Video Laryngoscopy Improves the Success of Neonatal Tracheal Intubation for Novices but Not for Experienced Medical Staff
- 1Department of Neonatology, Shanghai First Maternity and Infant Hospital, Tongji University School of Medicine, Shanghai, China
- 2Department of Anesthesiology, Shanghai First Maternity and Infant Hospital, Tongji University School of Medicine, Shanghai, China
Background: There is limited evidence on the use of video laryngoscopy (VL) in neonatal tracheal intubation (NTI) during neonatal resuscitation. In this study, we aimed to compare the difference between direct laryngoscopy (DL) and VL in NTI of trainees during neonatal resuscitation training.
Materials and Methods: A prospective observational study was conducted during a neonatal resuscitation training course to examine three circumstances: NTI by experienced medical staff (EMS) and less-experienced medical staff (LEMS) in a neonatal resuscitation scenario; NTI by EMS and LEMS with an ongoing chest compression; and NTI by midwives who were novices in the procedure. The trainees were given scenarios or were shown demonstrations on newborn simulation manikins and were required to perform an NTI on a simulation manikin using DL and/or VL. The mean intubation time and success rate of intubation were measured.
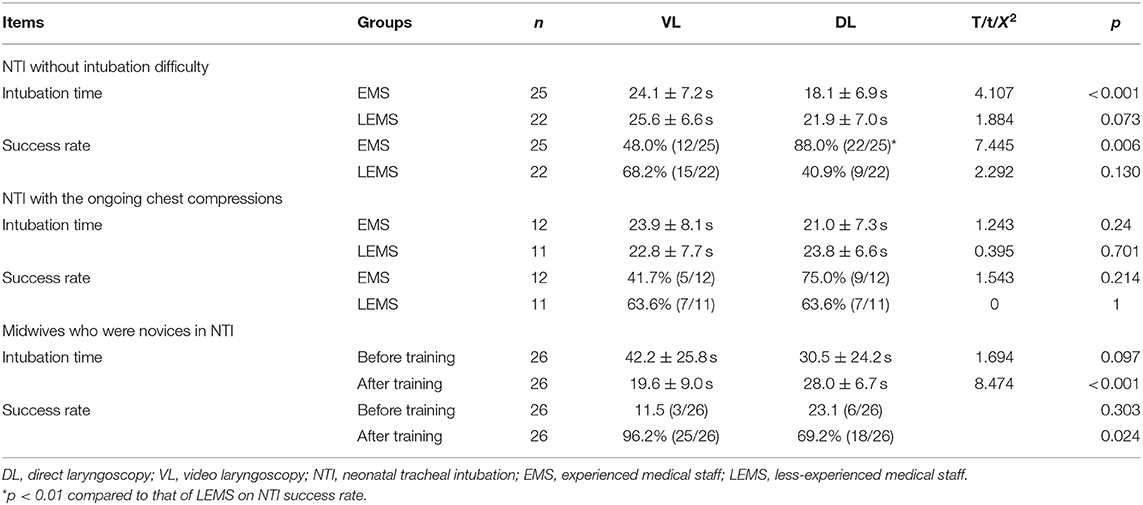
Results: The mean NTI time for EMS using VL (24.1 ± 7.2 s) was significantly longer than that using DL intubation (18.1 ± 6.9 s, P < 0.001), whereas there was no significant difference between using VL and DL for LEMS. EMS spent slightly less time on NTI than did LEMS using both VL and DL, but there were no statistically significant differences (both p > 0.05). The NTI success rate for EMS using VL (48.0%, 12/25) was significantly lower than that using DL (88.0%, 22/25, P = 0.004), while the NTI success rate for LEMS using VL (68.2%, 15/22 vs. 40.9%, 9/22) was higher than that using DL, but there was no statistical significance. When NTI was required with ongoing chest compressions, there was no significant difference in the mean NTI time and success rate between using VL and DL for EMS or LEMS. In the group of midwives who were novices in NTI, after they watched a demonstration teaching NTI, the intubation time using VL (19.6 ± 9.0 s) was significantly shorter than that using DL (28.0 ± 6.7 s, P < 0.001). The success rate of NTI using VL was significantly higher (96.2%; 25/26) than that using DL (69.2%; 18/26).
Conclusion: The video laryngoscopy could be an effective training tool for inexperienced staff in developing the skill of tracheal intubation.
