Parent and Teacher Training Increases Medication Adherence for Primary School Children With Attention-Deficit/Hyperactivity Disorder
- 1Department of Child Health Care, Shanghai Children's Hospital, Shanghai Jiaotong University, Shanghai, China
- 2School Affiliated With Shanghai Caoyang No. 2 High School, Shanghai, China
Objective: Attention-deficit/hyperactivity disorder (ADHD) is a common neurobiological disorder for which effective and safe medication is recommended as first-line treatment. However, many parents and teachers do not believe that ADHD is a disorder or do not accept medication treatment in China. Treatment is often short term or intermittent. Our study aimed to investigate the clinical effect of employing a 4-week, session-based training for both parents and teachers in improving medication adherence for primary school children with ADHD.
Methods: From January 2018 to December 2018, a total of 5,118 primary school children were screened. Among 211 children diagnosed with ADHD, 116 were assigned to the intervention group and 95 to the control group. This study provided systematic training for parents and teachers in the intervention group. The training consisted of education about the disorder and ADHD behavioral intervention for both parents and teachers as well as classroom management techniques for just the teachers. A cluster randomized controlled trial (RCT) was conducted to investigate the effect of this training at 6 months follow-up. The study determined medication adherence using a questionnaire and scoring with a rating scale at baseline and at the 6 month follow-up endpoint. The questionnaire was self-report.
Results: The study population had a relatively low rate of attention deficit hyperactivity disorder (4.1%) compared to the generally accepted prevalence. After the training, more parents and teachers believed that ADHD is a neurobiological disorder and that medication is the first line treatment. At 6 months follow-up, the Medication Adherence Report Scale (MARS) score for the intervention group was 22.8 ± 0.75 and 16.5 ± 1.63 for the control group (t = 5.217, P < 0.01). Based on parents' reports and medical records, 82 children (70.69%) were continuously taking medication for 6 months in the intervention group, while only 35 children (36.84%) were doing so in the control group. In the intervention group, the mean SNAP-IV score was 1.98 ± 0.42 at baseline but 0.99 ± 0.31 at 6-month follow-up. In the control group, the mean SNAP-IV score was 1.89 ± 0.47 at baseline but 1.37 ± 0.42 at 6-months follow-up (F = 2.67, P = 0.009). Factors influencing medication adherence for children with ADHD were parent's beliefs, teacher's beliefs, socioeconomic status, adverse effect, insurance coverage, gender, and trust of the medical system.
Conclusions: Our findings indicate that comprehensive training programs improve the understanding of ADHD and medication adherence for both children's parents and teachers, providing a promising approach for improving clinical efficacy for children with ADHD.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a common neurobiological disorder, characterized by symptoms of overactivity, impulsivity, and inattention (1). Approximately 7% of children are estimated to be affected by ADHD worldwide (2). Effective and safe medication is recommended as the first-line treatment for ADHD (3). Primary medications in China include methylphenidate (MPH) and atomoxetine (ATX). Stimulants such as MPH increase dopamine in the brain generally, while ATX leads to a selective increase in norepinephrine and an indirect increase of dopamine in the frontal cortex (4). Medication adherence is important because untreated ADHD can result in serious consequences with lifelong effects, such as school difficulties, fewer friends, arrests, unwanted pregnancy, and alcohol or drug abuse (5). It has been reported that medication treatment for children with ADHD can reduce the risk of criminality, comorbid psychiatric disorders, and substance abuse in adolescence and adulthood (6, 7). For example, high adherence to ADHD medication has been reported to result in higher academic achievement among children with ADHD (8, 9).
In recent years, with the expectation and hope that early treatment will diminish poor mental health and psychosocial outcomes in adolescence and adulthood, ADHD interventions have largely targeted children of primary school age (10). In China, the prevalence of ADHD among children and adolescents is 6.26% (11) or 23 million affected individuals. At present, the consultation rate of ADHD patients in China is low, at only 10%, and only about one third of families receive medication treatment (11). So far, the compliance of children with ADHD in China is relatively poor. A considerable number of children with ADHD have missed the ideal timing for treatment, leading to the occurrence or a significant increase of comorbidities before visiting doctors (11). In addition, increased age leads to increased ADHD-related comorbidities or secondary learning difficulties, along with oppositional defiant disorder. As a result, therapy for ADHD becomes more challenging.
However, many parents and teachers do not accept or continue medication treatment in China. They do not believe that ADHD is a neurobiological disorder or that medication is safe (11). For children, healthcare decisions are usually made by their parents, and beliefs and attitudes may differ widely. However, for other families, medication treatment is unacceptable. They prefer implementing behavioral strategies and other non-medication strategies (11). Choices about using medication are complex, with more recent work focusing on beliefs and attitudes that shape patient preferences (12, 13). In addition, effectiveness and adverse effects, two-parent families, higher socioeconomic status, insurance coverage, Caucasian racial background, and combined subtype are all important factors of increased adherence (14).
