Executive functions and borderline personality features in adolescents with major depressive disorder
- 1Department of Child and Adolescent Psychiatry and Psychotherapy, University Hospital of Psychiatry Zurich, University of Zurich, Zürich, Switzerland
- 2Psychiatric Hospital St. Gallen Nord, Wil, Switzerland
- 3Research Department of Child and Adolescent Psychiatry, Psychiatric University Hospitals Basel, University of Basel, Basel, Switzerland
- 4Child and Adolescent Psychiatric Services St. Gallen, St. Gallen, Switzerland
- 5Clienia Littenheid AG, Littenheid, Switzerland
- 6Child and Adolescent Psychiatry Klinik Sonnenhof, Ganterschwil, Switzerland
- 7Child and Adolescent Psychiatry Thurgau, Weinfelden, Switzerland
- 8Child and Adolescent Psychiatric Services Baselland, Basel, Switzerland
- 9University Clinic of the Martin-Luther University Halle – Wittenberg’s Medical Faculty, Halle, Germany
- 10Département de Psychiatrie, Hôpitaux Universitaires de Genève, Geneva, Switzerland
Background: Executive functions (EF) consolidate during adolescence and are impaired in various emerging psychiatric disorders, such as pediatric Major Depressive Disorder (pMDD) and Borderline Personality Disorder. Previous studies point to a marked heterogeneity of deficits in EF in pMDD. We examined the hypothesis that deficits in EF in adolescents with pMDD might be related to comorbid Borderline Personality features (BPF).
Methods: We examined a sample of 144 adolescents (15.86 ± 1.32) diagnosed with pMDD. Parents rated their child’s EF in everyday life with the Behavior Rating Inventory of Executive Function (BRIEF) and BPF with the Impulsivity and Emotion Dysregulation Scale (IED-27). The adolescents completed equivalent self-rating measures. Self- and parent-ratings of the BRIEF scores were compared with paired t-Tests. Correlation and parallel mediation analyses, ICC, and multiple regression analyses were used to assess symptom overlap, parent-child agreement, and the influence of depression severity.
Results: Over the whole sample, none of the self- or parent-rated BRIEF scales reached a mean score above T > 65, which would indicate clinically impaired functioning. Adolescents tended to report higher impairment in EF than their parents. Depression severity was the strongest predictor for BPF scores, with Emotional Control predicting parent-rated BPF and Inhibit predicting self-rated BPF. Furthermore, the Behavioral Regulation Index, which includes EF closely related to behavioral control, significantly mediated the relationship between depression severity and IED-27 factors emotional dysregulation and relationship difficulties but not non-suicidal self-injuries.
Conclusion: On average, adolescents with depression show only subtle deficits in executive functioning. However, increased EF deficits are associated with the occurrence of comorbid borderline personality features, contributing to a more severe overall psychopathology. Therefore, training of executive functioning might have a positive effect on psychosocial functioning in severely depressed adolescents, as it might also improve comorbid BPF.
Clinical trial registration: www.ClinicalTrials.gov, identifier NCT03167307.
Introduction
Adolescence as a period of transition is characterized by structural changes and a reorganization of brain functions, creating an imbalance between earlier maturing areas associated with the reward system and emotion processing and later maturing prefrontal areas associated with cognitive control (dual systems model) (Gogtay et al., 2004; Casey et al., 2008; Konrad et al., 2013; Luciana, 2013; Blackmore and Mills, 2014; Mills et al., 2015). Cognitive control is enabled by executive functions (EF), mainly in the prefrontal cortex (Diamond and Lee, 2011). EF include cognitive flexibility, inhibition (self-control and self-regulation), working memory, problem-solving, and planning (Miyake et al., 2000; Drechsler, 2007; Gürdere et al., 2023). An imbalance of these regulatory functions may lead to behaviors such as enhanced risk-taking or impulsive decision-making, often observed in teenagers. However, it may also increase the vulnerability to psychological distress, negative social environments, or peer adversity, which may in turn contribute to the development of psychopathology in this critical period of life (Luciana, 2016). Given that deficits in EF in adolescents have been described as a general risk marker for psychopathology, such as paediatric depression (Fenesy and Lee, 2019; Romer and Pizzagalli, 2021), the early identification of EF impairment is highly relevant for clinical practice, considering that in adolescents training can improve EF (Carr and Stewart, 2019; Pasqualotto et al., 2021).
Pediatric Major Depressive Disorder (pMDD) is among the most frequent psychopathological disorders in adolescents, with an estimated 12-month prevalence of 7.5% and a lifetime prevalence of 11% (Avenevoli et al., 2015; Polanczyk et al., 2015). Borderline Personality Features (BPF) and Borderline Personality Disorder (BPD) are frequent comorbidities of depression. More than half of the adolescents with a BPD diagnosis present a co-occurring pMDD diagnosis (Pham-Scottez, 2016). In adults, about half of the individuals with BPD meet the criteria for MDD, while 10–30% of individuals with MDD have co-occurring BPD (Rao and Broadbear, 2019). BPD is considered a disorder in its own right and not as a variant of either MDD or bipolar affective disorder (Beatson and Rao, 2012). Dysfunctional emotional regulation is a key feature (Chapman, 2019), other characteristics are inconsistent identity, and unstable interpersonal relations (Lieb et al., 2004; Bohus et al., 2021). According to DSM-5, at least five out of nine of the following features must be present for a diagnosis of BPD: fear of abandonment, unstable relationships, unstable self-image, impulsivity, self-harm, mood instability, feelings of emptiness, inappropriate anger, and dissociation/transient paranoid ideation (DSM-5 APA; see Bohus et al., 2021). For diagnosis in adolescence, symptoms need to persist for at least one year. In the past, personality disorders in adolescents have been underdiagnosed, as clinicians and researchers have been hesitant to apply the concept of personality disorders to children and adolescents in part to prevent pathologization and stigmatization (Kaess et al., 2020). At this point, there is sufficient evidence in favor of a BPD diagnosis in adolescents as it has major implications for treatment planning (Miller et al., 2008; Kaess et al., 2014). Prevalence estimates in adolescents vary between 1.4% (Johnson et al., 2008) and 6.3% (Guilé et al., 2021) in the population; but are much higher in clinical samples (11–50%; see Kaess et al., 2014).
Both BPD and pMDD have been explained using the biopsychosocial model, with a combination of genetic factors, personality traits, and adverse events during childhood as underlying factors (Lieb et al., 2004; Chapman, 2019). On a neuroanatomical level, BPD has been associated with volume reductions in the amygdala, the hippocampus, the orbitofrontal cortex (OFC), the frontal lobes, and the cingulate cortex in adults, and with OFC volume reduction in adolescents (Chanen et al., 2008). Particularly the amygdala has been associated with the regulation of negative affective stimuli, which is relevant for regulatory control (Soloff et al., 2017). fMRI studies have shown a hyper-arousal of the amygdala in patients with BPD, which lead to the projection of negative attributes onto neutral faces (Donegan et al., 2003). These processes of abnormal brain maturation may result in the characteristic features of BPD of emotional dysregulation and impulsivity in adolescents (Houston et al., 2005).
Executive functions in adolescent with pMDD and BPD
Performance deficits in EF have been observed both in pMDD and BPD. A meta-analysis by Wagner et al. (2015) based on 33 studies analysing cognitive functions in youth with depression provided evidence of EF deficits in the domains of inhibition, verbal fluency, working memory, cognitive flexibility, and planning, although findings in this regard are not consistent (Vilgis et al., 2015; Han et al., 2016). Evidence regarding EF deficits in BPD is also mixed, with several studies reporting problems in inhibition, planning, cognitive flexibility, and working memory (e.g. Hagenhoff et al., 2013), and others failing to find impairment in these domains or only in association with BPD subtypes or comorbidity (see McClure et al., 2016). Wante et al. (2017) showed a mediating effect of maladaptive and adaptive emotion regulation (ER) strategies on the association between EF impairment and depressive symptoms in adolescents. The greater the EF impairment the more maladaptive ER strategies were reported.
Assessment of executive functions in everyday life
Multi-informant rating scales, such as the Behavior Rating Inventory of Executive Function (BRIEF; Gioia et al., 2000, 2002) are used to assess deficits in EF in everyday life behavior. While the clinical validity of the BRIEF has been demonstrated in a large number of studies in samples with neurological, developmental, psychopathological, or somatic disorders (McCandless and O’Laughlin, 2007; Drechsler et al., 2015; de Vries et al., 2018), the association between deficits in EF assessed by rating scales or by objective EF tests, which purportedly measure the same underlying EF construct, is often low (e.g. Toplak et al., 2010; Tran et al., 2021). While this does not call the validity of either method into question, one must keep in mind that scale-based and performance test-based EF measures provide complementary rather than equal information.
The BRIEF has rarely been used in adolescents with major depressive disorder (pMDD) as the primary diagnosis, but BRIEF indices have been shown to lie above the clinical threshold (>T65) in untreated children and adolescents with mood disorders (Vesco et al., 2018). In the adult version of the BRIEF (BRIEF-A, Roth et al., 2005), young adult patients with first-episode MDD indicated significantly higher deficits in EF compared to controls, with the largest effect sizes on Task Monitor, Plan/Organize, Initiate, and Working Memory (Schmid and Hammar, 2021).
A recent study compared parent-rated BRIEF profiles in adolescents with BPD of both the externalizing and the internalizing subgroups and found substantially higher impairment in the externalizing subgroup on all EF except for Shift, Emotional Control, and Initiate. Even in the internalizing subgroups though, the scale scores were above T60, indicating that the EF were impaired to a certain degree (Kalpakci et al., 2018). The authors concluded that one reason for the inconsistent findings on deficits in EF in BPD might be that the impact of the possible BPD subtypes has not been sufficiently considered in research, with EF apparently being particularly affected in the externalizing BPD subtype.
Taken together, deficits in EF have been reported in pMDD and in BPD, but no study to date investigated how EF are affected in depressed adolescents with comorbid borderline personality features.
Agreement between parent- and self-report
In general, the agreement between self-reports and informant ratings on clinical impairment scales is often low to moderate at best, and concordance is affected by age, gender, and the nature of the impairment (van der Ende et al., 2012; De Los Reyes et al., 2015). Poor parent-child interrater agreement has been associated with poorer treatment outcome (Goolsby et al., 2018). The agreement is usually lower for internalizing disorders than for externalizing disorders, which has been attributed to the low observability of internalizing symptoms (see Vierhaus et al., 2018). Discrepancies between parents’ ratings and self-reports in adolescents with depression have been frequently observed (e.g. Kazdin et al., 1983; Baumgartner et al., 2020). The question whether adolescents or their parents tend to report more severe depression symptoms is unresolved; it has been claimed that in community samples, adolescents often report more severe depressive symptoms than do their parents (e.g. Eg et al., 2018; Stein et al., 2018), while the reverse can be found in clinical samples (see Makol and Polo, 2017), although the findings in this regard are not consistent. Interrater agreement for BPF in adolescents has rarely been analyzed, but Schuppert and colleagues reported poor informant agreement in a BPD interview, with parents reporting fewer symptoms than patients (Schuppert et al., 2012).
In depression, self-perception may be negatively biased, which may lead to an overestimation of cognitive deficits and other symptoms (e.g. Schwert et al., 2018; Serra-Blasco et al., 2019). Negative self-evaluations are also characteristic of BPD (Winter et al., 2017). Concerning ratings of EF, self-reports may also be biased because of cognitive impairment and diminished awareness (e.g. Krasny-Pacini et al., 2015). However, in individuals with relatively mild cognitive deficits, awareness of cognitive problems encountered in everyday life may be enhanced. At the same time, relatives may not notice these difficulties, which the affected person may try to compensate for or to dissimulate (e.g. Rizzo et al., 2012; Puhr et al., 2019). Parent ratings of depression and/or BPD symptoms may also be biased, e.g. underestimating, misidentifying, or – rarely – overestimating depressive symptoms in their teenage child (Madjar et al., 2020). Parents may be unaware of their child’s inner conflicts or suicidal thoughts (Jones et al., 2019).
This present study investigated EF in everyday life of adolescents with pMDD and analyzed the possible impact of deficits in EF on BPF tendencies in this group. The following research hypotheses and questions guided our analyses:
– We expected adolescents with pMDD to have deficits in EF, especially in the scales Monitor, Plan/Organize, Initiate, and Working Memory.
– We expected adolescents to report greater deficits on the BRIEF self-rating scales compared to their parents’ report on the BRIEF parent-rating scales, thus reflecting poor interrater agreement.
– We hypothesized that pMDD patients with more severe EF impairment and greater depression severity would show elevated BPF. In particular, we expected that more severe deficits on BRIEF scales Inhibit, Emotional Control, and Monitor, the three domains directly related to BPD core features, would predict higher BPF scores. We also sought to investigate the possible overlap between the concepts of BPF and EF.