Background
Intrapartum-related complications or birth asphyxia is one of the leading causes of neonatal death worldwide and in China (1). Worldwide, 0.7 million newborns die of birth asphyxia, accounting for 9% of childhood deaths under 5 years of age (2). It is also a major cause of neonatal morbidity and long-term sequelae (3). Some of the neonatal deaths associated with birth asphyxia can be prevented by prompt and effective neonatal resuscitation (4). Therefore, the American Academy of Pediatrics and the Chinese Academy of Pediatrics have recommended that at least one well-trained resuscitator should be present during delivery to address the possible risks (5, 6). Every medical staff member in the delivery room must be trained in neonatal resuscitation skills, including the initial step of resuscitation, positive pressure ventilation, intubation, chest compression, and medication administration via an umbilical vein catheters (UVC), in case neonatal resuscitation is necessary.
Among those who need resuscitation right after birth in the delivery room, ~3% of newborns need some help to start breathing, and 2% require tracheal intubation (TI) for further resuscitation (7). TI is an invasive and critical procedure. It is challenging for a resuscitator to intubate an ill newborn within a limited duration, mostly within 30 s, under the high stress associated with highly adverse events (8). It has been investigated whether medical staff has had decreasing opportunities for the practice of TI in the NICU (9). On the other hand, in 2015, NRP2015 recommended that TI should be performed to establish an artificial airway when external chest heart massage is performed. When CPR is started, it is usually necessary to stop massage to reduce the risk of TI failure (10). In recent years, video laryngoscopy (VL) has been widely used in adult and pediatric patients to establish artificial airways (11, 12). VL improves the view of the glottis and might reduce the risk of adverse events associated with TI. Limited evidence in the neonatal population has shown that VL also increases the success of neonatal intubation and has potential as a useful training tool (13). The purpose of this study was to compare the difference between direct laryngoscopy (DL) and VL in TI performed by trainees during neonatal resuscitation training and to explore the application value of VL.
Methods
This was a prospective study aiming to investigate the use of VL and DL in neonatal tracheal intubation (NTI). The subjects of this study were the participants of the neonatal resuscitation simulation training camp (NRSC) from November 9–11th, 2018, to March 22–24th, 2019, and the midwives of the delivery room of the Shanghai First Maternity and Infant Hospital, China. The NRSC training course has been provided every other month beginning in 2016. The curriculum of the NRSC comprises five skill stations (including initial steps, positive-pressure ventilation, the six corrective Step, i.e., mask adjustment, reposition airway, suction mouth and nose, open mouth, pressure increase, alternative Airway (MRSOPA), TI, chest compressions (CPR) and UVC insertion on the first day and five rounds of simulation training on the second day and the morning of the third day. There were 24 trainees in each camp from all over the country, and they were mainly the medical staff involved in neonatal resuscitation in the delivery room, including pediatricians, nurses, obstetricians, and midwives. This study was approved by the Ethical Committee of the hospital, and consent from the participants was waived because patient safety was not involved in this study.
Instruction for Intubation Procedure With VL or DL
Instructions for neonatal intubation were given as a demonstration to the trainee according to the NRP textbook (14). Briefly, the trainee stands by the head of the manikin and stabilizes the manikin's head with the right hand while the head is in the “sniffing” position. The manikin's mouth is gently opened; the laryngoscope blade is inserted into the right side of the mouth and slide over the right side of the tongue toward the midline. The tongue is gently pushed toward the left side of the mouth, and the blade is advanced until the tip lies just beyond the base of the tongue in the vallecula. The entire laryngoscope is lifted in the direction that the handle is pointing, moving the tongue out of the way to expose the glottis. The glottis appears at the very top of the view as facing the camera of the VL or the DL directly. Once the landmark is identified, the laryngoscope is held steady, the view of the vocal cords is maintained, and an assistant is asked to place the endotracheal tube in the right hand. The tube is inserted into the right side of the manikin's mouth. After insertion, the tube is directed into the hypopharynx and the tip is advanced toward the vocal cords. The tube is advanced until the vocal cords are positioned between the vocal cord guide lines. The tube is held securely against the manikin's upper palate. The laryngoscope is carefully removed without displacing the tube, and the endotracheal tube is secured.