In addition to parental decisions, teachers are an important part of children's school environments. Whether children's ADHD can be detected earlier depends to some extent on teacher beliefs about ADHD. In the clinical evaluation stage, doctors need to refer to teachers' opinions. In the treatment phase, medication dosing should also be adjusted according to teachers' feedback on school performances (15). Training for parents and teachers of children with ADHD is necessary and urgent in China. However, to our knowledge, few studies exist that examine the effect of parent/teacher training for children with ADHD in China. Our study was undertaken within primary schools to systematically implement parent and teacher training targeted at increasing medication adherence for children with ADHD. A cluster randomized controlled trial (RCT) was conducted to investigate the effect of training for parents and teachers of children with ADHD at 6 months follow-up.
Materials and Methods
This study was a cluster randomized controlled trial (RCT) to investigate the effect of parent and teacher training at 6 months follow-up. It consisted of three parts: ADHD screening and diagnosis, parent and teacher training, and evaluation of the effect of the training.
Study Design and Population
A RCT was carried out at 10 primary schools (children aged 6–11 years) located in Putuo District, Shanghai, China. First, an invitation and information letter was sent to each school's in-house health care professional (iHCP) and the headmaster, informing them about the study. Hospital pediatricians conducted a meeting for both teachers and parents to introduce the purpose of this project and the type of intervention. Parents who wanted to participate were asked to complete and return the informed consent letter within 3 days.
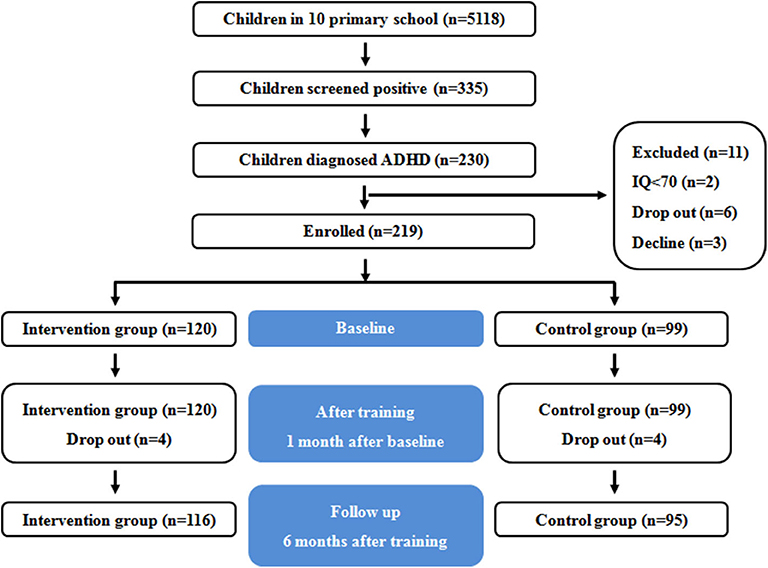
Students were enrolled in this study between January 2018 and June 2018. Conner's Parent Symptom Questionnaire (PSQ) and Conner's Teacher Rating Scale (TRS) were used for ADHD screening. Children whose results on both scales were positive received a call or a notification to have a pediatric examination in Shanghai Children's Hospital. Within 1 month of issuing the screening questionnaire, pediatricians identified 6- to 11-year-old children diagnosed with ADHD who also met inclusion or exclusion criteria. Hospital pediatricians sent a program invitation and informed consent form to the parents of these children. There were 116 children diagnosed with ADHD in the intervention group and 95 in the control group. A flow diagram of participants is shown in Figure 1.
Inclusion and Exclusion Criteria
Children were diagnosed with ADHD according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) (16), IQ ≥70 on the Wechsler Intelligence Scale (WISC), aged 6- to 11-years old, and with no prior ADHD medication use. Additional inclusion criteria were that parents or primary caregivers accepted medication therapy (methylphenidate or atomoxetine), can read and write the Chinese language, were legally able to sign informed consent, and signed the informed consent. Children who met the above criteria were invited to take part in this study.
Exclusion criteria were allergy to methylphenidate or atomoxetine, comorbidity with autism spectrum disorder, schizophrenia, epilepsy, head injury, or verified neurological disorder, intellectual disability (IQ <70), sensory retardation (hearing/vision problems), and unwilling or unable to give consent. Both the intervention group and the control group were treated with medication. This study provided a multimodal treatment for patients and teachers in the intervention group.
Randomization and Blinding
After the screening and diagnosis of students, the research team used a random number table method to divide the 10 primary schools participating in the study into the intervention group and the control group (5 schools in each group) stratified by school size. This occurred at the school, not at the class or individual level, in order to avoid contamination between individuals. Outcomes were obtained through questionnaires filled out by parents or teachers, and a limitation of the study is that teachers' and parents' assessment (questionnaires) are non-blinded. Statistical analysis was blinded to school intervention status when performing analysis of data results.
Parent Training
Parent training involved 4 weekly 2-h sessions, delivered in primary schools and consisted of: (1) knowledge about ADHD: etiology, manifestation, harm, and treatments; (2) medication: side effects and how to deal with them, teaching parents how to evaluate their children's behavior with the SNAP-IV scale; (3) teaching parents behavioral strategies to manage conduct problems, typically apply principles of positive and negative reinforcement; and (4) teaching parents to combine procedures and behavior management techniques, which can constructively target impairments in underlying processes, such as attention, impulse control, self-regulation, and working memory (17).
