- Department of Obstetrics and Gynecology, Shengjing Hospital of China Medical University, Shenyang, China
Background: Intravascular leiomyomatosis is a rare benign lesion with malignant potential. The cases are sporadic. Most patients have no clinical symptoms, and the preoperative diagnostic rate is low. Case 1 was misdiagnosed, passively managed during operation, recurred quickly, and underwent a secondary operation. We learned lessons from case 1 and treated the case 2 patient differently. The case 2 patient had a good prognosis. We hope the report will be helpful to other gynecologists.
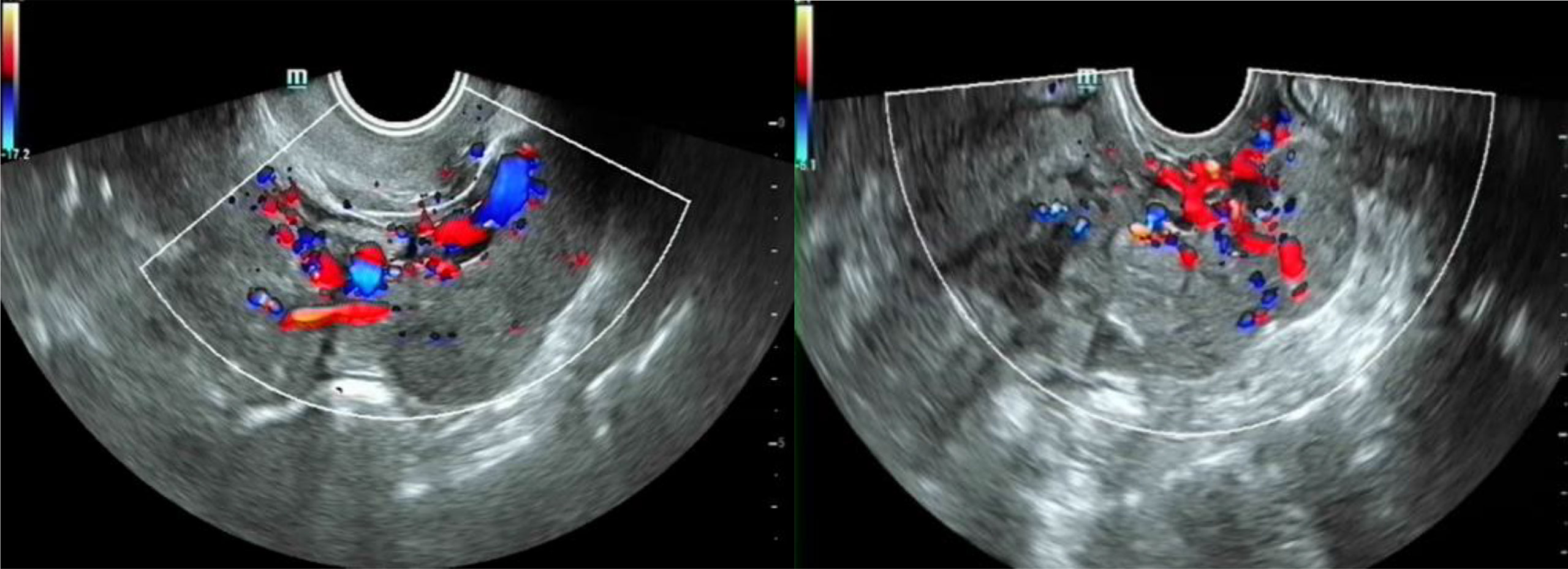
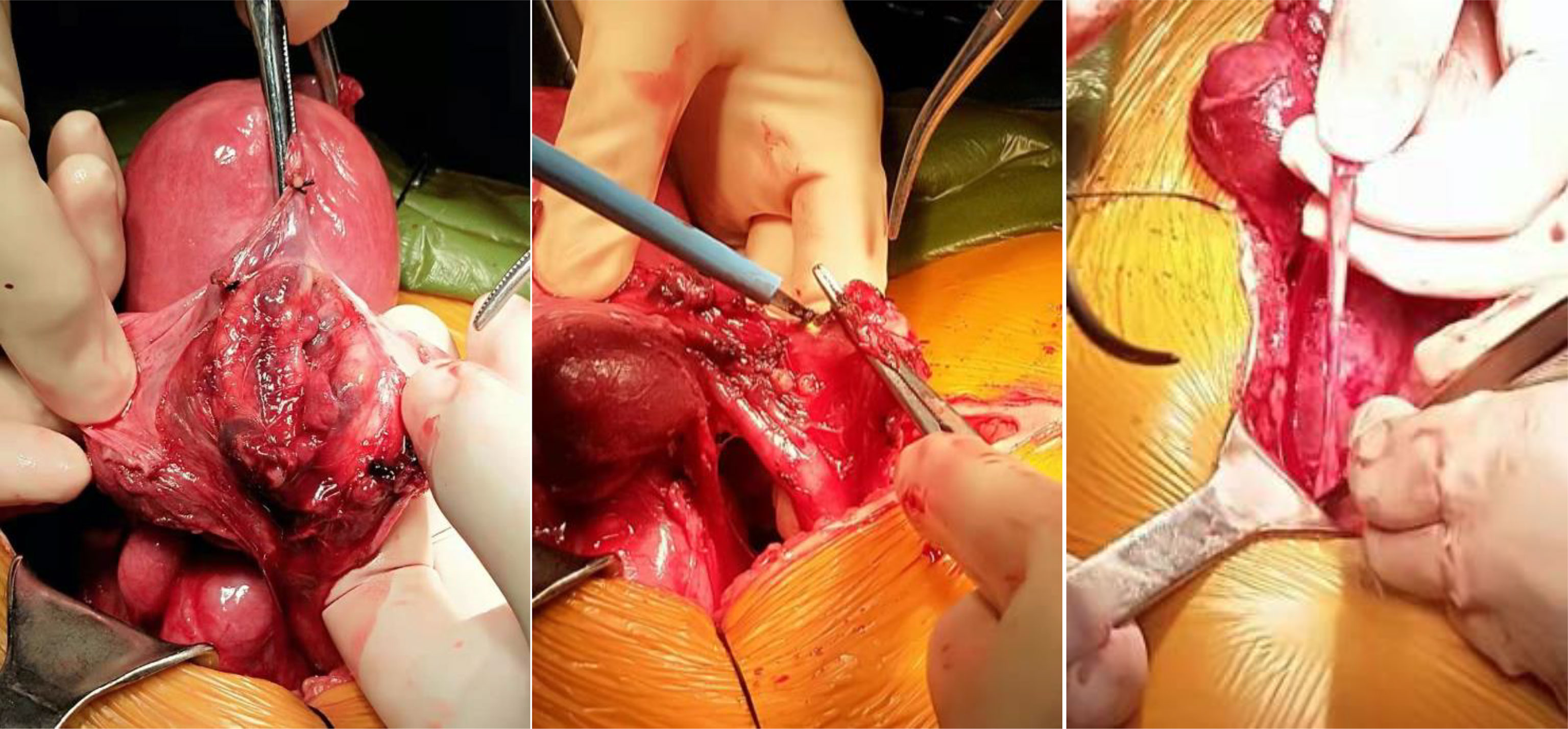
Case Summary: Case 1: a 49-year-old woman complained of dysmenorrhea. Traditional ultrasound showed adenomyosis and a solid mass 6 * 3 cm in the right appendix. After routine examination, the patient underwent transabdominal total hysterectomy + bilateral salpingectomy + IVL tumor resection, with both ovaries kept. No medication was used after operation. Routine ultrasound was performed every 3 months. The disease recurred, and the patient underwent a secondary surgery 9 months after the first time. So far, 25 months after the secondary surgery, there is no sign of recurrence. Case 2: a 41-year-old woman underwent a routine body examination, where a left adnexal mass 7 cm was found. The patient underwent contrast-enhanced ultrasonography and was diagnosed and prepared well preoperatively. The patient underwent transabdominal total hysterectomy + bilateral salpingectomy + IVL tumor resection. GnRH-a drugs were used after operation for 3 cycle. Now, there is no sign of recurrence after operation for 23 months.
