- 1Department of Thyroid Surgery, China-Japan Union Hospital of Jilin University, Jilin Provincial Key Laboratory of Translational Medicine in Surgery, Jilin Provincial Engineering, Laboratory of Thyroid Disease Prevention and Treatment Changchun, Changchun, China
- 2Division of Surgery, Istituto Auxologico Italiano IRCCS (Istituto di Ricovero e Cura a Carattere Scientifico), Milan, Italy
- 3Department of Pathophysiology and Transplantation, University of Milan, Milan, Italy
Background: Although intraoperative neural monitoring (IONM) is well established in thyroid surgery, it is less commonly analyzed in parathyroid operations. This study presents the results of IONM for primary and secondary hyperparathyroidism surgery.
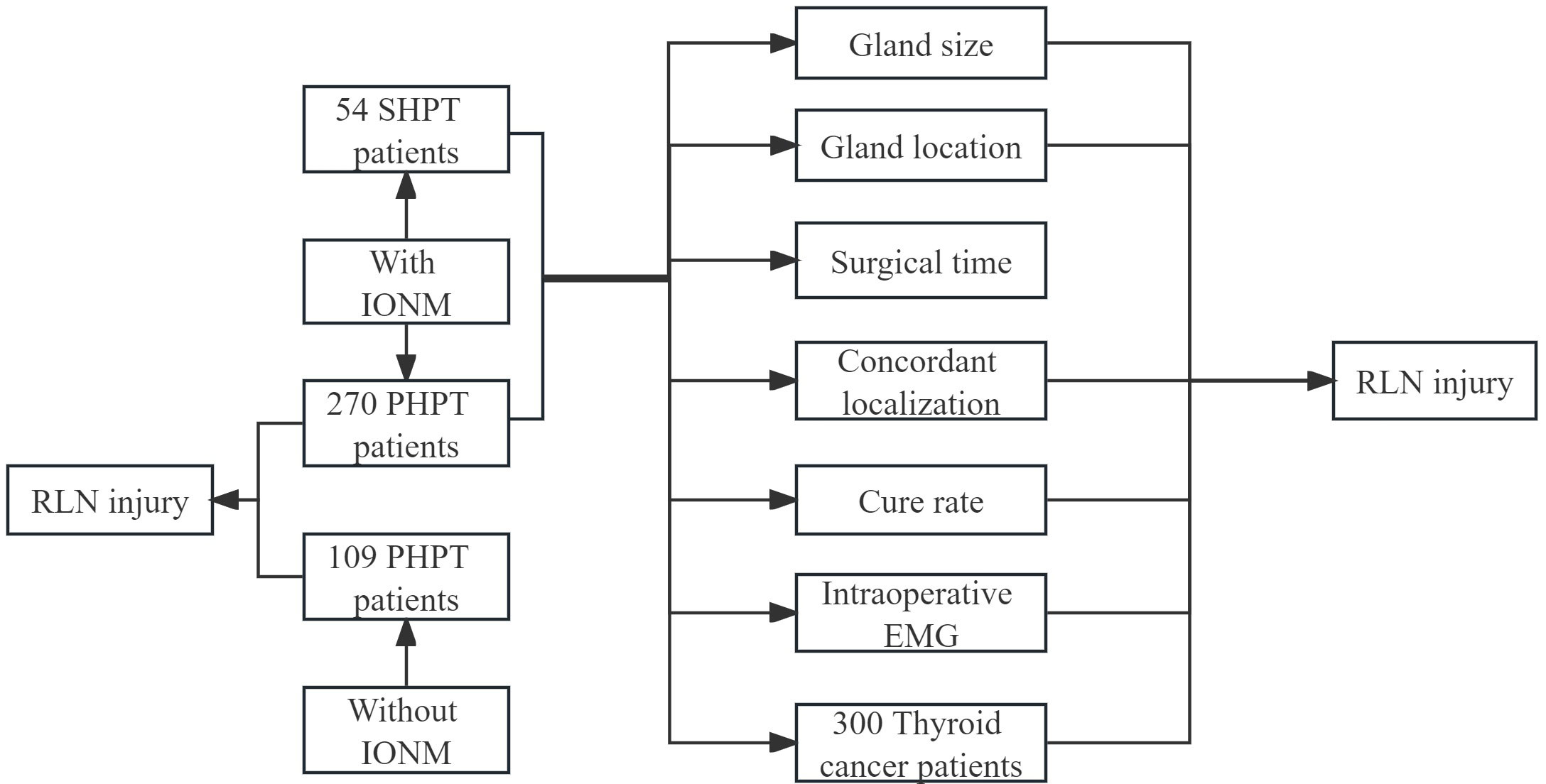
Methods: We retrospectively assessed 270 patients with primary hyperparathyroidism (PHPT), 53 patients with secondary hyperparathyroidism (SHPT), and 300 patients with thyroid cancer from June 2010 to June 2022 in one hospital in China. The follow-up was 12 months. Demographic, electromyography data from IONM, laboratory, and clinical information were collected. Laryngoscopy was collected from 109 patients with PHPT in whom IONM was not used. All groups were assessed by Pearson’s chi-square test and Fisher’s exact probability method to verify the relationship between parathyroid size and location, duration of surgery, preoperative concordant localization, laryngeal pain, IONM outcomes, cure rate, and RLN injury. Visual analog scale (VAS) assessed laryngeal pain. RLN outcomes were measured according to nerves at risk (NAR).
Results: The study comprehended 918 NAR, that is 272, 105, 109, and 432 NAR for PHPT, SHPT with IONM, PHPT without IONM, and thyroid surgery control group, respectively. IONM successfully prevented RLN injury (P<0.001, P=0.012): Fifteen (5.51%) RLNs experienced altered nerve EMG profiles during surgery, and five (1.84%) experienced transient RLN injury in PHPT patients. Five (4.76%) RLNs were found to have altered EMG profiles during surgery, and one (0.95%) RLN had a transient RLN injury in SHPT patients. There was no permanent nerve injury (0.00%) in this series. There was no association between location, gland size, preoperative concordant localization, cure rate, duration of surgery, and IONM (P >0.05). Duration of surgery was associated with postoperative pharyngeal discomfort (P=0.026, P=0.024). Transient RLN injury was significantly lower in patients with PHPT who underwent IONM than in those who did not. Intraoperative neuromonitoring played an effective role in protecting the recurrent laryngeal nerve (P=0.035). Compared with parathyroidectomy, thyroidectomy had a higher rate of RLN injury (5.32%, P<0.001).
Conclusion: IONM for SHPT and PHPT offers rapid anatomical gland identification and RLN functional results for effective RLN protection and reduced RLN damage rates.
1 Introduction
Parathyroidectomy (PTX) is an effective treatment for drug-refractory primary hyperparathyroidism (PHPT) and secondary hyperparathyroidism (SHPT) (1, 2). PHPT and SHPT have a high prevalence in China, and the incidence of PHPT and SHPT is increasing every year (3, 4).
Recurrent laryngeal nerve (RLN) injuries occur during PTX (5–11). The prevalence of transient RLN injury is 0.8% to 10.6% (8–11). The probability of permanent RLN injury ranges from 0.0% to 14.0% (8–11).
Although intraoperative nerve monitoring (IONM) is well-established in thyroid surgery, it is less frequently analyzed in parathyroid surgery (12–14). According to the international IONM guidelines, nerve monitoring is recommended in parathyroid surgery, but this suggestion is based on evidence from thyroid surgery, not parathyroid surgery (15).
This study presents the results of IONM in primary and secondary hyperparathyroidism surgery, focusing on surgical success rate, RLN outcomes, size and location of the parathyroid, duration of surgery, and pain compared to patients undergoing surgery without IONM.
