Improved clinical outcomes in response to a 12-week blended digital and community-based long-COVID-19 rehabilitation programme
- 1Nuffield Health, Epsom, United Kingdom
- 2Department of Health Sciences, University of York, York, United Kingdom
- 3School of Sport and Exercise Sciences, Liverpool John Moores University, Liverpool, United Kingdom
- 4National Centre for Sport and Exercise Medicine, Loughborough University, Loughborough, United Kingdom
- 5NIHR Leicester Biomedical Research Centre, University Hospitals of Leicester NHS Trust, University of Leicester, Leicester, United Kingdom
- 6Department of Health Professions, Faculty of Health and Education, Manchester Metropolitan University, Manchester, United Kingdom
Introduction: Two million people in the UK are experiencing long COVID (LC), which necessitates effective and scalable interventions to manage this condition. This study provides the first results from a scalable rehabilitation programme for participants presenting with LC.
Methods: 601 adult participants with symptoms of LC completed the Nuffield Health COVID-19 Rehabilitation Programme between February 2021 and March 2022 and provided written informed consent for the inclusion of outcomes data in external publications. The 12-week programme included three exercise sessions per week consisting of aerobic and strength-based exercises, and stability and mobility activities. The first 6 weeks of the programme were conducted remotely, whereas the second 6 weeks incorporated face-to-face rehabilitation sessions in a community setting. A weekly telephone call with a rehabilitation specialist was also provided to support queries and advise on exercise selection, symptom management and emotional wellbeing.
Results: The 12-week rehabilitation programme significantly improved Dyspnea-12 (D-12), Duke Activity Status Index (DASI), World Health Orginaisation-5 (WHO-5) and EQ-5D-5L utility scores (all p < 0.001), with the 95% confidence intervals (CI) for the improvement in each of these outcomes exceeding the minimum clinically important difference (MCID) for each measure (mean change [CI]: D-12: −3.4 [−3.9, −2.9]; DASI: 9.2 [8.2, 10.1]; WHO-5: 20.3 [18.6, 22.0]; EQ-5D-5L utility: 0.11 [0.10, 0.13]). Significant improvements exceeding the MCID were also observed for sit-to-stand test results (4.1 [3.5, 4.6]). On completion of the rehabilitation programme, participants also reported significantly fewer GP consultations (p < 0.001), sick days (p = 0.003) and outpatient visits (p = 0.007) during the previous 3 months compared with baseline.
Discussion: The blended and community design of this rehabilitation model makes it scalable and meets the urgent need for an effective intervention to support patients experiencing LC. This rehabilitation model is well placed to support the NHS (and other healthcare systems worldwide) in its aim of controlling the impacts of COVID-19 and delivering on its long-term plan.
Clinical trial registration: https://www.isrctn.com/ISRCTN14707226, identifier 14707226.
Introduction
COVID-19 is a highly infectious respiratory disease that has elicited catastrophic health, care and economic effects. Officially declared as a global pandemic by the World Health Organization (WHO) in March 2020, there have since been 523 million cases of COVID-19, of which six million cases have resulted in death (as of May 2022) (1). Though the majority of patients recover from acute COVID-19 infection, it is now evident that survivors are at risk of suffering further long-term adverse side effects (2). Prolonged complications of COVID-19, or “long-COVID,” is defined by the National Institute for Health and Care Excellence (NICE) as “a set of persistent physical, cognitive and/or psychological symptoms that continue for more than 12 weeks after illness and which are not explained by an alternative diagnosis” (3).
The most frequently reported symptoms of long COVID (LC) include breathlessness and fatigue, as well as impaired pulmonary function and reductions in health-related quality of life (HR-QoL) (4, 5). In May 2022, it was estimated that two million people in the UK were experiencing LC (6), of which 1.4 million people reported that their day-to-day activities were adversely effected. While some symptoms of LC ease over time, research demonstrates that certain symptoms such as dyspnea and weakness are repeatedly evident up to a year post-infection. The risk for lingering LC symptoms is higher in adults aged 41–60 and >60 years as well as in those who were unvaccinated against COVID-19 (7). To date, evidence-based guidelines do not exist for the treatment of LC and its associated complications, with NICE highlighting the need for effective interventions to manage this condition (3). Outpatient pulmonary rehabilitation, a multi-component exercise and education programme for patients with chronic lung disease, has now been shown effective in improving the symptoms of LC (2). However, a scalable solution, enrolled via a community rehabilitation setting, is required due to the large number of people experiencing this condition and to reduce strain on an already pressured healthcare system.
The purpose of this study was to assess the clinical effectiveness of a novel 12-week blended community rehabilitation programme for individuals experiencing LC. These are the first results from a scalable rehabilitation programme for participants presenting with LC. The findings demonstrate substantial improvements in LC symptoms and suggest that this rehabilitation model can support the NHS (and other healthcare systems worldwide) in its aim of controlling the impacts of COVID-19 and delivering on its long-term plan.
Materials and methods
Study design and participants
This study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures were approved by the Ethics Advisory Committee at Manchester Metropolitan University (Ref: 25307). Participants were able to enroll into the rehabilitation programme online via self-referral or referral from an NHS practitioner. Following enrollment, participants underwent triage with a physiotherapist to assess eligibility for inclusion in the study. Eligible participants were then assigned a start date for the programme.
All participants reported in this manuscript provided written informed consent for the inclusion of outcomes data in external publications.
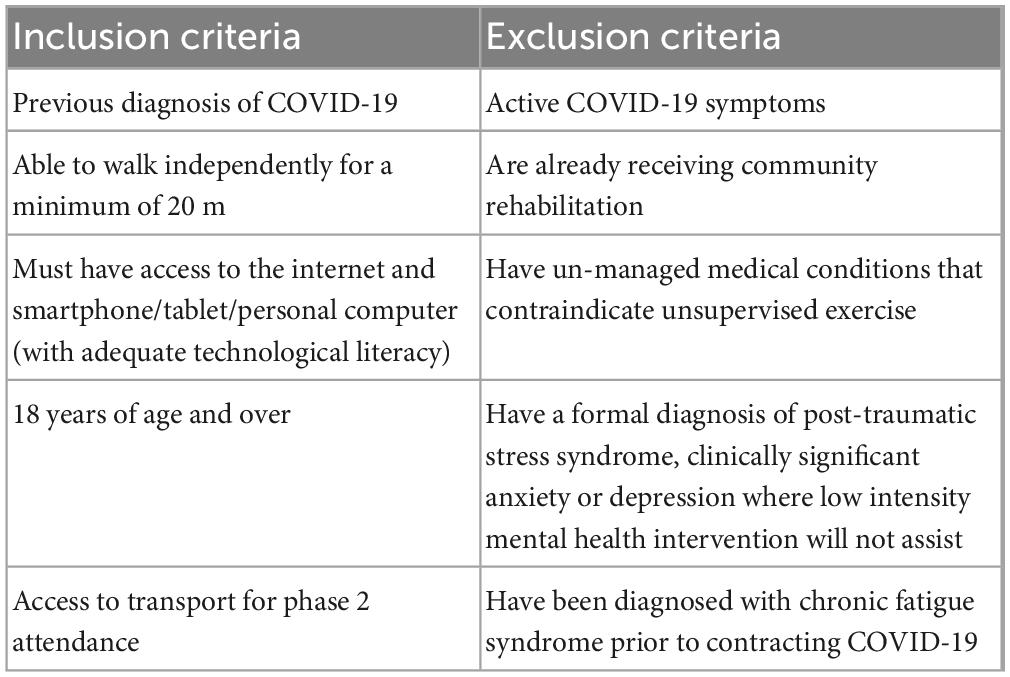
This service evaluation used baseline and follow-up data (at 12 weeks) from 601 people with LC undertaking the Nuffield Health COVID-19 Rehabilitation Programme between February 2021 and March 2022. This trial is registered at the ISRCTN Registry (ID: 14707226). A full overview of inclusion and exclusion criteria is provided in Table 1.