Conclusion: The incidence rate of IVL is low, and there are no typical clinical symptoms. It is easy to be ignored by gynecologists. Contrast-enhanced ultrasound is helpful to diagnose preoperatively and reduce misdiagnosis. Good preparation, full exploration of the pelvic and abdominal vessels, removal of lesions completely as much as possible, and anti-estrogen therapy after operation can reduce the recurrence of disease.
Introduction
Intravascular leiomyomatosis (IVL) is a special type of uterine myoma. The preoperative diagnosis rate is low because of no specific symptom, which leads to misdiagnosis. Inadequate pelvic exploration and missed lesions will increase the recurrence rate. This paper summarizes the experience and lessons from one misdiagnosed case; the second case is fully prepared and the treatment effect is good. We review the relevant literature, hoping to provide help to other clinical colleagues.
Case Introduction
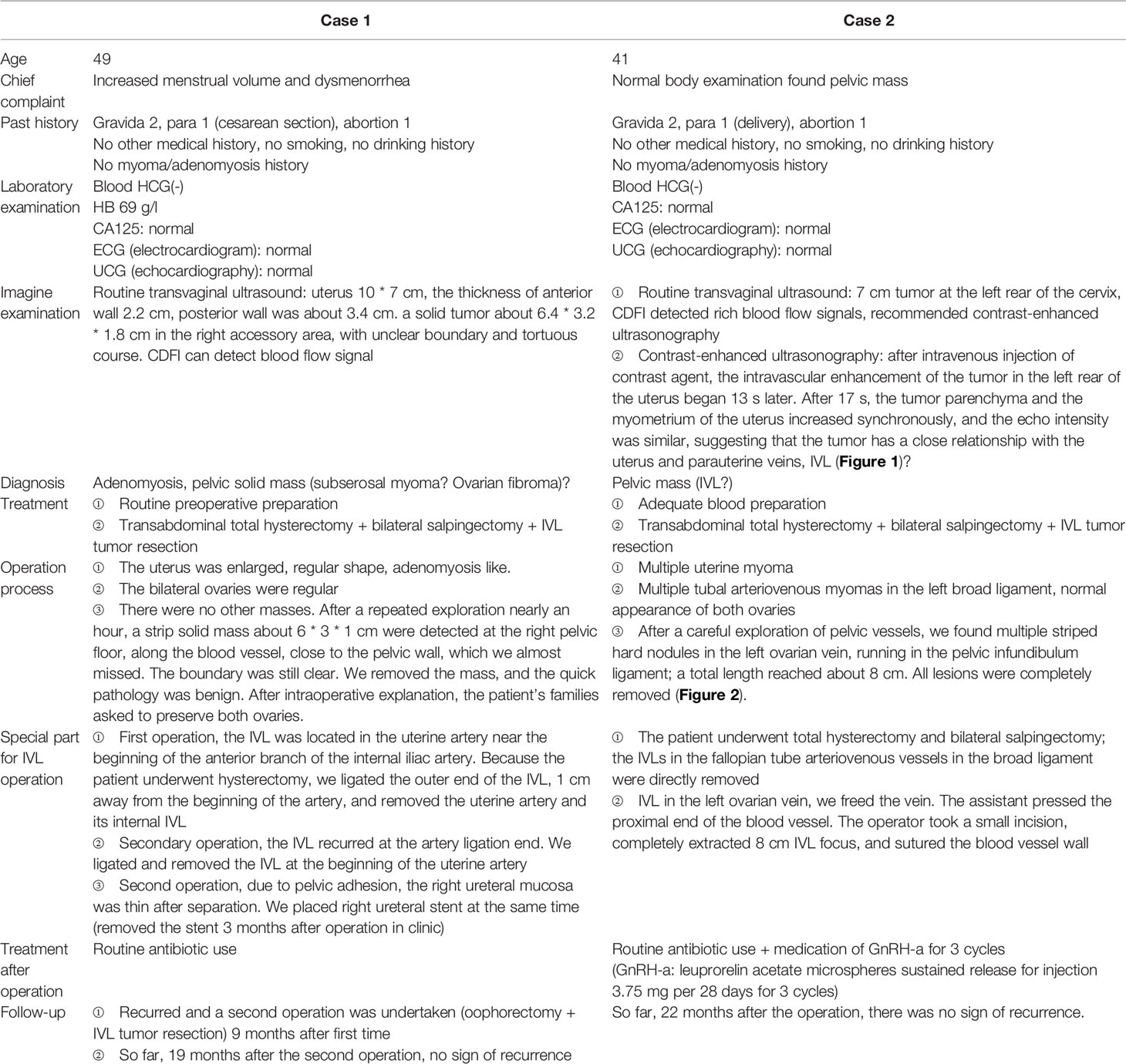
Medical history of the two cases displayed in Table 1.