Teacher Training
Teacher training involved 4 weekly 2-h sessions, delivered in primary schools and conducted simultaneously with parent training. The teacher training was delivered in primary schools and conducted concurrently with parent training. It consisted of: (1) knowledge about ADHD: etiology, manifestation, harm, treatment, and follow-up; (2) behavioral strategies to manage conduct problems, typically applying principles of positive and negative reinforcement; (3) classroom behavior management; (4) teaching teachers how to use scaffolding to promote the development of self-regulation in children with ADHD, and how to take on the role of skilled tutor to create settings and occasions in a positive emotional climate, which can produce playful and reciprocal interactions (18).
When we designed training for parents and teachers, we referred to Family School Success (FSS) and simplified it. FSS is an integrative and novel psychosocial intervention for children with ADHD, which combines components of efficacious interventions to improve children's behavioral and academic functioning at home and school settings (19). FSS aims to improve parental involvement in education and parent–teacher collaboration in order to improve children's behavior and academic performance. However, there are currently only 135,524 pediatricians in China, just four per 10,000 children (20). Therefore, when we did the behavior management training, we simplified the course to make the training feasible and effective in China. Our goal is to extend the training program to more areas of China in order to validate our findings with a larger-scale population.
Statistical Analysis
The Statistical Package for the Social Sciences (SPSS) 21.0 was used. Descriptive statistics, means, standard deviations and frequencies were calculated. T-test was used for continuous variables and chi-square tests for categorical variables between the intervention group and the control group. Multiple regression models were created in which the scores of the total MARS were used as dependent variables.
Questionnaires
Conner's Parent Symptom Questionnaire and Conner's Teacher Symptom Questionnaire
Conner's Parent Symptom Questionnaire (PSQ)
PSQ is used to assess ADHD symptoms in primary school patients. It is a 48-item, parent-reported questionnaire using a four-point scale ranging from 0 to 3 and six subscales: conduct problems, learning problems, psychosomatic, hyperactivity–impulsivity, anxiety, and ADHD index (21). If the ADHD index is ≥1.5, it suggests that the patient may have ADHD.
Conner's Teacher Rating Scale (TRS)
TRS is a widely used instrument for evaluating behavioral problems in children and adolescents. It contains a 28-item teacher-reported questionnaire using a four-point scale ranging from 0 to 3 and four subscales: conduct, hyperactivity, inattention, and ADHD index (22). If the ADHD index is ≥1.5, it suggests that the patient may have ADHD.
Medication Adherence Report Scale
The Medication Adherence Report Scale (MARS) questionnaire is used to assess adherence to prescribed medication, which includes five statements using a five-point scale ranging from 1 to 5. One statement is related to the subscale of unintentional non-adherence (forgot to take them) and four statements are related to intentional non-adherence behaviors (altering the dosage, stopping medication use, missing a dose, taking less than instructed) (23). Higher scores indicate higher levels of medication adherence.
Swanson Nolan and Pelham, Version IV Scale Score
The Chinese Version of Swanson Nolan and Pelham, Version IV Scale (SNAP-IV) is used as the measure for the severity of ADHD symptoms. It consists of 26 items using a four-point scale ranging from 0 to 3 and three subscales: inattention, hyperactivity, and impulsivity (24). The primary outcome measure is the difference in the severity of ADHD core symptoms as measured by the SNAP-IV scales between the intervention group and the control group at baseline and 6 months follow-up.
Results
Baseline
From the 5,118 children who completed the screening questionnaire, 335 (6.55%) were positive from the screening. From those children, 230 (68.66%) were physician- diagnosed with ADHD. However, 19 students were excluded: 5 had intellectual disability, 1 dropped out of school, and 13 declined to participate in this study. One hundred sixteen children were assigned to the intervention group, and 95 were assigned to the control group.
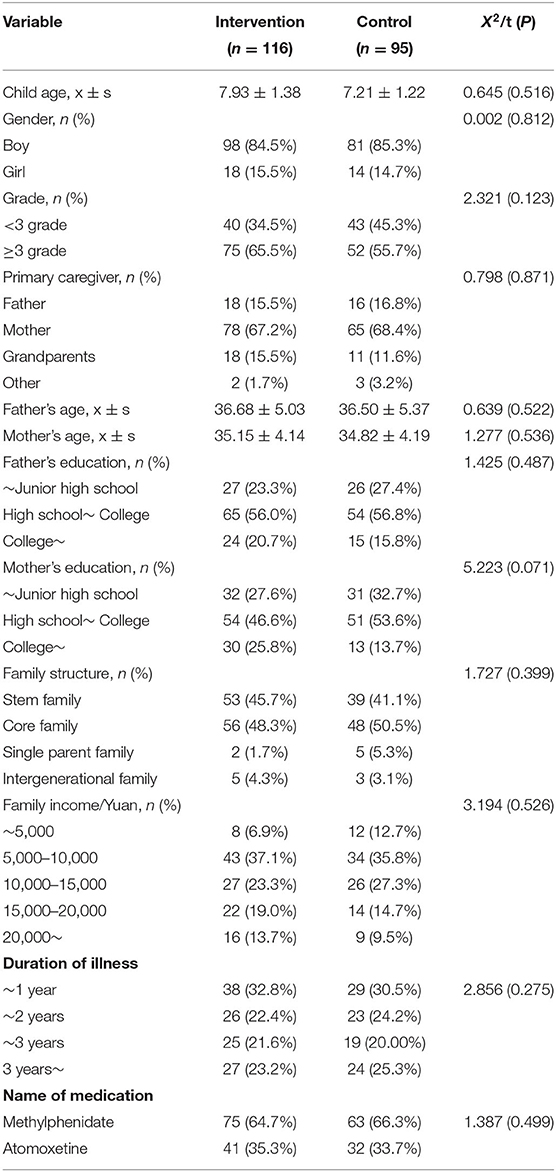
Table 1 shows the demographics of children in both groups. There were no statistically significant baseline differences between the intervention group and the control group (P > 0.05).