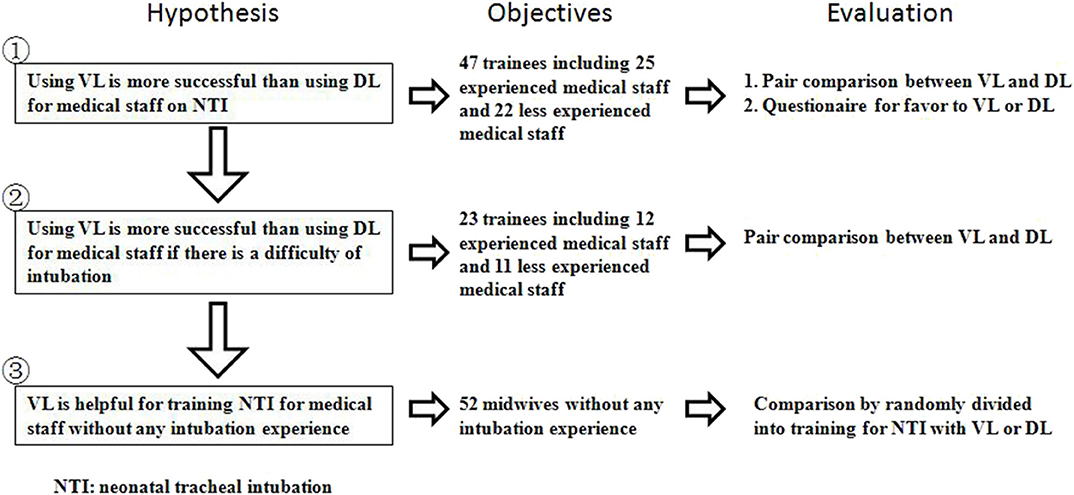
The study was divided into three parts according to the difficulty of intubation (Figure 1) and the level of NTI experience. The level of NTI experience was identified by self-reporting many intubation experiences as experienced medical staff (EMS) or self-reporting few intubation experiences as less-experienced medical staff (LEMS).
Part 1: Medical staff intubated a manikin under neonatal resuscitation. From November 9–11, 2018, to March 22–24, 2019 (during two consecutive training camps), the participants of the courses were randomly selected according to odd or even numbers of the group label number to test the difference between DL and VL in the neonatal resuscitation training by performing TI on a simulation manikin (SimNewB, Lardel) with a direct laryngoscope (Rlester, Germany) or a video laryngoscope (VDO-100c, VDO MEDICAL INC, Shanghai, China) (Figure 2) on the first and second day, respectively. The scenario was as follows: The infant was a non-vigorous, 40-wk singleton, and the amniotic fluid was clear. After positive-pressure ventilation (PPV) with bag and mask, there was insufficient manikin lung inflation, and the requirement for TI was identified. Participants were required to perform endotracheal intubation, with assistance from an instructor, within 30 s with a #1 blade 3.5-F tracheal tube. The other instructor used a stopwatch to monitor the time between when the blade was inserted into the mouth and when the blade was taken out of the mouth after the intubation was success or failure. After the intubation was completed, the trainee was required to ventilate through the resuscitation capsule 40–60 times/min and judge whether the intubation was successful by monitoring the air entry into the artificial chest by the computer of the manikin.
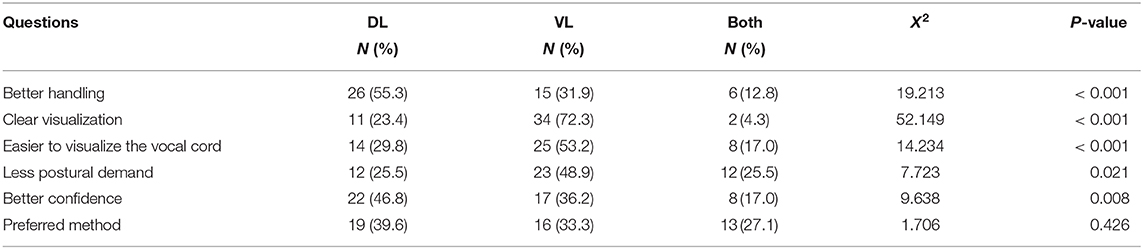
After 2 days of the TI training in both courses, participants were asked to complete a questionnaire on the differences between the direct laryngoscope and the video laryngoscope. There were six single-choice questions on the questionnaire, including questions regarding better handling, clearer visualization, easier visualization of the glottis, less postural demand, better confidence, and preferred method (Table 1).
Part 2: Medical staff intubated a manikin with intubation difficulty. To test the difference in intubation between DL and VL under difficult conditions during neonatal resuscitation training, 24 participants from March 22–24, 2019, were asked to perform another intubation procedure under difficult intubation circumstances after the previous test. The scenario was as follows: The infant was a 40-week singlenton with fetal heart rate deceleration before delivery, and the amniotic fluid was clear. The heart rate was still 50 beats/min after 30 s of effective ventilation. It was decided to start chest compressions after TI. However, the endotracheal tube was observed to be dislodged after chest compressions, and the participants were asked to perform intubation with a #1 blade and 3.5-F tracheal tube within 30 s with ongoing chest compressions. One instructor was an assistant for tracheal intubation, and another participant in the same training group was required to perform external chest compressions 90 times per minute. The other instructor used a stopwatch to time the participant as in the previous test (Figure 3). After the intubation was completed, the trainees were required to carry out chest compressions and ventilation coordinated at a ratio of 3:1. The success of intubation was confirmed as in the previous test.
