- 1Epidemiology and Biostatistics Unit, INRS-Institut Armand-Frappier, Institut National de la Recherche Scientifique (INRS), University of Quebec, Laval, QC, Canada
- 2School of Public Health, Department of Social and Preventive Medicine, University of Montreal, Montreal, QC, Canada
- 3University of Montreal Hospital Research Center (CRCHUM), Montreal, QC, Canada
Background: Evidence is lacking regarding the potential role of chronic psychological stress on cancer incidence. The workplace is reported to be the main source of stress among Canadian men. We examined the association between perceived lifetime workplace stress and prostate cancer (PCa) risk in a large case–control study.
Methods: Cases were 1,933 men, aged ≤ 75 years, newly diagnosed with PCa in 2005–2009 across hospitals in Montreal, Canada. Concurrently, 1994 population controls frequency-matched on age were randomly selected from the electoral list based on cases’ residential districts. Detailed lifestyle and work histories (including perceived stress, from any type of work stressor, for each job held) were collected during in-person interviews. Logistic regression was used to estimate odds ratios (OR) and 95% confidence intervals (CI) for the association between work-related stress and PCa risk in multivariate analyses.
Results: Over the lifetime, 58% of subjects reported at least one job as stressful. Occupations described as stressful were most often among white-collar workers. Perceived workplace stress duration was associated with a higher risk of PCa (OR = 1.12, 95% CI:1.04–1.20 per 10-year increase) among men younger than 65 years, but not among older men. Associations were similar irrespective of PCa aggressiveness. Frequent or recent screening for PCa, age at first exposure and time since exposure to work-related stress, and socioeconomic and lifestyle factors, had little influence on risk estimates.
Conclusion: Findings are in line with an association between reporting prolonged workplace stress and an increase in risk of PCa before age 65.
Introduction
Chronic psychological stress has been found to have a deleterious impact on health, increasing the risk of cardiovascular disease (1), hypertension (2), mental illness (3), and diabetes (4). Its role in cancer etiology is of growing interest and was earmarked as a high-priority exposure for review by the International Agency for Research on Cancer (5). Chronic stress may have an impact on cancer development via the activation of the sympathetic nervous system and the hypothalamic–pituitary–adrenal axis (6). Most studies to date have been conducted on breast cancer risk (7–9); only four focused on prostate cancer (PCa) risk (10–13). Few of them assessed chronic stress at work. The workplace is the main source of stress among Canadian workers, particularly in men (14). Previous studies have most often assessed work-related stress using the Karasek model focusing on job strain, defined as an imbalance between high demand and low control (15). However, this objective measure may not correspond to the perception of stress by the subject and does not account for sources of stress other than job strain in the workplace. It has been advanced that the perception of threat from stressors may in fact be key in determining the behavioral and physiologic responses to stress (6, 16, 17).
A major issue to previous studies is that their assessment of stress was most often limited to one (usually at study baseline) or two time point(s), thereby rarely capturing changes in stress level over the entire career. We present here findings on the association between perceived stress, from any type of job stressor and over the entire work history, and PCa risk.
Materials and Methods
Study Population
The Prostate Cancer & Environment Study (PROtEuS) is a population-based case–control study conducted in Montreal, Canada, to assess the role of environmental factors in the development of PCa. In brief, eligible subjects were men, younger than 76 years of age at the time of diagnosis or selection, residents of the greater Montreal area, registered on Quebec’s permanent electoral list. In order to comply with institutional regulations and insure comprehensive population coverage at recruitment, the study base was restricted to men who referred or would be expected to refer to a French hospital for a PCa diagnosis. This represents the vast majority of Montreal residents as according to census data, French was the language used at home by 76% of Montrealers in 2006.
Cases were all patients newly diagnosed with primary histologically confirmed PCa, actively ascertained through pathology departments across French hospitals which diagnose and treat PCa in the Montreal area between 2005 and 2009. This covered over 80% of all PCa cases diagnosed in the region of Montreal during the study period according to registry information. There are no specific reference hospitals for PCa in Montreal. Concurrently to case recruitment, controls were randomly selected from the electoral list of French-speaking men residing in the same districts as cases and frequency matched to cases by 5-year age groups. For 3% of cases and 4% of controls, interviews were conducted with a proxy, usually the spouse.
Study participants (1,933 cases and 1,994 controls) represented 79% of eligible cases and 56% of eligible controls.
This study was approved by the Ethics Committees of the following institutions: Institut national de la recherche scientifique, Centre de Recherche du Centre Hospitalier de l’Université de Montréal, Hôpital Maisonneuve-Rosemont, Hôpital Jean-Talon, Hôpital Fleury, and Hôpital Charles-LeMoyne. The study was carried out in compliance with their recommendations. All subjects provided written informed consent in accordance with the Declaration of Helsinki.
Data Collection
During face-to-face interviews, subjects provided information on socio-demographic characteristics, lifestyle (including smoking habits, alcohol consumption, and dietary habits) and medical history (including depression and treatment with medication, family history of cancer, and PCa screening). A detailed occupational history, including workplace physical activity and perceived stress at work, was collected.
Job categories were defined according to the Canadian Classification and Dictionary of Occupations. We used socioeconomic classifications of occupations from the Euro ESeC matrix (employment relation: employee/self-employed/employer; socioeconomic position: salariat/intermediate/working class) (18) and from Pineo et al. (“white-collar” jobs: professional and high-level managerial/semi-professional, technical and middle managerial/supervisors and foremen; “blue-collar” jobs: skilled workers and employees/semi-skilled workers and employees/unskilled workers and employees) (19). The degree of aggressiveness of PCa, defined by the Gleason score, was extracted from pathology reports.
Workplace Stress Assessment
A primary focus of the study was the assessment of occupational chemical exposures. Toward this, trained interviewers elicited detailed descriptions of each job held for at least 2 years over the lifetime, including tasks, equipment, and products used, work environment and conditions. This often required 1–2 h. Toward the end of questioning about each job, participants were asked “Did this job make you feel tense, anxious, or stressed out most of the time?” This question was used to define perceived workplace stress for a given job, based on a dichotomous response (yes/no).
Statistical Analyses
Analyses were restricted to participants who had completed the occupational questionnaire for at least one job. The distribution of stressful jobs was described according to job characteristics and occupational categories.
Unconditional logistic regression was used to assess the risk of PCa associated with perceived workplace stress, using men who had never experienced job stress as the reference. Odds ratios (ORs) for low-grade (Gleason scores <7 or [3 + 4]) and high-grade (Gleason scores > 7 or [4 + 3]) PCa (20) were estimated in polynomial logistic models, and their respective regression coefficients were compared using a Wald test.