– We hypothesized that deficits in EF would mediate the association between depression severity and BPF, especially for the BRIEF Behavioural Regulation Index, as it includes the Inhibit and Emotional Control scales.
Materials and methods
Recruitment, participants, and procedure
The data used for this analysis were gathered at the baseline visits of the omega-3-pMDD study of the University of Zurich (Switzerland). The main goal of the study is to assess the efficacy and safety of omega-3 fatty acids in the early course of paediatric major depressive disorder (pMDD) (Häberling et al., 2019). Inclusion criterion was a major depressive disorder according to DSM-IV (APA, 1994) with at least moderate symptom severity (cut-off score of the Children’s Depression Rating Scale-Revised (CDRS-R) ≥ 40). Exclusion criteria were pre-existing neurological disorders, lifetime diagnosis of schizophrenia or bipolar affective disorder, pervasive developmental disorder, severe conduct disorder, intellectual disability, substance dependency, but not misuse (ICD-10 F1x.2) or eating disorders (ICD-10 F 50.0 and 50.2) within the last six months. Additional inclusion criteria for the present study were age 13 to 17 years and complete data sets for the relevant instruments (BRIEF self-rating (SR), BRIEF parent-rating (P), Scale of Impulsivity and Emotion Dysregulation self-rating (IED-27 SR), Scale of Impulsivity and Emotion Dysregulation parent-rating (IED-27 P)).
Recruitment took place in various inpatient and outpatient units of seven departments of child and adolescent psychiatry in the German speaking part of Switzerland. The data were collected before randomization to one of the two treatment arms. The participants were visited by trained study staff either in the psychiatric hospital or at home. Patients and parents gave informed written consent before entering the study. The study was approved by the local ethics committees (www.ClinicalTrials.gov, identifier NCT03167307).
A total of 310 children and adolescents were screened, and 257 were randomized. After data cleaning, the sample for the present study consisted of 144 parent-child dyads. The adolescents’ mean age was 15.86 years (SD = 1.32), and 74.3% of the sample were female.
Measures
Executive functions
Deficits of EF in everyday life were assessed using the German version of the BRIEF (Gioia et al., 2002; Drechsler and Steinhausen, 2013), as briefly described in the introduction. The original BRIEF structure was supposed to have a two-factor structure, which is reflected by two overarching indices: the Behavioural Regulation Index (BRI) with its scales Inhibition, Shift, Emotional Control, and the Metacognition Index (MI), comprising the scales Working Memory, Initiate, Monitor, Plan/Organize, and Organization of Materials. However, the initial two-factor structure has been questioned by various studies (e.g. Halvorsen et al., 2019). In 2015, a shorter form, the BRIEF-2 (Behaviour Rating Inventory of Executive Function, Second Edition; Gioia et al., 2015) was published, which is based on a three-factor structure, reflected by three indices: the Behavior Regulation Index (BRI), the Emotion Regulation Index (ERI), and the Cognitive Regulation Index (CRI). In the present paper, the original BRIEF scales are used. For comparison, additional analyses based on the BRIEF-2 scale structure can be found in Supplementary Tables 3, 4.
Borderline personality features
Borderline personality features (BPF) were assessed using the Scale of Impulsivity and Emotion Dysregulation (IED-27-J) in its adapted version for children and adolescents (Kröger and Kosfelder, 2011; Kröger et al., 2017; Dreysse et al., 2021). The IED-27-J is a 27-item questionnaire rated by children and their parents (see Supplementary Table 1 for self-rating items and Supplementary Table 2 for parents’ items). Borderline specific experiences and behavioral tendencies during the past month are to be rated on a 5-point Likert-scale (“never”, “1-2 times”, “3-10 times”, “daily”, “multiple times daily”) by the adolescents themselves and on a 3-point Likert-scale by the parents. While the scale was originally been developed for adults, the adaptation for adolescents has demonstrated good validity and rel iability (Kröger et al., 2017). Factorial analysis of the adult’s version resulted in three main factors: emotional dysregulation, relationship difficulties, and self-injuries and suicidal behavior (Dreysse et al., 2021).
Clinical assessment and IQ
Diagnosis of pMDD and other possible comorbid psychopathological disorders were based on the German version (Delmo et al., 2001) of the diagnostic interview Kiddie Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS; Kaufman et al., 1997), and depression severity was rated using the German version of the Children’s Depression Rating Scale – Revised (CDRS-R) (Poznanski et al., 1996; Keller et al., 2011, 2012). Both assessments are based on the clinician’s evaluation of the combined interviews of the adolescent and his or her parents. The interviews are conducted with the child and the parent separately and the trained clinician then integrates the parents’ and children’s reports to reach a final score. The 17 items of the CDRS-R quantify depressive symptoms over the past two weeks. A total score below 30 indicates no diagnosis of depression, 30–40 a mild depressive episode, and 40–60 a moderate depressive episode, and ≥ 60 a severe depressive episode. The maximum possible score is 113. The scale has been extensively used in research (Häberling et al., 2019). The IQ was assessed using the German adaptation (Hagmann-von Arx and Grob, 2014) of the Reynolds Intellectual Scales (RIAS; Reynolds and Kamphaus, 2003).
Statistical analysis
For the BRIEF scales, either raw scores or age- and gender adjusted T-values were used. BRIEF-T-values were used for all analyses except when analysing the conceptual overlap of EF and BPF using simple correlations, as described below (Drechsler and Steinhausen, 2013). Generally, a T-value above 65 indicates a clinical impairment, with T-values above 60 indicating subclinical deficits. For comparisons between parent-rating (P) and self-rating (SR), the BRIEF P Self-Monitor subscale was compared with the BRIEF SR Monitor scale because of the respective item structure. The comparison of self-rated and parent-rated EF was calculated with t-tests for paired samples with Bonferroni correction for multiple comparisons applied.
Agreement between parent and child ratings on the BRIEF scales was analyzed with the intraclass correlation coefficient (ICC) (McGraw and Wong, 1996; Koo and Li, 2016), which is a standard reliability index. According to Koo and Li (2016), based on the 95% confidence interval of the ICC estimate, values below 0.5 indicate poor reliability and values between 0.5 and 0.75 indicate moderate reliability. The possible overlap of the concepts of EF and BPF was analyzed based on correlations of the BRIEF SR and BRIEF P scales (raw-scores) with the three factors structure of the IED-27 SR and IED-27 P proposed by Dreysse et al. (2021), applying Bonferroni correction to control for multiple comparisons.
To investigate the relationship between depression severity, EF and BPF, we calculated two multiple regression analyses: 1. self-rated IED-27 total score as dependent variable with self-rated BRIEF scales and CDRS total score as independent variables; 2. parent-rated IED-27 total score as dependent variables with parent-rated BRIEF scales and CDRS total scores as independent variables (pre-requirements were met).
To examine whether EF mediate the relationship between depression severity and BPF. we conducted three parallel mediation models using model 4 of the SPSS PROCESS macro by Hayes (2018). As the CDRS includes items about suicidal behavior and suicidal thoughts, we extracted four factors of the IED-27 SR: emotional dysregulation, relationship difficulties, suicidal behavior, and non-suicidal self-injuries (nssi) (based on Dreysse et al. (2020)). The factor suicidal behaviour was not included in any analysis. Three different mediation models were calculated, with BRI and MI of the BRIEF SR as parallel mediators of the relationship between depression severity and the three IED-27 SR factors emotional dysregulation, relationship difficulties, and nssi. The CDRS score used in the analysis was based on the child’s assessment of items 1–14, as ratings of items 15–17 are based solely on the clinician’s perception. As covariates, we included age, gender, and IQ. Process uses a standard bootstrapping approach based on 5,000 samples that provides confidence intervals for indirect effects. Confidence intervals that do not include 0 provide evidence for a statistically significant mediation effect. Statistical analyses were conducted using SPSS Version 27 for Windows and Version 28 for Mac (IBM Corp, 2020, 2021), Excel (Microsoft Excel, 2018), and R Version 2022.07.2+576 for Mac (R Core Team, 2022).
Results
Sample description
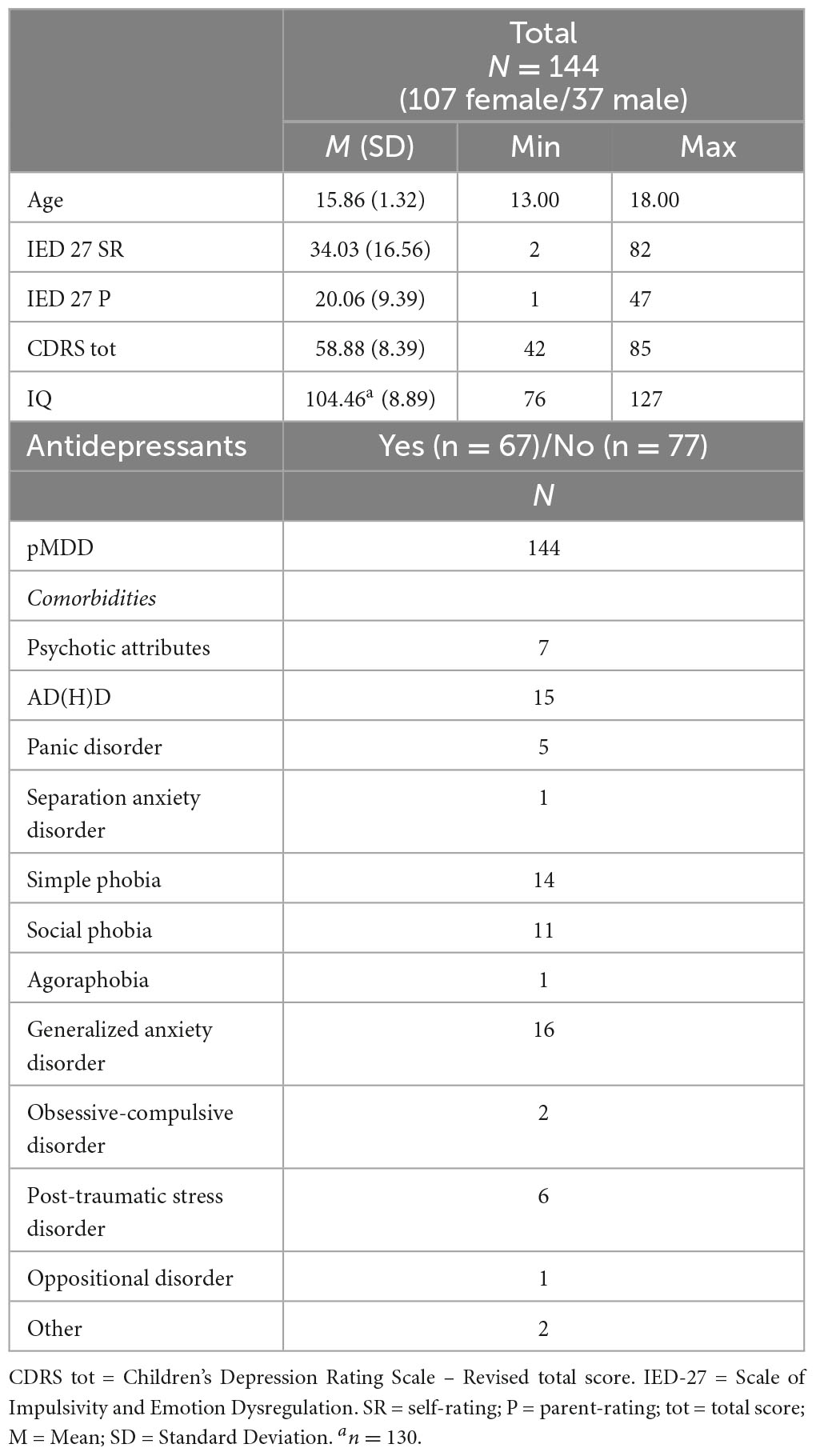
Descriptive statistics of the sample is listed in Table 1. The adolescents in our sample reported a mean IED-27 SR score of M = 34.03 (SD = 16.56; Min = 2, Max = 82). Parents reported a mean IED-27 P score of M = 20.06 (SD = 9.39; Min = 1, Max = 47). The mean depression severity score of our sample was M = 58.88 (SD = 8.39; Min = 42, Max = 85). The mean IQ was M = 104.46 (SD = 8.89; Min = 76, Max = 127). 67 adolescents reported the intake of antidepressants.