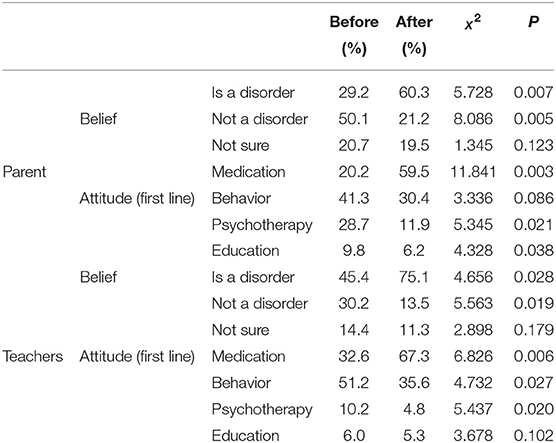
Beliefs and Attitudes Toward Treatment Before and After Training
Among parents, only 29.2% believed that ADHD was a neurological disorder before training, while after training, 60.3% believed that. In addition, only 20.2% believed that medication was the first-line treatment for ADHD before training, while after training, 60.3% believed that. Among teachers, only 45.4% believed that ADHD was a neurological disorder before treatment, while after training, 75.1% believed that. Before training, only 32.6% believed that medication was the first line-treatment for ADHD, while after training, 67.3% believed that. The differences were statistically significant (Table 2). Beliefs and attitudes were also compared in control groups between baseline and 6-month follow-up, and there is no statistical significance.
Medication Adherence at 6-Month Follow-Up in the Two Groups
A statistically significant difference was found in adherence measured by MARS. The MARS score for the intervention group was 22.8 (SD = 0.75), while it was 16.5 (SD = 1.63) for the control group (t = 5.217, P < 0.01), as shown in Figure 2. The difference was statistically significant.
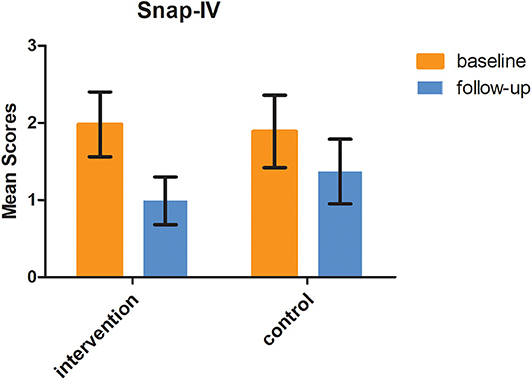
Figure 2. SNAP-IV scores at baseline and 6 months follow-up in the two groups (F = 2.67, P = 0.009).
Taking medication continuously for 6 months based on parents' reports and medical records was considered good medication adherence. In the intervention group, there were 82 children (70.69%) continuously taking medication for 6 months, while in the control group, there were only 35 children (36.84%) (Figure 3). The difference was statistically significant (X2 = 15.246, P < 0.001).
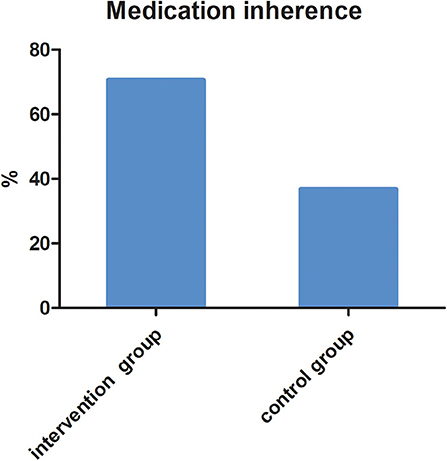
Figure 3. The proportion of children taking medication continuously for 6 months in two groups (X2 = 15.246, P = 0.001).
Multiple regression analysis was used to determine the factors influencing medication adherence. They were parent beliefs, teacher beliefs, socioeconomic status, adverse effects, insurance coverage, gender, and trust of the medical system (Table 3).