Rehabilitation programme
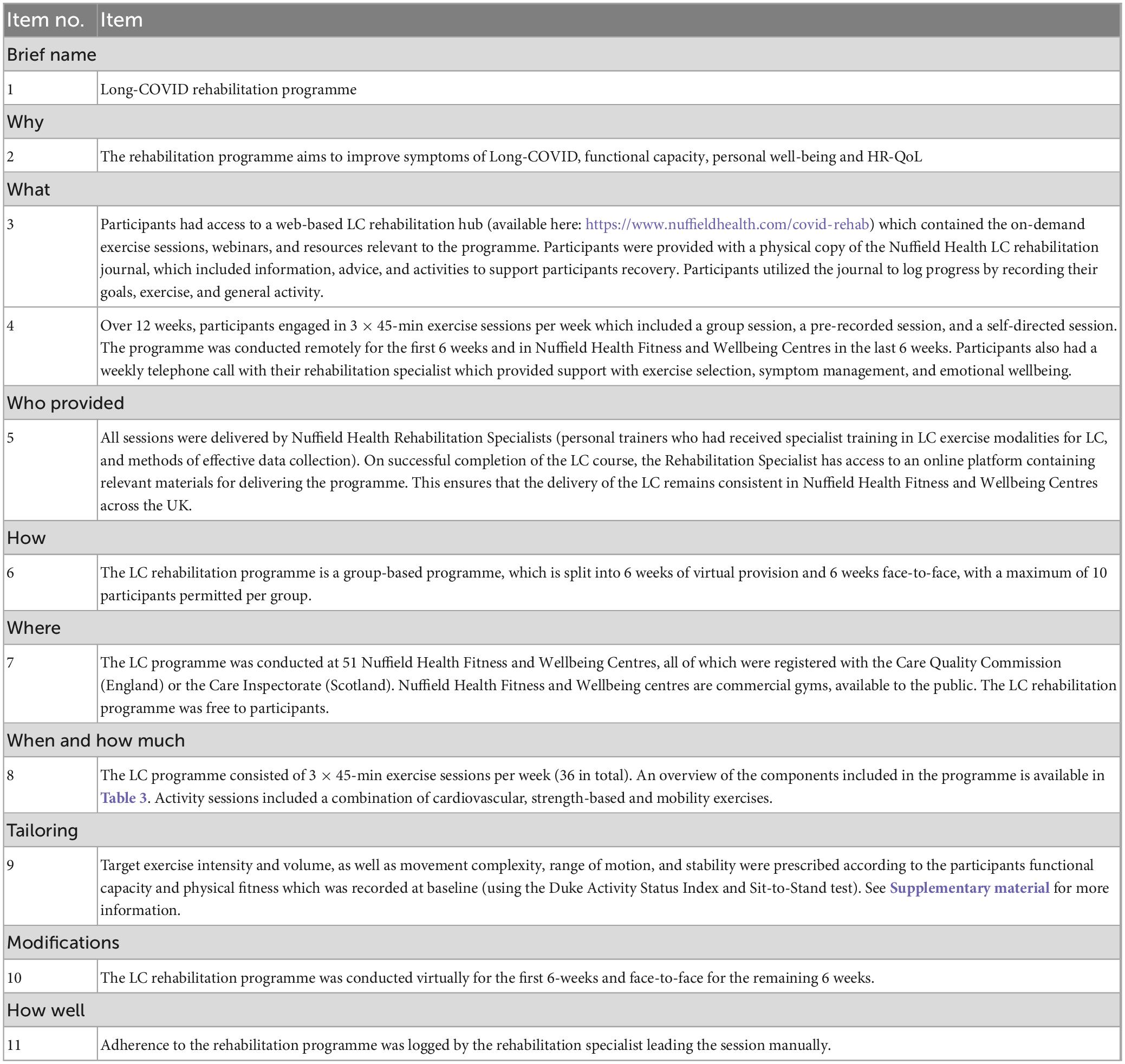
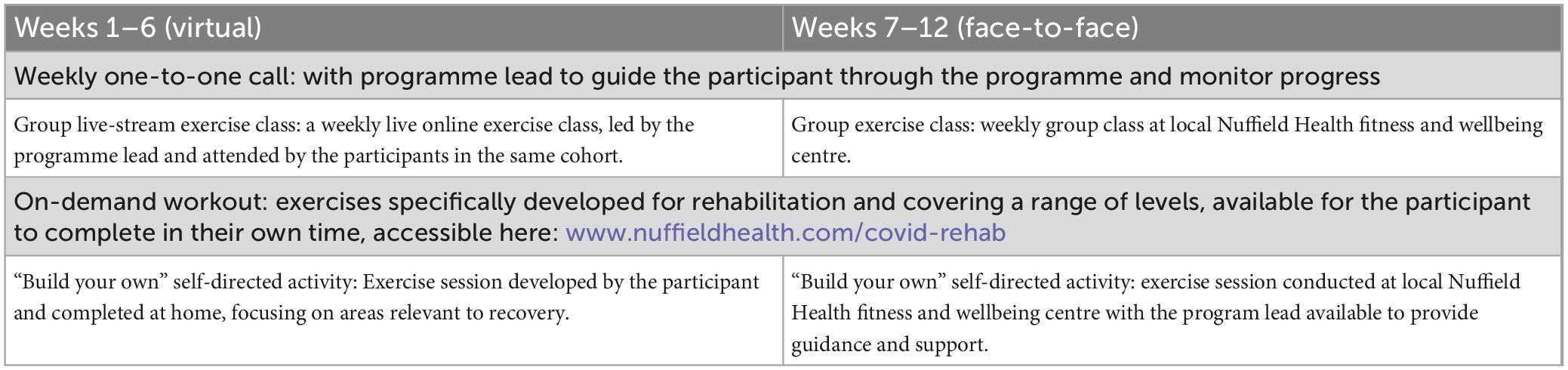
The LC rehabilitation programme aims to improve symptoms of LC, functional capacity, personal well-being and HR-QoL. The LC rehabilitation programme is a 12-week, group-based programme split into two 6-week phases consisting of 3 × 45-min exercise sessions per week and continued support from a programme lead, with a maximum of 10 participants per group. Table 2 details the intervention according to the Template for Intervention Description and Replication checklist.