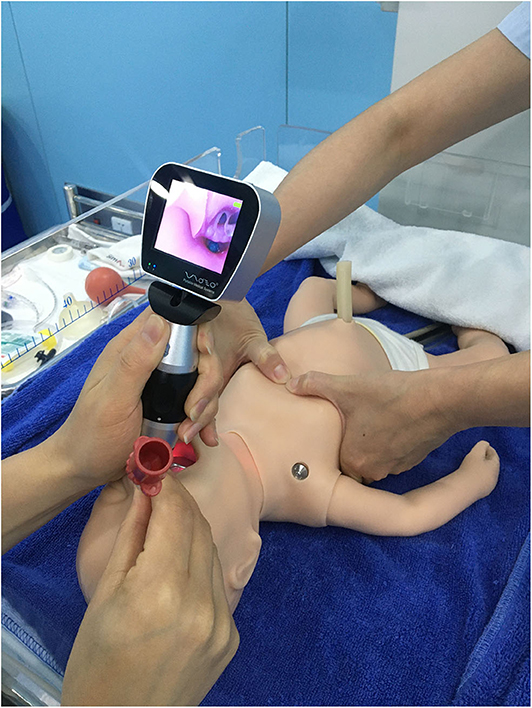
Figure 3. Neonatal tracheal intubation using a direct laryngoscope or a video laryngoscope when chest compression was continuous.
Part 3: Midwives without intubation experience performed NTI. To investigate the benefit of VL on the training of medical staff with no experience or training in NTI, endotracheal intubation training was set up in the delivery room of our hospital for midwives because they are unfamiliar with TI. The midwives were randomly divided into the DL and VL groups according to block randomization. TI was demonstrated by instructors using DL or VL with the midwives after the first attempt to intubate the manikin as previously (SimNewB, Lardel). The second attempt was made immediately after the trainees were instructed by the instructors using DL or VL according to the randomization. The measures of intubation were the same as in the previous tests.
Statistical Analysis
The mean value ± standard deviation was used for measurement data, and the paired t-test was used for the comparison of normally distributed data between the two groups on NRSC course groups. The t-test was used for the comparison of data from the midwives' intubation training. The chi-square test was used for the count data. P < 0.05 was statistically significant.
Results
There were 47 participants in these two training courses: 25 pediatricians or neonatologists, including 16 attending doctors with an average of 12.3 ± 6.4 years of experience, and 9 residents with an average of 4.6 ± 2.2 years of experience; three pediatric nurses with 6, 12, and 15 years of experience; 12 obstetricians, including 6 attending doctors with 18.8 ± 7.3 years of experience and 6 residents with 3.5 ± 3.0 years of experience; and 7 midwives with 11.6 ± 4.6 years of experience.
Mean NTI Time and Success Rate Using VL or DL
Among the 47 trainees, there were 25 EMS who self-reported many intubation experiences and 22 LEMS who self-reported few intubation experiences. The mean intubation time of EMS using VL was longer than that using DL (24.1 ± 7.2 vs. 18.1 ± 6.9 s), whereas there was no significant difference between VL and DL for LEMS (25.6 ± 6.6 s vs. 21.9 ± 7.0 s). It took a much longer time for trainees to visualize the field of view through the camera when using VL than when using DL. EMS spent slightly less time on NTI than did LEMS using both VL and DL, but there were no statistically significant differences (both p > 0.05) (Table 1).
The success rate of EMS using VL was significantly lower (48.0%, 12/25) than that using DL (88.0%, 22/25). Interestingly, the success rate of LEMS using VL was higher than that using DL, while there was no statistical significance between VL and DL (68.2%, 15/22 vs. 40.9%, 9/22). Although the success rate of EMS was significantly higher than that of LEMS using DL (88%, 22/25 vs. 40.9%, 9/22, x2 = 9.555, p = 0.002), VL improved the success rate of LEMS compared to that of EMS (68.2%, 15/22 vs. 48.0%, 12/25, x2 = 1.212, p = 0.271).
Questionnaire on the Use of VL or DL
Overall, the medical staff favored DL with respect to handling and confidence in intubation, whereas they favored VL with respect to clear visualization, visualization of the glottis and less postural demand (Table 2).
Mean NTI Time and Success Rate Using VL or DL Intubation Difficulty
The scenario of ongoing chest compressions when NTI was required was designed to increase the difficulty of intubating the manikin in this study. The mean intubation time for EMS was slightly longer using VL than using DL (23.9 ± 8.1 vs. 21.0 ± 7.3 s), while the mean intubation time for LEMS was slightly shorter using VL than DL (22.8 ± 7.7 vs. 23.8±6.6 s). There were no differences in the mean NTI time using VL or DL between EMS and LEMS (p > 0.05) with ongoing chest compressions (Table 1).