Workplace stress was assessed based on the cumulative number of years in jobs reported as stressful over the lifetime. Work stress duration was entered in the model as a quantitative variable (after confirming linearity of the logit of PCa risk) or categorized as follows: 0, ]0–15], ]15–30], and >30 years, whereas exposed categories were approximate tertiles of the distribution among controls in the main analyses.
Two regression models were built, the first adjusting for age only (in years, continuous), the second also including other factors known or suspected to be associated with PCa diagnosis: ancestry (European/Sub-Saharan/Asian/Greater Middle East/Other/Do not know), first-degree family history of PCa (Yes/No/Do not know), family income (<$C30,000/$C30,000–79,999/$C80,000 and more/Preferred not to respond/Do not know), education (Primary or secondary/College or university), marital status (Married or common law/Separated or divorced/Single/Widower), body mass index (kg/m2, continuous), type 2 diabetes (Yes/No), depression treated with medication (Yes/No), alcohol consumption (drink-years), smoking (pack-years), physical activity at work (in Metabolic equivalents—hours/day), and dietary habits (frequency of fruit and vegetable intake). There were no missing data for age, family history of PCa, type 2 diabetes, and depression treated with medication. For other variables, the numbers of missing data were as follows (numbers in parentheses): family income (2), education (7), marital status (1), physical activity at work (3), BMI (23), alcohol consumption (118), smoking (30), and frequency of fruit and vegetable intake (46). Terms indicating missing data for each covariate were entered in the models. Effect of additional adjustment for PCa screening frequency [≥ 5 prostatic specific antigen (PSA) tests and/or digital rectal exam (DRE) tests during the previous 5 years: Yes/No] was examined.
Different analyses were carried out to evaluate whether the timing of exposure to stress had an influence on PCa risk. We investigated if the association between work-related stress duration and PCa risk differed according to age at first stress experience. We also examined if this association was impacted by the time elapsed (</≥5 years) between the last stress exposure and the index (diagnosis/interview) date. In addition, we applied a lag time of 5 years preceding the index date to take into consideration a possible latency of effect. We also tested whether the occupational socioeconomic class (White-collar/Blue-collar workers), age (</≥ age 65) or retirement at index date modified the association between workplace stress and PCa. Indeed, age and occupational classes have been suggested to modulate the relationship between job stress and well-being (21) or cardiovascular diseases (22, 23). Effect modification was examined considering either the P-value of the likelihood ratio test comparing models before and after inclusion of product interaction terms, or the P-value for any of the individual product terms.
Sensitivity analyses were performed restricting to subjects with available information on workplace stress for each job or to subjects screened for PCa (PSA or DRE) within 2 years of the index date. We also performed analyses stratified according to any experience of night work, defined as at least one job including three working hours between midnight and 5 a.m. Finally, we examined if restricting analyses to self-respondents or to subjects without treatment for depression had an impact on the results.
All analyses were performed using SAS software (9.3; SAS Institute Inc., Cary, NC, USA).
Results
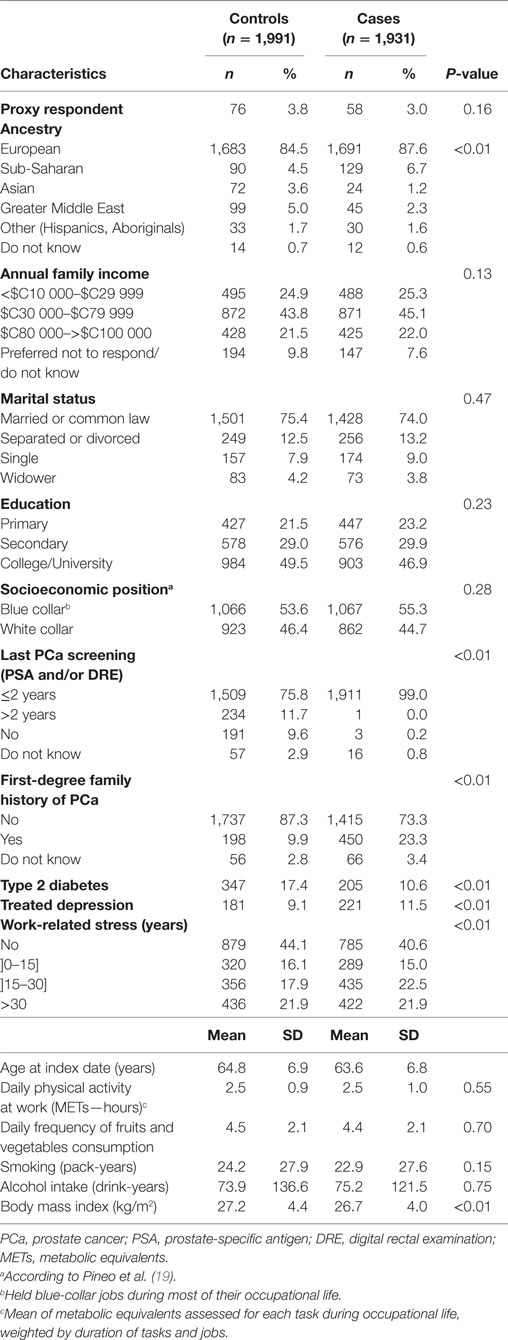
The study population for analyses comprised 1,931 cases (including 538 high-grade PCa) and 1,991 controls. Compared to subjects included in the analyses, the 202 subjects who were excluded because of incomplete occupational questionnaires were older (66.0 vs 64.1 years), more often proxy respondents (9.4 vs 3.1%), less educated (37.2 vs 48.8% with a post-secondary level), had a lower family income (33.0 vs 24.6% with an income <$C30 000) and reported higher levels of daily physical activity at work (2.7 vs 2.5 METS-hours). They were comparable according to other characteristics. Cases were slightly younger (64 vs 65 years, on average) and less educated than controls (Table 1). As expected, cases were more likely than controls to have a family history of PCa, to be of Sub-Saharan ancestry and to have been screened for PCa in the last 2 years. They were less likely to be of Greater Middle East or Asian ancestry. Annual family income, marital status, and socioeconomic class of occupations (Professional/Non-professional) did not differ according to case–control status. Cases and controls were similar in terms of workplace physical activity, fruit and vegetable consumption, smoking habits, and alcohol consumption. Average BMI was slightly lower and type 2 diabetes less frequent among cases.
