Comparison of Corneal Biomechanics in Post-SMILE, Post-LASEK, and Keratoconic Eyes
- 1Eye Institute and Department of Ophthalmology, Eye and ENT Hospital, Fudan University, Shanghai, China
- 2NHC Key Laboratory of Myopia, Fudan University, Shanghai, China
- 3Key Laboratory of Myopia, Chinese Academy of Medical Sciences, Shanghai, China
- 4Shanghai Research Center of Ophthalmology and Optometry, Shanghai, China
- 5Department of Ophthalmology, University of Pittsburgh School of Medicine, Pittsburgh, PA, United States
Significance: Our study found that SP-A1 (stiffness parameter at time of first applanation) was statistically different between post-laser-assisted subepithelial keratomileusis (LASEK) and post-small incision lenticule extraction (SMILE) eyes. The stiffness of keratoconus was lower than that of post-refractive surgery corneas.
Purpose: To compare corneal biomechanics among post-SMILE, post-LASEK, and keratoconic eyes.
Methods: In this retrospective study, 36 eyes of 36 patients after SMILE, 36 eyes of 36 patients after LASEK, and 36 eyes of 36 patients with keratoconus with matching (±5 μm) central corneal thickness (CCT) were examined using Scheimpflug corneal topography (Pentacam HR) and dynamic Scheimpflug analyzer (CorVis ST). Mixed linear model analysis with Bonferroni-adjusted post-hoc comparisons was performed to compare the differences in corneal biomechanics and topographic parameters among the three groups with the CCT and the bIOP (intraocular pressure with biomechanical correction) as the random factor.
Results: All groups had comparable CCT at baseline. The bIOPs between the three groups were comparable. The mean values of the Belin/Ambrósio Deviation (BAD-D) in the keratoconus group were significantly higher than those of the SMILE (post hoc p < 0.001) and LASEK groups (post hoc p < 0.001). The SP-A1 in the keratoconus group was the lowest when compared with those of the SMILE (post hoc p = 0.003) and LASEK groups (post hoc p < 0.001). The SMILE group SP-A1 values were slightly lower than those of the LASEK group (post hoc p = 0.044).
Conclusions: Keratoconus eyes were significantly softer when compared to post-refractive surgery corneas with comparable corneal thickness in terms of SP-A1 and BAD-D values, while the LASEK group may have the greatest stiffness. Post-SMILE and post-LASEK corneas showed significant differences in SP-A1.
Introduction
Keratoconus is a bilateral, progressive ectatic disorder, which causes thinning of the corneal stroma, irregular astigmatism, and loss of best spectacle-corrected vision (1–3). The prevalence is around 1/2,000 in the general population (2). Another form of corneal ectasia is seen after refractive surgeries, mainly after laser in situ keratomileusis (LASIK) (4–6). On the other hand, small incision lenticule extraction (SMILE) (7, 8) and laser-assisted subepithelial keratomileusis (LASEK) are stromal flap-free surgeries, which are rarely associated with corneal ectasia. This might be attributed to the lack of corneal flap and other factors such as corneal stromal bed thickness (9). Post-SMILE and post-LASEK eyes are therefore good models for understanding the effect of tissue removal on the cornea.
