringer M, Bajema I, et al. 2019 Update of the joint European league against rheumatism and European renal association-European dialysis and transplant association (EULAR/ERA-EDTA) recommendations for the management of lupus nephritis. Ann Rheum Dis. (2020) 79:713–23. doi: 10.1136/annrheumdis-2020-216924
22. Boneparth A, Radhakrishna SM, Greenbaum LA, Yen E, Okamura DM, Cooper JC, et al. Approach to membranous lupus nephritis: a survey of pediatric nephrologists and pediatric rheumatologists. J Rheumatol. (2017) 44:1619–23. doi: 10.3899/jrheum.170502
23. Mubarak M. Hidden face of lupus nephritis exposed: isolated tubulointerstitial lupus nephritis. J Nephropathol. (2013) 2:71–2. doi: 10.5812/nephropathol.8998
24. Mori Y, Kishimoto N, Yamahara H, Kijima Y, Nose A, Uchiyama-Tanaka Y, et al. Predominant tubulointerstitial nephritis in a patient with systemic lupus nephritis. Clin Exp Nephrol. (2005) 9:79–84. doi: 10.1007/s10157-004-0338-3
25. Gur H, Kopolovic Y, Gross DJ. Chronic predominant interstitial nephritis in a patient with systemic lupus erythematosus: a follow up of three years and review of the literature. Ann Rheum Dis. (1987) 46:617–23. doi: 10.1136/ard.46.8.617
26. Smith EMD, Yin P, Jorgensen AL, Beresford MW. Clinical predictors of active LN development in children – evidence from the UK JSLE cohort study. Lupus. (2018) 27:2020–8. doi: 10.1177/0961203318801526
27. Bertsias GK, Tektonidou M, Amoura Z, Aringer M, Bajema I, Berden JH, et al. Joint European league against rheumatism and European renal association-European dialysis and transplant association (EULAR/ERA-EDTA) recommendations for the management of adult and paediatric lupus nephritis. Ann Rheum Dis. (2012) 71:1771–82. doi: 10.1136/annrheumdis-2012-201940
28. Moroni G, Radice A, Giammarresi G, Quaglini S, Gallelli B, Leoni A, et al. Are laboratory tests useful for monitoring the activity of lupus nephritis? A 6-year prospective study in a cohort of 228 patients with lupus nephritis. Ann Rheum Dis. (2009) 68:234–7. doi: 10.1136/ard.2008.094508
29. Almaani S, Meara A, Rovin BH. Update on lupus nephritis. Clin J Am Soc Nephrol. (2017) 12:825–35.
30. Ruiz Irastorza G, Espinosa G, Frutos MA, Jiménez Alonso J, Praga M, Pallarés L, et al. Diagnosis and treatment of lupus nephritis. Consensus document from the systemic auto-immune disease group (GEAS) of the Spanish society of internal medicine (SEMI) and Spanish society of nephrology (S.E.N.). Nefrologia. (2012) 32:1–35. doi: 10.3265/Nefrologia.pre2011.Dec.11298
31. van Tellingen A, Voskuyl AE, Vervloet MG, Bijl M, de Sévaux RG, Berger SP, et al. Dutch guidelines for diagnosis and therapy of proliferative lupus nephritis. Netherlands J Med. (2012) 70:199–207.
32. Hahn BH, McMahon MA, Wilkinson A, Wallace WD, Daikh DI, Fitzgerald JD, et al. American college of rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Care Res. (2012) 64:797–808. doi: 10.1002/acr.21664
33. Lanata CM, Nititham J, Taylor KE, Chung SA, Torgerson DG, Seldin MF, et al. Genetic contributions to lupus nephritis in a multi-ethnic cohort of systemic lupus erythematous patients. PLoS One. (2018) 13:e0199003. doi: 10.1371/journal.pone.0199003
34. Feldman CH, Hiraki LT, Liu J, Fischer MA, Solomon DH, Alarcón GS, et al. Epidemiology and sociodemographics of systemic lupus erythematosus and lupus nephritis among US adults with Medicaid coverage, 2000-2004. Arthritis Rheum. (2013) 65:753–63. doi: 10.1002/art.37795
35. Wenderfer SE, Lane JC, Shatat IF, von Scheven E, Ruth NM. Practice patterns and approach to kidney biopsy in lupus: a collaboration of the midwest pediatric nephrology consortium and the childhood arthritis and rheumatology research alliance. Pediatr Rheumatol Online J. (2015) 13:26. doi: 10.1186/s12969-015-0024-x
36. Mejía-Vilet JM, Ayoub I. The use of glucocorticoids in lupus nephritis: new pathways for an old drug. Front Med. (2021) 8:622225. doi: 10.3389/fmed.2021.622225
37. Cooper JC, Rouster-Stevens K, Wright TB, Hsu JJ, Klein-Gitelman MS, Ardoin SP, et al. Pilot study comparing the childhood arthritis and rheumatology research alliance consensus treatment plans for induction therapy of juvenile proliferative lupus nephritis. Pediatr Rheumatol Online J. (2018) 16:65. doi: 10.1186/s12969-018-0279-0
38. Smith E, Al-Abadi E, Armon K, Bailey K, Ciurtin C, Davidson J, et al. Outcomes following mycophenolate mofetil versus cyclophosphamide induction treatment for proliferative juvenile-onset lupus nephritis. Lupus. (2019) 28:613–20. doi: 10.1177/0961203319836712
39. Gilbert M, Goilav B, Hsu JJ, Nietert PJ, Meidan E, Chua A, et al. Differences in rituximab use between pediatric rheumatologists and nephrologists for the treatment of refractory lupus nephritis and renal flare in childhood-onset SLE. Pediatr Rheumatol Online J. (2021) 19:137. doi: 10.1186/s12969-021-00627-w
40. Rivera F, Mérida E, Illescas ML, López-Rubio E, Frutos MA, García-Frías P, et al. Mycophenolate in refractory and relapsing lupus nephritis. Am J Nephrol. (2014) 40:105–12.