On average, cases and controls had held 4.9 (SD: 2.6, range: 1–20) and 5.2 (SD: 2.7, range: 1–24) jobs over their lifetime, respectively. Subjects reporting at least one job as stressful represented 59.4% of cases (N = 1,146) and 55.8% of controls (N = 1,112). Perceived stress was less frequently reported by proxy respondents (50.0%). Overall, the mean cumulative duration of stressful jobs was of 24.8 (SD: 12.4) years. Subjects ever stressed by their job tended to be younger and more frequently treated for depression (data not shown). They were also more likely to be employed in white-collar occupations (52.0 vs 36.9% among never exposed), to have a higher annual family income and education, and lower levels of physical activity at work, and of tobacco and alcohol consumption (data not shown).
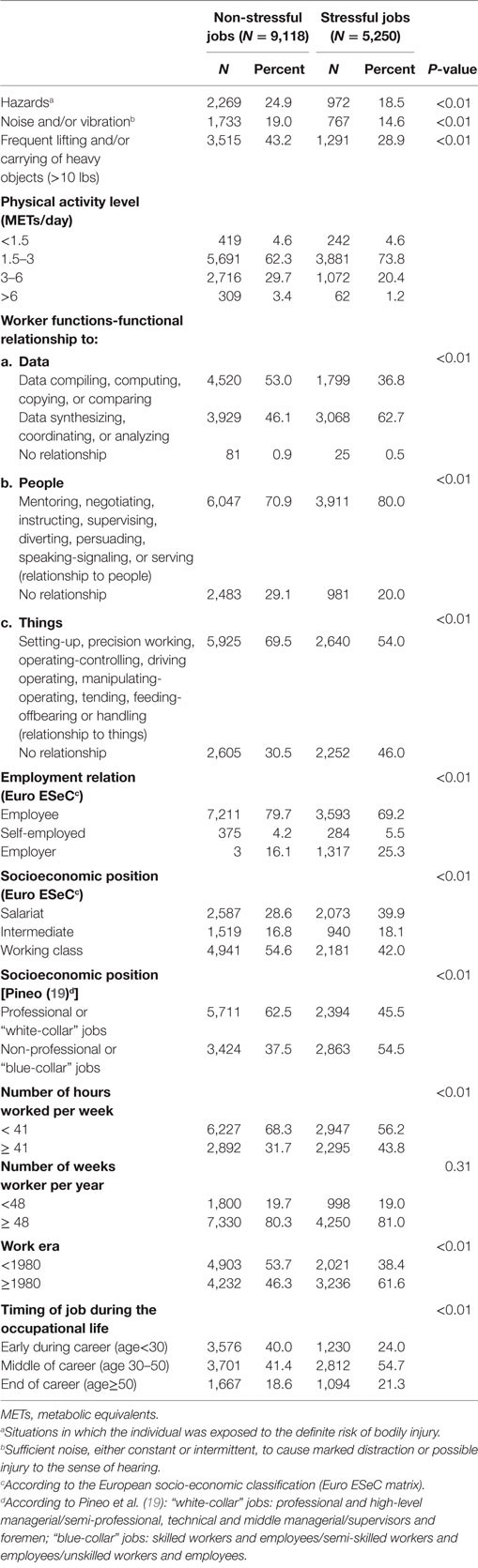
When comparing non-stressful jobs to stressful ones (Table 2), the latter were characterized by less exposure to hazards or noise/vibration, less physical or manual activities, increased socioeconomic position, and increased number of hours worked per week. Stressful jobs occurred more recently (≥1980), and more often in the middle of the career (at ages 30–50 years).
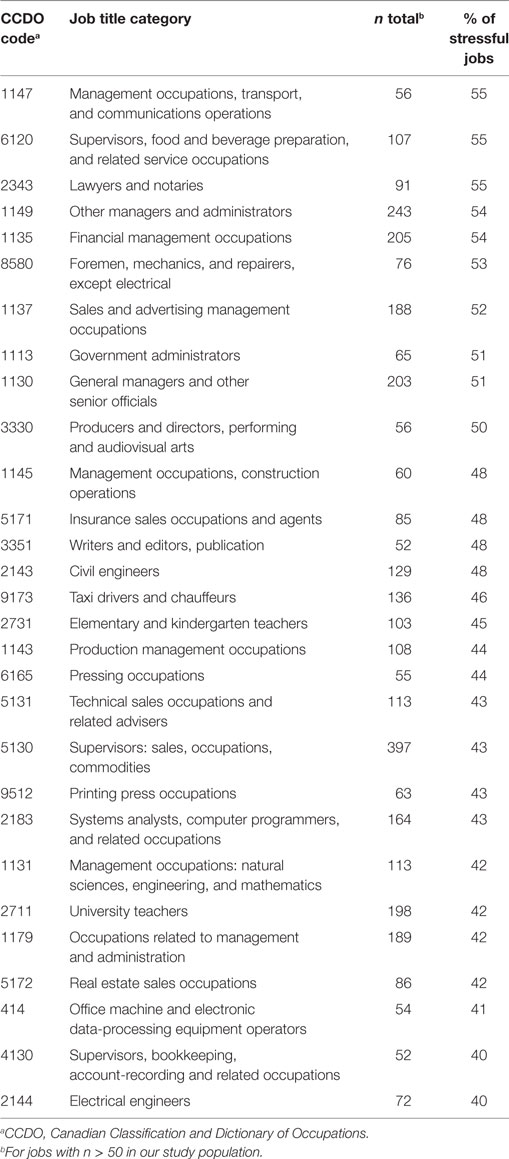
The job categories with the greater proportions of stressful jobs (55% of all jobs within a category) were Management occupations, transport and communications operations; Supervisors, food and beverage preparation and related service occupations, and; Lawyers and notaries (Table 3).
As there appeared to be some interaction between workplace stress duration (categorical variable) and age at index date (</≥ age 65, p = 0.06), the remaining sets of results were stratified by age.
Among subjects aged 65 or more, PCa risk was not associated with perceived workplace stress duration (Table 4). By contrast, among subjects younger than age 65, a dose–response trend was observed between PCa risk and stress duration categories (P trend <0.01, Table 5). PCa risk was elevated among younger men reporting more than 30 years of workplace stress; risk increased linearly with workplace stress duration (OR = 1.12, 95% CI: 1.04–1.20 per 10-year increment). Low-grade and high-grade PCa followed generally similar patterns of risk. Models adjusting for age only or for several potential socio-demographic and lifestyle confounders yielded similar risk estimates.