Comparison of self-rated and parent-rated EF (BRIEF scales)
Only the BRIEF SR scales Emotional Control (M = 61.10, SD = 10.80), Working Memory (M = 63.60, SD = 13.37), and Plan/Organize (M = 60.60 SD = 12.34) and the index BRI (M = 63.66, SD = 11.31) were rated above T > 60 by the adolescents (Table 2). None of the parent-rated BRIEF P scales scored above T > 60. The paired sample t-tests showed a significant differences between self-rating and parent-rating for the BRIEF scales Inhibit (t = 3.228, p < 0.001), Emotional Control (t = 3.314, p = 0.011), Working Memory (t = 4.898, p < 0.001), Plan/Organize (t = 2.948, p = 0.002), Organization of Materials (t = 2.711, p = 0.004) and the Index MI (t = 3.365, p < 0.001), with medium effect sizes (d) (Cohen, 1988). After Bonferroni correction for multiple comparisons (0.05/9 = 0.006), the rating difference for Emotional Control was no longer significant (Table 2 and Figure 1). Agreement between self-and parent-rated BRIEF scales was poor (<0.50) for all scales and indices.
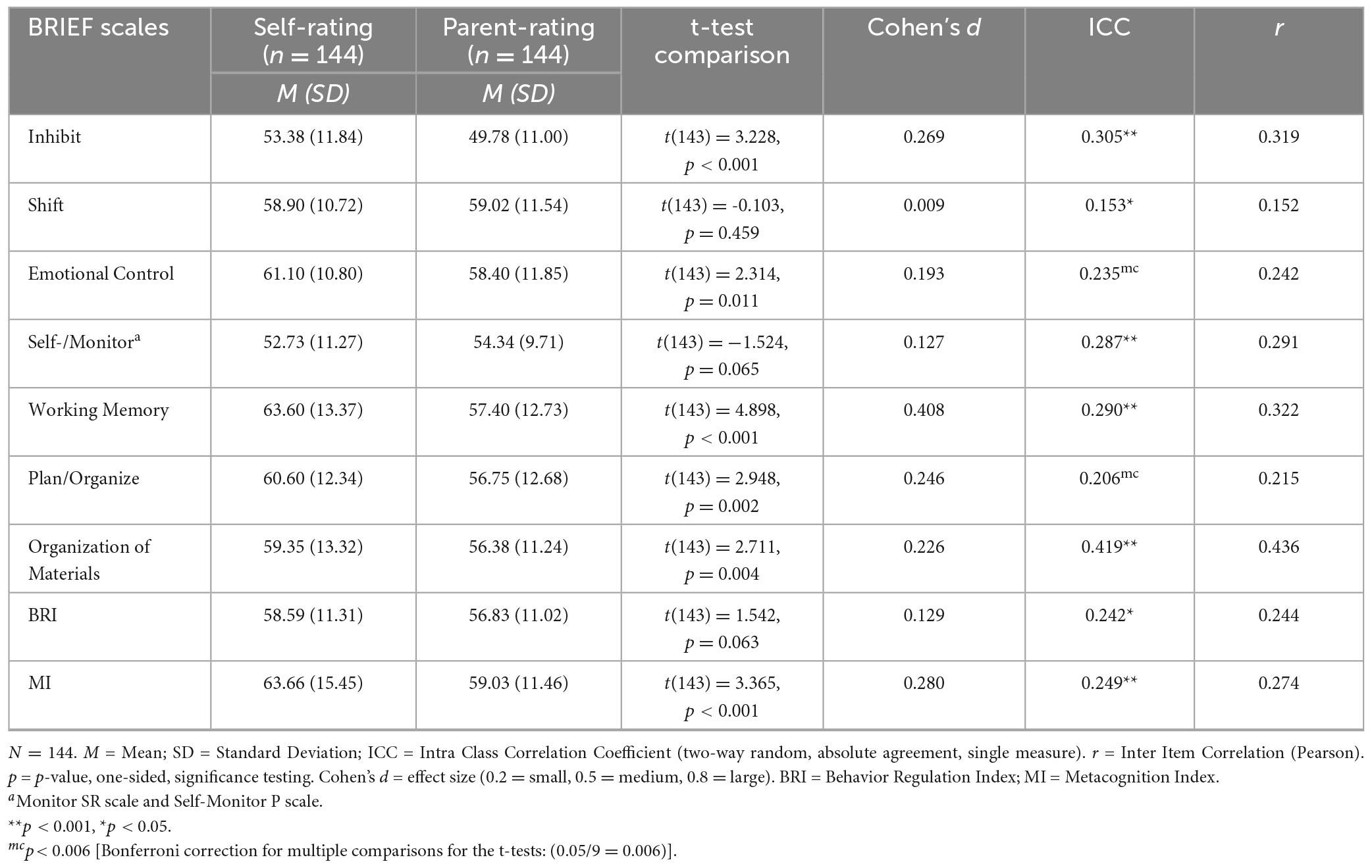
Table 2. Total sample: t-Test comparison of BRIEF-SR and BRIEF-P scales and intraclass correlations – T-values.
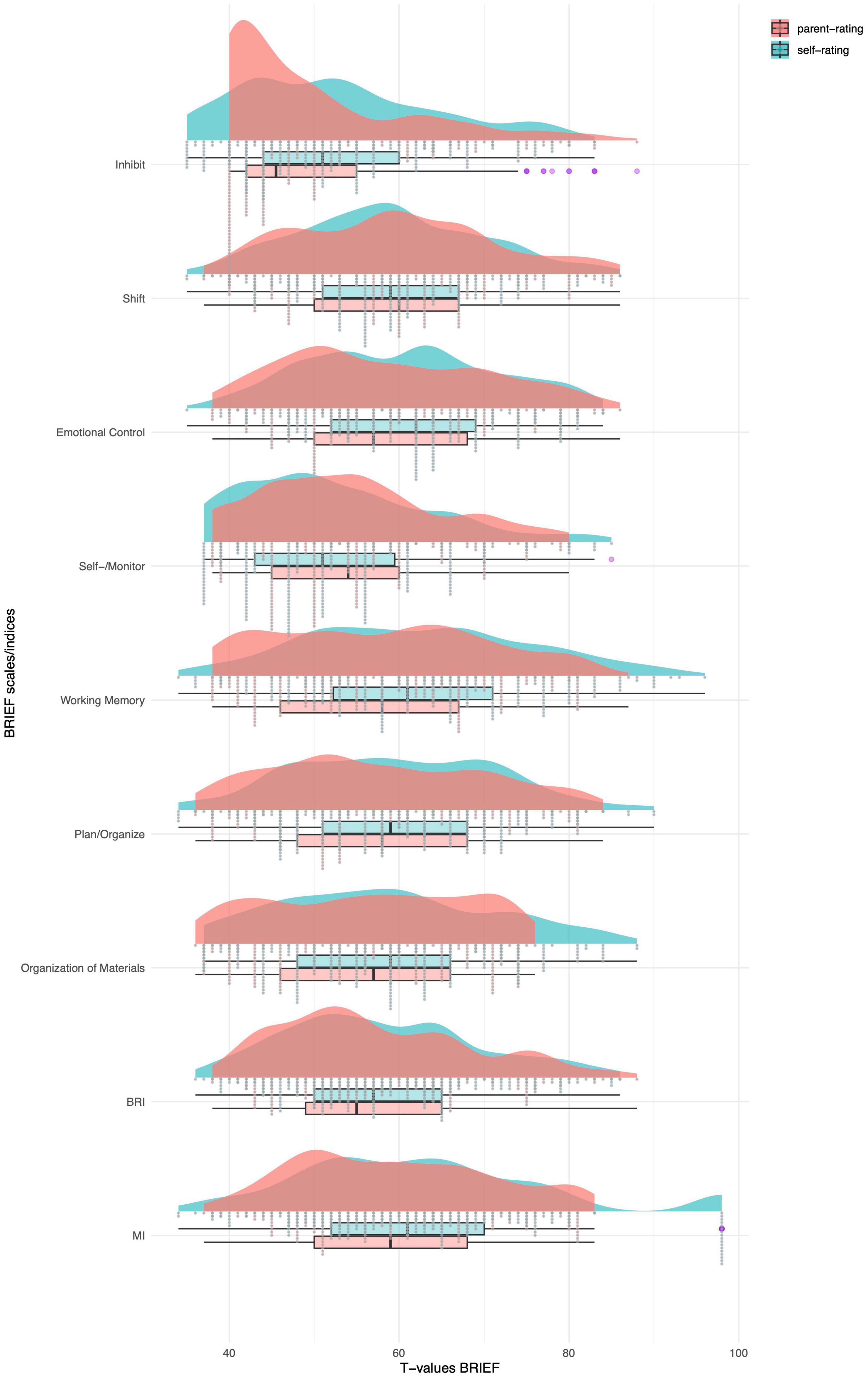
Figure 1. Means of self-rated and parent-rated BRIEF scales – T-values, N = 144. Monitor self-rating and self-monitor parent-rating scale. BRI = Behavior Regulation Index; MI = Metacognition Index; Purple = outliers.
Association between EF [BRIEF scales and BPF (IED-27 factors)]
We performed a correlation analysis to test for a possible overlap between BRIEF scales and IED-27 factors (Table 3). The emotional dysregulation factor correlated only weakly with the BRIEF scales and indices. The relationship difficulties factor, however, correlated highly with the parent-rated Emotional Control (r = 0.561, p < 0.001) scale and the index BRI (r = 0.548, p < 0.001). For the self-rated version, the relationship difficulties factor correlated highly with the scales Inhibit (r = 0.595, p < 0.001), Emotional Control (r = 0.624, p < 0.001) and the BRI (r = 0.659, p < 0.001). The self-injuries and suicidal behavior factor, on the other hand, did not correlate with any of the self-or parent-rated BRIEF scales or indices. A complete overview of the correlations between individual IED-27 SR/P items and the BRIEF scales can be found in the Supplementary Table 1 (self-rating) and Supplementary Table 2 (parent-rating). In the supplement Supplementary Tables 3, 4 the correlations between the BRIEF 2 subscales and the three IED-27 factors are listed, revealing a very similar pattern of correlation to the original BRIEF scales presented here.
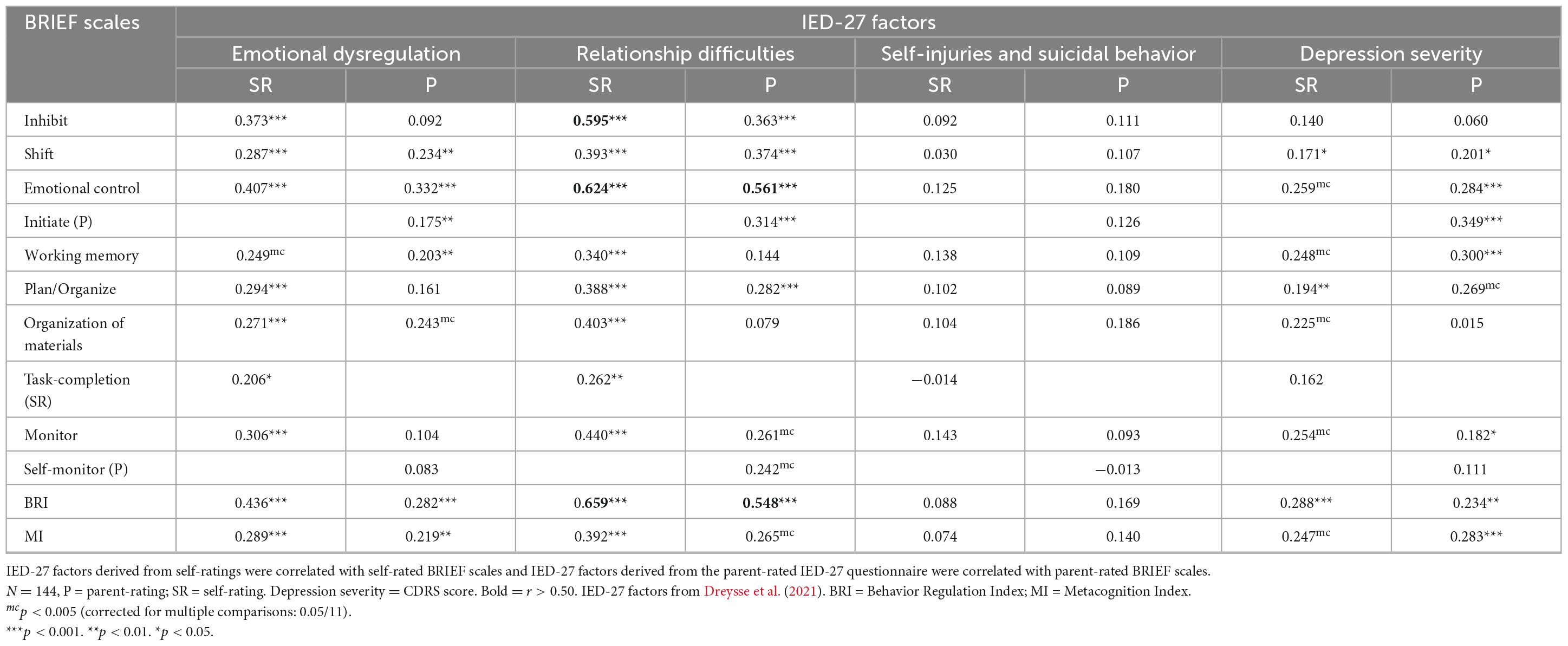
Table 3. Correlations between the three IED-27 factors and the BRIEF scales and indices (raw scores).