2 Materials and methods
2.1 Time frame, patients, and setting
From June 2010 to June 2022, 270 patients with PHPT, 53 SHPT, 300 patients with thyroid cancer treated intraoperatively with IONM, and 109 patients with PHPT who did not receive IONM from the Department of Thyroid Surgery, China-Japan Union Hospital, Jilin University, China.
2.2 Ethics
Study registration number: 20230630016. The study was approved by the Institutional Review Board. Patients or their legal guardians will sign a detailed informed consent form before surgery.
2.3 PHPT and SHPT epidemiology in China
PHPT patients are increasing year by year. The number of patients with asymptomatic hyperparathyroidism is on the rise and has exceeded 50 percent of all patients until now (3). The number of patients with SHPT is increasing year by year, and according to statistics, the prevalence of CKD in China is estimated at 10.8 percent (4).
2.4 Inclusion and exclusion criteria
2.4.1 Inclusion criteria
We analyzed patients operated on for PHPT and SHPT compared with patients operated on for thyroid cancer with IONM and patients operated on for PHPT without IONM. Only patients with pre- (L1) and post-laryngoscopy (L2) were included on the first postoperative day. Patients with or without imaging concordant were included. All patients enrolled were ≥ 18 years old. Reoperation patients and patients with preoperative RLN injury included.
2.4.2 Exclusion criteria
(i) Patients with incomplete data or incomplete follow-up. (ii) Patients with concomitant thyroidectomy. (iii) Patients without L1 and/or L2. (iiii) Tertiary hyperparathyroidism and multiple endocrine neoplasms were excluded.
2.5 Definitions
PHPT was diagnosed by the presence of hypercalcemia and a concomitant elevated or inappropriately normal serum PTH level - specifically, PTH > 20 pg/ml with a serum Ca level of > 2.6 mmol/L. The diagnosis of asymptomatic PHPT (aPHPT) was based on the absence of typical symptoms or signs associated with hypercalcemia; the diagnosis was made incidentally on serum Ca level testing or neck ultrasound (US). SHPT is the release of increased amounts of parathyroid hormone, which is an appropriate response to a low calcium or vitamin D level to try to restore calcium levels to normal. Recurrent SHPT is defined as PTH <300 pg/ml within 6 months after surgery and PTH >300 pg/ml after 6 months again. Persistent SHPT is defined as PTH consistently >300 pg/ml after surgery. Laboratory tests included serum Ca (reference range, 2.00-2.60 mmol/L), serum phosphate (0.60-1.60 mmol/L), fasting blood glucose (FBS; 3.7-6.0 mmol/L), alkaline phosphatase (AKP; 50-135 U/L), serum creatinine (sCr; 58-133 umol/L), PTH (15-65 pg/mL) and 25-hydroxyvitamin D (25(OH)D; ≥30 ng/mL). Patients were referred and followed up by their referring endocrinologist.
2.6 Indications for surgery in SHPT patients
Patients with SHPT who undergo surgical treatment are mainly those who have failed medical treatment, whose PTH cannot be controlled within 9 times the normal reference value, and who have complications caused by HPT, or those who are inclined to undergo surgical treatment. The major complications are (1) uncontrolled hypercalcemia or hyperphosphatemia; (2) calcification defense or systemic severe extraosseous calcification; (3) cortical bone fracture; (4) weakened limb muscles and bone or joint pain that affects the quality of life; (5) uncontrolled itching that leads to lesions and/or affects the quality of life; and (6) patients with proximity to renal transplantation at risk of severe post-transplant hypercalcemia (16).
2.7 Preoperative localization examinations
Preoperative localization was performed by cervical ultrasound (US) and 99mTc-labelled sestamibi image. If the localization scans matched, the abnormal gland was identified using a focused minimally invasive approach, and if the scans did not match, standard bilateral neck exploration was performed.
2.8 Intraoperative gland localization
The localization (originating from the right superior, right inferior, left superior, or left inferior parathyroid gland) was determined perioperatively. The superior and inferior parathyroid glands may be very close to each other on a craniocaudal axis, but the typical landmark that was always used was the position of the parathyroid glands and any adenoma relative to the RLN. The upper parathyroid glands typically lie dorsal to the plane of the RLN, while the lower parathyroid glands lie ventral to the plane of the RLN, and in adenomatous enlargement, the migratory pathways of the upper and lower gland adenomas tend to respect this plane.
2.9 Intraoperative PTH
IOPTH values were initially checked after induction of anesthesia. They were then rechecked 30 minutes after surgical removal of the parathyroid gland. A > 50% drop in IOPTH levels 30 minutes after removal was used to confirm the successful removal of the abnormal gland.
2.10 Treatment
Surgical procedures were divided into (a) conventional: bilateral cervical exploration, visualization of all parathyroid glands, and removal of the pathological gland(s). (b) focused by open minimally invasive approach: identification and targeted removal of the gland(s) identified as pathological.
2.11 Variables
Sex, age, BMI, preoperative serum calcium, postoperative serum calcium, preoperative serum phosphorus, preoperative parathyroid hormone (PTH), IOPTH, alkaline phosphatase (ALP), IONM data, laryngoscopy data, parathyroid gland location and size, course of RLN, postoperative paraffin pathology. The most common postoperative complications were recorded (transient or permanent hypocalcemia; unilateral or bilateral paralysis of the vocal cords).
2.12 Grouping method
We analyzed: (a) the effect of IONM on RLN injury in PHPT and SHPT patients with IONM. (b) IONM compared to PHPT patients without IONM. (c) RLN injury rate compared to patients operated on for thyroid cancer in the same study period.
2.13 IONM technique
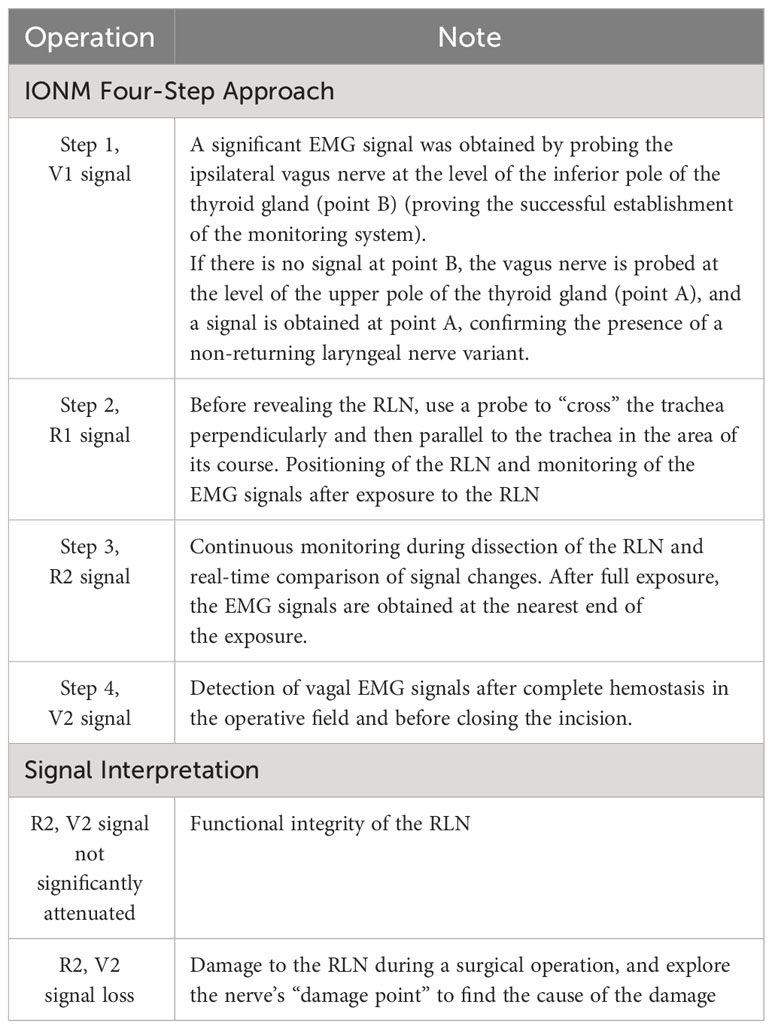
The RLN was monitored (Nerve Integrity Monitor 3.0 from Medtronic (USA)) according to the “four-step RLN monitoring method” proposed by Chiang et al. (17), i.e., V1, R1, V2, and R2 were recorded. During the surgery, intermittent monitoring was the main method, we continuously monitored the patient’s RLN with the IONM when the nerves were dissected. In the event of RLN injuries, we have archived all information, i.e. possible cause of injury, anatomical details of the parathyroid, and anatomical details of the nerve. The operating steps of the IONM are shown in Table 1. V1 and V2 were stimulated without dissection of the carotid sheath.