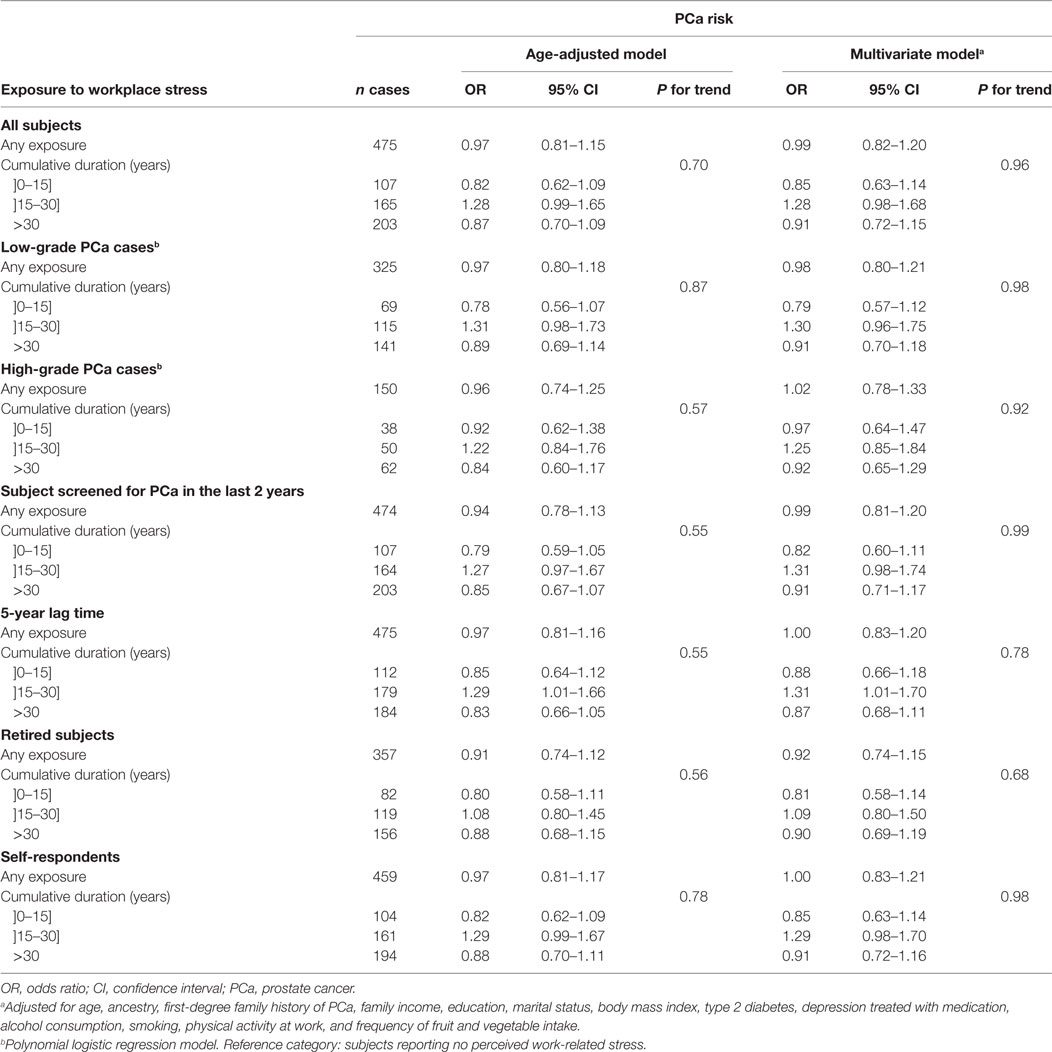
Table 4. OR for the risk of PCa associated with the duration of perceived workplace stress among subjects aged 65 or more at diagnosis or interview.
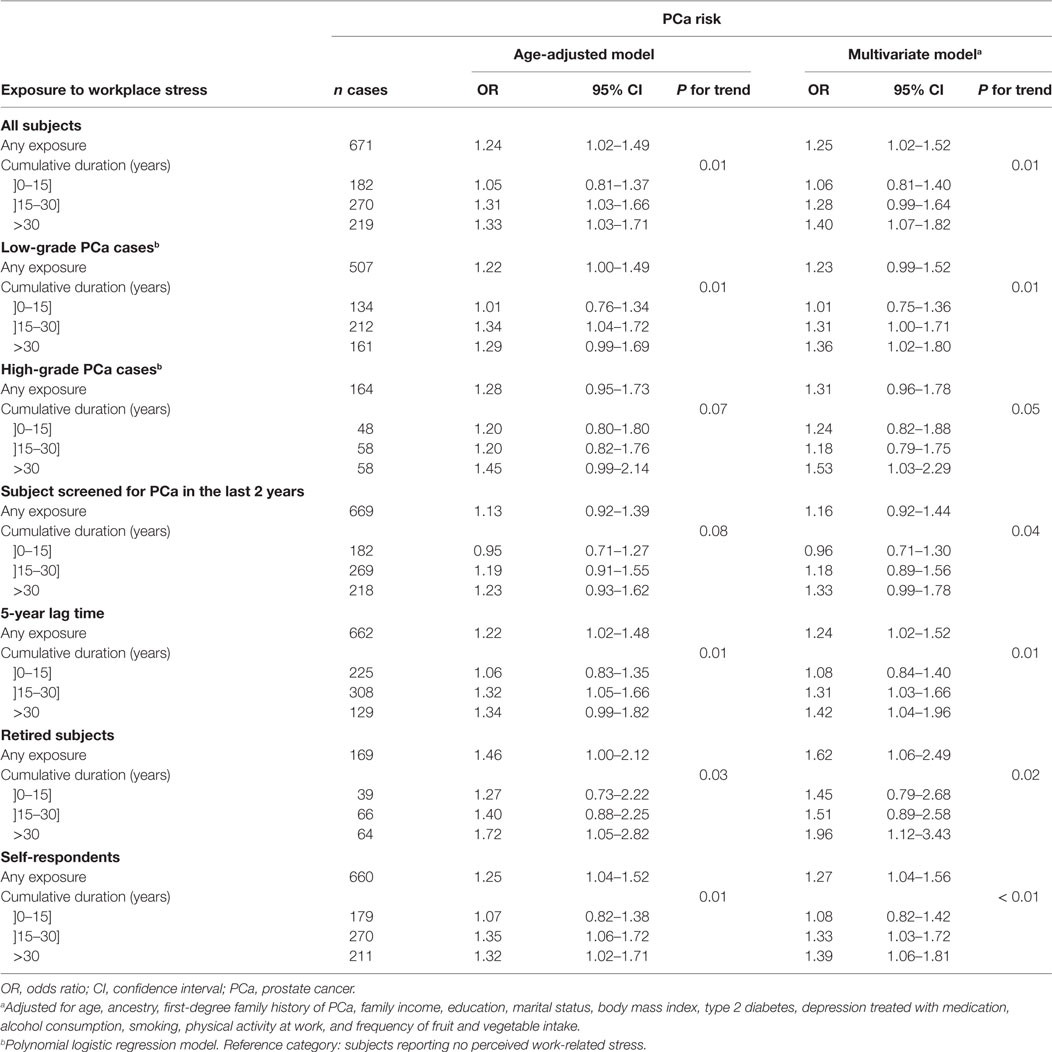
Table 5. Odds ratios (OR) for the risk of PCa associated with the duration of perceived workplace stress among subjects younger than age 65 at diagnosis or interview.