EF deficits and depression severity as predictors for BPF
To test the association between deficits in EF and BPF, we conducted two separate multiple regression analyses, as shown in Table 4. For the self-rating, the overall model was significant F(8,135) = 9.774, p < 0.001 with an adjusted R2 = 0.329. The CDRS total score (b = 0.729, p < 0.001) and the BRIEF scale Inhibit (b = 0.330, p < 0.033) significantly predicted the self-rated IED score. For the parent ratings, the model was also significant (F(8,135) = 7.214, p < 0.001) with an adjusted R2 = 0.258. The BRIEF scale Emotional Control (b = 0.173, p = 0.032) and the CDRS total score (b = 0.364, p < 0.001) significantly predicted the parent-rated IED total score.
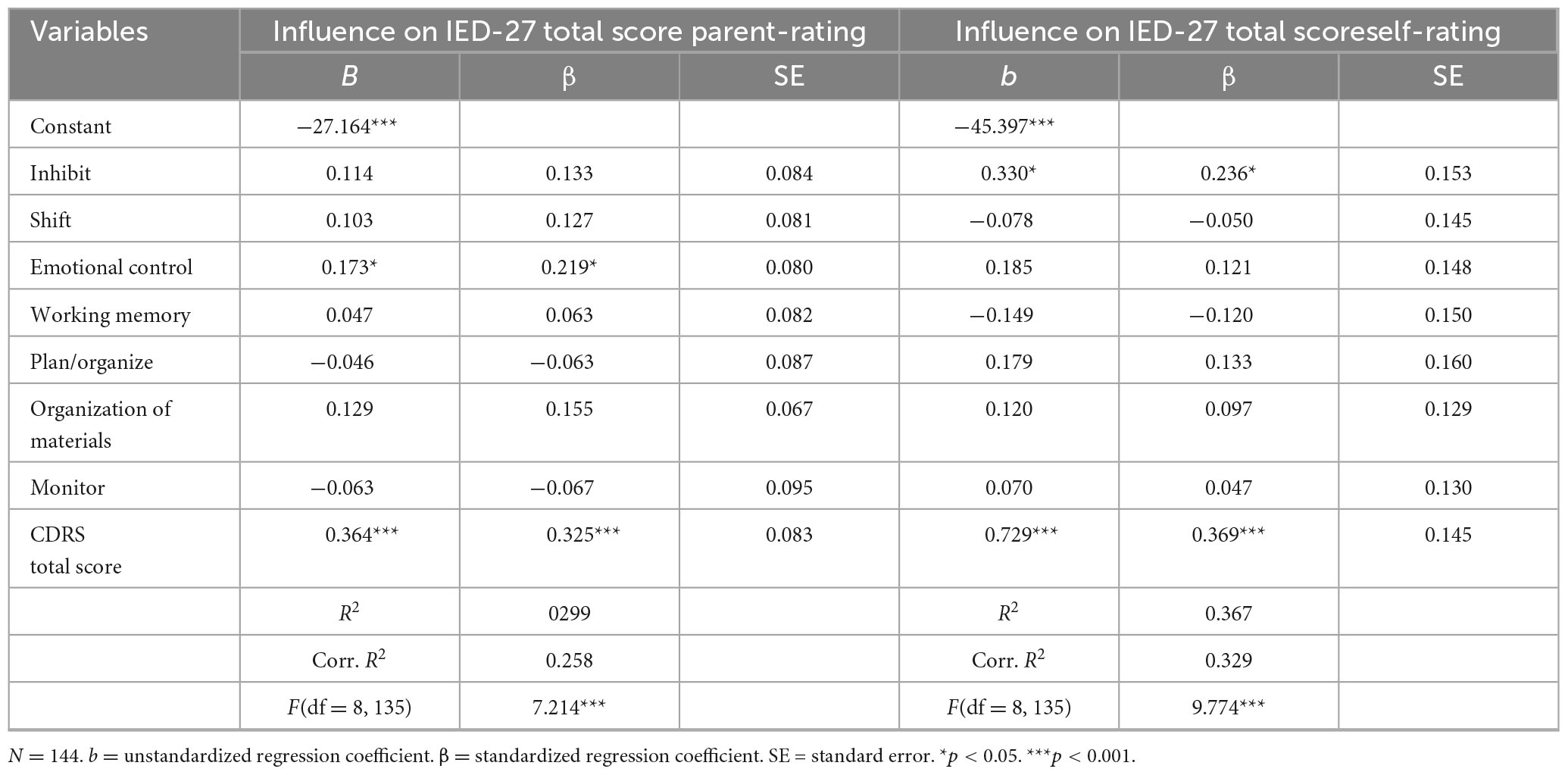
Table 4. Multiple regression analyses for IED-27 total score with BRIEF scales and CDRS total score – parent-rating and self-rating – T-values.
Parallel mediation models – does EF impairment mediate the relationship between depression severity and borderline personality features?
To further investigate the relationship between depression severity EF impairment and borderline personality features, we conducted three parallel mediation models in which EF impairment (BRIEF SR indices BRI and MI) mediate the association between depression severity (CDRS) and one of the three factors emotional dysregulation, relationship difficulties and nssi (IED 27 SR factors). The parallel mediation models confirmed a significant association between depression severity and EF impairment for all three factors (see Figure 2 for the factor emotional dysregulation (total effect c: β = 0.0453, p < 0.001), Figure 3 for the factor relationship difficulties (total effect c: β = 0.0351, p < 0.001) and Figure 4 for the factor nssi (total effect c: β = 0.0423, p < 0.001)). After entering the mediators BRI and MI into the parallel mediation models, depression severity predicted both mediators significantly, BRI: β = 0.3103, p = 0.006, MI: β = 0.3506, p = 0.012 (same values for all three models). The BRI predicted emotional dysregulation significantly, β = 0.0165, p = 0.011; while the MI did not, β = 0.0037, p = 0.467. We found that the relationship between depression severity and emotional dysregulation is mediated by the BRI (95% CI [0.0007–0.0118]), but not the MI (95% CI [−0.0020–0.0061]), (Figure 2). Similarly, relationship difficulties were predicted significantly by the BRI, β = 0.0392, p < 0.001, but not the MI: β = 0.0024, p = 0.581. We found that the relationship between depression severity and relationship difficulties is mediated by the BRI (95% CI [0.0036–0.0215]) but not the MI (95% CI [−0.0019–0.0048]) (Figure 3). In contrast, neither the BRI (95% CI [−0.0043–0.0050]) nor the MI (95% CI [−0.0057–0.0033]) significantly mediated the relationship between depression severity and nssi (Figure 4).
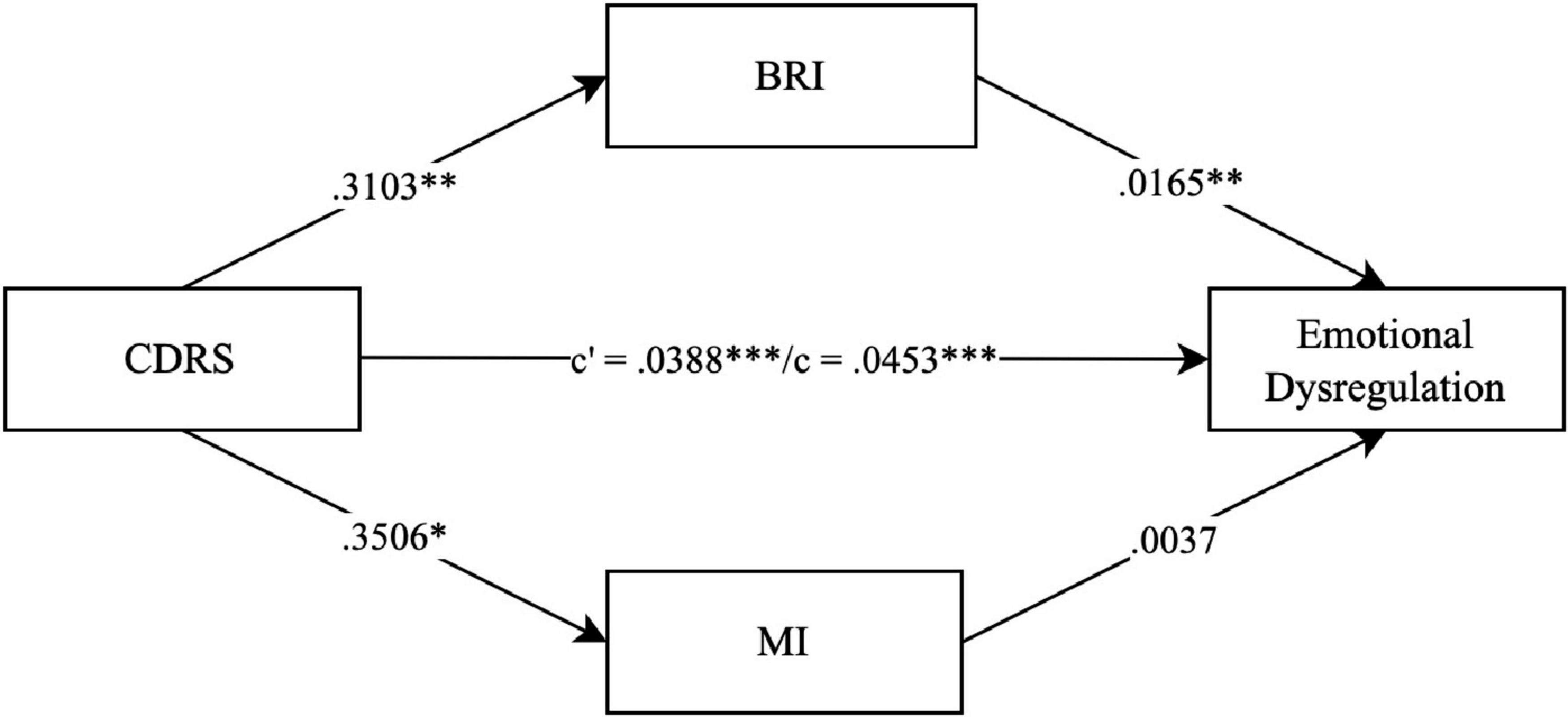
Figure 2. Parallel mediation model – CDRS, IED-27 SR factor emotional dysregulation. N = 144. CDRS score = items 1–14 child rating. BRI = Behavior Regulation Index; MI = Metacognition Index; BRIEF SR T-values. c’ = direct effect. c = total effect. ***p < 0.001. **p < 0.01. *p < 0.05. Covariates gender, age and IQ were included in the mediation, not shown due to non-significance.