2.14 RLN follow-up
Intraoperative temporary nerve signal abnormalities were defined as the loss of nerve signal intraoperatively but recovery of nerve signal at the end of surgery. Intraoperative persistent nerve signal abnormalities are defined as the loss of nerve signal intraoperatively until the end of surgery. Patients with abnormal vocal fold movements were reexamined by laryngoscopy at the second, fourth, and sixth postoperative weeks.
Transient RLN injury is defined as symptoms of neuropraxia resolving within six months. Permanent RLN injury is defined as symptoms of neuropraxia persisting for six months.
2.15 Assessment of postoperative pharyngeal pain
The visual analog scale (VAS) (18) was used to assess the degree of pharyngeal pain experienced by patients on the first day after surgery.
2.16 Pathology
Paraffin pathology was done on all parathyroid glands removed and all pathology reports were recorded in detail.
2.17 Statistical methods
Statistics are for nerves at risk(NAR), not patients.SPSS 27.0 software was used for statistical analysis. Measurement data were expressed as mean ± standard deviation; count data were expressed as frequency and percentage (%). The Kruskal-Wallis rank sum test was used to compare continuous variables, the Pearson chi-square test was used for categorical variables, and Fisher’s exact probability method was used to compare theoretical frequencies < 1. P < 0.05 was statistically significant, and P < 0.01 was statistically significant.
3 Results
3.1 Basic information
3.1.1 Basic population
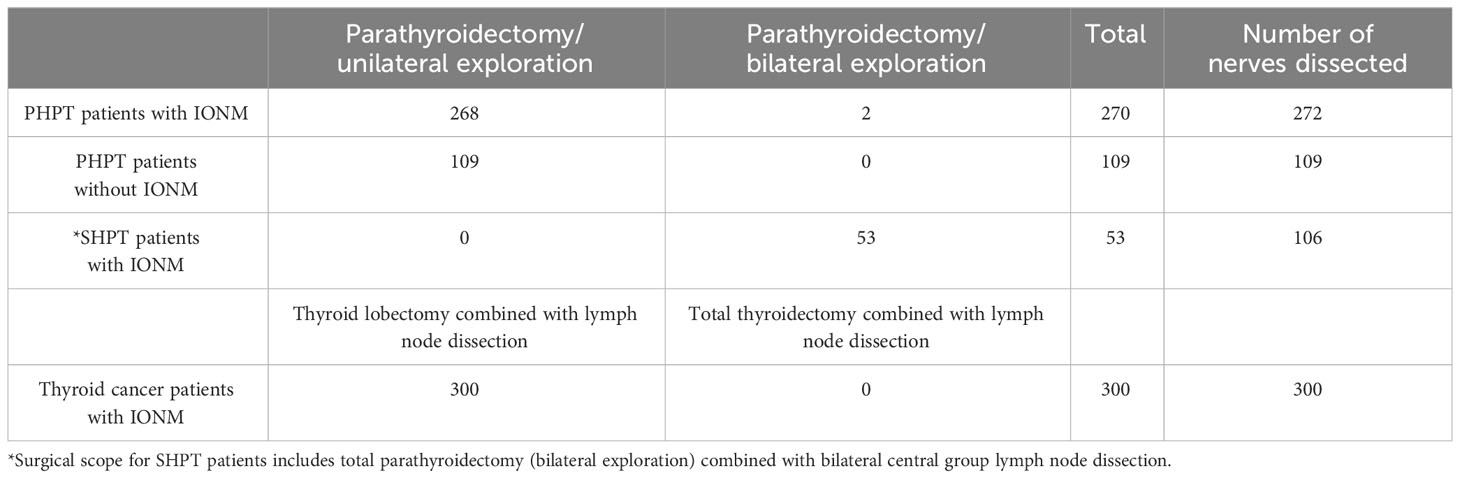
The study consists of 270 patients with PHPT, 53 SHPT, 300 patients with thyroid cancer treated intraoperatively with IONM, and 109 patients with PHPT who did not receive IONM. Some patients did not use IONM because of financial problems or for their own reasons. See Figure 1.
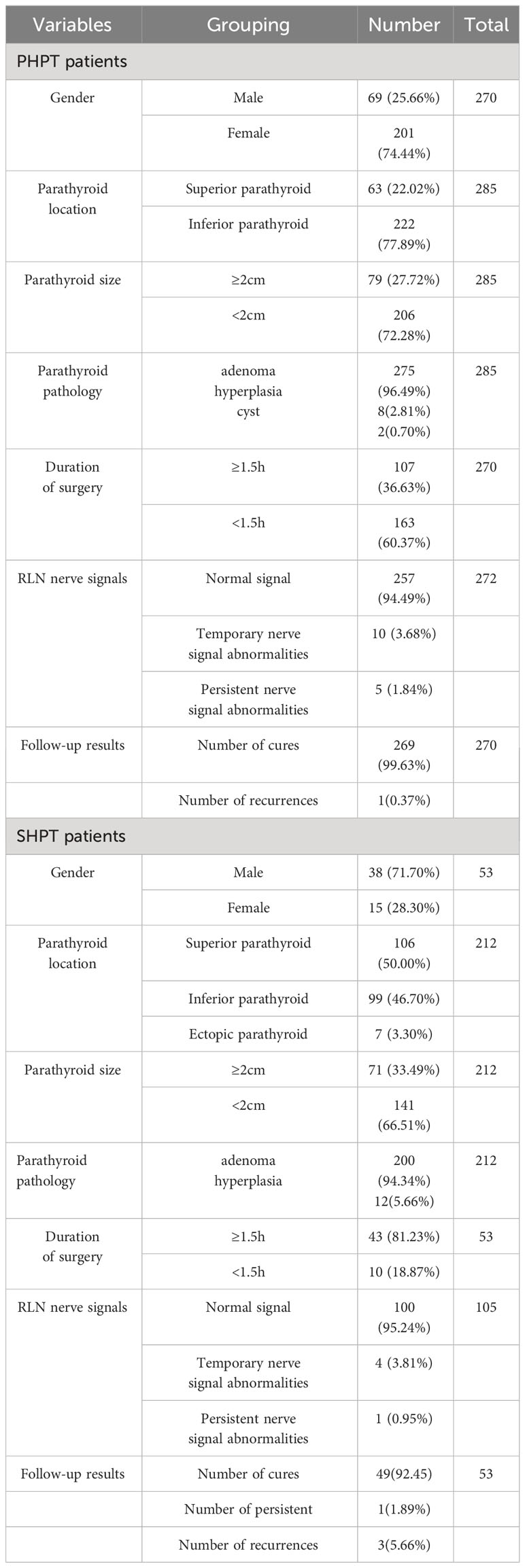
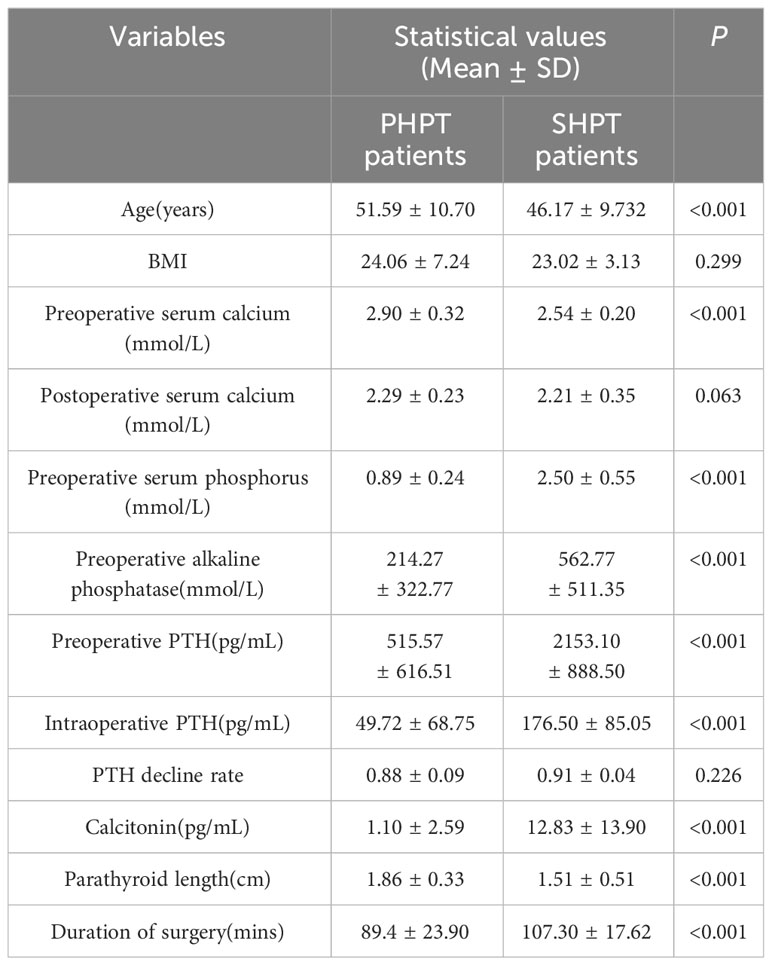
A higher percentage of female patients (74.4%) than male patients (25.6%) participated in the study with PHPT. The ratio of male to female patients at SHPT was 2.5:1. PHPT and SHPT patients were statistically significantly different in terms of age, preoperative serum calcium, preoperative serum phosphorus, preoperative alkaline phosphatase, preoperative PTH, intraoperative PTH, calcitonin, parathyroid length and duration of surgery (P < 0.05). See Tables 2, 3.
3.1.2 Pathology
In the PHPT group, more diseased parathyroid glands were located in the lower thyroid (77.89%) and less than 2 cm (72.28%); surgery lasted less than 1.5 hours in most patients (60.37%). In the SHPT group, 7 ectopic parathyroid glands were found, of which, 2 parathyroid glands were in the carotid sheath and 5 parathyroid glands were in the thymic horn. See Table 2.
Of 285 parathyroid glands in PHPT patients, adenomas were seen in 275 (96.49%), hyperplasia in eight (2.81%), and cysts in two (0.70%). Of 212 parathyroid glands of SHPT patients, adenomas appeared in 200 (96.34%) and hyperplasia in 12 (5.66%). See Table 2.
3.1.3 Follow-up examination