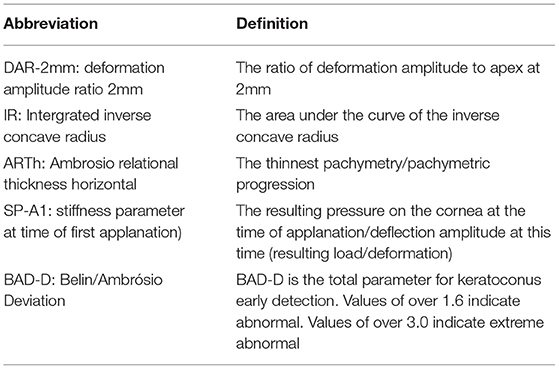
It is generally believed that the compromise of corneal biomechanics precedes the occurrence of topographic abnormality (10). CorVis ST is a dynamic Scheimpflug analyzer, which is able to capture the corneal deformation process caused by an air puff. By analyzing the parameters including deformation amplitude, time, length, and velocity, in-vivo corneal biomechanics are assessed and quantified (9). The new Vinciguerra Screening Report provides parameters such as deformation amplitude ratio at 2 mm, (DAR-2mm), integrated inverse concave radius (IR), Ambrosio relational thickness horizontal (ARTh), and stiffness parameter at the first applanation (SP-A1) to describe corneal biomechanics. The present study intended to detect the difference in corneal biomechanics between the corneas that underwent flapless corneal refractive surgeries (SMILE and LASEK) keratoconus under the condition of the similar corneal thickness (and bIOP). A post-LASEK cornea (myopia correction) lacks Bowman's layer, and the central corneal thickness is much thinner than the peripheral. A post-SMILE cornea remains a relative intact anterior stroma, but a potential gap formed in the anterior stroma after the stromal lenticular extraction. In the present study, we compared the DAR-2mm, IR, ARTh, SP-A1, and Belin/Ambrósio Deviation (BAD-D) values (Table 1) among keratoconic, post-SMILE, and post-LASEK patients. We hope that through this study, we can better understand the corneal biomechanical differences between keratoconus and after corneal refractive surgery.
Patients and Methods
Patients
In this retrospective study, we included participants who had undergone SMILE or LASEK procedure with matching (±5 μm) central corneal thickness (CCT). We also included patients with keratoconus. Keratoconus was diagnosed following the Global Consensus guidelines (11). Besides, the cones were within 4 mm in the center. One eye of each participant was selected. A total of 36 eyes of 36 patients with keratoconus (keratoconus group), 36 eyes of 36 participants who had undergone SMILE (SMILE group), and 36 eyes of 36 participants who had undergone LASEK (LASEK group) were enrolled from the Department of Ophthalmology, Eye and ENT Hospital of Fudan University. Among them, the keratoconus group was randomly selected from patients who visited our hospital in the recent 2 years and did not receive any eye surgical treatment, and the examination was measured immediately at the time of first visit as routine. As for the other two groups, we selected the patients who underwent refractive surgery who met the requirement of CCT, then selected them randomly, and then the examination was performed 2 years after the operation. In addition, some keratoconus patients failed to enter the study because of the difference of CCT between keratoconus patients and patients who underwent corneal surgery which was beyond 5 μm. The study protocol followed the tenets of the Declaration of Helsinki and was approved by the ethics committee of the Eye and ENT Hospital of Fudan University. An informed consent was obtained from all participants. The ethical committee approval code is KJ2010-18.
Surgeries
All the procedures were performed by one surgeon (XTZ). All the target diopters were set to 0D. SMILE procedures were performed using a VisuMax femtosecond laser system (Carl Zeiss Meditec, Jena, Germany) with a pulse energy of 130 nJ. The cap was set to 120-μm thickness and 7.5-mm diameter. The side cut was set to 2 mm. The superior surface and the inferior surface of the lenticule were separated from the anterior stroma. The lenticule was then extracted through the side cut. LASEK was performed using a Mel 80 excimer laser (Carl Zeiss Meditec, Jena, Germany) system. Corneal epithelial trephines (Model 52503B; 66 Vision Tech Co., Ltd., Suzhou, China) with an inner diameter of 8.5 mm and a 20% ethanol-aqueous solution were employed to create an epithelial flap. The excimer laser with a repetition rate of 250 kHz and pulse energy of 150 nJ was used to ablate the corneal stroma. The epithelial flap was repositioned after the excimer laser treatment (9).
Measurement
Each patient underwent manifest refraction spherical equivalent (MRSE), best spectacle-corrected distant visual acuity (BSCDVA), and slit-lamp examination. Measurements were performed preoperatively and 2 years postoperatively. Corneal topographies were captured using Pentacam HR. CCT from Pentacam was used for statistical comparison. Corneal biomechanical assessments were measured with CorVis ST. Pentacam and CorVis measurements were performed three times for each eye, and the quality of the image was OK. The DAR-2mm, IR, SP-A1, Belin/Ambrosio Deviation (BAD-D) values were exported (4, 5, 12–16).