For EMS, the success rate of intubation was lower using VL than using DL (41.7%, 5/12 vs. 75.0%, 9/12), whereas for LEMS, it was the same using VL and DL (Table 1). The success rate of EMS was lower than that of LEMS using VL, but it was slightly higher than that of LEMS by using DL (both p > 0.05).
VL for NTI in Medical Staff Without Intubation Experience
A total of 52 midwives without any intubation experience participated in the study. They were randomly divided into two groups, the VL and DL groups, according to block randomization. The intubation time before training was 42.2 ± 25.8 s vs. 30.5 ± 24.2 s, respectively. VL took longer than DL, but there was no significant difference (t = 1.694, P = 0.097). The intubation success rate was 11.5% (3/26) vs. 23.1% (6/26) (p = 0.303).
After simulation training, the mean intubation time was 19.6 ± 9.0 s for VL vs. 28.0 ± 6.7 s for DL, and the NTI time was significantly shorter using VL than DL (t = 8.474, P < 0.001). The intubation success rate using VL was significantly higher (96.2%, 25/26) than that using DL (69.2%, 18/26; p = 0.024).
Discussion
In neonatal resuscitation, TI is a critical and dangerous technique for medical staff to implement under the stressful circumstance of birth asphyxia (8). Although medical staff in the delivery room is trained in TI as a part of the resuscitation curriculum, it is difficult to maintain the skill, especially in small maternal centers, with very few opportunities for resuscitation (15). In addition to simulating and practicing on a manikin regularly to maintain the knowledge and skill of TI, VL might demonstrate the anatomy of the glottis more easily than DL for novices during intubation (16).
Neonatal intubation has been used since 1940 to establish an artificial airway in pediatric patients who need airway management (17). The exposure and identification of the anatomy of the larynx are the most important steps for successful TI using DL (18). An attendant in the delivery room responding to neonatal resuscitation needs much practice to improve the success rate of intubation (19). Failed intubation is associated with multiple intubation attempts, desaturation, airway trauma, and even brain damage if artificial airway establishment is delayed (20). Therefore, a video laryngoscope, or an indirect laryngoscope, was designed and introduced to improve the view of the glottis via a fiber optic scope and a video camera at the tip of the blade (Figure 1). It has been shown in adult studies that VL improved the view of the glottis and the success rate of intubation and reduced the incidence of complications associated with the intubation procedure (11). However, the conclusions among these studies were inconsistent (21, 22). There was no improvement in the intubation success rate in these studies, although it is an alternative to DL. In pediatric patients, VL also improved visualization of the glottis but not the success rate of intubation (12). However, intubation took longer using VL than DL in this population. The National Emergency Airway Registry for Children database in the US includes data on 8,875 TIs in this population; 10% of intubations were performed by VL. VL was more often used in cases of airway difficulty and failed respiratory ventilation. It reduced the risk of adverse events in TI but not the risk of severe adverse events or number of intubation attempts (23). In addition, the use of VL in emergency airway management has been increasing (24).
Neonatal resuscitation is a very stressful form of technology, and medical staff needs to make judgments and decisions in a very short timeframe and complete a series of operations to save lives. In this case, these processes will significantly affect the success rate of TI. Even for very experienced doctors, under stressful circumstances, the success rate of endotracheal intubation decreased from 88 to 69%, and the time required will be extended by 4 s in our study. If CPR is not expected to stop during intubation, the impact on intubation must be minimized. VL is an important technique to improve the visual field and minimize posture-related requirements. In our study, the success rate using VL was still significantly lower than that using the familiar DL technique, but the intubation time was not different, which shows that good visualization, and posture can improve the TI experience. Currently, data on VL and DL as intubation tools for neonatal subjects are limited and controversial. In neonatal clinical practice, an international registry study of intubation reported 2,607 neonatal intubations in the US, Singapore and Canada (25). The study showed that 21% of neonatal intubations in the NICU and 11% in the delivery room were implemented by VL and independently associated with a reduced rate of intubation-associated adverse events. VL provides a better view of the glottis but does not decrease the intubation time or improve the success rate. The use of VL might be beneficial and shorten the intubation time if a view of the glottis is difficult to achieve (26). Failed intubation has been shown to be highly associated with anatomical visualization (18). Another training study using a simulation also proved that VL increased the success of intubation performed by pediatric residents (27). However, a meta-analysis of these trials demonstrated that while VL improved the success rate of neonatal intubation, the evidence was not strong (13). The intubation success rate was lower and the time requirement was longer using VL than using DL for the EMS in our training courses. Medical staff with a high level of experience with neonatal intubation prefers to use DL, since they feel more confident and comfortable with handling a familiar tool during an intubation practice in our training course (28). For resuscitators experienced with DL, it may take longer to finish the procedure, but with little difference in the success rates (29).