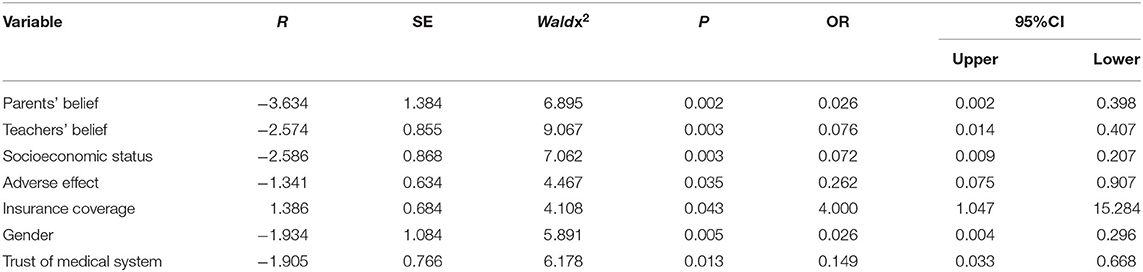
Table 3. Factors influencing medication adherence for children with attention-deficit/hyperactivity disorder (ADHD).
Swanson Nolan and Pelham, Version IV Scale Scores at Baseline and 6-Month Follow-Up in the Two Groups
In the intervention group, the SNAP-IV score was 1.98 ± 0.42 at baseline, while it was 0.99 ± 0.31 at 6-month follow-up. In the control group, the SNAP-IV score was 1.89 ± 0.47 at baseline and 1.37 ± 0.42 at 6-month follow-up. The difference of SNAP-IV score changes between the two groups was statistically significant (F = 2.67, P = 0.009), as shown in Figure 4.
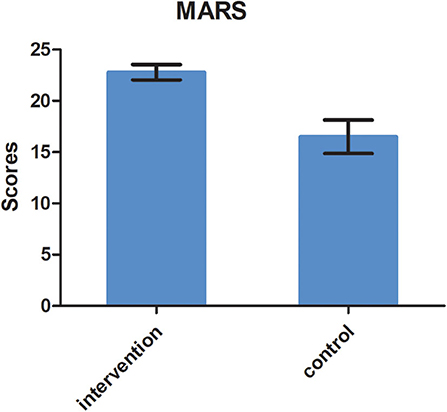
Figure 4. Medication adherence at 6 months follow-up in the two groups measured by MARS (t = 5.217, P = 0.01).
Discussion
In our study, there were many more parents and teachers who believed that ADHD was a neurobiological disorder, and medication was first-line treatment after training. There are about 20 million children with ADHD in China, but less than one third of them receive medication. Among those children who use medication, only 10% take it continuously and for an extended period. That means only 3% of the children with ADHD take medicine continuously in China. Medication treatment is often intermittent or short term. Thus, in China many children with ADHD do not receive proper treatment (25). Parent and teacher training is necessary and urgent because the most significant determinant of medication initiation is parent belief about ADHD and attitudes toward treatment (26). For instance, some parents who believe that the child's difficulties are a medical disorder that requires a biological intervention will accept using medication and encourage long-term use (27). However, in China, many parents would like to choose behavioral strategies and other non-medication strategies, such as counseling, exercise, or dietary changes (28). A lot of parents often weigh concerns about social disapproval and adverse effects and have complex feelings about starting medication (29). They will take a long time to make a decision and miss the best treatment window. Good treatment effects also need the cooperation of teachers. Doctors need to refer to teachers' evaluation reports both in the evaluation and treatment periods. Teachers should know that the difficulties are a neurobiological disorder and should have the correct understanding of medication treatment. Therefore, the training should include teachers as well.
In our study, the MARS score in the intervention group was much higher than that in the control group, which suggested better adherence in the intervention group. The MARS contains only five items, so it is convenient and advantageous in clinical settings (30). As far as we know, the MARS has not been used to study medication adherence in ADHD in China. At 6-month follow-up, there were 82 children (70.69%) continuously taking medication for 6 months in the intervention group, and so we concluded that medication adherence was 70.69% in the intervention group. This finding is consistent with a previous study. Adherence has been reported to range between 20 and 81% in children and adolescents with ADHD (31). Medication adherence in ADHD varies considerably, depending on the method of measurement and sample characteristics.
Medication adherence consists of multidimensional factors related to the children, parent/family, health-care system, therapy, and socioeconomic circumstances (32). In our study, factors influencing medication adherence for children with ADHD were parent beliefs, teacher beliefs, socioeconomic status, adverse effects, insurance coverage, gender, and trust of the medical system. For children with ADHD, medication decisions are usually made by their parents, and so parent beliefs and attitudes toward ADHD are of critical importance. Charach and Fernandez further highlighted that parent beliefs about ADHD medication outweigh evidence of the real benefits and risks (33). It was found that parent beliefs and attitudes have more impact on medication use.
In our study, children with higher socioeconomic status had better adherence. This finding is consistent with other studies. In the United States, children from higher income groups are more likely to accept prescriptions and to use medication consistently than children from lower income groups (34).
Of course, adverse effects should be taken into consideration in medication adherence studies. Converging studies described concerns about potential short- and long-term adverse effects. It was reported that as many as 29% of children experienced non-serious adverse events with methylphenidate use (14). Prior notification of possible side effects along with preventive and therapeutic measures during parent and teacher training can help to increase adherence to medication. The better adherence in boys may be due to the more explicit and severe symptoms they experience.