Throughout the 12-week programme participants completed three exercise sessions per week: (1) group rehabilitation exercise session lasting 45 min; (2) on-demand exercise session lasting 45 min, using a pre-recorded guided exercise session located on a dedicated online platform (Vimeo, New York, USA); (3) a “build your own” exercise session whereby participants selected from a menu of activities provided within their rehabilitation workbook to populate a session commensurate with their personal threshold. An overview of the components included in the 12-week programme are presented in Table 3.
The first phase of the programme was conducted remotely in Weeks 1–6. The group exercise session was performed via an online live-streaming platform (Microsoft Teams®), with the programme lead delivering the session.
This session was immediately followed by a 15-min period for further questions using either the online chat function or device microphones. In accordance with the remote nature of the first phase of the rehabilitation programme, participants completed the on-demand exercise session and the “build your own” exercise session from their own homes.
The second phase of the programme was conducted in Weeks 7–12 and incorporated face-to-face rehabilitation sessions. This was achieved by conducting the group rehabilitation exercise sessions on-site at the respective Nuffield Health Fitness and Wellbeing Centre. Although the structure of the sessions remained the same as during Phase 1 of the programme, the face-to-face nature enabled two-way interaction with the rehabilitation specialist leading the session, as well as with fellow participants to foster a supportive environment. The on-demand exercise session remained as a remote aspect of the programme throughout Weeks 7–12 of the programme. Participants were encouraged to complete their “build your own” rehabilitation session within a supervised gym environment, with the rehabilitation specialist available to offer advice and guidance.
All activity sessions included a combination of cardiovascular, strength-based, and mobility exercises. Exercise intensity and volume, as well as movement complexity, range of motion and stability were prescribed according to the participants functional capacity and physical fitness, which was recorded at baseline (see Supplementary material for further information). Following exercise sessions, participants were advised to record their perceived effort score on a scale which ranged from 0 (no effort) to 10 (extremely hard). Self-recording exercise effort allowed for participants to monitor their progress and adjust effort accordingly over the 12-week programme. Participants were also encouraged to progress movement complexity, range of motion, stability, and volume where possible.
Participants also received a weekly telephone call with a rehabilitation specialist lasting up to 45 min to support with any queries on the programme and provide advice on exercise selection, symptom management and emotional wellbeing. Participants had access to a web-based LC rehabilitation hub1 which contained the on-demand exercise sessions, webinars, and resources relevant to the programme. Participants were provided with a printed copy of the Nuffield Health LC rehabilitation journal which contained information on physical and emotional wellbeing, and an activity record to log exercise sessions completed each week.
The LC programme was conducted at 51 Nuffield Health Fitness and Wellbeing Centres, all of which were registered with the Care Quality Commission (England) or the Care Inspectorate (Scotland). Nuffield Health Fitness and Wellbeing centres are commercial gyms, available to the public. The LC rehabilitation programme was free to participants.
Full details of the rehabilitation programme are provided in the published study protocol (8).
Training of rehabilitation specialists
All sessions were delivered by Nuffield Health Rehabilitation Specialists (personal trainers who had received specialist training in LC exercise modalities for LC, and methods of effective data collection). On successful completion of the LC course, the Rehabilitation Specialist has access to an online platform containing relevant materials for delivering the programme. This ensures that the delivery of the LC remains consistent in Nuffield Health Fitness and Wellbeing Centres across the UK.
Measures
Outcome data were collected for all participants at baseline and on completion of the rehabilitation programme at Week 12 via a digital application (MyWellbeing, Nuffield Health, London, UK). Data were objectively measured by the Rehabilitation Specialist or self-reported and stored on a web-based platform (Lumeon, London, UK).
Dyspnea
Breathlessness was measured using the Dyspnea-12 tool (D-12) (9). The D-12 assesses multiple breathless sensations within a single instrument. Total scores from the D-12 range from 0 to 36, with higher scores corresponding to greater severity of breathlessness.
Functional capacity
Functional capacity was assessed using the Duke Activity Status Index (DASI) (10). The DASI produces a score between 0 and 58.2 points, with higher scores indicating a higher functional status.
Physical fitness
Physical fitness was assessed using the 30-s sit-to-stand test (11). The 30-s sit-to-stand test involves recording the number of stands a person can complete in 30 s. Higher scores indicate a greater fitness level.
Mental wellbeing
Mental wellbeing was assessed using The World Health Organization- Five Well-Being Index (WHO-5) (12). The WHO-5 is a short, generic global rating score which measures subjective wellbeing. The WHO-5 produces a score between 0 and 25 which is translated to a percentage scale from 0 (absence of wellbeing) to 100 (maximal wellbeing).
Health status
Health status was assessed using the EuroQoL Five Dimension Five Level (EQ-5D-5L) and visual analog scale (VAS) (13). The descriptive system consists of five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Patients indicate their health state by ticking the box next to the appropriate statement: no problems, slight problems, moderate problems, severe problems, and extreme problems. The EQ-5D-5L scores were mapped to utility values in accordance with the England-specific valuation set (14). The EQ VAS records health on a vertical VAS, where the endpoints are labeled “The best health you can imagine” for a score of 100 and “The worst health that you can imagine” for a score of 0.
Illness burden
At baseline and Week 12, participants also reported the number of general practitioner (GP) consultations, outpatient hospital episodes, inpatient hospital episodes and days absent from work due to illness (“sick days”) experienced during the past 3-months (for participants who were engaged in employment at baseline). This enabled a comparison of illness burden during the rehabilitation programme compared with the preceding 3-month period.
Statistical analysis
The primary analyses were conducted in 601 participants who completed the LC rehabilitation programme and provided outcome measures at Week 0 and 12. A subgroup of 539 participants provided D-12, DASI, WHO-5, EQ-5D-5L and sit-to-stand test outcomes at the midpoint of the intervention. The outcomes for these participants were analyzed at Weeks 0, 6, and 12 to understand the time-course of changes in response to the programme.
Graphical representations of the results are provided as mean (95% confidence interval [CI]). Descriptions of data in the text for individual timepoints are provided as mean (SD), with the difference between timepoints provided as mean (95% CI). Paired samples t-tests were used to determine significant differences between timepoints. Additionally, the 95% CIs of differences between timepoints were compared against the minimum clinically important difference (MCID) thresholds identified for relevant outcomes from the wider research literature. Where the 95% CIs of a difference between timepoints exceeded the MCID, this demonstrated that the change was significantly greater than the MCID. Two-sided 95% CIs were used for all analyses and all significance tests were performed at the 5% alpha level.
The MCID for each outcome was obtained from the research literature, as follows: D-12 score (2.83 points) (15), WHO-5 score (10 points) (16), EQ-5D-5L utility (0.05 points) (17), EQ-5D VAS (7 points) (17), sit-to-stand score (2 points) (11). To the authors’ knowledge a MCID is not established for DASI score; consequently, a threshold of 5 points was used based on this representing a significant difference in score between patients who did versus did not suffer 1-year new disability or death after non-cardiac surgery (18).
All analyses were performed using R version 4.1.2 (19).
Results
Complete case analysis was conducted for the 601 participants who completed the Nuffield Health COVID-19 Rehabilitation Programme and provided the relevant outcome measures at Weeks 0 and 12.