Data Analysis
Data analysis was performed using SPSS Version 22.0 software. The Kolmogorov–Smirnov test was used for normality tests. The Friedman test was used to analyze the differences in age, gender, CCT, MRSE, bIOP (intraocular pressure with biomechanical correction), Flat K, Steep K, and Kmax among the three groups. Mixed linear models with Bonferroni-adjusted post-hoc comparisons were used to analyze the differences in the mean values of DAR-2mm, IR, ARTh, SP-A1, and BAD-D with the operation mode as the fixed factor and the CCT and the bIOP as the random factors.
Results
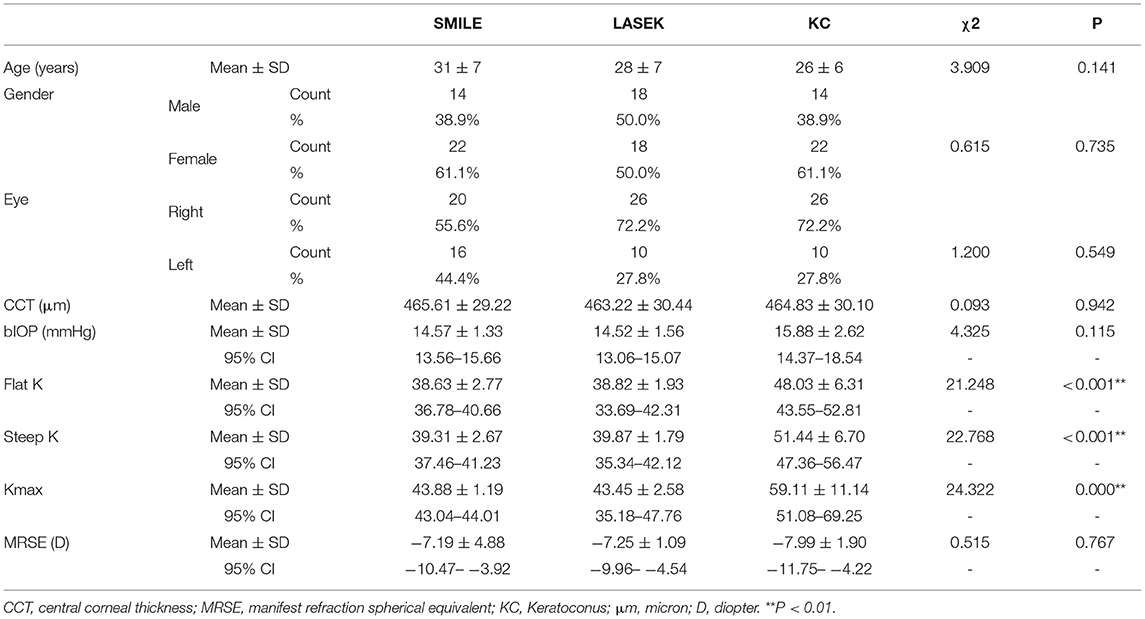
Table 2 summarizes the demographic characteristics in all groups. The mean age of patients in the SMILE, LASEK, and keratoconus groups was 31 ± 7 years, 28 ± 7 years, and 26 ± 6 years, respectively. The mean CCT values were 465.61 ± 29.22 μm, 463.22 ± 30.44 μm, and 464.83 ± 30.10 μm, respectively. The age of the patients (χ2 = 3.909, p = 0.141), gender (χ2 = 0.615, p = 0.735), left/right eyes (χ2 = 1.200, p = 0.549), CCT(χ2 = 0.093, p = 0.942), bIOP (χ2 = 4.325, p = 0.115), and MRSE (χ2 = 0.515, p = 0.767) were statistically comparable in all three groups. Flat K (χ2 = 21.248, p < 0.001) of the three groups were 38.63 ± 2.77, 38.82 ± 1.93, and 48.03 ± 6.31. Steep k (χ2 = 22.768, p < 0.001) were 39.31 ± 2.67, 39.87 ± 1.79, and 51.44 ± 6.70. Kmax (χ2 = 24.322, p < 0.001) were 43.88 ± 1.19, 43.45 ± 2.58, and 59.11 ± 11.14, respectively.