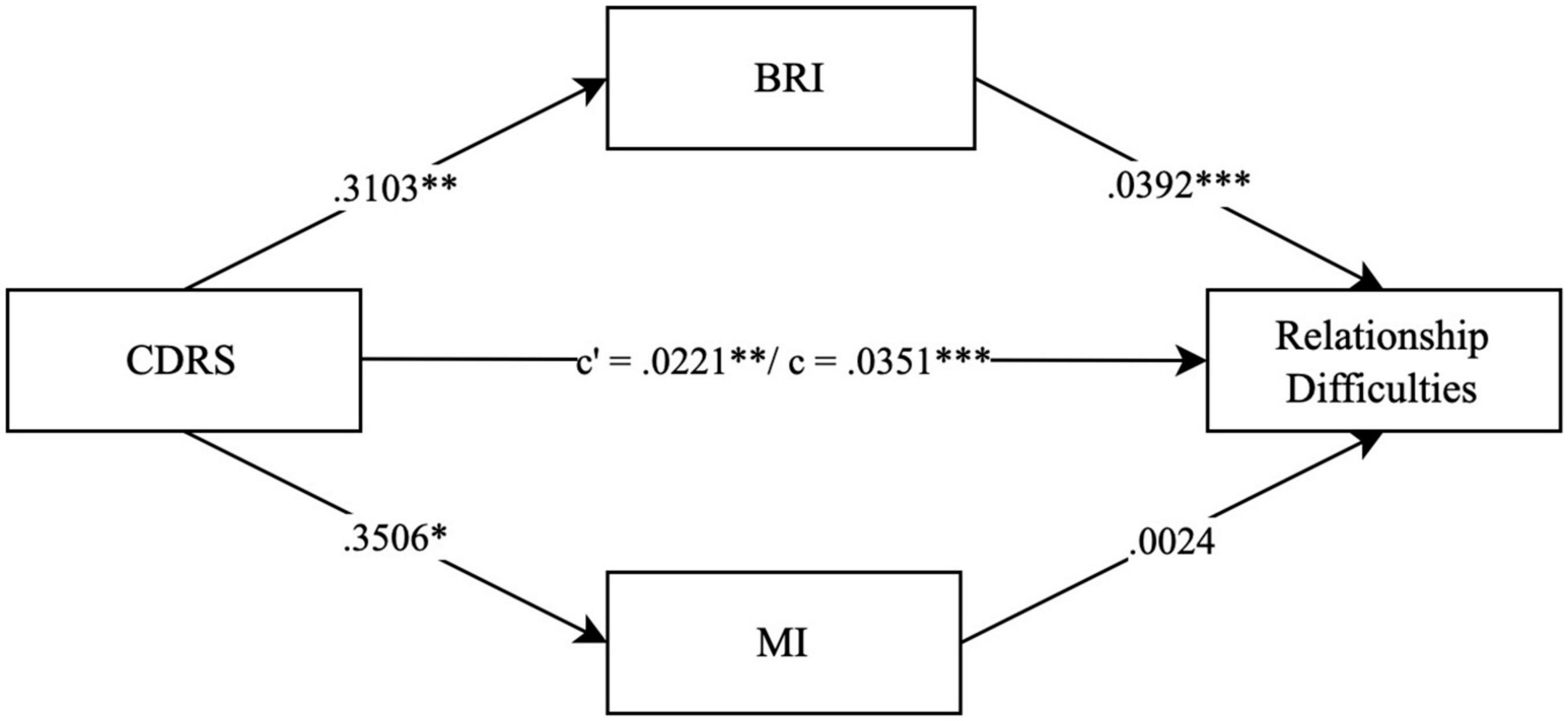
Figure 3. Parallel mediation model – CDRS, IED-27 SR factor relationship difficulties. N = 144. CDRS score = items 1-14 child rating. BRI = Behavior Regulation Index; MI = Metacognition Index; BRIEF SR T-values. c’ = direct effect. c = total effect. ***p < 0.001. **p < 0.01. *p < 0.05. Covariates gender, age and IQ were included in the mediation, not shown due to non-significance.
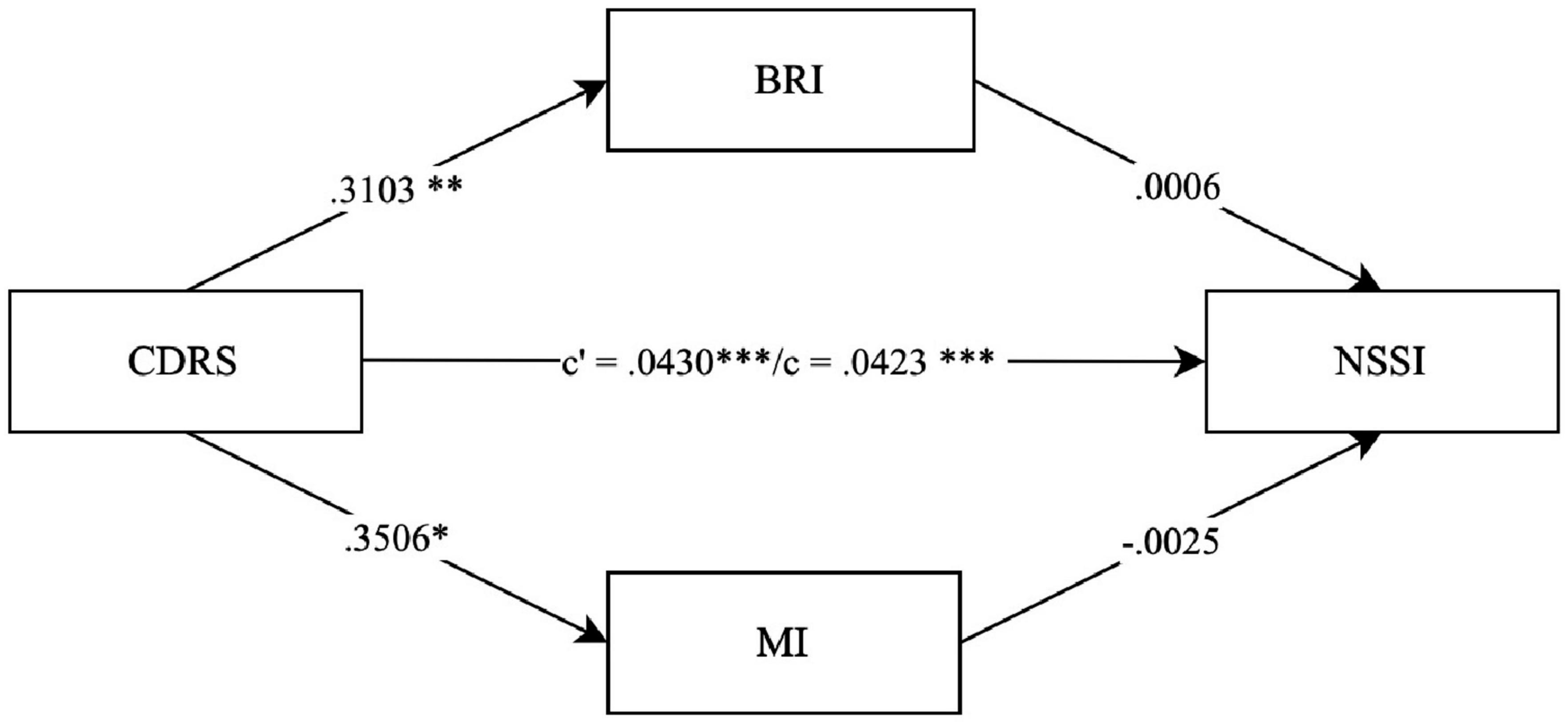
Figure 4. Parallel mediation model – CDRS, IED-27 SR factor nssi. N = 144. CDRS score = items 1-14 child rating. BRI = Behavior Regulation Index; MI = Metacognition Index; BRIEF SR T-values. c’ = direct effect. c = total effect. ***p < 0.001. **p < 0.01. *p < 0.05. Covariates gender, age and IQ were included in the mediation, not shown due to non-significance.
Discussion
The present study investigated the deficits of EF in daily life in moderately to severely depressed adolescents and whether the observed deficits in EF are related to borderline personality features. Furthermore, we examined the agreement between self- and parent-rated deficits in EF.
Executive functioning in clinically depressed adolescents
Overall, none of the BRIEF scale scores lay above T > 65 indicating clinical impairment, neither for the self-rated nor for the parent-rated scales of the present sample. The self-rated scales Emotional Control, Working Memory, and Plan/Organize, as well as the index MI, had a mean score above T > 60, which might indicate subclinical deficits. On average, the deficits seem to be subtle and more cognitive rather than behavioural, which is reflected by the high score of the Metacognition Index. In the present sample, parents did not rate their children as clinically impaired, as none of the scales scored within the subclinical or clinical range. This is in contrast to the study by Vesco et al. (2018), who found the MI and the BRI in the clinical range according to the parents’ ratings in a sample of 95 depressed children with a mean age of 11 years. This difference may be explained by the fact that their sample was mixed, with children presenting depressive or bipolar disorder and a high comorbidity with ADHD (61%). In the study by Schmid and Hammar (2021) the MI was in a clinical range in the group of patients who still had depressive symptoms one year after the onset of the first MDD episode. Unfortunately, the scores from the first episodes were not published.
The adolescents in our sample reported the greatest T-values for the scale Working Memory. Deficits in working memory in adolescent patients with pMDD compared to healthy controls have been reported in previous studies (Baune et al., 2014; Friedman et al., 2018), and working memory seems to be one of the EF most strongly affected by depression. While deficits in other EF have been reported in several studies with adult MDD patients based on objective tests (Stordal et al., 2004; Wagner et al., 2012). Vilgis et al. (2015) concluded in their systematic review that there is little support for deficits in EF in pMDD in minors. Our results seem to corroborate this conclusion given that only the adolescents themselves described subtle EF deficits in some of the cognitive scales.
Comparison and agreement of self-rated and parent-rated EF
Overall, the adolescents in this sample reported significantly stronger deficits in EF than their parents, especially on the BRIEF scales Inhibit, Emotional Control, Working Memory, Plan/Organize, and Organization of Materials. The difference between the self-perceived and the parents’ EF ratings is also reflected in the poor agreement between the two reports. This is in contrast to the results of Egan et al. (2018), who compared the BRIEF self- and parent-rated scores in a community sample. There are at least two possible explanations for this discrepancy; first, adolescents with pMDD might overestimate their deficits because they have a biased perception due to the pMDD symptomology (Dozois et al., 2012; Jónsdóttir et al., 2021). Second, parents are potentially underestimating the deficits in their children. Orchard et al. (2019) found that parents of adolescents with subthreshold depression struggle to observe subtler cognitive deficits. However, the present study’s sample consists of adolescents with more pronounced pMDD symptoms. Therefore, it is reasonable to assume that parents may underestimate deficits in their children, as suggested by Upton et al. (2008). This underestimation may be due to a lack of awareness or understanding of their children’s experiences or even a tendency to minimize or deny the presence of issues to avoid confronting them. Recognizing the discrepancies between self-ratings and parent-ratings of EF deficits can help clinicians identify potential biases and better interpret the assessments. This understanding can lead to more accurate diagnoses and personalized treatment plans. Furthermore, incorporating both self-ratings and parent-ratings into the assessment process can provide a more comprehensive picture of the adolescent’s functioning, allowing clinicians to address areas of concern that may otherwise go unnoticed. Involving both adolescents and parents in the treatment process can also foster open communication, enhance therapeutic alliance, and improve treatment adherence and outcomes.
Associations between EF and BPF
To investigate the possible overlap between BPF and EF, we conducted two correlation analyses, one with BRIEF SR scales and IED-27 SR factors and one with BRIEF P scales and IED-27 P factors. The analysis revealed that the BRIEF scales Inhibit and Emotional Control correlated strongly with the IED-27 relationship difficulties factor for parent- and self-rating. The scales of the MI, such as Working Memory, Organisation of Materials, and Monitor, did not correlate as highly, but were nevertheless still higher when based on the adolescents’ self-ratings. Very similar results were obtained when we used BRIEF 2 scales and indices (Gioia et al., 2015) (Supplementary Tables 3, 4), suggesting that the present findings are not dependent on the original BRIEF two-factor structure.
Some of the behaviors that are characteristic of BPF, such as emotional instability, were found to be related to EF deficits. This is also reflected in the fact that the questionnaires contain similar items (see supplement Supplementary Table 1 for IED-27 SR items). For example, the IED-27 SR item “My feelings went up and down like a roller coaster” (Dreysse et al., 2020) is similar to the BRIEF SR item on the Emotional Control scale “mood changes rapidly”. Therefore, it is somewhat surprising that the BRIEF scale Emotional Control showed the strongest correlation with the IED-27 relationship difficulties factor and not with the emotional dysregulation factor. Perhaps it is in relationship difficulties that deficits in EF may be observed best as they come into light in social interactions. The IED-27 SR emotional dysregulation factor also correlated with Inhibit and Emotional Control, but only moderately. Thus, this typical BPF of emotional dysregulation is only partly attributable to a perceived deficit in the executive function of Emotional Control and might encompass further aspects that are not related to EF deficits per se. The mediation models support these findings, as the BRI significantly mediated the relationship between depression severity and the factors emotional dysregulation and relationship difficulties for self-rating. Similar to the results of Wante et al. (2017), who defined emotion regulation strategies as a mediator between EF impairment and depressive symptoms; however, adolescents in our sample have a clinically diagnosed pMDD.
The self-injuries and suicidal behavior factor of the IED-27, which is a symptom of both pMDD and BPD, did not correlate with any of the BRIEF scales, either in parent-ratings or in self-ratings. In the mediation model, although depression severity predicted the level of nssi, this relationship was not mediated by neither of the BRIEF indices. In contrast to our findings, Fikke et al. (2011) reported working memory deficits in adolescents with high-severity non-suicidal self-injury (NSSI) and impaired inhibitory control in adolescents with low-severity NSSI compared with healthy controls. Other studies linked suicidality to impaired decision-making in adolescents (Bridge et al., 2012) and adults (Allen et al., 2019). In adults, the most consistent findings of deficits in EF were found for suicide attempters with depression (Lara et al., 2015; Lalovic et al., 2022). However, one study reported that adolescents at risk of suicide did not show any EF deficits but rather impairments in other neurocognitive domains, such as complex cognition, episodic memory, or social cognition (Ortuño-Sierra et al., 2020). As in our sample, suicidal and non-suicidal self-harm behaviour appeared to be unrelated to perceived EF deficits.