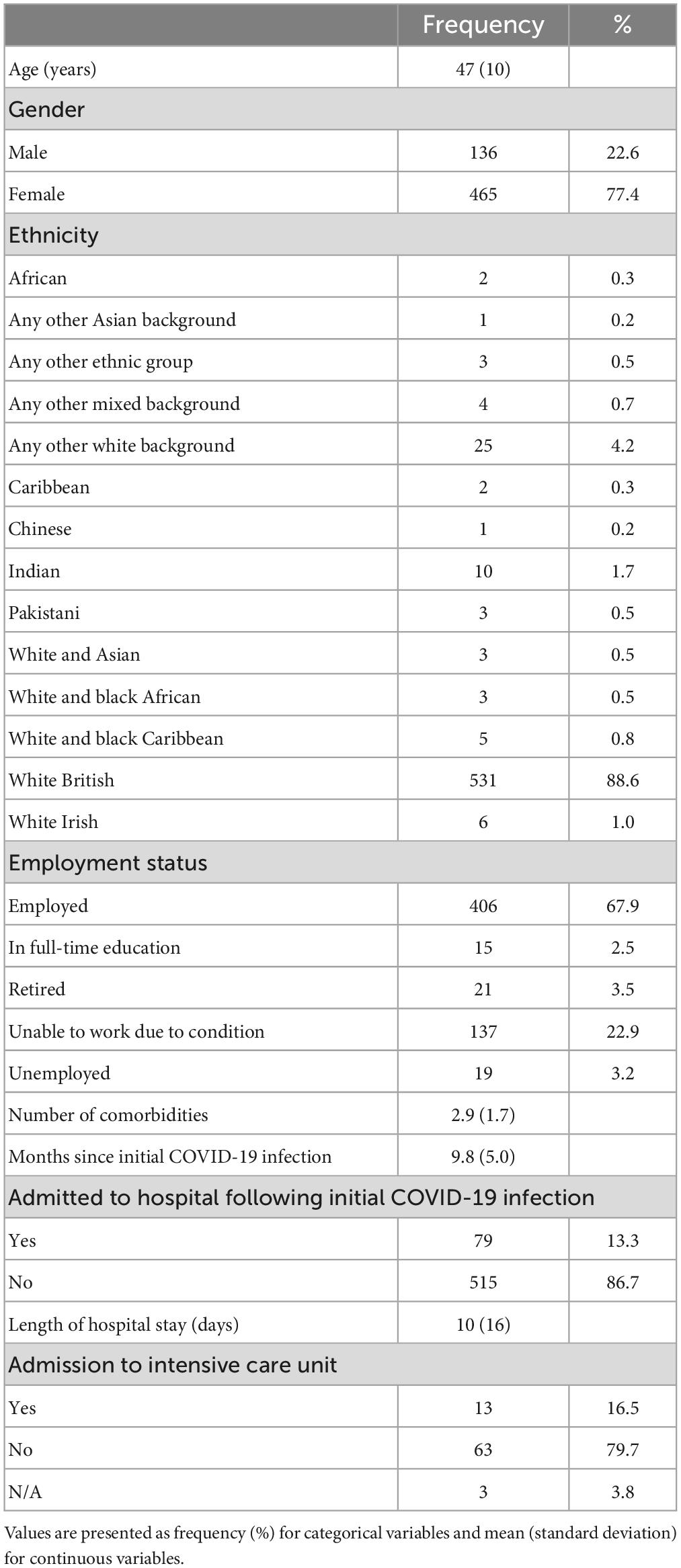
Participant characteristics
All participants had been previously diagnosed with COVID-19 and were currently experiencing symptoms of LC, with a mean period of 9.8 (SD 5.0) months between COVID-19 diagnosis and commencing the rehabilitation programme. During COVID-19 infection 13.3% of participants were admitted to hospital, with a mean hospital stay duration of 10 (SD 16) days and 16.5% of these participants being admitted to an intensive care unit. On programme enrollment, participants had a mean age of 47 (SD 10) years and 2.9 (SD 1.7) comorbidities. The majority of participants were female (77.4%) and of White British ethnicity (88.6%). Participant characteristics are presented in Table 4.
The 12-week rehabilitation programme significantly improved D-12, DASI, WHO-5 and EQ-5D-5L utility values (Figure 1; all p < 0.001). Additionally, the 95% CIs for the improvement in each of these outcomes exceeding the MCID for each measure (mean change [CI]: D-12: −3.4 [−3.9, −2.9]; DASI: 9.2 [8.2, 10.1]; WHO-5: 20.3 [18.6, 22.0]; EQ-5D-5L utility: 0.11 [0.10, 0.13]). Significant improvements in EQ-5D VAS (Week 0: 47.5 [20.6]; Week 12: 62.2 [23.6]; p < 0.001) and sit-to-stand test results (Week 0: 11.5 [4.8]; Week 12: 15.6 [6.1]; p < 0.001) were also observed, with the 95% Cis of the improvements exceeding the MCID for each measure (EQ5D VAS: 14.7 [12.6, 16.9]; sit-to-stand test: 4.1 [3.5, 4.6]).
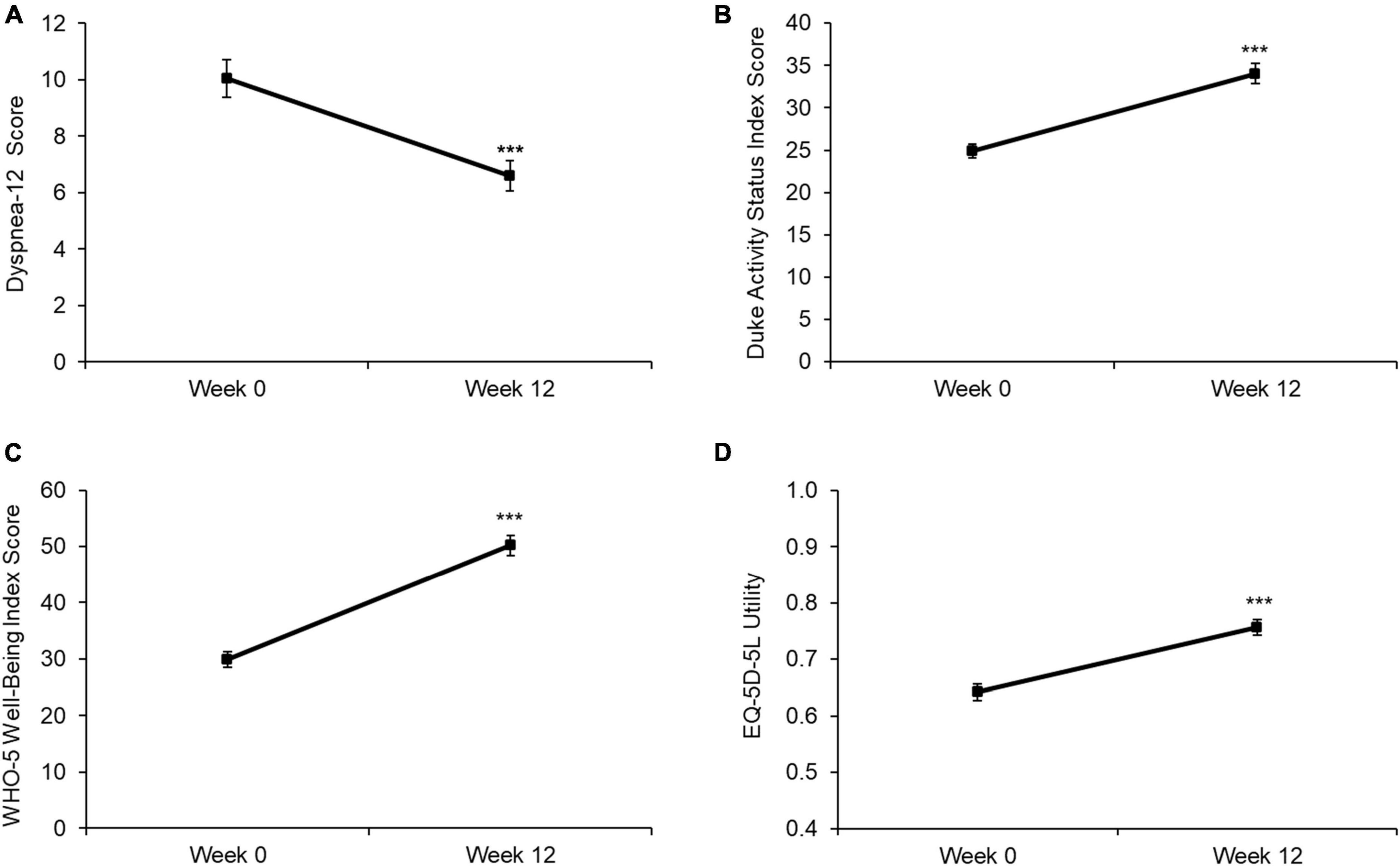
Figure 1. Baseline and Week 12 values for (A) D-12 score, (B) DASI score, (C) WHO-5 score, and (D) EQ-5D-5L utility. Values are presented as mean (95% CI). Higher scores indicate a worse health state for D-12, while lower scores indicate a worse health state for DASI, WHO-5, and EQ5D. Differences between time points were analyzed using paired t-tests. ***p < 0.001. D12 score: n = 598; DASI score: n = 594; WHO-5 score: n = 600; EQ5D utility: n = 600.