The biomechanical parameters are listed in Table 3. Overall, statistically significant differences were detected in the mean values of SP-A1 between post-refractive surgery and keratoconus eyes (p < 0.05). Figure 1A shows that the mean IR values in the LASEK group and in the SMILE group were significantly lower than those in the keratoconus group (post hoc P (LASEK vs. keratoconus) < 0.001, post hoc P (SMILE vs. keratoconus) = 0.014).
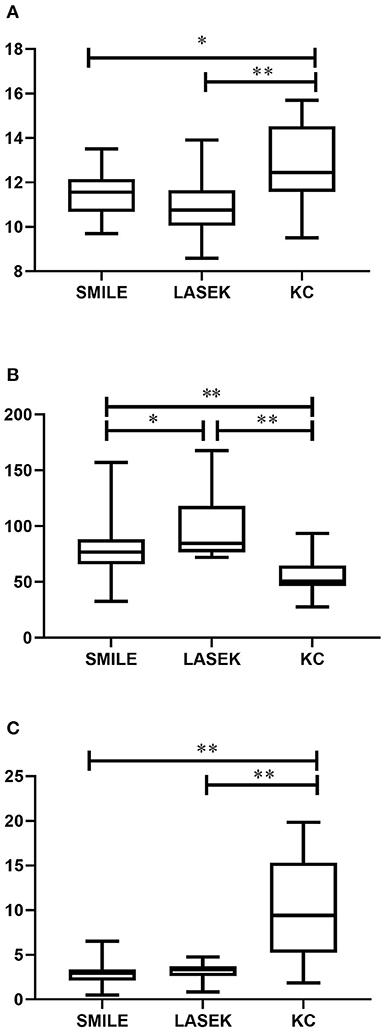
Figure 1. Corneal biomechanics among post-SMILE, post-LASEK, and keratoconic eyes. (A) IR; (B) SP-A1; (C) BAD-D. SMILE, small incision lenticule extraction; LASEK, laser-assisted subepithelial keratomileusis; KC, keratoconus. *P < 0.05 and **P < 0.01.
Statistically significant differences were also noted between LASEK and SMILE groups in SP-A1 (post hoc p = 0.044) but not in IR (post hoc p = 0.338) (Figure 1B). Figure 1C shows the mean BAD-D values in all groups. The keratoconus group had significantly higher BAD-D values when compared to SMILE (post hoc p < 0.001) and LASEK groups (post hoc p < 0.001). The difference in the mean BAD-D values between the SMILE and LASEK groups was not significant statistically (post hoc p = 1.000).
The differences in the mean values of the DAR-2mm and ARTh were not significant among the three groups (F = 2.572; p = 0.093 and F = 1.478, p = 0.495, respectively).
Discussion
It is hypothesized that alterations in corneal biomechanics and bIOP play a key role in primary and post-LASIK corneal ectasia (17). Therefore, measurement of biomechanical parameters is important for identification of corneal ectasia at an early stage (18, 19). The present study investigated the differences in corneal topography and biomechanics in keratoconus and post-refractive surgery eyes using CorVis ST and Pentacam HR platforms. We noted that SP-A1 was the lowest in the keratoconus group, while it was highest in the LASEK group. SP-A1 describes the deformation resistance of the cornea (4). Our findings indicated that for matched CCT, bIOP, and age, corneas of keratoconus patients were less “stiff” than those of patients who underwent LASEK or SMILE. Simultaneously, the mean IR value was the lowest in the LASEK group and highest in the keratoconus group, again indicating the degree of compromised biomechanics in keratoconus patients. These findings are consistent with previous reports showing that keratoconus is characterized by decreasing corneal thickness, disruption of Bowman's layer, and disintegration of corneal collagen lamellae (20). The difference of SP-A1 between the SMILE group and LASEK group may be related to the stromal layer removed during SMILE operation, while LASEK retained the integrity of the stromal layer. When detecting SP-A1, its essence is to measure the deformation degree of the cornea when it is stressed and sunken by air impact. For LASEK, the cornea will deform as a whole when it is impacted, but SMILE is not. Due to the existence of a cap, a potential gap will be formed between the cap and the residual corneal stroma. Although the selected patients after SMILE have been followed up for 2 years, theoretically, this gap cannot heal, and the existence of this gap may be the reason for the greater deformation of the cornea when impacted by force.