Depression severity and impaired EF as predictors for BPF
For self- and parent-rated models, depression severity was the strongest predictor of elevated BPF in our sample, highlighting the high comorbidity rate of pMDD and BPD (Pham-Scottez, 2016). Furthermore, the Emotional Control (parent-rating) and Inhibit (self-rating) scales also significantly predicted BPF. For parents, emotional control might be one of the most discerning executive functions and it is associated with emotional instability as well as relationship difficulties. Interestingly, in the self-rated version, inhibit was the EF scale most strongly associated with BPF. More so, the BRI, which includes the Inhibt subscale, significantly mediated the relationship between depression severity, and emotional dysregulation and relationship difficulties. This suggests that problems with inhibition may be one of the mechanisms leading to the typical symptoms of BPD in depressed adolescents. Ernst et al. (2018) found a general inhibitory dysfunction in adult patients with MDD and BPD compared to those with MDD only.
The mediation analysis suggests that depression symptoms could lead to deficits in executive functions related to behavioral control, which in turn negatively affect emotional regulation and lead to problems in social relationships. Allan et al. (2016) argued in a review article that there is a positive feedback loop between EF and health-related behaviour. Accordingly, depressive symptoms might be related to deficits in executive functioning and BPF in a negative feedback loop. For example, problems in relationships with others might exacerbate depressive symptoms such as guilt and self-worth, which increases the severity of depression which in turn negatively affects EF. According to a recent review, EF in MDD is related to theory of mind (ToM) (Pagnoni et al., 2022). Deficits in ToM could hinder accurate categorization of another person’s mental state and lead to relationship problems.
Recognizing the relationship between pMDD, BPF, and EF can help clinicians develop a more nuanced understanding of the factors contributing to an adolescent’s psychopathology. This insight can guide the selection of targeted interventions for at-risk adolescents, such as cognitive-behavioral therapy (CBT) that addresses both emotion regulation and executive function skills. By focusing treatment on the overlapping features of pMDD and BPF and targeting the underlying cognitive and emotional processes involved in both, clinicians may be able to provide more effective interventions (Basharpoor et al., 2022). This in turn can lead to improvements in patient well-being and quality of life by enhancing overall psychosocial functioning in adolescents with comorbid BPF.
Limitations
The main limitation of our analysis lies in the sample. We assessed deficits in EF in a sample of adolescents diagnosed with pMDD with moderate to severe symptom severity and assessed the impact of BPF, without diagnosing BPD itself. Thus, it remains unclear whether these results might also apply to manifest BPDs. Furthermore, our sample might be somewhat biased due to the inclusion criteria of the Omega-3-pMDD Study, such as the exclusion of patients with substance dependency (Sansone and Sansone, 2011). This might have contributed to the imbalance between girls and boys in this sample, which was about 3:1. Nevertheless, this girl-boy ratio is in accordance with most of the literature about pMDD, 3:1 (Bernaras et al., 2019). In addition, EF were assessed only using rating scales and was not based on objective measures.
Conclusion
To summarize, our data show that adolescents with depression generally do not perceive their EF as clinically impaired. However, adolescents who perceive greater deficits in EF in their daily life also report higher borderline personality features. Parents confirmed the relationship between EF deficits and greater BPF but did not report the EF deficits to be as high as the adolescents themselves. It is difficult to determine whether the perceived deficits are present but not perceived by the parents or related to a deficit in self-perception in adolescents with elevated BPF. Depression is characterized by a negative bias in self-perception, and these negative distortions in perception might be aggravated by comorbid BPF, likely leading to an overestimation of deficits in EF in daily life. Even more so, impairment in certain executive functions, especially in the executive functions related to behavioural control, might be related to borderline personality features, such as emotional dysregulation and relationship difficulties. EF have a strong impact on various aspects of daily life and intact executive functioning is crucial for succeeding in school and early professional development. Deficits in these executive functions might lead to problems typically associated with borderline personality disorder, further affecting psychosocial functioning and possibly reinforcing depressive symptoms in a negative feedback loop. Therefore, the assessment and treatment of deficits in executive functioning in adolescents with depression might have a positive impact on overall symptomatology in this highly affected patient group.
Data availability statement
The raw data of this study will be made available by the authors upon request.
Ethics statement
The studies involving human participants were reviewed and approved by Kantonale Ethikkommission Zürich (KEK): Lead-Ethic Commission, Ethikkommission Ostschweiz (EKOS), Ethikkommission Nordwest- und Zentralschweiz (EKNZ), number: 2016-02116. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin and the study participants.
Author contributions
MA and IH: analysis and interpretation of the data. MA, IH, SoE, and GB: writing, editing, and revision of the manuscript. KS, SoE, SB, LW, UM-K, BC-W, and BR: Resources. GB: Funding acquisition. All authors have read and agreed to the published version of the manuscript.
The Omega-3 Study Team
The Omega-3 Study Team contributed with implementation of the design with following roles: Sponsor-investigator of the trial is GB (Department of Child and Adolescent Psychiatry, University Hospital of Psychiatry, University of Zurich, Neumünsterallee 9, 8032 Zurich, Switzerland; gregor.berger@puk.zh.ch; +4143 499 26 26). Chief investigator is KS. IH is study coordinator. Principal investigators and research psychologist from the clinical sites are as follows: Research psychologists: Noemi Baumgartner, Sophie Emery, Mona Albermann, and Kristin Nalani (Department of Child and Adolescent Psychiatry, University Hospital of Zurich); Principal Investigator Basel: KS; Investigators and research psychologists: Oliver Pick, Alain Di Gallo, and Michael Strumberger (Department of Child and Adolescent Psychiatry, Psychiatric University Hospitals Basel); Principal Investigator Basel-Stadt: Brigitte Contin; Investigator: Stefan Müller (Child and Adolescent Psychiatric Services Baselland); Principal Investigator: Silke Bachmann and Lars Wöckel, Investigator: Simone Heitzer (Clienia Littenheid); Principal Investigator: Bruno Rhiner; Investigators: Amir Yamini (Child and Adolescent Psychiatric Services Thurgau); Principal Investigator: Suzanne Erb; Investigators: Michael Schmid (Child and Adolescent Psychiatric Services St. Gallen); Principal Investigator: Ulrich Müller-Knapp; Investigator: Ioannis Christodoulakis (Klinik Sonnenhof). Ulrike Held and Burkhardt Seifert (retired) are statistical consultants. Edna Grünblatt is head of the department for translational molecular psychiatry (Department of Child and Adolescent Psychiatry, University Hospital of Zurich). Martin Hersberger is head of the division of Clinical Chemistry and Biochemistry at the University Children’s Hospital Zürich and his Ph.D student Ivan Hartling of the division of Clinical Chemistry and Biochemistry who will analyze the bioactive lipids; Romuald Brunner (University of Heidelberg), Jürgen Drewe (University of Basel), and Julia Braun (Epidemiology, Biostatistics, and Prevention Institute, University of Zürich) are members of the Data Monitoring Committee. Jenny Peterson, Clinical Trials Pharmacy (Kantonsapotheke) Zürich, responsible for the packaging, handling, and quality of the study medication.
Funding
The Omega-3-pMDD trial was funded by the Swiss National Foundation, grant number 33IC30_166826 and has been registered on www.ClinicalTrials.gov protocol no. NCT03167307. Ph.D. projects were supported by the Ebnet Foundation, the Thalmann Foundation, and the Vontobel Foundation. Infrastructure and administrative staff support was provided by the Research Department of Child and Adolescent Psychiatry, University Hospital of Psychiatry Zurich of the University of Zurich. Burgerstein, Antistress AG, Rapperswil-Jona (SG, Switzerland) provided the study medication free of charge for the clinical trial with no restrictions regarding data analysis or publication rights. Burgerstein provided no additional funding to the study, and was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication. No additional industrial funding is provided throughout the study.
Conflict of interest
KS has received royalties from Springer, Hogrefe, Schattauer, and Vandenhoeck & Ruprecht. His work was supported by the Swiss National Science Foundation (SNF), the Swiss Ministry of Justice, the Botnar Foundation, Stiftung zur Förderung von Psychiatrie und Psychotherapie, and Gertrud Thalmann Fonds. GB was supported by the Swiss National Science Foundation, Gesundheitsförderung Schweiz, the Stanley Foundation, the Gertrud Thalmann Fonds, and the Ebnet Foundation and he has received lecture honoraria from Lundbeck, Opopharma, Antistress AG (Burgerstein) in the last five years.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnhum.2023.957753/full#supplementary-material
References
Allan, J. L., McMinn, D., and Daly, M. (2016). A bidirectional relationship between executive function and health behavior: evidence, implications, and future directions. Front. Neurosci. 10:386. doi: 10.3389/fnins.2016.00386.
Allen, K. J. D., Bozzay, M. L., and Edenbaum, E. R. (2019). Neurocognition and suicide risk in adults. Curr. Behav. Neurosci. Rep. 6, 151–165. doi: 10.1007/s40473-019-00189-y
APA (1994). Diagnostic and Statistical Manual of Mental Disorders - DSM-IV, 4th Edn. Virginia: American Psychiatric Association.
Avenevoli, S., Swendsen, J., He, J., Burstein, M., and Merikangas, K. (2015). Major depression in the national comorbidity survey- adolescent supplement: prevalence, co. J. Am. Acad. Child Adolesc. Psychiatry 54, 37–44. doi: 10.1016/j.jaac.2014.10.010
Basharpoor, S., Zakibakhsh Mohammadi, N., Heidari, F., Azarkolah, A., Vicario, C. M., and Salehinejad, M. A. (2022). Emotional working memory training improves cognitive inhibitory abilities in individuals with borderline personality trait: a randomized parallel-group trial. J. Affect. Disord. 319, 181–188. doi: 10.1016/j.jad.2022.09.089
Baumgartner, N., Häberling, I., Emery, S., Strumberger, M., Nalani, K., Erb, S., et al. (2020). When parents and children disagree: informant discrepancies in reports of depressive symptoms in clinical interviews. J. Affect. Disord. 272, 223–230. doi: 10.1016/j.jad.2020.04.008
Baune, B. T., Fuhr, M., Air, T., and Hering, C. (2014). Neuropsychological functioning in adolescents and young adults with major depressive disorder - a review. Psychiatry Res. 218, 261–271. doi: 10.1016/j.psychres.2014.04.052
Beatson, J. A., and Rao, S. (2012). Depression and borderline personality disorder. Med. J. Australia 1, 24–27. doi: 10.5694/mja12.10474
Bernaras, E., Jaureguizar, J., and Garaigordobil, M. (2019). Child and adolescent depression: a review of theories, evaluation instruments, prevention programs, and treatments. Front. Psychol. 10:543. doi: 10.3389/fpsyg.2019.00543
Blackmore, S. J., and Mills, K. L. (2014). Is adolescence a sensitive period for sociocultural processing? Annu. Rev. Psychol. 65, 187–207. doi: 10.1146/annurev-psych-010213-115202
Bohus, M., Stoffers-Winterling, J., Sharp, C., Krause-Utz, A., Schmahl, C., and Lieb, K. (2021). Borderline personality disorder. Lancet 398, 1528–1540.
Bridge, J. A., McBee-Strayer, S. M., Cannon, E. A., Sheftall, A. H., Reynolds, B., and Campo, J. V. (2012). Impaired decision making in adolescent suicide attempters. J. Am. Acad. Child Adolesc. Psychiatry 51, 394–403. doi: 10.1016/j.jaac.2012.01.002
Carr, K. L., and Stewart, M. W. (2019). Effectiveness of school-based health center delivery of a cognitive skills building intervention in young, rural adolescents: potential applications for addiction and mood. J. Pediatric Nursing 47, 23–29. doi: 10.1016/j.pedn.2019.04.013
Chanen, A. M., Velakoulis, D., Carison, K., Gaunson, K., Wood, S. J., Pan, H., et al. (2008). Orbitofrontal, amygdala and hippocampal volumes in teenagers with first-presentation borderline personality disorder. Psychiatry Res. Neuroimaging 163, 116–125. doi: 10.1016/j.pscychresns.2007.08.007
Chapman, A. L. (2019). Borderline personality disorder and emotion dysregulation. Dev. Psychopathol. 31, 1143–1156. doi: 10.1017/S0954579419000658
Cohen, J. (1988). Statistical Power Analysis for the Behavioral Sciences. Milton Park: Taylor and Francis.