Related Literature Learning
IVL mainly consists of benign smooth muscle tissue spreading and growing along the venous lumen. It is a rare special type of uterine myoma in gynecology. The onset age was 40–60 years, and 60% of the patients had a history of uterine myoma. The two patients we met had no previous history of hysteromyoma, but multiple hysteromyoma or adenomyosis was found in both cases during our operations. IVL invades not only the pelvic vein, inferior vena cava, renal vein, and pulmonary artery but also distant metastasis to the heart, lung, brain, and lymph nodes (1–3). The cases have been sporadic and mainly female. It is found that up to 10% of the cases invade the heart (4). Once the heart is involved, there may be symptoms such as palpitation, dyspnea, syncope, and edema of both lower limbs, and may even be life-threatening. At present, the cause of its pathogenesis is not completely clear. Most scholars believe that it is related to hormone level, local small injury, and venous congestion (5).
IVL has no obvious clinical symptoms and signs, and the preoperative diagnosis rate is very low. It is often misdiagnosed as uterine myoma, adenomyosis, pelvic malignancy, and so on. Our first case was misdiagnosed as uterine subserosal myoma or ovarian solid mass before operation. We were passive in finding the IVL lesion during operation, almost missing it. We spent nearly an hour to search the mass and only gave the patient routine blood preparation before operation. IVL is an estrogen-dependent benign disease and is recurrent. According to the intraoperative findings and quick frozen pathology, for older patients, bilateral oophorectomy can be considered to reduce recurrence. In our case 1, because the possibility of IVL was not fully considered before operation, we felt passive during the operation and almost missed the focus. The families were not fully prepared for oophorectomy during operation. Bilateral ovaries were preserved, and there was no medication after operation; the disease recurred half a year after operation. 