Regarding the influence of the type of ADHD medication on adherence, our study found there was no difference between stimulants and non-stimulants. The evidence is limited and conflicting regarding the influence of the type of ADHD medication on adherence. Sixty-seven percent less adherence to immediate-release stimulant treatment compared with non-stimulant treatment has been found in 3- to 18-year-old children (35). Another study showed similar rates of medication adherence with stimulants vs. non-stimulants (36). At 6-month follow-up, the mean SNAP-IV score in the intervention group was much lower than that in the control group, suggesting that medication combined with parent–teacher behavior management is more effective in alleviating the core symptoms in children with ADHD (37). Behavioral interventions implemented by teachers at school and by parents at home are well-established for children with ADHD (38). Multimodal treatments are beneficial because they can help providers address impairments directly in multiple domains through parent–teacher collaboration. Recent findings emphasize the need to enhance training for parents and teachers of children with ADHD with strategies for increasing family and school involvement in their child's academic life (39).
The possible reasons for the increase in medication adherence when the parent and teacher trainings focused on education and behavior management components. There is evidence that parental acceptance is higher for combined and behavioral intervention approaches compared to medication alone, and parents like parent training components of intervention; this may have been part of why adherence was improved compared to the medication only group (40). In addition, there is research suggesting that implementation of behavioral intervention in combination with medication management may reduce medication dosages for treatment of ADHD, resulting in lower side effects and higher parental satisfaction with treatment (41). Therefore, children in the intervention group may have had lower medication dosages, resulting in fewer side effects and increased tolerability and acceptance by parents.
Strengths and Limitations
The study provided a piloted, simplified, integrated training program for improving the knowledge, awareness, skill of management for ADHD children's parents and their teachers, which might help to facilitate the short-term clinical outcome and quality of life for children with ADHD.
There are several limitations in this study. The methodology for sampling and intervention in the study was single centered and district oriented, which limited the generalization of the conclusion. In addition, the evaluation tools for measuring the primary results were neither structured (questionnaire of beliefs and attitudes toward treatment) nor child-specific (MARS, five items), which weakened the interpretation of results. Risk factors identified to contribute to medication adherence were not validated because statistical results from multiple regression showed that OR value for insurance coverage only passed 1. Finally, information regarding the medication management of children in this study, both in the intervention and control groups, was not provided regarding changes in doses or medications utilized.
Conclusion
Our study employed 4-week, session-based training for both parents and teachers and determined the medication adherence with questionnaire and score of rating scale baseline and endpoint of 6-month following up. The findings from our study indicate that comprehensive training programs improve the knowledge of ADHD and medication inherence for both children's parents and teachers, providing a promising approach for improving clinical efficacy for children with ADHD.
Data Availability Statement
All datasets generated for this study are included in the article/Supplementary Material.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of Shanghai Children's Hospital. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
XZ, GY, and YW contributed to the conception, data analysis, and writing. LJ contributed to the data analysis and editing of the manuscript. LS, XS, and YX contributed to the data analysis. All authors approved of the final submitted version of this manuscript.
Funding
This work was funded by the project of the Shanghai Health and Hygiene Commission (2020YJZX0203), Shanghai Science and Technology Commission (18411967700, GWV-10.1-XK19, and GWV10.1-XK14), Rehabilitation Program of Shanghai (K2018007), and Shanghai Children's Health Services Capacity Planning Special Program for Advanced Pediatric Overseas Research Team Training Program (GDEK201710).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors are extremely grateful to all the members who took part in the project for their cooperation and help and to all of the volunteers whose efforts made this study possible.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2020.486353/full#supplementary-material
References
1. Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention- deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics. (2015) 135:e994–1001. doi: 10.1542/peds.2014-3482
2. Setyawan J, Fridman M, Grebla R, Harpin V, Korst LM, Quintero J. Variation in presentation, diagnosis, and management of children and adolescents with ADHD across European countries. J Atten Disord. (2018) 22:911–23. doi: 10.1177/1087054715597410
3. Mark LW, Joseph FH, Carla A, Eugenia C, Dale D, Marian E, et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention- deficit/ hyperactivity disorder in children and adolescents. Pediatrics. (2019) 144:e20192528. doi: 10.1542/peds.2019-2528