De Los Reyes, A., Augenstein, T., Wang, M., Thomas, S. A., Darbick, D. A. G., Burgers, D. E., et al. (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychol. Bull. 141, 858–900. doi: 10.1037/a0038498
de Vries, M., de Ruiter, M. A., Oostrom, K. J., Schouten-Van Meeteren, A. Y. N., Maurice-Stam, H., Oosterlaan, J., et al. (2018). The association between the behavior rating inventory of executive functioning and cognitive testing in children diagnosed with a brain tumor. Child Neuropsychol. 24, 844–858. doi: 10.1080/09297049.2017.1350262
Delmo, C., Weiffenbach, O., Stalder, C., Gabriel, M., and Poustka, F. (2001). Diagnostisches Interview Kiddie-Sads-Present and Lifetime Version (K-SADS-PL): 5: Auflage der Deutschen Forschungsversion, Erweitert Um ICD-10-Diagnostik, 5th Edn. Frankfurt: Klinik für Psychiatrie.
Diamond, A., and Lee, K. (2011). Interventions shown to aid executive function development in children 4 to 12 years old. Science 334:6054. doi: 10.1126/science.1204529
Donegan, N. H., Sanislow, C. A., Blumberg, H. P., Fulbright, R. K., Lacadie, C., Skudlarski, P., et al. (2003). Amygdala hyperreactivity in borderline personality disorder: implications for emotional dysregulation. Biol. Psychiatry 54, 1284–1293. doi: 10.1016/s0006-3223(03)00636-x
Dozois, D. J. A., Eichstedt, J. A., Collins, K. A., Phoenix, E., and Harris, K. (2012). Core beliefs, self-perception, and cognitive organization in depressed adolescents. Int. J. Cogn. Therapy 5, 99–112. doi: 10.1017/S0954579417001912
Drechsler, R. (2007). Exekutive funktionen übersicht und taxonomie. Zeitschrift Für Neuropsychologie 18, 233–248. doi: 10.1024/1016-264X.18.3.233
Drechsler, R., and Steinhausen, H.-C. (2013). Verhaltensinventar zur Beurteilung exekutiver Funktionen BRIEF. Deutschsprachige Adaption des Behavior Rating Inventory of Executive Function. Bern: Verlag Hans Huber.
Drechsler, R., Zulauf Logoz, M., Walitza, S., and Steinhausen, H. C. (2015). The relations between temperament, character, and executive functions in children with ADHD and clinical controls. J. Attention Disord. 22, 764–775. doi: 10.1177/1087054715583356
Dreysse, K., Beller, J., Armbrust, M., and Kröger, C. (2020). A hierarchical analysis of the latent trait of borderline personality disorder and its possible clinical implications. Psychiatry Res. 288:113023. doi: 10.1016/j.psychres.2020.113023
Dreysse, K., Zöllner, E., Behrens, C., Armbrust, M., and Kröger, C. (2021). Faktorielle und konvergente Validität der Skala zur Erfassung der Impulsivität und emotionalen Dysregulation (IES-27) bei Borderline-Persönlichkeitsstörung. Psychother. Psychosom. Med. Psychol. 71, 177–184. doi: 10.1055/a-1322-3334
Eg, J., Bilenberg, N., Costello, E. J., and Wesselhoeft, R. (2018). Self- and parent-reported depressive symptoms rated by the mood and feelings questionnaire. Psychiatry Res. 268, 419–425. doi: 10.1016/j.psychres.2018.07.016
Egan, K. N., Cohen, L. A., and Limbers, C. (2018). Parent–child agreement on the behavior rating inventory of executive functioning (BRIEF) in a community sample of adolescents. Appl. Neuropsychol. Child 8, 264–271. doi: 10.1080/21622965.2018.1438896
Ernst, M., Mohr, H. M., Schött, M., Rickmeyer, C., Fischmann, T., Leuzinger-Bohleber, M., et al. (2018). The effects of social exclusion on response inhibition in borderline personality disorder and major depression. Psychiatry Res. 262, 333–339. doi: 10.1016/j.psychres.2017.03.034
Fenesy, M. C., and Lee, S. S. (2019). Association of ADHD and executive functioning with childhood depression. J. Attention Disord. 23, 1368–1378. doi: 10.1177/1087054717723983
Fikke, L. T., Melinder, A., and Landrø, N. I. (2011). Executive functions are impaired in adolescents engaging in non-suicidal self-injury. Psychol. Med. 41, 601–610. doi: 10.1017/S0033291710001030
Friedman, N. P., du Pont, A., Corley, R. P., and Hewitt, J. K. (2018). Longitudinal relations between depressive symptoms and executive functions from adolescence to early adulthood: a twin study. Clin. Psychol. Sci. 6, 543–560. doi: 10.1177/2167702618766360
Gioia, G. A., Isquith, P. K., Guy, S. C., and Kenworthy, L. (2000). Child neuropsychology test revieW behavior rating inventory of executive function. Child Neuropsychol. 6, 235–238. doi: 10.1076/chin.6.3.235.3152
Gioia, G. A., Isquith, P. K., Guy, S. C., and Kenworthy, L. (2015). *BRIEF - 2 Behavior Rating Inventory of Executive Function, 2nd Edn. Available online at: https://www.wpspublish.com/brief-2-behavior-rating-inventory-of-executive-function-second-edition (accessed February 8, 2021).
Gioia, G. A., Isquith, P. K., Retzlaff, Kimberly, P. D., and Espy, A. A. (2002). Confirmatory factor analysis of the behavior rating inventory of executive function (BRIEF) in a clinical sample. Child Neuropsychol. 8, 249–257. doi: 10.1076/chin.8.4.249.13513
Gogtay, N., Giedd, J. N., Lusk, L., Hayashi, K. M., Greenstein, D., Vaituzis, A. C., et al. (2004). Dynamic mapping of human cortical development during childhood through early adulthood. Proc. Natl. Acad. Sci. U S A. 101, 8174–8179. doi: 10.1073/pnas.0402680101
Goolsby, J., Rich, B. A., Hinnant, B., Habayeb, S., Berghorst, L., De Los Reyes, A., et al. (2018). Parent–child informant discrepancy is associated with poorer treatment outcome. J. Child Family Stud. 27, 1228–1241. doi: 10.1007/s10964-019-01107-x
Guilé, J. M., Zavaglia, E., Berthiaume, C., and Bergeron, L. (2021). Prevalence and comorbidity of borderline personality traits in the Quebec general population aged 12–14 years. Soc. Psychiatry Psychiatric Epidemiol. 56, 2053–2062. doi: 10.1007/s00127-021-02067-z
Gürdere, C., Strobach, T., Pastore, M., and Pfeffer, I. (2023). Do executive functions predict physical activity behavior? a meta-analysis. BMC Psychol. 11:33. doi: 10.1186/s40359-023-01067-9
Häberling, I., Berger, G., Schmeck, K., Held, U., and Walitza, S. (2019). Omega-3 fatty acids as a treatment for pediatric depression. a phase III, 36 weeks, multi-center, double-blind, placebo-controlled randomized superiority study. Front. Psychiatry 10:863. doi: 10.3389/fpsyt.2019.00863
Hagenhoff, M., Franzen, N., Koppe, G., Baer, N., Scheibel, N., Sammer, G., et al. (2013). Executive functions in borderline personality disorder. Psychiatry Res. 210, 224–231. doi: 10.1016/j.jad.2012.05.007
Hagmann-von Arx, P., and Grob, A. (2014). RIAS - Reynolds Intellectual Assessment Scales and Screening: Deutschsprachige Adaptation der Reynolds Intellectual Assessment Scales (RIAS) & des Reynolds Intellectual Screening Test (RIST) von Cecil R. Reynolds und Randy W. Kamphaus: Manual. Bern: Verlag Hans Huber.
Halvorsen, M., Mathiassen, B., Amundsen, T., Ellingsen, J., Brøndbo, P. H., Sundby, J., et al. (2019). Confirmatory factor analysis of the behavior rating inventory of executive function in a neuro-pediatric sample and its application to mental disorders. Child Neuropsychol. 25, 599–616. doi: 10.1080/09297049.2018.1508564
Han, G., Helm, J., Iucha, C., Zahn-Waxler, C., Hastings, P. D., and Klimes-Dougan, B. (2016). Are executive functioning deficits concurrently and predictively associated with depressive and anxiety symptoms in adolescents? J. Clini. Child Adoles. Psychol. 45, 44–58. doi: 10.1080/15374416.2015.1041592
Hayes, A. (2018). Introduction to Mediation, Moderation, and Conditional Process Analysis, Second Edition (Methodology in the Social Sciences, 2nd Edn. New York: The Guildford Press.
Houston, R. J., Ceballos, N. A., Hesselbrock, V. M., and Bauer, L. O. (2005). Borderline personality disorder features in adolescent girls: P300 evidence of altered brain maturation. Child Neurophysiol. 116, 1424–1432.
Johnson, J. G., Cohen, P., Kasen, S., Skodol, A. E., and Oldham, J. M. (2008). Cumulative prevalence of personality disorders between adolescence and adulthood. Acta Psychiatrica Scand. 118, 410–413. doi: 10.1111/j.1600-0447.2008.01231.x
Jones, J. D., Boyd, R. C., Calkins, M. E., Ahmed, A., Moore, T. M., Barzilay, R., et al. (2019). Parent-adolescent agreement about adolescents’ suicidal thoughts. Pediatrics 143:e20181771. doi: 10.1542/peds.2018-1771
Jónsdóttir, H., Agnarsdóttir, H., Jóhannesdóttir, H., Smárason, O., Harðardóttir, H. H., Højgaard, D. R. M. A., et al. (2021). Parent–youth agreement on psychiatric diagnoses and symptoms: results from an adolescent outpatient clinical sample. Nordic J. Psychiatry 76, 466–473.
Kaess, M., Brunner, R., and Chanen, A. (2014). Borderline personality disorder in adolescence. Pediatrics 134, 782–793.
Kaess, M., Herpertz, S. C., and Plener, P. L. (2020). Borderline-persönlichkeitsstörungen. Zeitschrift Für Kinder- Und Jugendpsychiatrie Und Psychotherapie 48, 435–439.
Kalpakci, A., Ha, C., and Sharp, C. (2018). Differential relations of executive functioning to borderline personality disorder presentations in adolescents. Pers. Mental Health 12, 93–106. doi: 10.1002/pmh.1410
Kaufman, J., Birmaher, B., Brent, D., Rao, U., Flynn, C., Moreci, P., et al. (1997). Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J. Am. Acad. Child Adolesc. Psychiatry 36, 980–988. doi: 10.1097/00004583-199707000-00021
Kazdin, A. E., French, N. H., and Uni, A. S. (1983). Child, mother, and father evaluations of depression in psychiatric inpatient children. J. Abnormal Child Psychol. 11, 167–180. doi: 10.1007/BF00912083
Keller, F., Grieb, J., Ernst, M., Spröber, N., Fegert, J. M., and Kölch, M. (2011). Children’s depression rating scale-revised (CDRS-R) - entwicklung einer deutschen version und psychometrische gütekriterien in einer klinischen stichprobe. Zeitschrift Fur Kinder- Und Jugendpsychiatrie Und Psychotherapie 39, 179–185.
Keller, F., Grieb, J., Kölch, M., and Spröber, N. (2012). CDRS-C Children’s Depression Rating Scale – Revised by E. O. Poznanski and H. B. Mokros, 1st Edn. Boston, MA: Hogrefe.
Konrad, K., Firk, C., and Uhlhaas, P. J. (2013). Brain development during adolescence. Deutsches Ärzteblatt Int. 110, 425–431. doi: 10.3238/arztebl.2013.0425
Koo, T. K., and Li, M. Y. (2016). A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropractic Med. 15, 155–163. doi: 10.1016/j.jcm.2016.02.012
Krasny-Pacini, A., Limond, J., Evans, J., Hiebel, J., Bendjelida, K., and Chevignard, M. (2015). No TitleSelf-awareness assessment during cognitive rehabilitation in children with acquired brain injury: a feasibility study and proposed model of child anosognosia. Disabil. Rehabil. Int., Multidisciplinary J. 37, 2092–2106. doi: 10.3109/09638288.2014.998783
Kröger, C., Andrea, del Pozo, M., Kosfelder, J., Allroggen, M., Grabowski, G., et al. (2017). Erfassung von Impulsivität und emotionaler Dysregulation bei Jugendlichen mit Borderline- Persönlichkeitsstörung. Diagnostica 63, 297–308.
Kröger, C., and Kosfelder, J. (2011). IES-27 - Skala zur Erfassung der Impulsivität und Emotionalen Dysregulation der Borderline-Persönlichkeitsstörung. Boston, MA: Hogrefe.