On completion of the rehabilitation programme, participants reported significantly fewer GP consultations (Figure 2A; p < 0.001), sick days (Figure 2B; p = 0.003) and outpatient visits (Figure 2C; p = 0.007) during the previous 3 months compared with baseline. The number of inpatient episodes experienced during the past 3 months did not change in response to the rehabilitation programme but was limited by the small number of episodes at baseline (Figure 2D; p = 0.235).
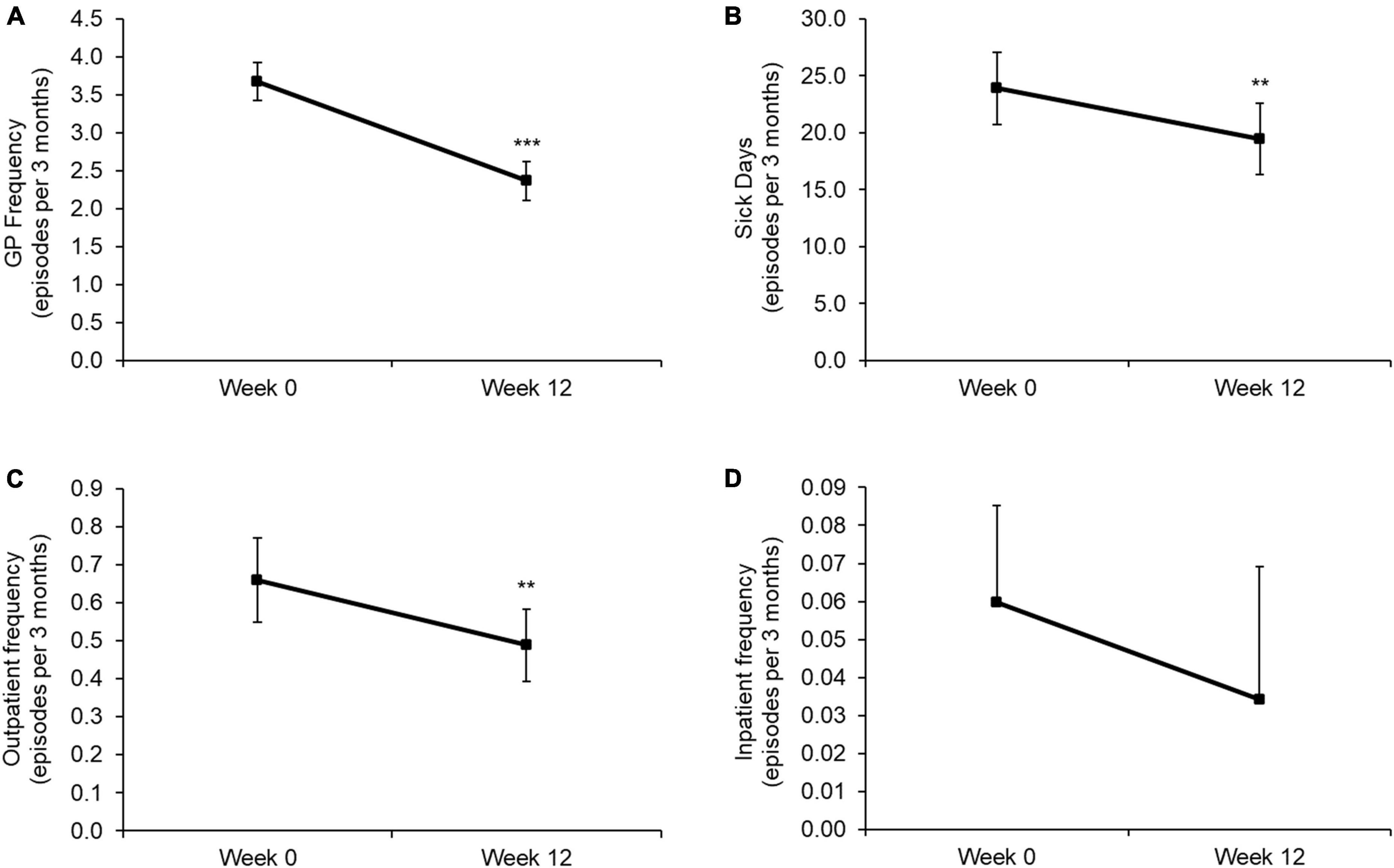
Figure 2. Baseline and Week 12 values for (A) the number of GP consultations, (B) sick days, (C) outpatient admissions, and (D) inpatient admissions during the past 3 months. Values are presented as mean (95% CI). Differences between time points were analyzed using paired t-tests. **p < 0.01; ***p < 0.001. GP frequency: n = 585; sick days: n = 402; outpatient frequency: n = 585; inpatient frequency: n = 585. Note, the lower error bar has been removed from panel (D) due to this crossing the x-axis.
A subgroup of patients with measures collected at Weeks 0, 6, and 12 demonstrated significant improvements in D-12, DASI, WHO-5 and EQ-5D-5L utility values from Week 0 to 6 (all p < 0.001), and further significant improvements from Week 6 to 12 (all p < 0.001) (Figure 3). Significant improvements for Week 0–6 and Week 6–12 were also observed for EQ-5D VAS (Week 0: 47.2 [20.7]; Week 6: 55.8 [25.0]; Week 12: 62.0 [23.9]; both p < 0.001) and sit-to-stand test results (Week 0: 11.5 [4.2]; Week 6: 13.9 [4.5]; Week 12: 15.4 [5.3]; both p < 0.001).