4. Osland ST, Steeves TD, Pringsheim T. Pharmacological treatment for attention deficit hyperactivity disorder (ADHD) in children with comorbid tic disorders. Cochrane Database Syst Rev. (2018) 6:CD007990. doi: 10.1002/14651858.CD007990.pub3
5. Franke B, Michelini G, Asherson P, Banaschewski T, Bilbow A, Buitelaar JK, et al. Live fast, die young? A review on the developmental trajectories of ADHD across the lifespan. Eur Neuropsychopharmacol. (2018) 28:1059–88. doi: 10.1016/j.euroneuro.2018.08.001
6. Turgay A, Goodman DW, Asherson P, Lasser RA, Babcock TF, Pucci ML, et al. Lifespan persistence of ADHD: the life transition model and its application. J Clin Psychiatry. (2012) 73:192–201. doi: 10.4088/JCP.10m06628
7. Chang Z, Lichtenstein P, Halldner L, B D'Onofrio, Serlachius E, Fazel S, et al. Stimulant ADHD medication and risk for substance abuse. J Child Psychol Psychiatry. (2014) 55:878–85. doi: 10.1111/jcpp.12164
8. Lichtenstein P, Larsson H. Medication for attention deficit-hyperactivity disorder and criminality. N Engl J Med. (2013) 368:776. doi: 10.1056/NEJMc1215531
9. Lopez FA, Leroux JR. Long-acting stimulants for treatment of attention- deficit/hyperactivity disorder: a focus on extended-release formulations and the prodrug lisdexamfetamine dimesylate to address continuing clinical challenges. Atten Defic Hyperact Disord. (2013) 5:249–65. doi: 10.1007/s12402-013-0106-x
10. de Sousa A, Kalra G. Drug therapy of attention deficit hyperactivity disorder: current trends. Mens Sana Monogr. (2012) 10:45–69. doi: 10.4103/0973-1229.87261
11. Wang T, Liu K, Li Z, Yu Y, Liu Y, Shi W, et al. Prevalance of attention deficit/hyperactivity disorder among children and adolescents in China: a systematic review and meta-analysis. Epidemiol Psychiatr Sci. (2017) 26:624–34. doi: 10.1186/s12888-016-1187-9
12. Regina B, Mirka KL, Kenji N, Dana M, Gillian M, Garvan CW. Willingness to use ADHD treatments: a mixed methods study of perceptions by adolescents, parents, health professionals and teachers. Soc Sci Med. (2012) 74:92–100. doi: 10.1016/j.socscimed.2011.10.009
13. Susan D, Matthew PM, Sara EEL, Alicia B, Riley AW, Myres MA. The meaning of attention-deficit/hyperactivity disorder medication and parents initiation and continuity of treatment for their child. J Child Adolesc Psychopharmacol. (2009) 19:377–83. doi: 10.1089/cap.2008.0118
14. Charach A, Fernandez R. Enhancing ADHD medication adherence: challenges and opportunities. Curr Psychiatry Rep. (2013) 15:371. doi: 10.1007/s11920-013-0371-6
15. Jin W, Du Y, Zhong X, David C. Prevalence and contributing factors to attention deficit hyperactivity disorder: a study of five- to fifteen-year-old children in Zhabei District, Shanghai. Asia Pac Psychiatry. (2014) 6:397–404. doi: 10.1111/appy.12114
16. Power TJ, Mautone JA, Soffer SL, Clarke AT, Marshall SA, Sharman J, et al. A family-school intervention for children with ADHD: results of a randomized clinical trial. J Consult Clin Psychol. (2012) 80:611–23. doi: 10.1037/a0028188
17. Tyrer P. Diagnostic and statistical manual of mental disorders: a classification of personality disorders that has had its day. Clin Psychol Psychother. (2012) 19:372–4. doi: 10.1002/cpp.1810
18. Webster-Stratton CH, Reid MJ, Beauchaine T. Combining parent and child training for young children with ADHD. J Clin Child Adolesc Psychol. (2011) 40:191–203. doi: 10.1080/15374416.2011.546044
19. Johnston C, Mash EJ, Miller N, Ninowski JE. Parenting in adults with attention- deficit/hyperactivity disorder (ADHD). Clin Psychol Rev. (2012) 32:215–28. doi: 10.1016/j.cpr.2012.01.007
20. Zhang Y, Huang L, Zhou X, Zhang X, Ke Z, Wang Z, et al. Characteristics and workload of pediatricians in China. Pediatrics. (2019) 144:e20183532. doi: 10.1542/peds.2018-3532
21. Evans SW, Owens JS, Wymbs BT, Ray AR. Evidence-based psychosocial treatments for children and adolescents with attention deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. (2018) 47:157–98. doi: 10.1080/15374416.2017.1390757
22. Conners CK, Sitarenios G, Parker JD, Epstein JN. The revised conners' parent rating scale (CPRS-R): factor structure, reliability, criterion validity. J Abnorm Child Psychol. (1998) 26:257–68.
23. Fumeaux P, Roche S, Mercier C, Iwaz J, Bader M, Stephan P, et al. Validation of the French version of conners' parent rating scale-revised, short version (CPRS- R:S): scale measurement invariance by sex and age. J Atten Disord. (2017) 24:1693–1700. doi: 10.1177/1087054717696767
24. Sampaio R, Azevedo LF, Dias CC, Horne R, Castro Lopes JM. Portuguese version of the medication adherence report scale (MARS-9): validation in a population of chronic pain patients. J Eval Clin Pract. (2019) 25:346–52. doi: 10.1111/jep.13098
25. Wagner DJ, McLennan JD. An alternative approach to scoring the MTA- SNAP-IV to guide attention-deficit/hyperactivity disorder medication treatment titration towards symptom remission: a preliminary consideration. J Child Adolesc Psychopharmacol. (2015) 25:749–53. doi: 10.1089/cap.2015.0081
26. Kivumbi A, Byansi W, Damulira C, Namatovu P, Mugisha J, Sensoy Bahar O, et al. Prevalence of behavioral disorders and attention deficit/hyperactive disorder among school going children in Southwestern Uganda. BMC Psychiatry. (2019) 19:105. doi: 10.1186/s12888-019-2069-8
27. Coletti DJ, Pappadopulos E, Katsiotas NJ, Berest A, Jensen PS, Kafantaris V. Parent perspectives on the decision to initiate medication treatment of attention- deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. (2012) 22:226–37. doi: 10.1089/cap.2011.0090
28. Dodangi N, Vameghi R, Habibi N. Evaluation of knowledge and attitude of parents of attention deficit/hyperactivity disorder children towards attention deficit/hyperactivity disorder in clinical samples. Iran J Psychiatry. (2017) 12:42–8.