In this study, patients were followed up for 1 year after surgery. We found that: after 1 year, the cure rate of PHPT patients was 99.63% and one patient (0.37%) had recurrence. The cure rate of SHPT was 92.45%, three (5.66%) patients had recurrence and one (1.89%) patient had persistent hyperparathyroidism. See Table 2.
3.1.4 NAR
In the PHPT group, two hundred and seventy-two RLNs were dissected during the procedure. Fifteen RLNs (5.56%) had abnormal RLN signals during the procedure, and five RLNs (1.85%) had abnormal RLN signals at the end of surgery.
In the SHPT group, one hundred and five RLNs were dissected intraoperatively. Five RLNs (9.43%) had abnormal intraoperative RLN signals, and one RLN (1.89%) had abnormal RLN signals at the end of surgery. See Table 2.
3.1.5 Laryngeal examination results
In the preoperative laryngoscopy, we found that three patients who underwent reoperation had their right vocal folds fixed in a paramedian position and were hoarse, including two patients with PHPT and one with SHPT; the other patients had good vocal fold movement and no RLN injury. Laryngoscopy was repeated on the first day after surgery. Five (1.85%, 5/270) PHPT patients had transient RLN injury and one (1.89%, 1/53) SHPT patient had transient RLN injury. Laryngoscopy revealed that the left vocal cord was fixed in the paramedian position in four patients and the right vocal fold was fixed in the paramedian position in two patients. Laryngoscopies were performed every fortnight after surgery in six patients, and six weeks after surgery the movement of the bilateral vocal folds was symmetrical and well closed, without hoarseness or cough.
3.1.6 Surgical procedures
In the 270 PHPT patients with intraoperative use of IONM, 2 patients underwent parathyroidectomy/bilateral exploration and the others underwent unilateral exploration. All PHPT patients without intraoperative IONM underwent parathyroidectomy/unilateral exploration. All SHPT patients (53) underwent total parathyroidectomy (bilateral exploration) combined with bilateral central group lymph node dissection. 300 thyroid cancer patients underwent thyroid lobectomy combined with lymph node dissection. The details are shown in Table 4.
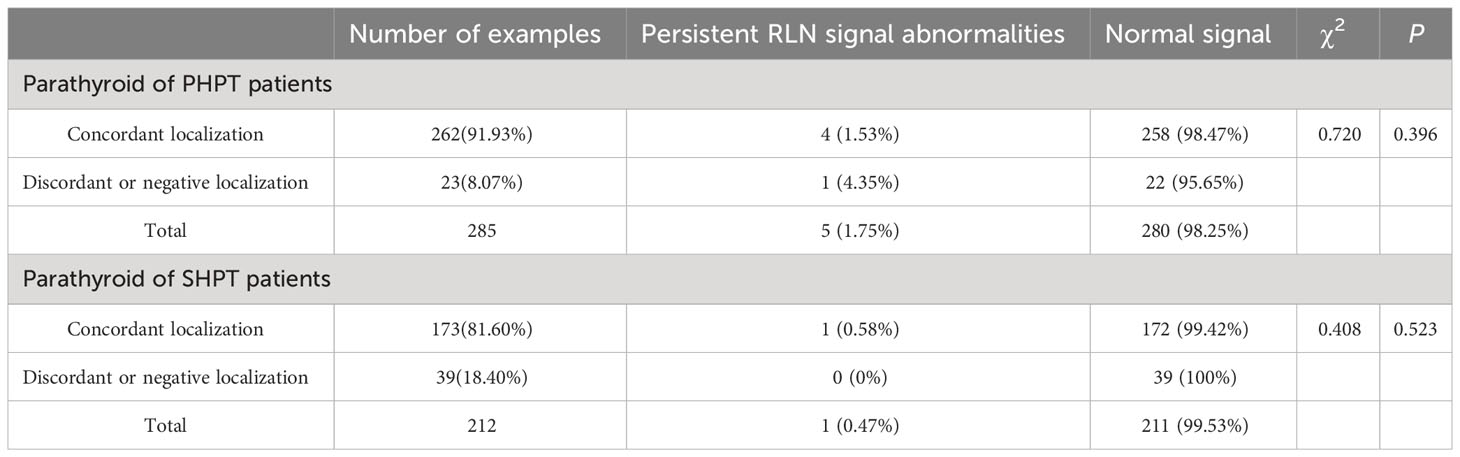
3.2 Relationship between RLN injury and preoperative concordant localization studies
Of the 285 parathyroids in patients with PHPT, a total of 262 (91.93%) parathyroids were localized consistently with the preoperative examination, of which four parathyroids were resected with persistent RLN nerve signal abnormality. Twenty-three (8.07%) parathyroids were localized inconsistently or without clear preoperative localization, and one parathyroid was resected with persistent RLN nerve signal abnormality. Of the 212 parathyroids in patients with SHPT, a total of 173 (81.60%) parathyroids were localized consistently with the preoperative examination, and one parathyroid was resected with persistent RLN nerve signal abnormality. Thirty-nine (18.40%) parathyroids were localized inconsistently or were not localized definitively preoperatively. Statistical findings: under IONM, there was no relationship between preoperative localization of parathyroids and RLN injury in PHPT patients (P=0.396) and SHPT patients (P=0.523). See Table 5.