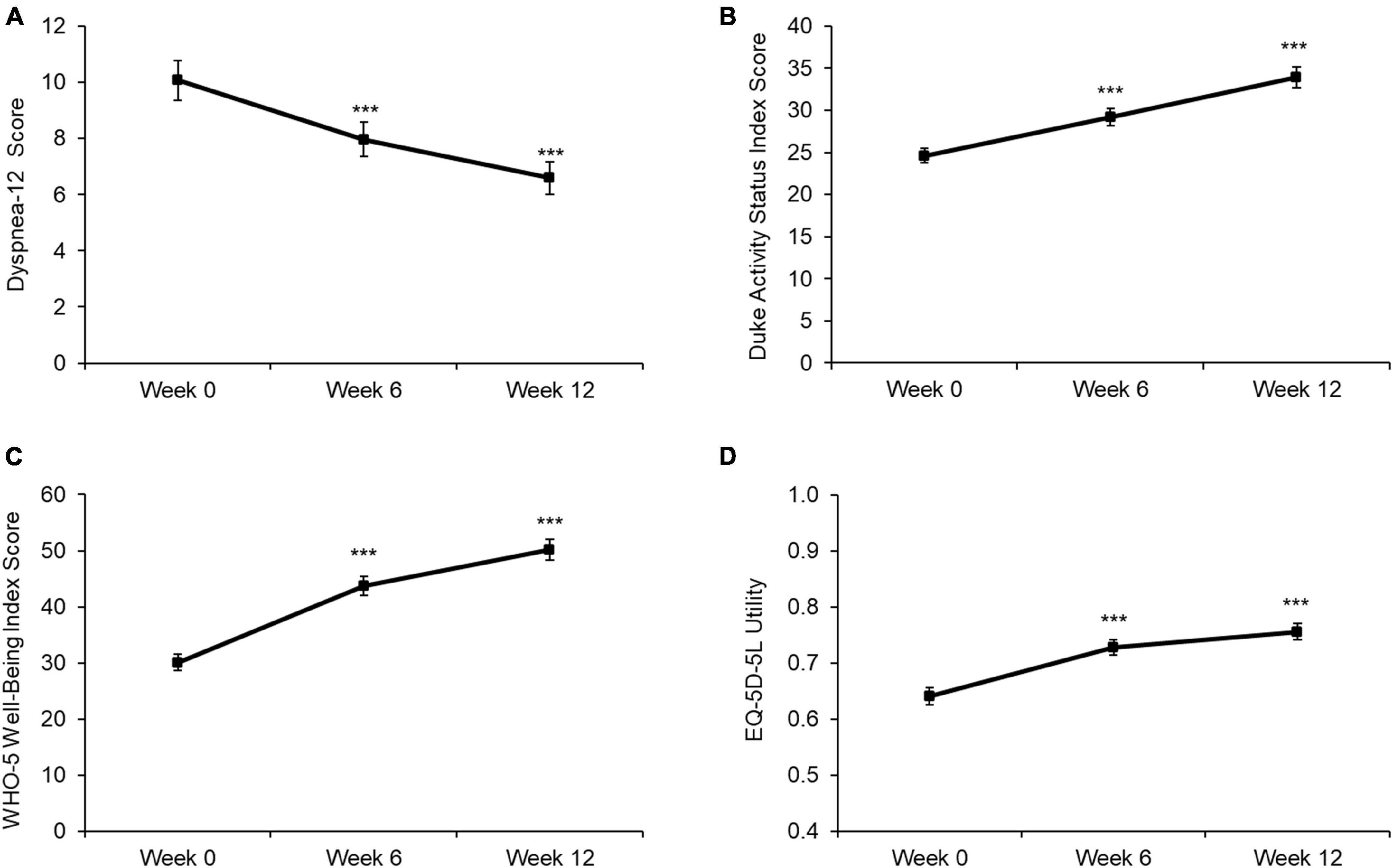
Figure 3. Baseline, Week 6, and Week 12 values for (A) D-12 score, (B) DASI score, (C) WHO-5 score, and (D) EQ-5D-5L utility. Values are presented as mean (95% CI). Higher scores indicate a worse health state for D-12, while lower scores indicate a worse health state for DASI, WHO-5, and EQ5D. Differences between time points were analyzed using paired t-tests. ***p < 0.001. D12 score: n = 535; DASI score: n = 528; WHO-5 score: n = 538; EQ5D utility: n = 526.
Changes in the individual components of the D-12, DASI, WHO-5 and EQ-5D-5L questionnaires are available in the Supplementary material for the primary analysis (Week 0 to 12) and time-course analysis (Week 0 to 6 to 12).
Discussion
This is the first evaluation of the effectiveness of a scalable community rehabilitation programme for participants presenting with LC. The outcomes demonstrate significant and clinically meaningful improvements in dyspnea, functional capacity, wellbeing and HR-QoL at programme completion. A reduced number of GP consultations, sick days and outpatient admissions were also observed during the programme compared with the preceding 3-month period. These findings suggest that the Nuffield Health COVID-19 Rehabilitation Programme can meet the urgent need for an effective and scalable LC rehabilitation model.
The improvements in functional capacity in response to the rehabilitation programme were demonstrated via a mean 9.2 point (37%) improvement in DASI score and a 4.1 score (36%) improvement in the 30-s sit-to-stand test. While the precise mechanisms of LC remain largely unknown (20), these findings suggest that the underlying pathology is responsive to exercise. The improvements in functional capacity are also likely to be linked with the observed reduction in dyspnea, as demonstrated through a mean 3.4 point (34%) improvement in D-12 score. Though several studies have utilized the 6-min walk test distance to assess improvements in exercise tolerance following pulmonary rehabilitation for LC (21), the sit-to-stand test is also highly recommended in the LC population (22). The sit-to-stand test was selected as it is simple to set up, easily conducted by trained, non-medical personnel, and manageable in restricted spaces. The exact mechanisms underlying exercise-induced LC improvements are yet to be fully elucidated, however, exercise is known to elicit structural and functional adaptations of the cardiovascular and musculoskeletal systems including enhanced lung function and respiratory muscle strength (23). Indeed, previous research in COPD patients has consistently demonstrated beneficial changes in exertional ventilation, breathing pattern, operating lung volume and static respiratory muscle strength in response to exercise training (24), even despite variability in the nature and composition of the rehabilitation protocols.
Consistent with the improvements in physical symptoms, significant and clinically meaningful increases in mental wellbeing and HR-QoL were observed in response to the 12-week rehabilitation programme. Participants demonstrated a mean 20.3 point (68%) improvement in WHO-5 score as a marker of mental wellbeing, alongside marked improvements in EQ-5D-5L utility and VAS scores. The mental wellbeing benefits of exercise are well documented in various chronic diseases including cardiovascular disease, diabetes and obesity, with regular physical activity shown to improve overall mood and symptoms of anxiety and depression (25). These effects may have been enhanced by the programme design of group exercise sessions and regular interactions with a rehabilitation specialist to increase feelings of social support and social connectedness with LC sufferers. These findings are notable, especially when considering that symptoms of PTSD, anxiety, and depression are frequently reported after COVID-19 infection, regardless of hospitalization status (26). As such, multidisciplinary rehabilitation models, targeting both the physical and mental health symptoms of LC are of critical importance, with the observed improvements in HR-QoL likely to be the result of combined improvements in both mental and physical wellbeing (27).