The resuscitator may sometimes perform intubation with ongoing chest compressions. Although few studies have reported that chest compressions may not interrupt the intubation process (30, 31), which is similar to the results of our study, it is important to reduce the risk of injury and relieve the stress of the intubator when continuous chest compressions are necessary. VL may improve the intubation time by providing a good view of the glottis compared with DL under the circumstances of uninterrupted chest compressions (32). These studies, including ours, reflect the performance of resuscitators or trainees in intubating manikins. Therefore, an observational study or clinical trial of VL vs. DL on this topic is warranted.
The trainees of the NRSC reported on our questionnaire that VL facilitates easier visualization of the anatomy and imposes less of a postural requirement on the medical staff, even with the first use of VL. One-third of the trainees with intubation experience favored its use as a result of the minor adaptation of visualization for intubation. The blade of the video laryngoscope may be designed to minimize the possibility of intubation-associated injury since the vocal cord do not have to be visualized for intubation (33). This method may help operators predict the difficulty of intubation (34). On the other hand, in efforts to train medical students with no intubation experience, VL improved the success rate of intubation in neonatal manikins, and this skill was transferrable to DL (35). As a training tool, VL provides feedback to learners. It allows learners to adapt the skill and translate it into clinical practice (36). VL could shorten the intubation time and improve the success rate significantly in training junior intubators or medical students. In our study, the novice providers tended to learn intubation skills more quickly using VL than using DL and translated them into clinical techniques, while more experienced providers performed better with DL (28).
There are some limitations to this study. First, it was a manikin study and may not fully reflect the clinical environment or the difficulty of neonatal intubation. The airway of the manikin is visually similar to that of a human newborn (Figure 1). We tried to minimize these effects in the simulation training course. The manikin training and the observations of this study can be translated into clinical practice. Second, the experience of the trainees was self–reported, which may have introduced bias. However, it was difficult to measure the intubation skill level of the trainees. Last, VL is a new intubation tool that many trainees were using for the first time, which may affect their performance intubating using VL. The trainees were given an opportunity to practice intubation on the same manikin using DL and VL at a skill station on the first day of the simulation course.
In conclusion, for medical staff with intubation experience using DL, VL did not improve the intubation success rate or the mean time. The intubation success rate using VL or DL was slightly affected by ongoing chest compressions. For midwives without any TI experience, VL training can significantly improve the intubation success rate, and shorten the intubation time.
Data Availability Statement
All datasets generated for this study are included in the article/supplementary material.
Ethics Statement
This study was approved by the Ethics Committee of Tongji University School of Medicine. The requirement for written informed consent was waived by the ethics committee.
Author Contributions
MZ and JQ-L analyzed the data and drafted the manuscript. XX, ML, and SW collected the data. ZL and JQ-L designed the study. All authors contributed to the article and approved the submitted version.
Funding
Shanghai municipal medical and health discipline construction projects (No. 2017ZZ02015); National continuing medical education project of China (2018-06-03-021, 2019-06-03-073); Science and Technology Commission of Shanghai Municipality (16DZ1930305).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
VL, video laryngoscopy; NTI, neonatal tracheal intubation; DL, direct laryngoscopy; NRSC, neonatal resuscitation simulation training camp; CPR, chest compression; UVC, umbilical vein catheters; MRSOPA, mask adjustment, reposition airway, suction mouth and nose, open mouth, pressure increase alternative Airway.
References
1. Song P, Theodoratou E, Li X, Liu L, Chu Y, Black RE, et al. Causes of death in children younger than five years in China in 2015: an updated analysis. J Glob Health. (2016) 6:020802. doi: 10.7189/jogh.06.020802
2. Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. (2012) 379:2151–61. doi: 10.1016/S0140-6736(12)60560-1
3. Milner KM, Neal EF, Roberts G, Steer AC, Duke T. Long-term neurodevelopmental outcome in high-risk newborns in resource-limited settings: a systematic review of the literature. Paediatr Int Child Health. (2015) 35:227–42. doi: 10.1179/2046905515Y.0000000043
4. Kamath-Rayne BD, Berkelhamer SK, Kc A, Ersdal HL, Niermeyer S. Neonatal resuscitation in global health settings: an examination of the past to prepare for the future. Pediatr Res. (2017) 82:194–200. doi: 10.1038/pr.2017.48
5. Pe Perlman JM, Wyllie J, Kattwinkel J, Atkins DL, Chameides L, Goldsmith JP. Neonatal resuscitation: 2010 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Pediatrics. (2010) 126:e1319–44. doi: 10.1542/peds.2010-2972B
6. Chinese steering committee of neonatal resuscitation. Update of neonatal resuscitation in 2011 Beijing. Chin J Perinatol. (2011) 14:415–9. doi: 10.3760/cma.j.issn.1007-9408.2011.03.003
7. Barber CA, Wyckoff MH. Use and efficacy of endotracheal versus intravenous epinephrine during neonatal cardiopulmonary resuscitation in the delivery room. Pediatrics. (2006) 118:1028–34. doi: 10.1542/peds.2006-0416
8. Umoren RA, Sawyer TL, Ades A, deMeo S, Foglia EE, Glass K, et al. Team stress and adverse events during neonatal tracheal intubations: a report from NEAR4NEOS. Am J Perinatol. (2019). doi: 10.1055/s-0039-1693698. [Epub ahead of print].