9 months after the first operation, the patient took a secondary operation and experienced physical, psychological, and economic trauma again. During the second operation, because of pelvic tissue inflammatory adhesion, the operation was very difficult, and the risk of injury of adjacent organs such as the ureter is also greatly increased.
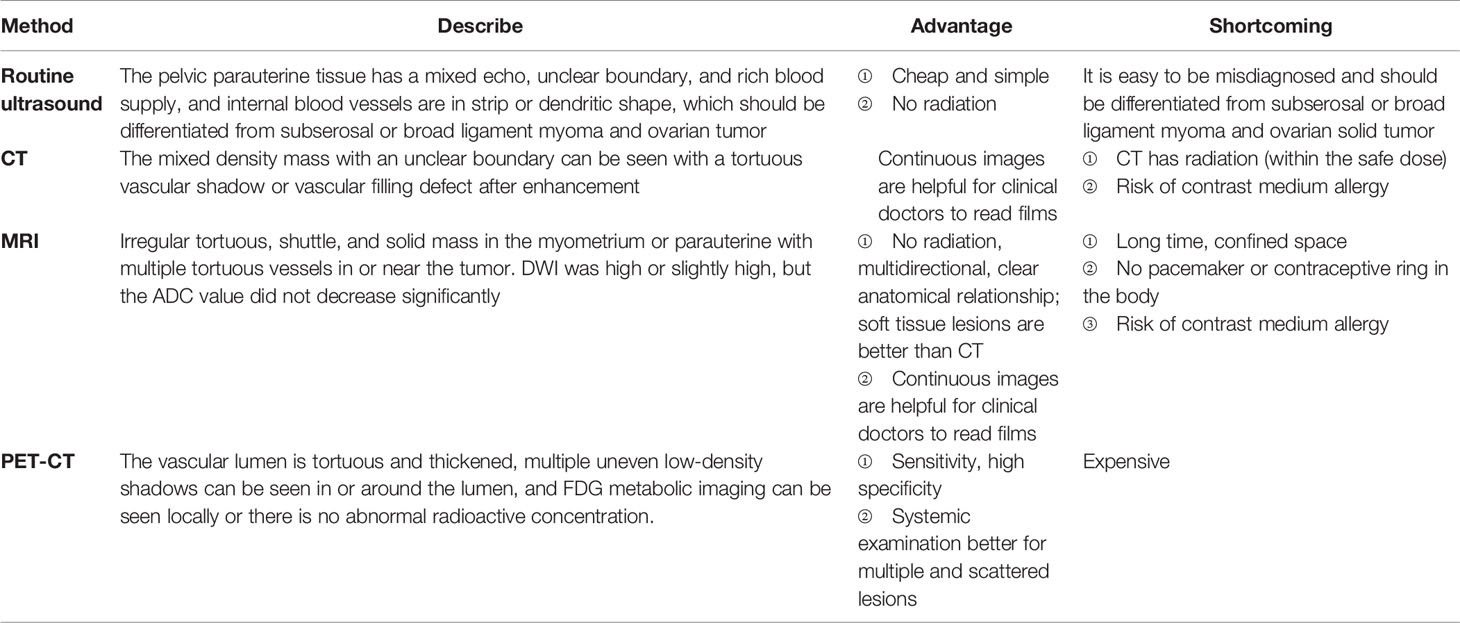
The advantages and disadvantages of common inspection methods are shown in Table 2. With the development of medicine, on the basis of ultrasound, the use of contrast agents has more and more advantages in the diagnosis of vascular-related diseases, especially in IVL. In this paper, the second patient was diagnosed clearly depending on the contrast-enhanced ultrasonography before operation and was fully prepared before operation; exploration during operation was comprehensive and supplementary medication after operation was timely. The prognosis was good.
In general, the uterus of IVL can be enlarged, most of which are complicated with uterine myoma or adenomyosis. Tumors can be seen in the uterine wall, parauterine ligament, and adnexal vein, most of which are cord like, Flammulina velutipes like, and bead like, which can twitch. The section is gray, pink white, and soft or hard. Microscopically, the tumor cells were spindle shaped, braided, or vortex shaped, and the surface was covered with a single layer of flat vascular endothelial cells. There was no or occasional mitotic image. Previous reports suggested specific immunohistochemical markers, including tumor cells vimentin (+), desmin (+), and SMA (+), and endothelial cells of venous vessels CD34 (+), especially ER and PR (+).
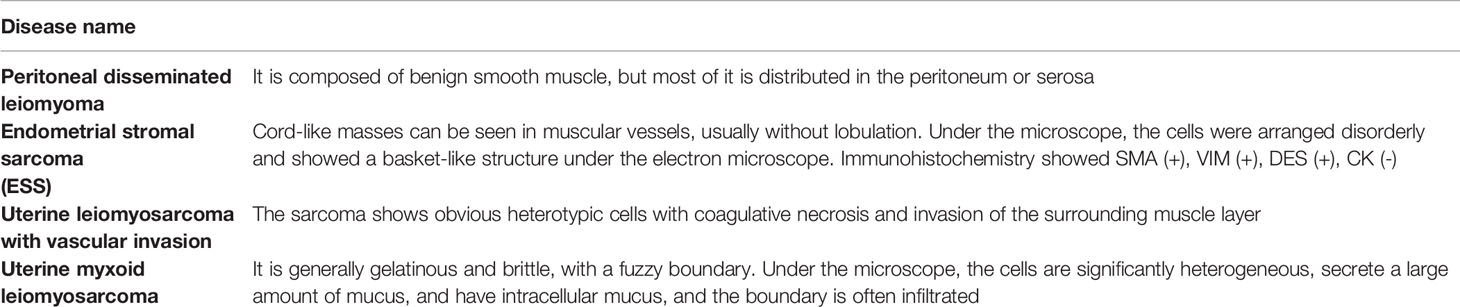
IVL should be differentiated from uterine fibroids and ovarian cysts, as well as the following diseases under a pathological microscope (Table 3).