29. Luan R, Mu Z, Yue F, He S. Efficacy and tolerability of different interventions in children and adolescents with attention deficit hyperactivity disorder. Front Psychiatry. (2017) 8:229. doi: 10.3389/fpsyt.2017.00229
30. Cao P, Xing J, Cao Y, Cheng Q, Sun X, Kang Q, et al. Clinical effects of repetitive transcranial magnetic stimulation combined with atomoxetine in the treatment of attention-deficit hyperactivity disorder. Neuropsychiatr Dis Treat. (2018) 14:3231–40. doi: 10.2147/NDT.S182527
31. Alsous M, Alhalaiqa F, Abu Farha R, Abdel Jalil M, McElnay J, Horne R. Reliability and validity of Arabic translation of Medication Adherence Report Scale (MARS) and beliefs about medication questionnaire (BMQ)-specific for use in children and their parents. PLoS ONE. (2017) 12:e0171863. doi: 10.1371/journal.pone.0171863
32. Tsai FJ, Tseng WL, Yang LK, Gau SS. Psychiatric comorbid patterns in adults with attention-deficit hyperactivity disorder: treatment effect and subtypes. PLoS ONE. (2019) 14:e0211873. doi: 10.1371/journal.pone.0211873
33. Burkhart PV, Sabate E. Adherence to long-term therapies: evidence for action. J Nurs Scholarsh. (2003) 35:207. doi: 10.1111/j.1547-5069.2003.tb00001.x
34. Bloom B, Jones LI, Freeman G. Summary health statistics for US children: National health interview survey 2012. Vital Health Stat. (2013) 10:1–81.
35. Storebo OJ, Simonsen E, Gluud C. Methylphenidate for attention- deficit/hyperactivity disorder in children and adolescents. JAMA. (2016) 315:2009–10. doi: 10.1001/jama.2016.3611
36. Gajria K, Lu M, Sikirica V, Greven P, Zhong Y, Qin P, et al. Adherence, persistence, and medication discontinuation in patients with attention-deficit/hyperactivity disorder - a systematic literature review. Neuropsychiatr Dis Treat. (2014) 10:1543–69. doi: 10.2147/NDT.S65721
37. Wehmeier PM, Dittmann RW, Banaschewski T. Treatment compliance or medication adherence in children and adolescents on ADHD medication in clinical practice: results from the COMPLY observational study. Atten Defic Hyperact Disord. (2015) 7:165–74. doi: 10.1007/s12402-014-0156-8
38. Chan SKC, Zhang D, Bögels SM, Chan CS, Lai KYC, Lo HHM, et al. Effects of a mindfulness-based intervention (MYmind) for children with ADHD and their parents: protocol for a randomised controlled trial. BMJ Open. (2018) 8:e022514. doi: 10.1136/bmjopen-2018-022514
39. Clarke A, Marshall S, Mautone J, Soffer S, Jones H, Costigan TE, et al. Parent attendance and homework adherence predict response to a family-school intervention for children with ADHD. J Clin Child Adolesc Psychol. (2015) 44:58–67. doi: 10.1080/15374416.2013.794697
40. Cristan AF, Nicole VB, Kenneth DG, Eugene AL, David GK, Robert LF. Comorbid symptomatology moderates response to risperidone, stimulant, and parent training in children with severe aggression, disruptive behavior disorder, attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. (2015) 25:213–24. doi: 10.1089/cap.2014.0109
Keywords: training, parent, teacher, ADHD, adherence, children
Citation: Zheng X, Shen L, Jiang L, Shen X, Xu Y, Yu G and Wang Y (2020) Parent and Teacher Training Increases Medication Adherence for Primary School Children With Attention-Deficit/Hyperactivity Disorder. Front. Pediatr. 8:486353. doi: 10.3389/fped.2020.486353
Received: 21 July 2019; Accepted: 05 October 2020;
Published: 09 November 2020.
Edited by:
Karen Muller Smith, University of Louisiana at Lafayette, United StatesReviewed by:
Erin Olufs, University of Iowa Hospitals and Clinics, United StatesE. Taylor Buckingham, The University of Iowa, United States
Copyright © 2020 Zheng, Shen, Jiang, Shen, Xu, Yu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu Wang, wy_rain@126.com; Guangjun Yu, gjyu@shchildren.com.cn
 Xiaofei Zheng1
Xiaofei Zheng1  Yu Wang
Yu Wang