9. Gozzo YF, Cummings CL, Chapman RL, Bizzarro MJ, Mercurio MR. Who is performing medical procedures in the neonatal intensive care unit? J Perinatol. (2011) 31:206–11. doi: 10.1038/jp.2010.121
10. Perlman JM, Wyllie J, Kattwinkel J, Wyckoff MH, Aziz K, Guinsburg R, et al. Part 7: neonatal resuscitation: 2015 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. (2015) 132(16 Suppl. 1):S204–41. doi: 10.1161/CIR.0000000000000276
11. Lewis SR, Butler AR, Parker J, Cook TM, Schofield-Robinson OJ, Smith AF. Video laryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation: a cochrane systematic review. Br J Anaesth. (2017) 119:369–83. doi: 10.1093/bja/aex228
12. Abdelgadir IS Phillips RS Singh D Moncreiff MP Lumsden JL. Video laryngoscopy versus direct laryngoscopy for tracheal intubation in children (excluding neonates). Cochrane Database Syst Rev. (2017) 5:CD011413. doi: 10.1002/14651858.CD011413.pub2
13. Lingappan K, Arnold JL, Fernandes CJ, Pammi M. Video laryngoscopy versus direct laryngoscopy for tracheal intubation in neonates. Cochrane Database Syst Rev. (2018) 6:CD009975. doi: 10.1002/14651858.CD009975.pub3
14. Weiner GM. Textbook of Neonatal Resuscitation. 7th ed. Elk Grove Village, IL: American Academy of Pediatrics (2016).
15. Andreatta PB, Dooley-Hash SL, Klotz JJ, Hauptman JG, Biddinger B, House JB. Retention curves for pediatric and neonatal intubation skills after simulation-based training. Pediatr Emerg Care. (2016) 32:71–6. doi: 10.1097/PEC.0000000000000603
16. Koele-Schmidt L, Vasquez MM. NewB for newbies: a randomized control trial training housestaff to perform neonatal intubation with direct and video laryngoscopy. Paediatr Anaesth. (2016) 26:392–8. doi: 10.1111/pan.12832
17. Doherty JS, Froom SR, Gildersleve CD. Pediatric laryngoscopes and intubation aids old and new. Paediatr Anaesth. (2009) 19(Suppl. 1):30–7. doi: 10.1111/j.1460-9592.2009.03001.x
18. O'Shea JE, Loganathan P, Thio M, Kamlin COF, Davis PG. Analysis of unsuccessful intubations in neonates using videolaryngoscopy recordings. Arch Dis Child Fetal Neonatal Ed. (2018) 103:F408–12. doi: 10.1136/archdischild-2017-313628
19. Mulcaster JT, Mills J, Hung OR, MacQuarrie K, Law JA, Pytka S. Laryngoscopic intubation: learning and performance. Anesthesiology. (2003) 98:23–7. doi: 10.1097/00000542-200301000-00007
20. Lee JH, Turner DA, Kamat P, Nett S, Shults J, Nadkarni VM, et al. The number of tracheal intubation attempts matters! A prospective multi-institutional pediatric observational study. BMC Pediatr. (2016) 16:58. doi: 10.1186/s12887-016-0593-y
21. Hoshijima H, Mihara T, Maruyama K, Denawa Y, Mizuta K, Shiga T, et al. C-MAC video laryngoscope versus macintosh laryngoscope for tracheal intubation: a systematic review and meta-analysis with trial sequential analysis. J Clin Anesth. (2018) 49:53–62. doi: 10.1016/j.jclinane.2018.06.007
22. Bhattacharjee S, Maitra S, Baidya DK. A comparison between video laryngoscopy and direct laryngoscopy for endotracheal intubation in the emergency department: a meta-analysis of randomized controlled trials. J Clin Anesth. (2018) 47:21–6. doi: 10.1016/j.jclinane.2018.03.006
23. Grunwell JR, Kamat PP, Miksa M, Krishna A, Walson K, Simon D, et al. Trend and outcomes of video laryngoscope use across PICUs. Pediatr Crit Care Med. (2017) 18:741–9. doi: 10.1097/PCC.0000000000001175
24. Goto Y, Goto T, Hagiwara Y, Tsugawa Y, Watase H, Okamoto H, et al. Techniques and outcomes of emergency airway management in Japan: an analysis of two multicentre prospective observational studies, 2010-2016. Resuscitation. (2017) 114:14–20. doi: 10.1016/j.resuscitation.2017.02.009