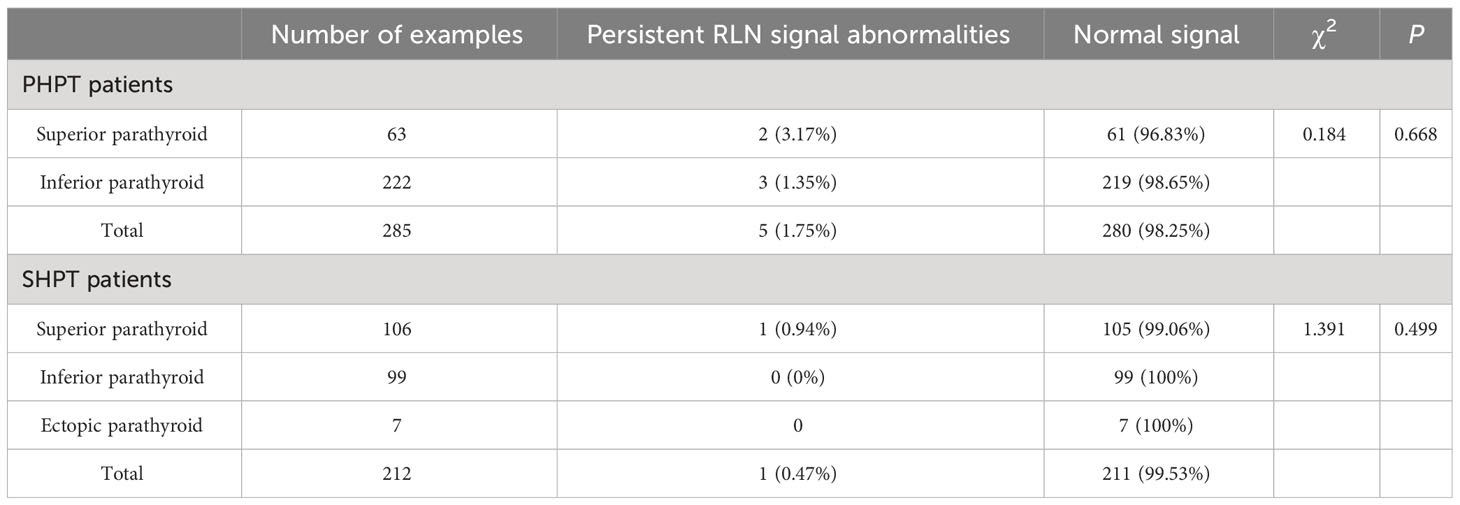
3.3 Relationship between glandular location and RLN injury
A total of 285 diseased parathyroid glands were resected in PHPT patients and 212 parathyroid glands in SHPT patients. In IONM, two RLNs had persistent RLN signaling abnormalities after resection of the upper parathyroid gland and three RLNs had persistent RLN signaling abnormalities after resection of the lower parathyroid gland in PHPT patients. One RLN had persistent RLN signaling abnormalities after upper parathyroid resection in SHPT patients. Statistically, there was no association between resection of a differently located parathyroid gland in PHPT (P=0.668) and SHPT patients (P=0.499) and RLN injury with IONM. See Table 6. Intraoperative pictures of our center which showed parathyroid glands in different locations with RLN. Figure 2.
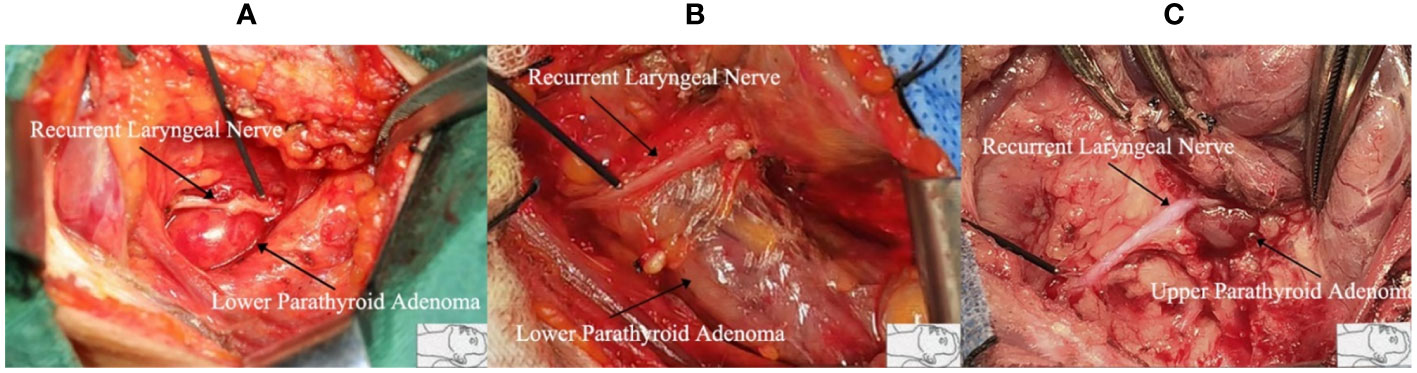
Figure 2 The different positions of the recurrent laryngeal nerve and parathyroid gland. (A) Inferior parathyroid adenoma protrudes upward. The recurrent laryngeal nerve is pushed up, and its course becomes shallow and easy to injure; (B) Inferior parathyroid adenoma is larger in size, grows toward the middle of the thyroid gland, and has a longer length of concomitant course with the recurrent laryngeal nerve, which makes the dissection of the recurrent laryngeal nerve more difficult; (C) Superior parathyroid adenoma is located at the point where the recurrent laryngeal nerve enters the larynx, where the surrounding tissues are dense. It is easy to injure and cause injury when the recurrent laryngeal nerve is separated from the mass.