IVL is mainly treated by surgery. Because the tumor is diffuse and the recurrence rate is high, complete resection of the tumor is the key of surgery. Li et al. (6) sorted and analyzed the clinical data, pathological characteristics, and treatment methods of 194 IVL patients whose lesions extended to the heart publicly reported abroad. It was found that incomplete resection of IVL lesions would increase the recurrence rate and postoperative mortality. Wang et al. (7) also reported that the recurrence rate of complete resection was 21.4%, and that of incomplete resection was 50%. The difference was statistically significant.
Kokawa et al. (8, 9) found that ER and PR were positively expressed in IVL, and the estrogen receptor in IVL tissue was 10 times higher than that in normal tissue, and the progesterone receptor was 50 times higher. At the same time, the level of estradiol in serum was significantly increased (8). Therefore, in addition to surgical resection, some hormone drugs such as GnRH-a and aromatase inhibitor anti-estrogen therapy have also been introduced into IVL treatment. There is a debate about the therapeutic effect of hormone drugs in some literature. Lin et al. (6) reported that the use of anti-estrogen therapy after operation cannot prevent disease recurrence, but Bondner (10) and Nishizawa (11) reported that the preoperative application of anti-estrogen drug GnRH-a can reduce the IVL tumor volume by up to 50% and improve the surgical resection rate. Some scholars also reported that GnRH-a can be used to treat residual IVL and reduce the risk of recurrence (12, 13).
For IVL patients, preserving of the uterus and ovary, unclean lesion resection, application of estrogen drugs, lesion infiltration into parauterine vessels, or distant invasion can increase the recurrence rate. The treatment of IVL should focus on surgery and remove the lesions as much as possible. The preferred surgical method is total hysterectomy with bilateral salpingo-oophorectomy + extrauterine lesion resection. For young patients, to preserve reproductive function, the IVL tumors should be removed completely as much as possible, and GnRH-a drugs should be supplemented for follow-up treatment to reduce the risk of recurrence.
In conclusion, although IVL is sporadic, there are still many cases reported in recent years. Because of its sporadicity, it is difficult to arouse the vigilance of gynecologists, and routine gynecological preoperative ultrasound is difficult to make a clear diagnosis from, which often leads to inadequate preoperative preparation, wrong selection of operation methods, passive treatment during operation, and lesions being easily missed. Our cases suggest that clinical gynecologists should be vigilant and not only rely on routine ultrasound to assist in diagnosis and treatment. If the veins in broad ligament, parauterine tissue, or adnexal area are found to be cord-like or Flammulina velutipes-like changes during operation, the disease should be considered, the blood vessels in the operation field should be fully explored, and the lesions should be completely and fully removed as much as possible. GnRH-a drugs or other anti-estrogen drugs can be used after operation to reduce the risk of recurrence. Regular reexamination and close follow-up are needed after operation.