41. Kasitanon N, Boripatkosol P, Louthrenoo W. Response to combination of mycophenolate mofetil, cyclosporin A and corticosteroid treatment in lupus nephritis patients with persistent proteinuria. Int J Rheum Dis. (2018) 21:200–7. doi: 10.1111/1756-185X.13152
42. Mok CC, To CH, Yu KL, Ho LY. Combined low-dose mycophenolate mofetil and tacrolimus for lupus nephritis with suboptimal response to standard therapy: a 12-month prospective study. Lupus. (2013) 22:1135–41. doi: 10.1177/0961203313502864
43. Sheikholeslami M, Hajialilo M, Rasi Hashemi SS, Malek Mahdavi A, Gojazadeh M, Khabbazi A. Low dose cyclosporine A in the treatment of resistant proliferative lupus nephritis. Modern Rheumatol. (2018) 28:523–9. doi: 10.1080/14397595.2017.1352479
44. Fei Y, Wu Q, Zhang W, Chen H, Hou Y, Xu D, et al. Low-dose tacrolimus in treating lupus nephritis refractory to cyclophosphamide: a prospective cohort study. Clin Exp Rheumatol. (2013) 31:62–8.
45. Alshaiki F, Obaid E, Almuallim A, Taha R, El-Haddad H, Almoallim H. Outcomes of rituximab therapy in refractory lupus: a meta-analysis. Eur J Rheumatol. (2018) 5:118–26. doi: 10.5152/eurjrheum.2018.17096
46. Weidenbusch M, Römmele C, Schröttle A, Anders HJ. Beyond the LUNAR trial. Efficacy of rituximab in refractory lupus nephritis. Nephrol Dial Transplant. (2013) 28:106–11. doi: 10.1093/ndt/gfs285
47. Davies RJ, Sangle SR, Jordan NP, Aslam L, Lewis MJ, Wedgwood R, et al. Rituximab in the treatment of resistant lupus nephritis: therapy failure in rapidly progressive crescentic lupus nephritis. Lupus. (2013) 22:574–82. doi: 10.1177/0961203313483376
48. Jónsdóttir T, Zickert A, Sundelin B, Henriksson EW, van Vollenhoven RF, Gunnarsson I. Long-term follow-up in lupus nephritis patients treated with rituximab–clinical and histopathological response. Rheumatology (Oxford). (2013) 52:847–55. doi: 10.1093/rheumatology/kes348
49. Rovin BH, Adler SG, Barratt J, Bridoux F, Burdge KA, Chan TM, et al. Executive summary of the KDIGO 2021 guideline for the management of glomerular diseases. Kidney Int. (2021) 100:753–79.