The improvements in physical and mental health and HR-QoL appeared to translate into reduced healthcare utilization during the rehabilitation programme. In this regard, participants reported significantly fewer GP consultations, sick days, and outpatient admissions during the 12-week rehabilitation programme compared with the 3-month period preceding the programme. This aligns with previous research in COPD patients showing reduced hospital readmission rates and medical costs during the 6 months after completion of a pulmonary rehabilitation programme, compared with patients who did not initiate rehabilitation (28). It is important to note that recall bias may have influenced the accuracy of participants reporting of healthcare utilization over the past 3 months. Nevertheless, considering the economic consequences of sickness absence and health-related productivity losses (29), as well as the healthcare resource utilization required for the treatment of LC, further investigation into the benefits of LC rehabilitation on these outcomes may be beneficial to understand the wider societal impacts of this intervention.
Importantly, beneficial effects of the rehabilitation programme for physical and mental health and HR-QoL were observed after 6 weeks, with further improvements then observed at 12 weeks. This finding strengthens the theory that pulmonary rehabilitation programs for LC may benefit from a duration of 12 weeks, rather than the 6–8 week duration seen in some studies (30). During the first 6 weeks of the programme all activities were conducted remotely, which demonstrates the effectiveness of a telerehabilitation model for LC rehabilitation. Further research is required to determine whether the additional improvements from 6 to 12 weeks occurred as a result of the extended duration or the incorporation of face-to-face rehabilitation sessions. Previous research in COPD has demonstrated that remote delivery of pulmonary rehabilitation provides similar outcomes to face-to-face PR, with improvements in exercise capacity, dyspnea and HR-QoL (31). These findings suggest that a fully remote or blended rehabilitation programme provides a clinically effective alternative to centre-based approaches for LC, with a fully remote model representing a potential approach to increase the reach of the programme while maintaining effectiveness.
Limitations
The present study has demonstrated the clinical effectiveness of a scalable LC rehabilitation model for improving physical, mental, and HR-QoL outcomes. This is particularly striking considering current evidence that LC does not appear to improve over time in the absence of targeted therapies (32). Nevertheless, some limitations must be acknowledged. First, a control group was not included. Therefore, we cannot directly attribute all of the observed benefits to the LC rehabilitation programme or understand the influence of factors such as support from Rehabilitation Specialists or social interaction with other participants. Nonetheless, the observed benefits exceed any improvements reported without intervention in the literature. Second, the majority of patients were female (77.4%) and of White British ethnicity (88.6%). Although LC is more common in women than men (33), the lack of diversity in this sample demonstrates the need for further work to engage with additional populations and communities. Further, people who were previously diagnosed with chronic fatigue syndrome prior to COVID-19 infection were excluded from the study, therefore the findings cannot be extended to this population. Third, we did not utilize a population-specific functionality measure such as the post-COVID functional status scale (PCFS) (34). This could be utilized in future research to monitor changes in function. Last, the effectiveness of the rehabilitation programme was monitored over a relatively short period of 12 weeks. Research in COPD suggests that the benefits of PR may last for 4 years after program discharge; however, further data maturity is required to understand whether the benefits observed in response to the present programme remain after completion.
Conclusion
In conclusion, this evaluation demonstrated significant and clinically meaningful improvements in dyspnea, functional capacity, mental wellbeing and HR-QoL in response to a 12-week rehabilitation programme for participants presenting with LC. A reduced number of GP consultations, sick days and outpatient admissions was also observed during the 3-month programme. The blended and community design of this rehabilitation model makes it scalable and meets the urgent need for an effective intervention to support patients experiencing LC. Improvements observed during the first 6 weeks of the programme also demonstrate the effectiveness of remote programme delivery. This rehabilitation model is well placed to support the NHS (and other healthcare systems worldwide) in its aim of controlling the impacts of COVID-19 and delivering on its long-term plan.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Manchester Metropolitan University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
AI, MH, LM, ZL, PD, GW, JK, DD, and BK contributed to the design and coordination of the intervention. KD performed the statistical analysis. JS and KD drafted the manuscript. BK accepted the full responsibility for the work and the decision to publish and attested that all authors meet authorship criteria and no others meeting the criteria have been omitted. All authors contributed to the final manuscript.
Funding
This work was funded through a grant from the Manchester Metropolitan University Partnership Board, a funding source dedicated to the advancement of health and wellbeing service development that have the potential to generate significant public benefit.
Conflict of interest
JS, KD, AI, MH, LM, ZL, DD, and BK were employed by Nuffield Health.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1149922/full#supplementary-material
Footnotes
References
1. WHO. WHO Coronavirus (COVID-19) Dashboard [Internet]. (2022). Available online at: https://covid19.who.int (accessed May 25, 2022).
2. Nopp S, Moik F, Klok FA, Gattinger D, Petrovic M, Vonbank K, et al. Outpatient pulmonary rehabilitation in patients with long COVID improves exercise capacity, functional status, dyspnea, fatigue, and quality of life. Respiration (2022) 101:593–601. doi: 10.1159/000522118
3. NICE. Overview | COVID-19 Rapid Guideline: Managing the Long-Term Effects of COVID-19 | Guidance | NICE [Internet]. (2022). Available online at: https://www.nice.org.uk/guidance/ng188 (accessed June 7, 2022).
4. Arnold DT, Hamilton FW, Milne A, Morley AJ, Viner J, Attwood M, et al. Patient outcomes after hospitalisation with COVID-19 and implications for follow-up: results from a prospective UK cohort. Thorax (2021) 76:399–401. doi: 10.1136/thoraxjnl-2020-216086
5. Chen H, Shi H, Liu X, Sun T, Wu J, Liu Z. Effect of pulmonary rehabilitation for patients with post-COVID-19: a systematic review and meta-analysis. Front. Med. (2022) 9:837420. doi: 10.3389/fmed.2022.837420
6. Office for National Statistics. Prevalence of Ongoing Symptoms Following Coronavirus (COVID-19) Infection in the UK - Office for National Statistics [Internet]. (2022). Available online at: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/1june2022 (accessed June 7, 2022).
7. Mizrahi B, Sudry T, Flaks-Manov N, Yehezkelli Y, Kalkstein N, Akiva P, et al. Long COVID outcomes at one year after mild SARS-CoV-2 infection: nationwide cohort study. BMJ (2023) 380:e072529. doi: 10.1136/bmj-2022-072529
8. Kelly B, Innes A, Holl M, Mould L, Powell S, Burns D, et al. Scalable modEls of community rehAbilitation for individuals recovering from COVID:19 reLated illnEss: a longitudinal service evaluation protocol—“SeaCole cohort evaluation”. Front. Public Health (2021) 9:628333. doi: 10.3389/fpubh.2021.628333
9. Yorke J, Russell AM, Swigris J, Shuldham C, Haigh C, Rochnia N, et al. Assessment of dyspnea in asthma: validation of the dyspnea-12. J. Asthma (2011) 48:602–8.