Author Contributions
XL is the first author. Y-SJ is the corresponding author. XL drafted the manuscript. N-YM collected the patients’ clinical data. YZ contributed to analyzing and interpreting the imagine findings. Y-SJ gave the patients’ operation and reviewed the literature. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lee S, Kim DK, Narm KS, Cho SH. Pulmonary Artery Embolization of Intravenous Leiomyomatosis Extending Into the Right Atrium. Korean J Thorac Cardiovasc Surg (2011) 44(3):243–6. doi: 10.5090/kjtcs.2011.44.3.243
2. Thian YL, Tan KH, Kwek JW, Wang J, Chern B, Yam KL. Leiomyomatosis Peritonealis Disseminata and Subcutaneous Myoma–A Rare Complication of Laparoscopic Myomectomy. Abdom Imaging (2009) 34(2):235–8. doi: 10.1007/s00261-008-9379-5
3. Lee HJ, Choi J, Kim KR. Pulmonary Benign Metastasizing Leiomyoma Associated With Intravenous Leiomyomatosis of the Uterus: Clinical Behavior and Genomic Changes Supporting a Transportation Theory. Int J Gynecol Pathol (2008) 27(3):340–5. doi: 10.1097/PGP.0b013e3181656dab
4. Lee E, LaBounty T, Romano M, Agarwal PP. Case of the Season: Intravenous Leiomyomatosis: A Rare Cause of Intracardiac Mass. Semin Roentgenol (2020) 55(3):226–9. doi: 10.1053/j.ro.2020.06.009
5. Ramesh P, Annapureddy SR, Khan F, Sutaria PD. Angioleiomyoma: A Clinical, Pathological and Radiological Review. Int J Clin Pract (2004) 58(6):587–91. doi: 10.1111/j.1368-5031.2004.00085.x
6. Li B, Chen X, Chu YD, Li RY, Li WD, Ni YM. Intracardiac Leiomyomatosis: A Comprehensive Analysis of 194 Cases. Interact Cardiovasc Thorac Surg (2013) 17(1):132–8. doi: 10.1093/icvts/ivt117
7. Wang J, Yang J, Huang H, Li Y, Miao Q, Lu X, et al. Management of Intravenous Leiomyomatosis With Intracaval and Intracardiac Extension. Obstet Gynecol (2012) 120(6):1400–6. doi: 10.1097/aog.0b013e31826ebb90
8. Kokawa K, Yamoto M, Yata C, Mabuchi Y, Umesaki N. Postmenopausal Intravenous Leiomyomatosis With High Levels of Estradiol and Estrogen Receptor. Obstet Gynecol (2002) 100(5 Pt 2):1124–6. doi: 10.1016/s0029-7844(02)02194-4
9. Akinseye OA, Nayyar M, Das P. Uterine Intravenous Leiomyomatosis With Femoral Vein, Intracaval, Intracardiac and Pulmonary Artery Extension. Future Cardiol (2020) 16(1):27–32. doi: 10.2217/fca-2019-0002
10. Bodner K, Bodner-Adler B, Wierrani F, Mayerhofer K, Grunberger W. Intravenous Leiomyomatosis of the Uterus. Anticancer Res (2002) 22(3):1881–3. doi: 10.1016/S0950-821X(05)80163-X
11. Nishizawa J, Matsumoto M, Sugita T, Matsuyama K, Tokuda Y, Yoshida K, et al. Intravenous Leiomyomatosis Extending Into the Right Ventricle Associated With Pulmonary Metastasis and Extensive Arteriovenous Fistula. J Am Coll Surg (2004) 198(5):842–3. doi: 10.1016/j.jamcollsurg.2003.06.009
12. Doyle MP, Li A, Villanueva CI, Peeceeyen SC, Cooper MG, Hanel KC, et al. Treatment of Intravenous Leiomyomatosis With Cardiac Extension Following Incomplete Resection. Int J Vasc Med (2015) 2015:756141. doi: 10.1155/2015/756141
Keywords: intravascular leiomyomatosis (IVL), misdiagnosis, recurrence, treatment, operation
Citation: Li X, Ma N-Y, Zhang Y and Jiao Y-S (2022) Gynecologists Need to Be Vigilant—Two Case Reports of Intravascular Leiomyomatosis and Literature Review. Front. Oncol. 12:840096. doi: 10.3389/fonc.2022.840096
Received: 20 December 2021; Accepted: 14 January 2022;
Published: 07 February 2022.
Edited by:
Andrea Tinelli, Moscow Institute of Physics and Technology, RussiaReviewed by:
Huri Güvey, Private PARKHAYAT Hospital, TurkeySafak Hatirnaz, Medicana Hospital, Turkey
Banuhan Şahin, Amasya University, Turkey
Kosmas P. Ioannis, General Hospital of Ioannina G. Hatzikosta, Greece
Copyright © 2022 Li, Ma, Zhang and Jiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi-Sheng Jiao, jiaoys9827@126.com
 Xiang Li
Xiang Li Ning-Ye Ma
Ning-Ye Ma Yao Zhang
Yao Zhang Yi-Sheng Jiao
Yi-Sheng Jiao