We observed in our study that DAR-2mm and ARTh were similar among the three groups. DAR-2mm is the ratio of deformation amplitude at the apex of the cornea to a point 2 mm away from the apex. ARTh is the quotient of corneal thickness at the thinnest point of the horizontal meridian and the thickness progression (16). For keratoconus, the CCT is much lower than the peripheral corneal thickness. The deformation amplitude in the central zone is larger than the peripheral zone, and hence the DAR-2mm value is higher in keratoconic eyes when compared to the normal eyes. Meanwhile, keratoconus has larger pachymetric progression than normal eyes. Since ARTh equals to the thinnest pachymetry divided by pachymetric progression, the value is lower in keratoconic eyes. The DAR-2mm and ARTh values could identify keratoconus from otherwise normal thin corneas. However, after corneal refractive surgery for myopia correction, more tissue would be ablated from the central zone of the cornea compared to the peripheral zone. As the central thickness would decrease more than the peripheral thickness, the deformation amplitude in the central zone would increase significantly, and thus the DAR-2mm value would increase. The ARTh value would also decrease postoperatively owing to a decrease in pachymetry in the central zone after myopia correction, which increases the pachymetric progression. The mean BAD-D value in the keratoconus group was much higher than those of the SMILE and LASEK groups, which corresponded with SP-A1 values among the three groups.
In our study, it was noteworthy that there was no significant difference in BAD-D values between SMILE and LASEK groups, but the LASEK group had higher SP-A1 values when compared with those of the SMILE group. Reinstein et al. established a mathematical model to investigate the effects of photorefractive keratectomy (PRK), LASIK, and SMILE on corneal biomechanics. It was reported that theoretically, SMILE should lead to a minimal effect on corneal biomechanics when compared with PRK and LASIK as the integrity of the anterior stroma is maximally maintained (21). However, in recent years, studies have shown that PRK had small effect on central biomechanics when compared with SMILE (22), which suggests that our biomechanical research needs to be further developed. In our study, we found that the SP-A1 value in the SMILE group was significantly lower than that in the LASEK group, indicating that overall the effect of LASEK on corneal biomechanics is less when compared to SMILE. SP-A1 describes the stiffness of cornea at the time of first applanation. In our previous study, it is possible that the potential gap between the cap and stromal bed after SMILE, which could be detected with Scheimpflug camera (23), may be a confounding factor that influences the accuracy of assessment in early stage. The patients selected in this study were assessed 2 years after surgery, and no obvious gap was found during the follow-up. Therefore, the cap/bed interface between two stressed regions after SMILE may be the biggest difference from LASEK. Further research is still necessary.
We originally considered that keratoconus stage may have an impact on corneal biomechanics, but in order to match CCT, which is different in patients after corneal refractive surgery, and CCT is also an important factor in keratoconus stage, we only matched CCT and bIOP which have great impact on corneal biomechanics.
The major limitation of our study is the small sample size. Studies with a larger sample size and long-term follow-up are recommended. Besides being a retrospective study and lacking preoperative parameters, the study may produce a degree of deviation, which needs further research in the future. Finally, in order to better match CCT, this study failed to unify the stage of keratoconus. This is also due to the limited sample size of this study. In the future, this point should be paid more attention.
In conclusion, our study found that SP-A1 was statistically different between post-LASEK and post-SMILE eyes. The stiffness of keratoconus was lower than that of post-refractive surgery corneas.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the ethics committee of the Eye and ENT Hospital of Fudan University. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JS: experimental design, data collection, and writing manuscript. YS: experimental design and data collection. VJ: data analysis and article embellishment. XuZ: data collection and analysis. JZ and YZ: design of experimental ideas. XiZ: experimental ideas design guidance, funds supply, and equipment supply. All authors contributed to the article and approved the submitted version.