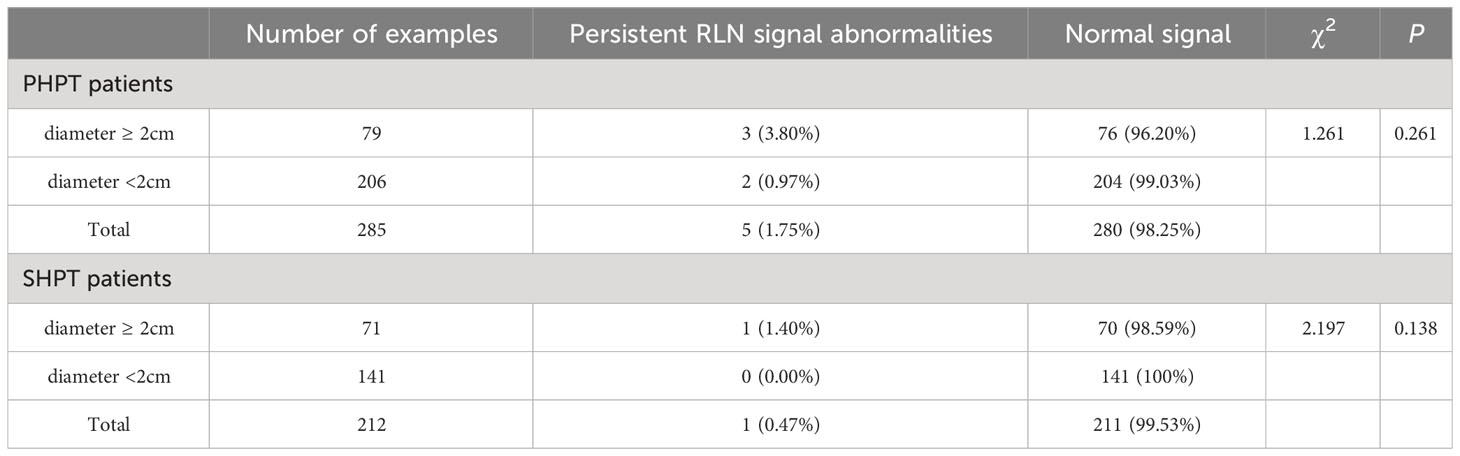
3.4 Gland size and RLN injury
The mean diameter of the diseased parathyroid gland in PHPT patients was 1.86 cm; seventy-nine parathyroid glands were ≥2 cm long, of which three (3.80%) RLNs had persistent RLN signaling abnormalities. Two hundred and six parathyroid glands were < 2 cm long, and two (0.97%) RLNs had persistent RLN signaling abnormalities. The mean diameter of the diseased parathyroid gland in SHPT patients was 1.51 cm, with 71 parathyroid glands ≥2 cm in length, of which one (1.40%) RLN had persistent RLN signaling abnormalities, and 141 parathyroid glands < 2 cm in length, without RLN injury. In IONM, RLN injury was not associated with parathyroid size in PHPT (P=0.261) and SHPT patients (P=0.138). See Table 7.
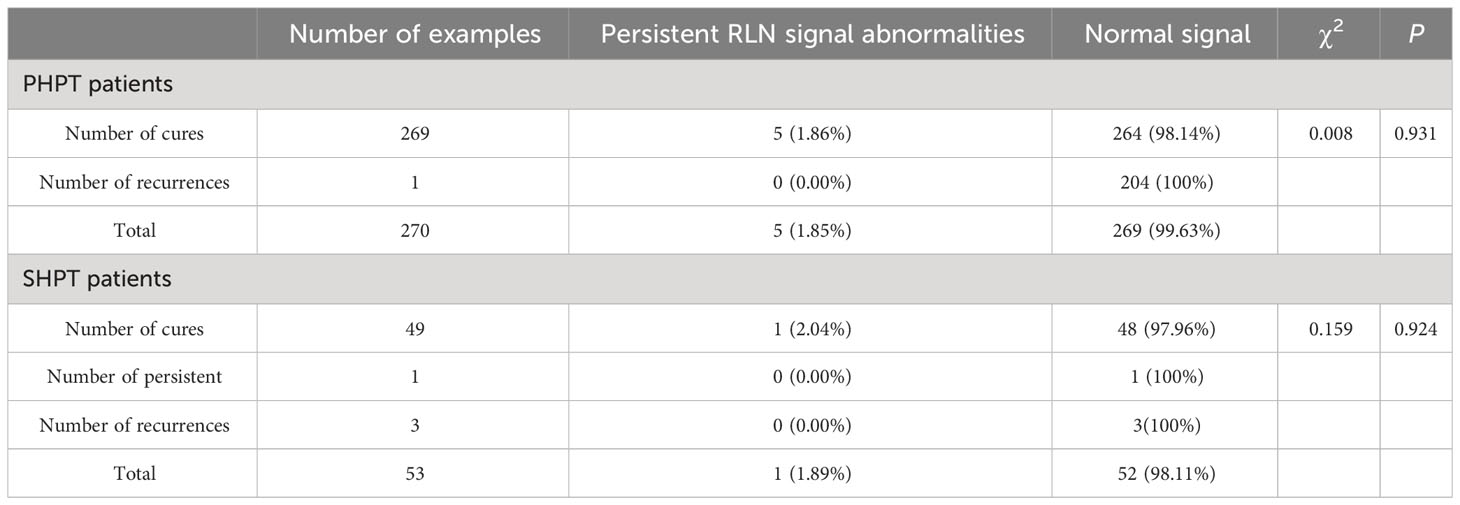
3.5 Cure rate and RLN injury
Of the 270 PHPT patients, all five (1.86%) patients who developed transient RLN damage were from the 269 cured patients. One (2.04%) of the 53 SHPT patients who developed transient RLN damage were from the cured patients. Statistical findings: under IONM, there was no relationship between cure rate, incidence of persistent hyperparathyroidism, recurrence rate, and RLN injury in PHPT patients (P=0.931) and SHPT patients (P=0.924). See Table 8.
3.6 Duration of surgery and RLN injury and pharyngeal symptoms
Of the 107 patients with PHPT whose surgery duration was more than 1.5 hours, four (3.73%) patients had temporary RLN injuries, and 91 (85.05%) patients had pharyngeal discomfort. Of the 163 patients with surgery duration of less than 1.5 hours, one (0.61%) patient was observed with transient RLN injury and 120 (73.62%) patients with pharyngeal discomfort. Forty-three patients with SHPT had a surgery duration of more than 1.5 hours, one (2.32%) patient with a transient RLN injury and 40 (90.67%) patients with pharyngeal complaints were observed. In the ten patients with surgery duration of less than 1.5 hours, there was no RLN injury and six patients (60.00%) had pharyngeal discomfort. The statistical results showed that in IONM, the duration of surgery (χ2 = 1.964, P=0.161; χ2 = 0.423, P=0.516) was not the cause of RLN injury and was a factor in postoperative pharyngeal discomfort (χ2 = 4.939, P=0.026; χ2 = 5.106, P=0.024) (see Figures 3A, B. The duration of surgery has a direct correlation with the incidence of postoperative pharyngeal discomfort, with longer surgeries resulting in a higher likelihood of patients experiencing this discomfort. Additionally, those who do experience postoperative pharyngeal discomfort are more likely to report moderate to severe pain. Figures 3C, D.