10. Hlatky MA, Boineau RE, Higginbotham MB, Lee KL, Mark DB, Califf RM, et al. A brief self-administered questionnaire to determine functional capacity (the duke activity status index). Am. J. Cardiol. (1989) 64:651–4. doi: 10.1016/0002-9149(89)90496-7
11. Zanini A, Crisafulli E, D’Andria M, Gregorini C, Cherubino F, Zampogna E, et al. Minimum clinically important difference in 30-s sit-to-stand test after pulmonary rehabilitation in subjects with COPD. Respir. Care (2019) 64:1261–9. doi: 10.4187/respcare.06694
12. WHO. Wellbeing Measures in Primary Health Care/the DEPCARE Project. Copenhagen: WHO Regional Office for Europe (1998). p. 45.
13. Herdman M, Gudex C, Lloyd A, Janssen MF, Kind P, Parkin D, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. (2011) 20:1727–36. doi: 10.1007/s11136-011-9903-x
14. Devlin NJ, Shah KK, Feng Y, Mulhern B, van Hout B. Valuing health-related quality of life: an EQ-5D-5L value set for England. Health Econ. (2018) 27:7–22.
15. Ekström MP, Bornefalk H, Sköld CM, Janson C, Blomberg A, Bornefalk-Hermansson A, et al. Minimal clinically important differences and feasibility of dyspnea-12 and the multidimensional dyspnea profile in cardiorespiratory disease. J. Pain Symptom Manage. (2020) 60:968–75.e1. doi: 10.1016/j.jpainsymman.2020.05.028
16. Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 well-being index: a systematic review of the literature. Psychother. Psychosom. (2015) 84:167–76.
17. Nolan CM, Longworth L, Lord J, Canavan JL, Jones SE, Kon SSC, et al. The EQ-5D-5L health status questionnaire in COPD: validity, responsiveness and minimum important difference. Thorax (2016) 71:493–500. doi: 10.1136/thoraxjnl-2015-207782
18. Wijeysundera DN, Beattie WS, Hillis GS, Abbott TEF, Shulman MA, Ackland GL, et al. Integration of the duke activity status index into preoperative risk evaluation: a multicentre prospective cohort study. Br. J. Anaesth. (2020) 124:261–70.
19. R Core Team. R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing (2021).
20. Crook H, Raza S, Nowell J, Young M, Edison P. Long covid-mechanisms, risk factors, and management. BMJ (2021) 374:n1648. doi: 10.1136/bmj.n1648
21. Soril LJJ, Damant RW, Lam GY, Smith MP, Weatherald J, Bourbeau J, et al. The effectiveness of pulmonary rehabilitation for post-COVID symptoms: a rapid review of the literature. Respir. Med. (2022) 195:106782. doi: 10.1016/j.rmed.2022.106782
22. Núñez-Cortés R, Rivera-Lillo G, Arias-Campoverde M, Soto-García D, García-Palomera R, Torres-Castro R. Use of sit-to-stand test to assess the physical capacity and exertional desaturation in patients post COVID-19. Chron. Respir. Dis. (2021) 18:1479973121999205. doi: 10.1177/1479973121999205
23. McKenzie DC. Respiratory physiology: adaptations to high-level exercise. Br. J. Sports Med. (2012) 46:381–4.
24. Marillier M, Bernard AC, Vergès S, Neder JA. Locomotor muscles in COPD: the rationale for rehabilitative exercise training. Front. Physiol. (2020) 10:1590.
25. Herbert C, Meixner F, Wiebking C, Gilg V. Regular physical activity, short-term exercise, mental health, and well-being among university students: the results of an online and a laboratory study. Front. Psychol. (2020) 11:509. doi: 10.3389/fpsyg.2020.00509
26. Houben-Wilke S, Goërtz YM, Delbressine JM, Vaes AW, Meys R, Machado FV, et al. The impact of long COVID-19 on mental health: observational 6-month follow-up study. JMIR Ment. Health (2022) 9:e33704. doi: 10.2196/33704
27. Healthy People. Health-Related Quality of Life and Well-Being | Healthy People 2020 [Internet]. (2022). Available online at: https://www.healthypeople.gov/2020/about/foundation-health-measures/Health-Related-Quality-of-Life-and-Well-Being (accessed June 29, 2022).
28. Zhang A, Wang L, Long L, Yan J, Liu C, Zhu S, et al. Effectiveness and economic evaluation of hospital-outreach pulmonary rehabilitation for patients with chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon. Dis. (2020) 15:1071–83.
29. Department of Health. Work, Health and Disability Green Paper Data Pack [Internet]. (2016). Available online at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/644090/work-health-and-disability-green-paper-data-pack.pdf (accessed October 31, 2016).
30. Fugazzaro S, Contri A, Esseroukh O, Kaleci S, Croci S, Massari M, et al. Rehabilitation interventions for post-acute COVID-19 syndrome: a systematic review. Int. J. Environ. Res. Public Health (2022) 19:5185.
31. Cox NS, Corso SD, Hansen H, McDonald CF, Hill CJ, Zanaboni P, et al. Telerehabilitation for chronic respiratory disease. Cochrane Datab. Syst. Rev. (2021). CD013040. doi: 10.1002/14651858.CD013040.pub2
32. The PHOSP-COVID Collaborative Group. Clinical characteristics with inflammation profiling of Long-COVID and association with one-year recovery following hospitalisation in the UK: a prospective observational study. Med. Lett. CDC FDA (2022) 10:761–75. doi: 10.1016/S2213-2600(22)00127-8
33. Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, et al. Attributes and predictors of long COVID. Nat. Med. (2021) 27:626–31.
Keywords: coronavirus, SARS-CoV-2, exercise, emotional wellbeing, digital health, fatigue, SeaCole
Citation: Smith JL, Deighton K, Innes AQ, Holl M, Mould L, Liao Z, Doherty P, Whyte G, King JA, Deniszczyc D and Kelly BM (2023) Improved clinical outcomes in response to a 12-week blended digital and community-based long-COVID-19 rehabilitation programme. Front. Med. 10:1149922. doi: 10.3389/fmed.2023.1149922
Received: 30 January 2023; Accepted: 02 May 2023;
Published: 24 May 2023.
Edited by:
Shisan Bao, The University of Sydney, AustraliaReviewed by:
Diana C. Sanchez-Ramirez, University of Manitoba, CanadaVicente Benavides-Cordoba, Pontificia Universidad Javeriana Cali, Colombia
Copyright © 2023 Smith, Deighton, Innes, Holl, Mould, Liao, Doherty, Whyte, King, Deniszczyc and Kelly. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Benjamin M. Kelly, Benjamin.Kelly@nuffieldhealth.com
†These authors share first authorship
 Jemma L. Smith
Jemma L. Smith Kevin Deighton
Kevin Deighton Aidan Q. Innes1
Aidan Q. Innes1  Laura Mould
Laura Mould Patrick Doherty
Patrick Doherty James A. King
James A. King Benjamin M. Kelly
Benjamin M. Kelly