Lalovic, A., Wang, S., Keilp, J. G., Bowie, C. R., Kennedy, S. H., and Rizvi, S. J. (2022). A qualitative systematic review of neurocognition in suicide ideators and attempters: implications for cognitive-based psychotherapeutic interventions. Neurosci. Biobehav. Rev. 132, 92–109. doi: 10.1016/j.neubiorev.2021.11.007
Lara, E., Olaya, B., Garin, N., Ayuso-Mateos, J. L., Miret, M., Moneta, V., et al. (2015). Is cognitive impairment associated with suicidality? a population-based study. Eur. Neuropsychopharmacol. 25, 203–213. doi: 10.1016/j.euroneuro.2014.08.010
Lieb, K., Zanarini, M. C., Schmahl, C., Linehan, P. M. M., and Bohus, P. M. (2004). Borderline personality disorder. Lancet 364, 453–461.
Luciana, M. (2013). Adolescent brain development in normality and psychopathology. Dev. Psychopathol. 25, 1325–1345. doi: 10.1017/S0954579413000643
Luciana, M. (2016). Executive function in adolescence: a commentary on regulatory control and depression in adolescents: findings from neuroimaging and neuropsychological research. J. Clin. Child Adolesc. Psychol. 45, 84–89. doi: 10.1080/15374416.2015.1123638
Madjar, N., Mansbach-Kleinfeld, I., Daeem, R., Farbstein, I., Apter, A., Fennig, S., et al. (2020). Discrepancies in adolescent-mother dyads’ reports of core depression symptoms: association with adolescents’ help-seeking in school and their somatic complaints. J. Psychosomatic Res. 137:110222. doi: 10.1016/j.jpsychores.2020.110222
Makol, B. A., and Polo, A. J. (2017). Parent-child endorsement discrepancies among youth at chronic-risk for depression. J. Abnormal Child Psychol. 46, 1077–1088. doi: 10.1007/s10802-017-0360-z
McCandless, S., and O’Laughlin, L. (2007). The clinical utility of the behavior rating inventory of executive function (BRIEF) in the diagnosis of ADHD. J. Attention Disord. 10, 381–389.
McClure, G., Hawes, D. J., and Dadds, M. R. (2016). Borderline personality disorder and neuropsychological measures of executive function: a systematic review. Pers. Mental Health 10, 43–57.
McGraw, K. O., and Wong, S. P. (1996). Forming inferences about some intraclass correlation coefficients. Psychol. Methods 1, 30–46.
Miller, A. L., Muehlenkamp, J. J., and Jacobson, C. M. (2008). Fact or fiction: diagnosing borderline personality disorder in adolescents. Clin. Psychol. Rev. 28, 969–981.
Mills, K. L., Dumontheil, I., Speekenbrink, M., and Blakemore, S. J. (2015). Multitasking during social interactions in adolescence and early adulthood. Royal Soc. Open Sci. 2:150117. doi: 10.1098/rsos.150117
Miyake, A., Friedman, N. P., Emerson, M. J., Witzki, A. H., Howerter, A., and Wager, T. D. (2000). The unity and diversity of executive functions and their contributions to complex “frontal lobe” tasks: a latent variable analysis. Cogn. Psychol. 41, 49–100. doi: 10.1006/cogp.1999.0734
Orchard, F., Pass, L., Cocks, L., Chessell, C., and Reynolds, S. (2019). Examining parent and child agreement in the diagnosis of adolescent depression. Child Adolesc. Mental Health 24, 338–344.
Ortuño-Sierra, J., Aritio-Solana, R., del Casal, A. D. G., and Fonseca-Pedrero, E. (2020). Neurocognitive functioning in adolescents at risk for suicidal behaviors. Arch. Suicide Res. 25, 657–671.
Pagnoni, I., Gobbi, E., Alaimo, C., Campana, E., Rossi, R., Manenti, R., et al. (2022). The relationship between theory of mind and executive functions in major depressive disorders: a review. Front. Psychiatry 13:980392. doi: 10.3389/fpsyt.2022.980392
Pasqualotto, A., Mazzoni, N., Bentenuto, A., Mulè, A., Benso, F., and Venuti, P. (2021). Effects of cognitive training programs on executive function in children and adolescents with autism spectrum disorder: a systematic review. Brain Sci. 11:1280.
Pham-Scottez, A. (2016). Eurnet-BPD: un reseau de recherche avec des adolescents borderline. Information Psychiatrique 92, 29–37. doi: 10.1521/pedi_2021_35_523
Polanczyk, G., Salum, G., Sugaya, L., Caye, A., and Rhode, L. (2015). Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J. Child Psychol. Psychiatry 56, 345–365.
Poznanski, E. O., Freeman, L. N., and Mokros, H. B. (1996). Children’s Depression Rating Scale-Revised (CDRS-R). Los Angeles, CA: Western Psychological Services.
Puhr, A., Ruud, E., Anderson, V., Due-Tønnesen, B. J., Skarbø, A. B., Finset, A., et al. (2019). Self-reported executive dysfunction, fatigue, and psychological and emotional symptoms in physically well-functioning long-term survivors of pediatric brain tumor. Dev. Neuropsychol. 44, 88–103.
R Core Team (2022). R: a Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing.
Rao, S., and Broadbear, J. (2019). Borderline personality disorder and depressive disorder. Australas. Psychiatry 27, 573–577.
Reynolds, C. R., and Kamphaus, R. W. (2003). Reynolds Intellectual Assessment Scales and Reynolds Intellectual Screening Test Professional Manual. Florida: Psychological Assessment Resources.
Rizzo, P., Steinhausen, H.-C., and Drechsler, R. (2012). Selbst- und Fremdwahrnehmung von Beeinträchtigungen exekutiver Funktionen bei Erwachsenen mit ADHSNo Title. Psychiatrie Psychol. Psychotherapie 60, 131–143.
Romer, A. L., and Pizzagalli, D. A. (2021). Is executive dysfunction a risk marker or consequence of psychopathology? a test of executive function as a prospective predictor and outcome of general psychopathology in the adolescent brain cognitive development study®. Dev. Cogn. Neurosci. 51:100994.
Roth, R. M., Isquith, P. K., and Gioia, G. A. (2005). BRIEF-A: Behavior rating inventory of executive function- adult version: Professional manual. Lutz, FL: Psychological Assessment Resources.
Sansone, R. A., and Sansone, L. A. (2011). Gender patterns in borderline personality disorder. Innovat. Clin. Neurosci. 8, 16–20.
Schmid, M., and Hammar, Å (2021). First-episode patients report cognitive difficulties in executive functioning 1 year after initial episode of major depressive disorder. Front. Psychiatry 12:667238. doi: 10.3389/fpsyt.2021.667238
Schuppert, M., Timmerman, M. E., Bloo, J., Van Gemert, T. G., Wiersema, H. M., Minderaa, R. B., et al. (2012). Emotion regulation training for adolescents with borderline personality disorder traits: a randomized controlled trial. J. Am. Acad. Child Adolesc. Psychiatry 51, 1314–1323. doi: 10.1016/j.jaac.2012.09.002
Schwert, C., Stohrer, M., Aschenbrenner, S., Weisbrod, M., and Schröder, A. (2018). Biased neurocognitive self-perception in depressive and in healthy persons. J. Affect. Disord. 232, 96–102. doi: 10.1016/j.jad.2018.02.031
Serra-Blasco, M., Torres, I. J., Vicent-Gil, M., Goldberg, X., Navarra-Ventura, G., Aguilar, E., et al. (2019). Discrepancy between objective and subjective cognition in major depressive disorder. Eur. Neuropsychopharmacol. 29, 46–56. doi: 10.1016/j.euroneuro.2018.11.1104
Soloff, P. H., Abraham, K., Burgess, A., Ramaseshan, K., Chowdury, A., and Diwadkar, V. A. (2017). Impulsivity and aggression mediate regional brain responses in borderline personality disorder: an fMRI study. Psychiatry Res. Neuroimaging 260, 76–85. doi: 10.1016/j.pscychresns.2016.12.009
Stein, S. F., Ngo, Q. M., Austic, E. A., Veliz, P., McCabe, S. E., and Boyd, C. B. (2018). The clinical relevance of divergence in adolescent–parent reports of adolescent depression and anxiety. Child Adolesc. Soc. Work J. 35, 611–623.
Stordal, K. I., Lundervold, A. J., Egeland, J., Mykletun, A., Asbjørnsen, A., Landrø, N. I., et al. (2004). Impairment across executive functions in recurrent major depression. Nordic J. Psychiatry 58, 41–47. doi: 10.1080/08039480310000789
Toplak, M. E., Sorge, G. B., Benoit, A., West, R. F., and Stanovich, K. E. (2010). Decision-making and cognitive abilities: a review of associations between iowa gambling task performance, executive functions, and intelligence. Clin. Psychol. Rev. 30, 562–581. doi: 10.1016/j.cpr.2010.04.002
Tran, T., Hagen, A. E. F., Hollenstein, T., and Bowie, C. R. (2021). Physical- and cognitive-effort-based decision-making in depression: relationships to symptoms and functioning. Clin. Psychol. Sci. 9, 53–67. doi: 10.1017/S0033291722000964
Upton, P., Lawford, J., and Eiser, C. (2008). Parent-child agreement across child health-related quality of life instruments: a review of the literature. Quality Life Res. 17, 895–913. doi: 10.1007/s11136-008-9350-5
van der Ende, J., Verhulst, F. C., and Tiemeier, H. (2012). Agreement of informants on emotional and behavioral problems from childhood to adulthood. Psychol. Assess. 24, 293–300. doi: 10.1037/a0025500
Vesco, A. T., Young, A. S., Arnold, L. E., Fristad, M. A., and Health, B. (2018). Omega-3 supplementation associated with improved parent- rated executive function in youth with mood disorders: secondary analyses of the Omega 3 and therapy (OATS) trials anthony. J. Child Psychol. Psychiatry 59, 628–636. doi: 10.1111/jcpp.12830
Vierhaus, M., Rueth, J. E., and Lohaus, A. (2018). The observability of problem behavior and its relation to discrepancies between adolescents’ self-report and parents’ proxy report on problem behavior. Psychol. Assess. 30, 669–677. doi: 10.1037/pas0000515
Vilgis, V., Silk, T. J., and Vance, A. (2015). Executive function and attention in children and adolescents with depressive disorders: a systematic review. Eur. Child Adolesc. Psychiatry 24, 365–384. doi: 10.1007/s00787-015-0675-7
Wagner, S., Doering, B., Helmreich, I., Lieb, K., and Tadić, A. (2012). A meta-analysis of executive dysfunctions in unipolar major depressive disorder without psychotic symptoms and their changes during antidepressant treatment. Acta Psychiatrica Scand. 125, 281–292. doi: 10.1111/j.1600-0447.2011.01762.x
Wagner, S., Müller, C., Helmreich, I., Huss, M., and Tadić, A. (2015). A meta-analysis of cognitive functions in children and adolescents with major depressive disorder. Eur. Child Adolesc. Psychiatry 24, 5–19. doi: 10.1007/s00787-014-0559-2
Wante, L., Mezulis, A., Van Beveren, M. L., and Braet, C. (2017). The mediating effect of adaptive and maladaptive emotion regulation strategies on executive functioning impairment and depressive symptoms among adolescents. Child Neuropsychol. 23, 935–953. doi: 10.1080/09297049.2016.1212986
Keywords: executive function, major depressive disorder, borderline personality disorder, adolescents, emotion regulation, inhibition
Citation: Albermann M, Emery S, Baumgartner N, Strumberger M, Erb S, Wöckel L, Müller-Knapp U, Rhiner B, Contin-Waldvogel B, Bachmann S, Schmeck K, Berger G, the Omega-3 Study Team and Häberling I (2023) Executive functions and borderline personality features in adolescents with major depressive disorder. Front. Hum. Neurosci. 17:957753. doi: 10.3389/fnhum.2023.957753
Received: 31 May 2022; Accepted: 26 May 2023;
Published: 22 June 2023.
Edited by:
Björn Albrecht, Philipps-University, GermanyReviewed by:
Joel Paris, McGill University, CanadaJosé C. García Alanis, Philipps University of Marburg, Germany
Copyright © 2023 Albermann, Emery, Baumgartner, Strumberger, Erb, Wöckel, Müller-Knapp, Rhiner, Contin-Waldvogel, Bachmann, Schmeck, Berger, the Omega-3 Study Team and Häberling. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mona Albermann, mona.albermann@pukzh.ch
 Mona Albermann
Mona Albermann Sophie Emery1
Sophie Emery1  Silke Bachmann
Silke Bachmann Klaus Schmeck
Klaus Schmeck Gregor Berger
Gregor Berger Isabelle Häberling
Isabelle Häberling