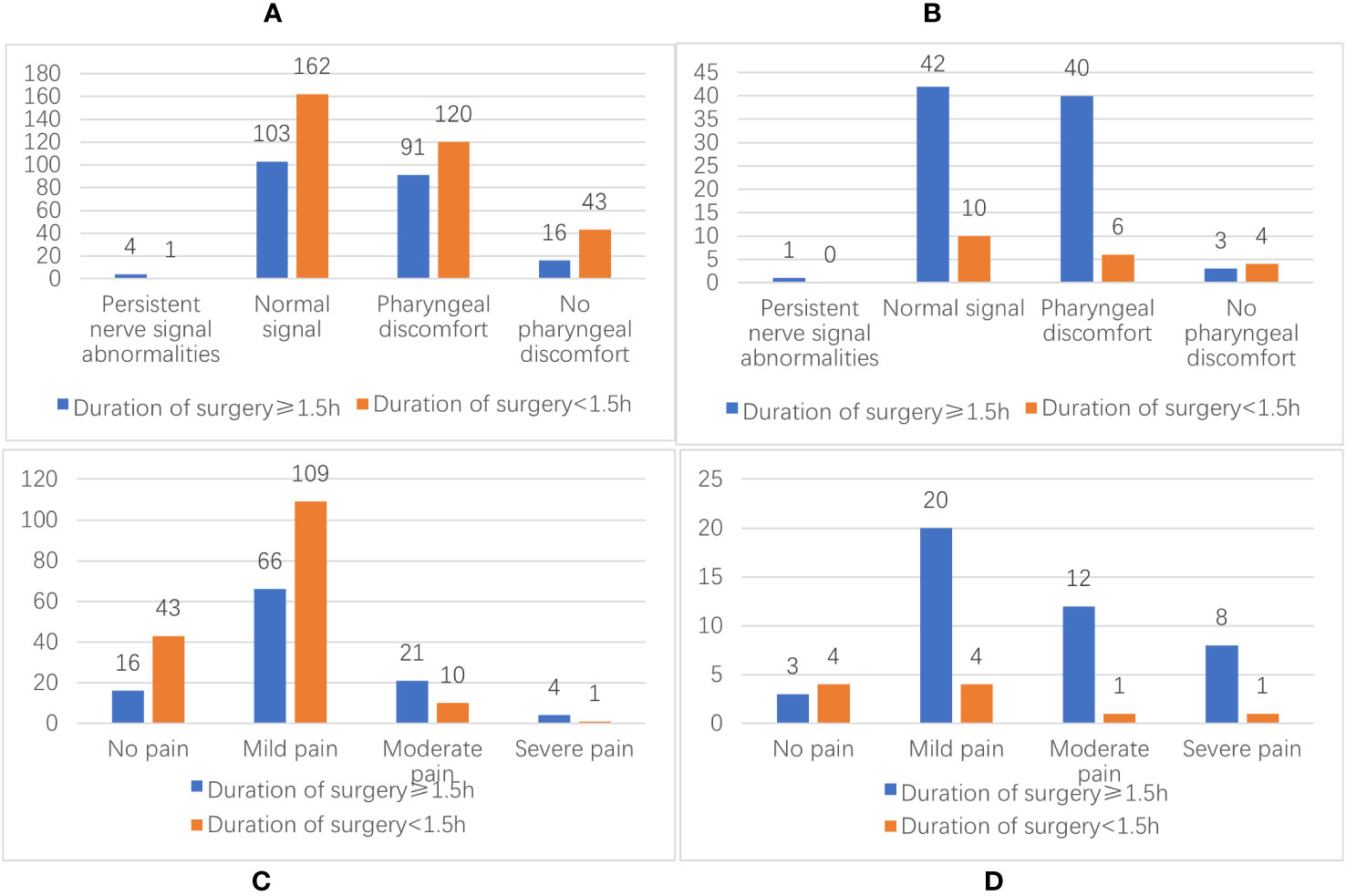
Figure 3 (A) Distribution of the duration of surgery and the number of RLN injuries and pharyngeal discomfort in PHPT patients; (B) Distribution of the duration of surgery and the number of RLN injuries and pharyngeal discomfort in SHPT patients; (C) Distribution of the number of PHPT patients with postoperative pharyngeal discomfort; (D) Distribution of the number of SHPT patients with postoperative pharyngeal discomfort.
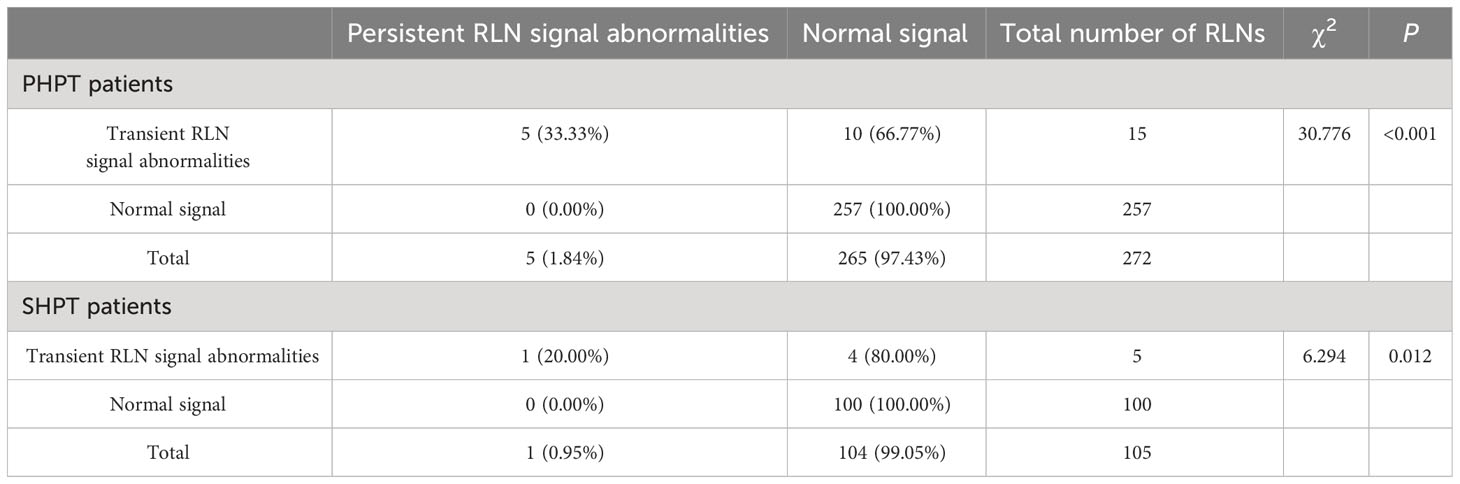
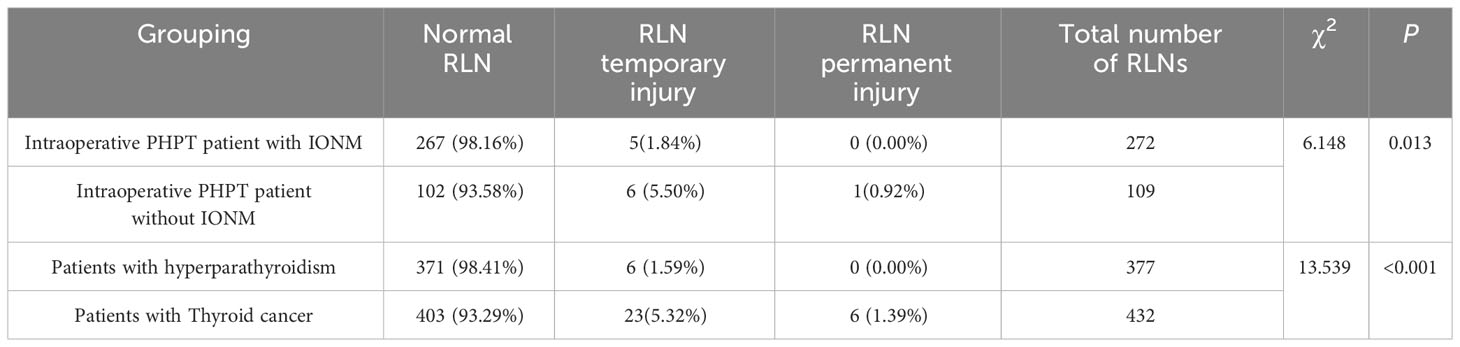
3.6.1 IONM for RLN injury (1)
With IONM, 15 (5.51%) RLNs had abnormal RLN signals, and only five (1.84%) had abnormal RLN signals at the end of surgery in 270 patients with PHPT. In 53 patients with SHPT, five RLNs (4.76%) had abnormal RLN signals during surgery, and only one RLN (0.95%) had abnormal RLN signals at the end of surgery. The statistical results showed that with IONM, the surgeon recognized the possible contributing factors for intraoperative nerve injury in time and avoided the risk. RLN injury was effectively prevented in PHPT patients (P < 0.001) and SHPT patients (P=0.012). See Table 9.