25. Foglia EE, Ades A, Sawyer T, Glass KM, Singh N, Jung P, et al. Neonatal intubation practice and outcomes: an International registry study. Pediatrics. (2019) 143:e20180902. doi: 10.1542/peds.2018-0902
26. Tao B, Liu K, Zhao P, Wang D, Liu Y, Yin H. Comparison of glidescope video laryngoscopy and direct laryngoscopy for tracheal intubation in neonates. Anesth Analg. (2019) 129:482–6. doi: 10.1213/ANE.0000000000003637
27. Parmekar S, Arnold JL, Anselmo C, Pammi M, Hagan J, Fernandes CJ, et al. Mind the gap: can video laryngoscopy bridge the competency gap in neonatal endotracheal intubation among pediatric trainees? A randomized controlled study. J Perinatol. (2017) 37:979–83. doi: 10.1038/jp.2017.72
28. Musharaf I, Daspal S, Shatzer J. Is video laryngoscopy the optimal tool for successful intubation in a neonatal simulation setting? A single-center experience. AJP Rep. (2020) 10:e5–10. doi: 10.1055/s-0039-3400970
29. Kim JW, Park SO, Lee KR, Hong DY, Baek KJ, Lee YH, et al. Video laryngoscopy vs. direct laryngoscopy: which should be chosen for endotracheal intubation during cardiopulmonary resuscitation? A prospective randomized controlled study of experienced intubators. Resuscitation. (2016) 105:196–202. doi: 10.1016/j.resuscitation.2016.04.003
30. Donoghue A, Hsieh TC, Nishisaki A, Myers S. Tracheal intubation during pediatric cardiopulmonary resuscitation: a videography-based assessment in an emergency department resuscitation room. Resuscitation. (2016) 99:38–43. doi: 10.1016/j.resuscitation.2015.11.019
31. Rodríguez-Núñez A, Moure-González J, Rodríguez-Blanco S, Oulego-Erroz I, Rodríguez-Rivas P, Cortiñas-Díaz J. Tracheal intubation of pediatric manikins during ongoing chest compressions. Does Glidescope® videolaryngoscope improve pediatric residents' performance? Eur J Pediatr. (2014) 173:1387–90. doi: 10.1007/s00431-014-2329-z
32. Truszewski Z, Czyzewski L, Smereka J, Krajewski P, Fudalej M, Madziala M, et al. Ability of paramedics to perform endotracheal intubation during continuous chest compressions: a randomized cadaver study comparing pentax AWS and macintosh laryngoscopes. Am J Emerg Med. (2016) 34:1835–9. doi: 10.1016/j.ajem.2016.06.054
33. Kirolos S, O'Shea JE. Comparison of conventional and videolaryngoscopy blades in neonates. Arch Dis Child Fetal Neonatal Ed. (2020) 105:94–7. doi: 10.1136/archdischild-2018-315644
34. Nausheen F, Niknafs NP, MacLean DJ, Olvera DJ, Wolfe AC Jr, Pennington TW. The HEAVEN criteria predict laryngoscopic view and intubation success for both direct and video laryngoscopy: a cohort analysis. Scand J Trauma Resusc Emerg Med. (2019) 27:50. doi: 10.1186/s13049-019-0614-6
35. Assaad MA, Lachance C, Moussa A. Learning neonatal intubation using the video laryngoscope: a randomized trial on Mannequins. Simul Healthc. (2016) 11:190–3. doi: 10.1097/SIH.0000000000000141
Keywords: simulation, neonate, tracheal intubation, video laryngoscopy, resuscitation
Citation: Zhou M, Xi X, Li M, Wang S, Liu Z and Liu J-Q (2020) Video Laryngoscopy Improves the Success of Neonatal Tracheal Intubation for Novices but Not for Experienced Medical Staff. Front. Pediatr. 8:445. doi: 10.3389/fped.2020.00445
Received: 03 March 2020; Accepted: 26 June 2020;
Published: 06 August 2020.
Edited by:
Eugene Dempsey, University College Cork, IrelandReviewed by:
Joyce O. Shea, Royal Hospital for Children, United KingdomLiam Mahoney, Southmead Hospital, United Kingdom
Copyright © 2020 Zhou, Xi, Li, Wang, Liu and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiang-Qin Liu, jiangqinliu@163.com
 Ming Zhou
Ming Zhou Xiaohong Xi1
Xiaohong Xi1  Zhiqiang Liu
Zhiqiang Liu Jiang-Qin Liu
Jiang-Qin Liu