50. Groot N, de Graeff N, Avcin T, Bader-Meunier B, Brogan P, Dolezalova P, et al. European evidence-based recommendations for diagnosis and treatment of childhood-onset systemic lupus erythematosus: the SHARE initiative. Ann Rheum Dis. (2017) 76:1788–96. doi: 10.1136/annrheumdis-2016-210960
51. Kanda H, Kubo K, Tateishi S, Sato K, Yonezumi A, Yamamoto K, et al. Antiproteinuric effect of ARB in lupus nephritis patients with persistent proteinuria despite immunosuppressive therapy. Lupus. (2005) 14:288–92. doi: 10.1191/0961203305lu2076oa
52. Tse KC, Li FK, Tang S, Tang CS, Lai KN, Chan TM. Angiotensin inhibition or blockade for the treatment of patients with quiescent lupus nephritis and persistent proteinuria. Lupus. (2005) 14:947–52. doi: 10.1191/0961203305lu2249oa
53. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. (2017) 140:e20171904. doi: 10.1542/peds.2017-1904
54. Tamirou F, Husson SN, Gruson D, Debiève F, Lauwerys BR, Houssiau FA. Brief report: the euro-lupus low-dose intravenous cyclophosphamide regimen does not impact the ovarian reserve, as measured by serum levels of anti-müllerian hormone. Arthritis Rheumatol. (2017) 69:1267–71. doi: 10.1002/art.40079
55. Brunner HI, Bishnoi A, Barron AC, Houk LJ, Ware A, Farhey Y, et al. Disease outcomes and ovarian function of childhood-onset systemic lupus erythematosus. Lupus. (2006) 15:198–206. doi: 10.1191/0961203306lu2291oa
56. Meistrich ML, Wilson G, Brown BW, da Cunha MF, Lipshultz LI. Impact of cyclophosphamide on long-term reduction in sperm count in men treated with combination chemotherapy for ewing and soft tissue sarcomas. Cancer. (1992) 70:2703–12. doi: 10.1002/1097-0142(19921201)70:11<2703::aid-cncr2820701123>3.0.co;2-x
57. Houssiau FA, Vasconcelos C, D’Cruz D, Sebastiani GD, Garrido Ed Ede R, Danieli MG, et al. Immunosuppressive therapy in lupus nephritis: the Euro-lupus nephritis trial, a randomized trial of low-dose versus high-dose intravenous cyclophosphamide. Arthritis Rheum. (2002) 46:2121–31. doi: 10.1002/art.10461
58. Koga T, Umeda M, Endo Y, Ishida M, Fujita Y, Tsuji S, et al. Effect of a gonadotropin-releasing hormone analog for ovarian function preservation after intravenous cyclophosphamide therapy in systemic lupus erythematosus patients: a retrospective inception cohort study. Int J Rheum Dis. (2018) 21:1287–92. doi: 10.1111/1756-185X.13318
59. Gajjar R, Miller SD, Meyers KE, Ginsberg JP. Fertility preservation in patients receiving cyclophosphamide therapy for renal disease. Pediatr Nephrol. (2015) 30:1099–106. doi: 10.1007/s00467-014-2897-1
60. Iudici M, Fasano S, Gabriele Falcone L, Pantano I, Montagna G., La Migliaresi S, et al. Low-dose aspirin as primary prophylaxis for cardiovascular events in systemic lupus erythematosus: a long-term retrospective cohort study. Rheumatology (Oxford). (2016) 55:1623–30. doi: 10.1093/rheumatology/kew231
61. Fasano S, Pierro L, Pantano I, Iudici M, Valentini G. Longterm hydroxychloroquine therapy and low-dose aspirin may have an additive effectiveness in the primary prevention of cardiovascular events in patients with systemic lupus erythematosus. J Rheumatol. (2017) 44:1032–8. doi: 10.3899/jrheum.161351
62. McMahon M, Hahn BH, Skaggs BJ. Systemic lupus erythematosus and cardiovascular disease: prediction and potential for therapeutic intervention. Expert Rev Clin Immunol. (2011) 7:227–41. doi: 10.1586/eci.10.98
Keywords: SLE, nephritis, T2T, mycophenolate mofetil, cyclophosphamide, corticosteroid, kidney biopsy
Citation: Vollbach K, Schuetz C, Hedrich CM, Speth F, Mönkemöller K, Brunner J, Neudorf U, Rietschel C, Hospach A, Kallinich T, Hinze C, Wagner N, Tönshoff B, Weber LT, Latta K, Thumfart J, Bald M, Wiemann D, Zappel H, Tenbrock K and Haffner D (2022) Working Towards a Treat-to-Target Protocol in Juvenile Proliferative Lupus Nephritis – A Survey of Pediatric Rheumatologists and Nephrologists in Germany and Austria. Front. Pediatr. 10:851998. doi: 10.3389/fped.2022.851998
Received: 10 January 2022; Accepted: 07 March 2022;
Published: 22 April 2022.
Edited by:
Deborah Levy, University of Toronto, CanadaReviewed by:
Sibel Balci, Republic of Turkey Ministry of Health Sciences, TurkeyBalahan Makay, Dokuz Eylül University, Turkey
Copyright © 2022 Vollbach, Schuetz, Hedrich, Speth, Mönkemöller, Brunner, Neudorf, Rietschel, Hospach, Kallinich, Hinze, Wagner, Tönshoff, Weber, Latta, Thumfart, Bald, Wiemann, Zappel, Tenbrock and Haffner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Klaus Tenbrock, ktenbrock@ukaachen.de
†These authors have contributed equally to this work
 Kristina Vollbach
Kristina Vollbach Catharina Schuetz
Catharina Schuetz Christian M. Hedrich
Christian M. Hedrich Fabian Speth5
Fabian Speth5  Jürgen Brunner
Jürgen Brunner Tilmann Kallinich
Tilmann Kallinich Norbert Wagner
Norbert Wagner Burkhard Tönshoff
Burkhard Tönshoff Lutz T. Weber
Lutz T. Weber Julia Thumfart
Julia Thumfart Martin Bald
Martin Bald Klaus Tenbrock
Klaus Tenbrock