Odds ratios were largely unchanged in analyses restricted to subjects with no missing data on workplace stress (data not shown), to subjects recently screened for PCa or to retired subjects (Tables 4 and 5). Results were unchanged when excluding proxy respondents, representing less than 4% of subjects, or subjects treated for depression. Applying a 5-year lag time did not affect the results. Age at first exposure, delay since last exposure (</≥5 years), ever experience of night work and occupational socioeconomic class did not modify the association between perceived workplace stress and PCa (data not shown). When the threshold to stratify analyses on age was moved from 65 to 60 years, the association with workplace stress duration was slightly more pronounced among younger subjects.
Discussion
Main Results
Perceived workplace stress duration was associated with higher risk of PCa (high- and low-grade cancers) among men less than 65 years of age, but not among older men. Occupations described as stressful were most often among white-collar workers. The timing of exposure to stress at work (age at exposure, time between exposure and index date) did not influence risk estimates. Adjustment for socio-demographic and lifestyle factors had a marginal impact on findings.
Comparisons with the Literature
According to Cancer Type
A number of studies have reported an association between stressful life events and breast cancer, with the overall evidence judged as unconvincing (24, 25). Work-related stress was also mostly studied in relation to risk of breast cancer, with conflicting results (7–9, 12, 26–28). However, hormonal response to stress (29, 30), work-related stress determinants (31), and the relative physiological (29) and psychological (32) impact of stressors from private and occupational life may differ between men and women (26, 29, 30). These findings justify the conduct of sex-specific studies of stress and health.
To our knowledge, only two studies analyzed PCa risk in relation to stress at work, where no association was observed. One was a meta-analysis of 12 European cohort studies (12). While the individual studies benefited from a detailed job strain assessment, it was conducted at baseline only (among subjects aged 17–70 years); job strain was infrequent, experienced by 9% of the 865 incident PCa cases. The other one was the Montreal Multisite Case-Control Cancer Study, using the same method as the current one to evaluate lifetime workplace perceived stress. This study was conducted in the early 1980s and was based on a small sample (400 PCa cases) (13).
According to Study Design
Case–control studies are more prone to recall bias. However, among studies investigating the relation between stress at work and cancer (any type), a similar proportion of studies observing a positive association was observed among case–control (3 out of 5) (26, 33–36) and cohort (3 out of 6) studies (7–9, 12, 27, 28).
According to Age
In our study, the relation between workplace stress duration and PCa risk was more pronounced among subjects less than 65 years of age. Two studies have focused on breast or colon cancer cases younger than age 65 at diagnosis, including one observing a positive association (7, 35). The absence of association among older subjects in our study may result from a non-differential recall bias (susceptible to become more pronounced with aging). Conversely, it might reflect a cohort effect, whereas stressors would differ depending on the era they occurred.
According to Workplace Stress Assessment
In previous studies focusing on cancer, work-related stress was assessed at only one or two time point(s), which hampered the investigation of the role of timing and duration of exposure. In view of recent arguments in favor of a reverse stressor–strain relationship (37) or of a role of age as a moderator (21), exploring the timing of the relation between work-related stress and cancer appears particularly pertinent. Our assessment of stress had the advantage of capturing changes in work stress over the entire career: 45% of subjects reported stress/non-stress or non-stress/stress sequences. Only 38.4% of exposed subjects reported having been stressed at work during more than 80% of their career. This suggests that a single stress measurement at baseline will result in substantial exposure misclassification and highlights the importance of measuring stress at multiple time points throughout the occupational life.
Stress at work has been mostly assessed in the past using the high demand-low control model developed by Karasek (15). Although it has been shown to be efficient in demonstrating a relation between chronic stress and cardiovascular (1, 2) or mental illness (3), this model might not capture cancer determinants of work-related stress. Our measure of workplace stress did not make assumptions about the stressors that could have an impact on cancer development. We found a greater proportion of white-collar workers among subjects ever stressed by their work. Our findings are in line with those of another study suggesting a role of job authority in the increased risk of breast cancer observed among higher-status occupations (9).
An advantage of measuring the individual’s perception of chronic stress is that it reflects subject susceptibility to stress health effects, whatever the stressor. Indeed the physiologic response to environmental stress depends on the individual’s perception of stress (6, 16). Only five studies assessed perceived stress in relation to cancer: three were based on the Copenhagen City Heart Study (10, 37, 38), two focused on PCa (10, 11), and one on breast cancer (26). None of them observed a positive association.
Strengths and Limitations
Selection Bias
Response rates could have affected results if socioeconomic characteristics associated with workplace stress influenced subjects’ participation. However, according to Canadian census tract data for 2006, the rates for recent immigration, unemployment, low educational level, and low household income were similar in living areas of participants and non-participants, both among cases and controls, indicating that selection bias is not of major concern in the study. Besides, a healthy worker effect is improbable since participants were not selected according to their employment status at index date.
Detection Bias
Misclassification of PCa status due to under-detection is a priori limited in the present study. Indeed, it was set in a population with free access to healthcare and which was relatively uniformly and regularly screened for PCa at the time of subjects’ ascertainment. However, subjects with a lower socioeconomic status tended to be less frequently screened. Since subjects having experienced stressful jobs were more likely to be white-collar workers, the positive association between workplace stress and PCa risk could be in part due to higher levels of screening behavior among these subjects. However, adjusting on socioeconomic factors or on screening frequency did not result in substantial changes. Furthermore, similar results were observed in the analysis restricted to subjects recently screened.