Funding
This work was supported in part by the National Natural Science Foundation of China (Grant No. 81770955), the Joint Research Project of New Frontier Technology in Municipal Hospitals (SHDC12018103), the Project of Shanghai Science and Technology (Grant No. 20410710100), the Major Clinical Research Project of Shanghai Shenkang Hospital Development Center (SHDC2020CR1043B), and the Project of Shanghai Xuhui District Science and Technology (2020-015). The funders had no role in study design, data collection and analysis, decision to publish, and preparation of the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor is a consultant for the manufacturer Corvis ST.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rabinowitz YS. Keratoconus. Surv Ophthalmol. (1998) 42:297–319. doi: 10.1016/S0039-6257(97)00119-7
2. mbrósio R Jr, Belin MW. Imaging of the cornea: topography vs tomography. J Refract Surg. (2010) 26:847–9. doi: 10.3928/1081597X-20101006-01
3. Belin MW, Khachikian SS. An introduction to understanding elevation-based topography: how elevation data are displayed—a review. Clin Exp Ophthalmol. (2009) 37:14–29. doi: 10.1111/j.1442-9071.2008.01821.x
4. Vinciguerra R, Ambrósio R Jr, Elsheikh A, Roberts CJ, Lopes B, Morenghi E, et al. Detection of keratoconus with a new biomechanical index. J Refract Surg. (2016) 32:803–10. doi: 10.3928/1081597X-20160629-01
5. Chan TCY, Wang YM, Yu M, Jhanji V. Comparison of Corneal Tomography and a New Combined Tomographic Biomechanical Index in Subclinical Keratoconus. J Refract Surg. (2018) 34:616–21. doi: 10.3928/1081597X-20180705-02
6. Wilson SE, Lin DT, Klyce SD, Reidy JJ, Insler MS. Topographic changes in contact lens-induced corneal warpage. Ophthalmology. (1990) 97:734–44. doi: 10.1016/S0161-6420(90)32516-2
7. Frings A, Vidic B, El-Shabrawi Y, Ardjomand N. Laser-assisted subepithelial keratomileusis with mitomycin C for myopic astigmatism ≥2.00 diopters using a Zeiss MEL 80 Excimer. Int Ophthalmol. (2014) 34:225–33. doi: 10.1007/s10792-013-9819-2
8. Ivarsen A, Hjortdal J. Correction of myopic astigmatism with small incision lenticule extraction. J Refract Surg. (2014) 30:240–7. doi: 10.3928/1081597X-20140320-02
9. Shen Y, Chen Z, Knorz MC, Li M, Zhao J, Zhou X. Comparison of corneal deformation parameters after SMILE, LASEK, and femtosecond laser-assisted LASIK. J Refract Surg. (2014) 30:310–8. doi: 10.3928/1081597X-20140422-01
10. Vinciguerra R, Ambrósio R Jr, Roberts CJ, Azzolini C, Vinciguerra P. Biomechanical Characterization of subclinical keratoconus without topographic or tomographic abnormalities. J Refract Surg. (2017) 33:399–407. doi: 10.3928/1081597X-20170213-01
11. Gomes JA, Tan D, Rapuano CJ, Belin MW, Ambrósio R Jr, Guell JL, et al. Global consensus on keratoconus and ectatic diseases. Cornea. (2015) 34:359–69. doi: 10.1097/ICO.0000000000000408
12. Roberts CJ, Mahmoud AM, Bons JP, Hossain A, Elsheikh A, Vinciguerra R, et al. Introduction of two novel stiffness parameters and interpretation of air puff-induced biomechanical deformation parameters with a dynamic scheimpflug analyzer. J Refract Surg. (2017) 33:266–73. doi: 10.3928/1081597X-20161221-03