Recall Bias
Recall bias may be at play in a case–control study, with cases being more prone to report stress. In a previous study investigating perceptions about the causes of breast cancer, nearly half of the women with breast cancer attributed their condition to mental or emotional factors (especially stress), whereas less than 30% of control women reported these factors to be causal (38). Such widespread belief could set the grounds for over-reporting of stress exposure by cases. However, the present study presents a number of attributes that may mitigate recall bias. The study was set among men; whether they would tend to ascribe PCa to stress has not been documented. Moreover, the PROtEuS project, presented as a “Study of the Environmental Causes of Prostate Diseases,” did not focus on stress, which represented only one question in a 2-h in-person interview eliciting information on a very large number of lifestyle and occupational factors. As well, the numerous and detailed questions asked about each job may have helped the subject in remembering past work environments and their context, regardless of their present situation. Finally, since depression has been shown to be associated with work-related stress (3), we used the report of a diagnosis of depression as an indicator of workplace stress less likely to be affected by a recall bias. We observed similar positive associations between workplace stress and depression among cases (OR = 1.31, 95% CI 0.96–1.78) and controls (OR = 1.44, 95% CI 1.05–1.99), which does not support an over-reporting of workplace stress among cases.
Workplace Stress Assessment
Our assessment of stress was based on a crude line of questioning, aimed at identifying the perception of stress associated with each job. Neither the degree nor the reasons (stressors) of reported workplace stress were elicited in our study. Our assessment went beyond job strain and could reflect other factors, such as job insecurity, hazardous environments, etc. We could document that stress was most often encountered in white-collars jobs, yet expected to benefit from more job control. These results are consistent with those of a Canadian survey, where workers stressed mainly about work were well-educated and held white-collar jobs (14). Among Quebec workers, self-rated workplace stress was positively associated with high psychological demand, but negatively associated with low skill discretion (39). Besides, the efficiency of Karasek’s demand-control model in predicting job strain has been challenged by recent findings suggesting that job control can act as a stressor among individuals low in emotional stability (40).
While the validity of the information on self-reported stress could not be verified, the interview-based job histories have been shown to be valid (41). The questionnaire used to obtain detailed work histories has been used extensively, notably in studies of lung, colon, and several other cancer types (42–46).
The detailed occupational history, including the question on perceived stress, was collected only for jobs held for 2 years and more, to keep interviews within a reasonable timeframe. However, this had a minimal impact as jobs lasting less than 2 years represented <4% of the overall career coverage in this population. Information about work stress was available for a subset of 24 jobs held for less than 2 years, allowing for some sensitivity analyses. Only four (16%) of these short jobs were reported to be stressful, representing a lower proportion than observed among longer jobs (36%). Besides, we found similar results in analyses restricted to subjects who never held a job lasting less than 2 years.
While unemployment or non-working time in other circumstances (subject was retired, sick or unavailable, homemaker, student, prisoner, refugee, or volunteer) could have been sources of stress related to work, these were not considered in the analyses as information about stress was only elicited for paid jobs. Perceived stress in at least one job was not associated with time since retirement.
Other Sources of Stress and Coping
We did not collect other sources of stress that may contribute to general day-to-day stress. Yet work is reported to be the main source of stress of daily life in Canadians, particularly among men, far ahead of financial concerns, lack of time, family matters, personal, and other issues (14). We did not account for personality characteristics and social support that may influence the way subjects cope with perceived stress, buffering adverse health effects of chronic stress (47). In a case–control study, high-effort coping was associated with increased PCa risk (11). Although modifying the relation between coping and PCa risk, neither social support nor perceived stress alone was associated with PCa risk in this study (11). Coping strategies may also be related to health seeking behaviors (i.e., attendance of screening examinations) and then to cancer diagnosis (48). We can hypothesize that personal characteristics such as anxiety could influence both stress perception and screening behavior. This could explain the association between workplace stress duration and PCa risk observed among men younger than age 65 but not among older men for whom screening for PCa is more common. However, whatever the age group considered, screening in the last 2 years was not associated with workplace stress duration among controls (adjusted on age, data not shown). Besides, including PCa screening frequency in multivariate models did not change substantially the results.
Other Methodological Issues
Another substantial strength of this study was its ability to take into account the potential confounding or effect modification by socioeconomic lifestyle and medical factors, albeit none, other than age, had a sizeable impact on findings. In the Danish Nurse Cohort, an interaction was observed between working nightshifts and job control on the association with hormone-related cancer risk in women (28). We did not observe an effect modification by night work when examining workplace stress in relation to PCa risk in our study.
Finally, this study is the largest to date to investigate the role of work-related stress in PCa risk and to consider PCa aggressiveness.
Possible Biological Pathways
Stress leads to the activation of the sympathetic nervous systems and the hypothalamic–pituitary–adrenal axis, inducing secretion of catecholamines and glucocorticoids (6). Persistent activation of these neuroendocrine pathways can downregulate various functions of the cellular immune response, by decreasing activities of mediators involved in immune surveillance of tumors or by promoting genomic instability (49, 50). As well, cortisol has been shown to stimulate the growth of androgen-independent PCa cells (51). Finally, the relation between chronic stress and testosterone levels observed in several studies (52, 53) suggests that stress-induced hormones could contribute to PCa development.
Conclusion
Unlike ours, previous studies did not observe an association between workplace stress and PCa. The inability of previous investigations to evaluate the role of exposure duration and to capture changes in stress levels over time, which were documented in the current study, could explain the divergent findings. Another issue is statistical power, as previous studies have included much fewer stress-exposed cases than ours. Our results suggest that perceived work-related stress may play a role in PCa development when experienced over a prolonged period. Stress was more often reported in white-collar jobs, and appeared to be essentially related to PCa risk diagnosed at a younger age.
Ethics Statement
This study was approved by the Ethics Committees of the following institutions: Institut national de la recherche scientifique, Centre de Recherche du Centre Hospitalier de l’Université de Montréal, Hôpital Maisonneuve-Rosemont, Hôpital Jean-Talon, Hôpital Fleury, and Hôpital Charles-LeMoyne. The study was carried out in accordance with their recommendations. All subjects gave written informed consent in accordance with the Declaration of Helsinki.
Author Contributions
AB-L conducted the data analysis and prepared the manuscript, M-EP led the conception, design and, data acquisition of the PROtEuS study. AB-L, M-CR, and M-EP contributed to the interpretation of the data and critical revision of the manuscript. All authors read and approved the final version to be published.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors wish to sincerely thank the entire Epidemiology and Biostatistics team at INRS-Institut Armand-Frappier for their contribution to the study. Additional thanks go to study participants and to the many urologists who provided access to their patients.
Funding
This study was supported financially through grants from the Canadian Cancer Society (grants no. 13149, 19500, 19864, 19865), the Cancer Research Society, the Fonds de Recherche du Québec - Santé (FRQS), FRQS—RRSE, and the Ministère du Développement économique, de l’Innovation et de l’Exportation du Québec. Marie-Élise Parent and Marie-Claude Rousseau held career awards from the FRQS and the Canadian Institutes of Health Research.