13. Muftuoglu O, Ayar O, Hurmeric V, Orucoglu F, Kilic I. Comparison of multimetric D index with keratometric, pachymetric, and posterior elevation parameters in diagnosing subclinical keratoconus in fellow eyes of asymmetric keratoconus patients. J Cataract Refract Surg. (2015) 41:557–65. doi: 10.1016/j.jcrs.2014.05.052
14. Ambrósio R Jr, Valbon BF, Faria-Correia F, Ramos I, Luz A. Scheimpflug imaging for laser refractive surgery. Curr Opin Ophthalmol. (2013) 24:310–20. doi: 10.1097/ICU.0b013e3283622a94
15. Vinciguerra R, Elsheikh A, Roberts CJ, Ambrósio R Jr, Kang DS, Lopes BT, et al. Influence of pachymetry and intraocular pressure on dynamic corneal response parameters in healthy patients. J Refract Surg. (2016) 32:550–61. doi: 10.3928/1081597X-20160524-01
16. Lopes BT, Ramos I, Salomão MQ, Canedo ALC, Ambrósio R Jr. Perfil paquimétrico horizontal para a detecção do ceratocone[J]. Revista Brasileira de Oftalmologia. (2015) 74:382–5. doi: 10.5935/0034-7280.20150080
17. Scarcelli G, Besner S, Pineda R, Yun SH. Biomechanical characterization of keratoconus corneas ex vivo with Brillouin microscopy. Invest Ophthalmol Vis Sci. (2014) 55:4490–5. doi: 10.1167/iovs.14-14450
18. Ambrósio R Jr, Dawson DG, Salomão M, Guerra FP, Caiado AL, Belin MW. Corneal ectasia after LASIK despite low preoperative risk: tomographic and biomechanical findings in the unoperated, stable, fellow eye. J Refract Surg. (2010) 26:906–11. doi: 10.3928/1081597X-20100428-02
19. Ambrósio R Jr, Nogueira LP, Caldas DL, Fontes BM, Luz A, Cazal JO, et al. Evaluation of corneal shape and biomechanics before LASIK. Int Ophthalmol Clin. (2011) 51:11–38. doi: 10.1097/IIO.0b013e31820f1d2d
20. Sawaguchi S, Fukuchi T, Abe H, Kaiya T, Sugar J, Yue BY. Three-dimensional scanning electron microscopic study of keratoconus corneas. Arch Ophthalmol. (1998) 116:62–8. doi: 10.1001/archopht.116.1.62
21. Reinstein DZ, Archer TJ, Randleman JB. Mathematical model to compare the relative tensile strength of the cornea after PRK, LASIK, and small incision lenticule extraction. J Refract Surg. (2013) 29:454–60. doi: 10.3928/1081597X-20130617-03
22. Guo H, Hosseini-Moghaddam SM, Hodge W. Corneal biomechanical properties after SMILE versus FLEX, LASIK, LASEK, or PRK: a systematic review and meta-analysis. BMC Ophthalmol. (2019) 19:167. doi: 10.1186/s12886-019-1165-3
Keywords: keratoconus, SP-A1, LASEK, corneal biomechanics, small incision lenticule extraction
Citation: Shang J, Shen Y, Jhanji V, Zhou X, Zhao J, Zhao Y and Zhou X (2021) Comparison of Corneal Biomechanics in Post-SMILE, Post-LASEK, and Keratoconic Eyes. Front. Med. 8:695697. doi: 10.3389/fmed.2021.695697
Received: 15 April 2021; Accepted: 12 August 2021;
Published: 14 September 2021.
Edited by:
Cynthia J. Roberts, The Ohio State University, United StatesReviewed by:
Ikhyun Jun, Yonsei University, South KoreaHamed Momeni-Moghaddam, Mashhad University of Medical Sciences, Iran
Copyright © 2021 Shang, Shen, Jhanji, Zhou, Zhao, Zhao and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xingtao Zhou, doctzhouxingtao@163.com
†These authors have contributed equally to this work and share first authorship
 Jianmin Shang1,2,3,4†
Jianmin Shang1,2,3,4†  Yang Shen
Yang Shen Vishal Jhanji
Vishal Jhanji Jing Zhao
Jing Zhao Yu Zhao
Yu Zhao Xingtao Zhou
Xingtao Zhou