Abbreviations
PCa, prostate cancer; OR, odds ratio; IARC, International Agency for Research on Cancer; PROtEuS, Prostate Cancer & Environment Study; CCDO, Canadian Classification and Dictionary of Occupations; PSA, prostatic specific antigen; DRE, digital rectal exam.
References
1. Backé E-M, Seidler A, Latza U, Rossnagel K, Schumann B. The role of psychosocial stress at work for the development of cardiovascular diseases: a systematic review. Int Arch Occup Environ Health (2012) 85:67–79. doi:10.1007/s00420-011-0643-6
2. Babu GR, Jotheeswaran AT, Mahapatra T, Mahapatra S, Kumar A, Detels R, et al. Is hypertension associated with job strain? A meta-analysis of observational studies. Postgrad Med J (2014) 90:402–9. doi:10.1136/postgradmedj-2013-101396rep
3. Stansfeld S, Candy B. Psychosocial work environment and mental health – a meta-analytic review. Scand J Work Environ Health (2006) 32:443–62. doi:10.5271/sjweh.1050
4. Nyberg ST, Fransson EI, Heikkilä K, Ahola K, Alfredsson L, Bjorner JB, et al. Job strain as a risk factor for type 2 diabetes: a pooled analysis of 124,808 men and women. Diabetes Care (2014) 37:2268–75. doi:10.2337/dc13-2936
5. International Agency for Research on Cancer. Report of the Advisory Group to Recommend Priorities for IARC Monographs during 2010–2014. Lyon, France: World Health Organisation, International Agency for Research on Cancer (2008).
6. McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med (1998) 338:171–9. doi:10.1056/NEJM199801153380307
7. Kuper H, Yang L, Theorell T, Weiderpass E. Job strain and risk of breast cancer. Epidemiology (2007) 18:764–8. doi:10.1097/EDE.0b013e318142c534
8. Schernhammer ES, Hankinson SE, Rosner B, Kroenke CH, Willett WC, Colditz GA, et al. Job stress and breast cancer risk: the nurses’ health study. Am J Epidemiol (2004) 160:1079–86. doi:10.1093/aje/kwh327
9. Pudrovska T, Carr D, McFarland M, Collins C. Higher-status occupations and breast cancer: a life-course stress approach. Soc Sci Med (2013) 89:53–61. doi:10.1016/j.socscimed.2013.04.013
10. Nielsen NR, Kristensen TS, Zhang Z-F, Strandberg-Larsen K, Schnohr P, Grønbaek M. Sociodemographic status, stress, and risk of prostate cancer. A prospective cohort study. Ann Epidemiol (2007) 17:498–502. doi:10.1016/j.annepidem.2007.02.001
11. Coker AL, Sanderson M, Ellison GL, Fadden MK. Stress, coping, social support, and prostate cancer risk among older African American and Caucasian men. Ethn Dis (2006) 16:978–87.
12. Heikkilä K, Nyberg ST, Theorell T, Fransson EI, Alfredsson L, Bjorner JB, et al. Work stress and risk of cancer: meta-analysis of 5700 incident cancer events in 116,000 European men and women. BMJ (2013) 346:f165. doi:10.1136/bmj.f165
13. Blanc-Lapierre A, Rousseau M-C, Weiss D, El-Zein M, Siemiatycki J, Parent M-É. Lifetime report of perceived stress at work and cancer among men: a case-control study in Montreal, Canada. Prev Med (2017) 96:28–35. doi:10.1016/j.ypmed.2016.12.004
14. Crompton S. What’s Stressing the Stressed? Main Sources of Stress among Workers. Statistics Canada (2011). Available from: http://www.statcan.gc.ca/pub/11-008-x/2011002/article/11562-eng.htm
15. Karasek R, Theorell T. Healthy Work: Stress, Productivity and the Reconstruction of Working Life. New York, NY: Basic Books Inc. Publishers (1990).
17. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav (1983) 24:385–96. doi:10.2307/2136404
18. EuroESeC Matrix (Appendix 5). (2006). Available from: https://www.iser.essex.ac.uk/files/esec/guide/docs/Appendix5.xls
19. Pineo P, Porter J, McRoberts HG. The 1971 census and the socioeconomic classification of occupations. Can Rev Sociol (1977) 14:91–102. doi:10.1111/j.1755-618X.1977.tb00333.x
20. Wright JL, Salinas CA, Lin DW, Kolb S, Koopmeiners J, Feng Z, et al. Prostate cancer specific mortality and Gleason 7 disease differences in prostate cancer outcomes between cases with Gleason 4 + 3 and Gleason 3 + 4 tumors in a population based cohort. J Urol (2009) 182:2702–7. doi:10.1016/j.juro.2009.08.026
21. Mauno S, Ruokolainen M, Kinnunen U. Does aging make employees more resilient to job stress? Age as a moderator in the job stressor-well-being relationship in three Finnish occupational samples. Aging Ment Health (2013) 17:411–22. doi:10.1080/13607863.2012.747077
22. Ferrario MM, Veronesi G, Bertù L, Grassi G, Cesana G. Job strain and the incidence of coronary heart diseases: does the association differ among occupational classes? A contribution from a pooled analysis of Northern Italian cohorts. BMJ Open (2017) 7:e014119. doi:10.1136/bmjopen-2016-014119
23. Tsutsumi A, Kayaba K, Ishikawa S. Impact of occupational stress on stroke across occupational classes and genders. Soc Sci Med (2011) 72:1652–8. doi:10.1016/j.socscimed.2011.03.026
24. Santos MC, Horta BL, Amaral JJ, Fernandes PF, Galvão CM, Fernandes AF. Association between stress and breast cancer in women: a meta-analysis. Cad Saude Publica (2009) 25(Suppl 3):S453–63. doi:10.1590/S0102-311X2009001500010
25. Schoemaker MJ, Jones ME, Wright LB, Griffin J, McFadden E, Ashworth A, et al. Psychological stress, adverse life events and breast cancer incidence: a cohort investigation in 106,000 women in the United Kingdom. Breast Cancer Res (2016) 18:72. doi:10.1186/s13058-016-0733-1
26. Kruk J, Aboul-Enein HY. Psychological stress and the risk of breast cancer: a case-control study. Cancer Detect Prev (2004) 28:399–408. doi:10.1016/j.cdp.2004.07.009
27. Achat H, Kawachi I, Byrne C, Hankinson S, Colditz G. A prospective study of job strain and risk of breast cancer. Int J Epidemiol (2000) 29:622–8. doi:10.1093/ije/29.4.622
28. Vesterlund GK, Høeg BL, Johansen C, Heitmann BL, E Bidstrup P. Prolonged job strain and subsequent risk of cancer in women – a longitudinal study, based on the Danish Nurse Cohort. Acta Oncol (2017) 56:301–6. doi:10.1080/0284186X.2016.1267399
29. Lundberg U. Stress hormones in health and illness: the roles of work and gender. Psychoneuroendocrinology (2005) 30:1017–21. doi:10.1016/j.psyneuen.2005.03.014
30. Goel N, Workman JL, Lee TT, Innala L, Viau V. Sex differences in the HPA axis. Compr Physiol (2014) 4:1121–55. doi:10.1002/cphy.c130054
31. Herrero SG, Saldaña MÁ, Rodriguez JG, Ritzel DO. Influence of task demands on occupational stress: gender differences. J Safety Res (2012) 43:365–74. doi:10.1016/j.jsr.2012.10.005
33. Jansson C, Johansson ALV, Jeding K, Dickman PW, Nyrén O, Lagergren J. Psychosocial working conditions and the risk of esophageal and gastric cardia cancers. Eur J Epidemiol (2004) 19:631–41. doi:10.1023/B:EJEP.0000036806.51918.40
34. Jansson C, Jeding K, Lagergren J. Job strain and risk of esophageal and cardia cancers. Cancer Epidemiol (2009) 33:473–5. doi:10.1016/j.canep.2009.10.008
35. Courtney JG, Longnecker MP, Peters RK. Psychosocial aspects of work and the risk of colon cancer. Epidemiology (1996) 7:175–81. doi:10.1097/00001648-199603000-00012
36. Spiegelman D, Wegman DH. Occupation-related risks for colorectal cancer. J Natl Cancer Inst (1985) 75:813–21. doi:10.1093/jnci/75.5.813
37. Tang K. A reciprocal interplay between psychosocial job stressors and worker well-being? A systematic review of the “reversed” effect. Scand J Work Environ Health (2014) 40:441–56. doi:10.5271/sjweh.3431
38. Thomson AK, Heyworth JS, Girschik J, Slevin T, Saunders C, Fritschi L. Beliefs and perceptions about the causes of breast cancer: a case-control study. BMC Res Notes (2014) 7:558. doi:10.1186/1756-0500-7-558
39. Institut de la statistique du Québec. Stress au travail et santé mentale chez les adultes Québécois. Québec (2008). Available from: http://sante.gouv.qc.ca
40. Rubino C, Perry SJ, Milam AC, Spitzmueller C, Zapf D. Demand-control-person: integrating the demand-control and conservation of resources models to test an expanded stressor-strain model. J Occup Health Psychol (2012) 17:456–72. doi:10.1037/a0029718
41. Baumgarten M, Siemiatycki J, Gibbs GW. Validity of work histories obtained by interview for epidemiologic purposes. Am J Epidemiol (1983) 118:583–91. doi:10.1093/oxfordjournals.aje.a113663
42. Gérin M, Siemiatycki J, Kemper H, Bégin M. Obtaining occupational exposure histories in epidemiologic case-control studies. J Occup Med (1985) 27:420–6.
43. Siemiatycki J, Richardson L, Gérin M, Goldberg M, Dewar R, Désy M, et al. Associations between several sites of cancer and nine organic dusts: results from an hypothesis-generating case-control study in Montreal, 1979–1983. Am J Epidemiol (1986) 123:235–49. doi:10.1093/oxfordjournals.aje.a114232
44. Parent ME, Rousseau MC, Boffetta P, Cohen A, Siemiatycki J. Exposure to diesel and gasoline engine emissions and the risk of lung cancer. Am J Epidemiol (2007) 165(1):53–62. doi:10.1093/aje/kwj343
45. Goldberg MS, Parent ME, Siemiatycki J, Désy M, Nadon L, Richardson L, et al. A case-control study of the relationship between the risk of colon cancer in men and exposures to occupational agents. Am J Ind Med (2001) 39(6):531–46. doi:10.1002/ajim.1052
46. Sauvé JF, Lavoué J, Parent ME. Occupation, industry, and the risk of prostate cancer: a case-control study in Montréal, Canada. Environ Health (2016) 15(1):100. doi:10.1186/s12940-016-0185-1
47. Adler N, Matthews K. Health psychology: why do some people get sick and some stay well? Annu Rev Psychol (1994) 45:229–59. doi:10.1146/annurev.ps.45.020194.001305
48. Svensson T, Inoue M, Sawada N, Charvat H, Iwasaki M, Sasazuki S, et al. Coping strategies and cancer incidence and mortality: the Japan Public Health Center-based prospective study. Cancer Epidemiol (2016) 40:126–33. doi:10.1016/j.canep.2015.12.003
49. Reiche EMV, Nunes SOV, Morimoto HK. Stress, depression, the immune system, and cancer. Lancet Oncol (2004) 5:617–25. doi:10.1016/S1470-2045(04)01597-9
50. Lutgendorf SK, Sood AK. Biobehavioral factors and cancer progression: physiological pathways and mechanisms. Psychosom Med (2011) 73:724–30. doi:10.1097/PSY.0b013e318235be76
51. Zhao XY, Malloy PJ, Krishnan AV, Swami S, Navone NM, Peehl DM, et al. Glucocorticoids can promote androgen-independent growth of prostate cancer cells through a mutated androgen receptor. Nat Med (2000) 6:703–6. doi:10.1038/76287
52. Theorell T, Karasek RA, Eneroth P. Job strain variations in relation to plasma testosterone fluctuations in working men – a longitudinal study. J Intern Med (1990) 227:31–6. doi:10.1111/j.1365-2796.1990.tb00115.x
Keywords: psychological stress, workplace, prostate cancer, case–control study, occupational health
Citation: Blanc-Lapierre A, Rousseau M-C and Parent M-E (2017) Perceived Workplace Stress Is Associated with an Increased Risk of Prostate Cancer before Age 65. Front. Oncol. 7:269. doi: 10.3389/fonc.2017.00269
Received: 04 July 2017; Accepted: 26 October 2017;
Published: 13 November 2017
Edited by:
Cristina Bosetti, Istituto Di Ricerche Farmacologiche Mario Negri, ItalyReviewed by:
Paulina Gomez-Rubio, Centro Nacional de Investigaciones Oncológicas CNIO—Fundación Cáncer FUCA, SpainYuan-Chin Amy Lee, University of Utah, United States
Copyright: © 2017 Blanc-Lapierre, Rousseau and Parent. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marie-Elise Parent, marie-elise.parent@iaf.inrs.ca
 Audrey Blanc-Lapierre
Audrey Blanc-Lapierre Marie-Claude Rousseau
Marie-Claude Rousseau Marie-Elise Parent
Marie-Elise Parent