3.6.2 IONM and RLN injury (2)
To investigate whether IONM can protect RLN, 270 PHPT patients who used intraoperative IONM and 109 PHPT patients who did not use intraoperative IONM were counted. The rates of temporary RLN injury were 1.84% (5/272) and 5.50% (6/109) for both. The rates of permanent RLN injury were 0.00% and 0.92% (1/109), indicating that using IONM during surgery effectively protected against RLN (P =0.013). See Table 10.
3.7 Comparison of RLN injury between parathyroidectomy and thyroidectomy
Of the 323 patients who underwent parathyroidectomy with IONM, six (1.59%) RLN had transient RLN and no permanent injury. In comparison, twenty-three (5.32%) RLNs had a transient RLN injury and six (1.39%) RLNs had a permanent RLN injury in 432 RLNs in 300 patients who underwent thyroid lobectomy combined with lymph node dissection. The results showed that the likelihood of RLN injury was higher in patients who underwent radical thyroidectomy (P<0.001). See Table 10.
4 Discussion
IONM allows rapid localization of the nerve. Patients are characterized by morphological changes in the parathyroid gland, variable anatomical location, variations of the laryngeal nerve, and other features (19, 20). The incidence of the non-recurrent laryngeal nerve is statistically 0.26% to 0.99% on the right side and about 0.04% on the left side (21–24). 60.8% of the RLN runs within the tracheoesophageal groove, 4.9% of the RLN is more lateral to the trachea, and 28.3% of the RLN is directly posterior to the thyroid gland (25). The right RLN is more oblique in the paratracheal region than the left RLN (26); the RLN may be localized with the inferior thyroid artery in as many as 20 different ways (27, 28). Two non-recurrent laryngeal nerves have been identified at our center. Sometimes the arteriovenous thickness and morphology resemble the nerve, which is difficult to see with the naked eye; patients must undergo reoperation if the anatomy has changed, fibrous tissue is proliferating and there are severe tissue adhesions (5). All these conditions affect the accurate localization of the RLN, which in turn compromises the safety of the procedure. By using IONM to strictly implement the “four-step RLN monitoring method”,” continuous intraoperative monitoring, and other technical nerve monitoring procedures (17, 29), the nerve can be quickly localized and differentiated, improving the protection of the nerve and shortening the localization time.
4.1 Analysis of the relationship between IONM and preoperative localization of parathyroid glands
Currently, ultrasonography (US), computed tomography (CT), and single-photon emission computed tomography (SPECT)-CT with sestamibi Tc99m can achieve 100% accuracy in the preoperative localization of parathyroid glands (2, 30). Therefore intraoperative exploration of parathyroid glands that are not localized is common. According to the data in this study, there was no relationship between the preoperative accuracy of parathyroid gland localization and RLN injury in PHPT patients and SHPT patients under IONM. This suggests that IONM also plays a role in laryngeal recurrent nerve protection in the exploration and removal of parathyroid glands that fail to be accurately localized. The study by Karakas E et al. (31) also confirms that IONM in combination with other techniques can be effective in protecting the RLN during PHPT surgery.
4.1.1 Analysis of the relationship between IONM and parathyroid gland location
The literature reports that the upper parathyroid gland is mainly located within 2 cm of the junction of the inferior thyroid artery and the RLN in the cricothyroid joint area (4), which is a risk area for RLN injury during upper parathyroid resection. The lower parathyroid gland is mainly located in the lower pole of the thyroid gland, usually on the lateral side of the RLN. Some ectopic parathyroid glands even continue into the anterior mediastinum; in some SHPT patients, a partial thymectomy is required for surgery (32). The above area has a long RLN pathway and is difficult to detect, and it is also a vulnerable area for RLN injury in PTX. In our study, there was no statistically significant effect of parathyroid location on RLN injury, suggesting that the neurological safety of PTX in PHPT and SHPT patients was significantly improved by the use of IONM. The study by Brian R et al. (33) is identical to the present study.
4.2 Analysis of the relationship between IONM and parathyroid gland size
Nowadays, more and more surgeons choose to perform resection of the diseased parathyroid gland with a monopolar or bipolar electrometer (34), which has the advantages of less bleeding, faster clotting, and a gentle procedure, but also increases the risk of mild nerve damage such as heat conduction. According to a study by Zhao et al. (35), the distance between the electric knife and the nerve is unsafe within 3 mm. In the present study, it was found that some normal-sized or hyperplastic parathyroid glands may have a smaller distance to the recurrent laryngeal nerve, up to 1.5 mm. In the present study, there was no statistically significant effect of parathyroid gland size on RLN injury, suggesting that the neurological safety of PTX is significantly improved with IONM in PHPT and SHPT patients. One study shared the results of the present study, in which the right upper parathyroid mass was up to 0.25 ± 0.39 cm closer to the RLN compared to other parathyroid glands, and there was no permanent RLN injury after surgery in 136 patients with IONM (33).
IONM enables analysis of the mechanisms of nerve injury, prevention of nerve injury, and appropriate protection of nerves. With IONM, fifteen (5.51%) RLNs and five (4.76%) RLNs had abnormal intraoperative nerve signals in PHPT patients and SHPT patients in this study, and only five (1.84%) RLNs and one (0.95%) RLN, respectively, had abnormal nerve signals at the end of surgery. This is due to the continuous monitoring by the IONM, which provides real-time nerve signals to the surgeon. Any factors affecting the RLN signal are displayed and the surgeon can detect and avoid them in time through the IONM, which really protects the RLN. In an SHPT patient with a 2.1 x 0.9 cm left parathyroid gland, the RLN electromyographic signal R decreased from 1,226 V to 135 V when the parathyroid gland was exposed by pulling the thyroid gland during resection of the left upper parathyroid gland. The signal was restored by exposing the thyroid gland, indicating that the ligaments Berry was stuck in the left RLN, and the RLN signal was normal at the end of surgery. Three hundred and seventy-seven RLNs were identified in this group and dissected using IONM. The rate of transient injury in this group was 1.59%, with no permanent injury, and the rate of RLN injury was much lower than in PHPT patients without IONM (5.50%). It is also much lower than previous reports (6, 9, 36), which fully demonstrates the function of IONM in revealing and analyzing the mechanism of RLN injury and protecting the nerves.
Compared to parathyroidectomy, thyroid surgery poses a greater challenge to the protection of the RLN. In addition to the RLN anatomical factors described above, the infiltration of nerves by thyroid cancer, the greater length of the naked RLN, the presence of perioperative complications, the management of Berry’s ligament, the high likelihood of bleeding and difficulty of hemostasis near the RLN, lymph node dissection of the central group and multiple surgeries may affect the RLN signal (37–39). Therefore, thyroid surgery has a higher probability of RLN injury than parathyroid surgery, with the same statistical results as in the present study, with a probability of transient RLN injury of 5.32% and 1.59%, respectively. The rate of RLN injury in patients with thyroid cancer after IONM currently ranges from 2.6% to 6.0% (9, 14, 40).
Several studies have shown that IONM reduces the time to intraoperative detection of RLN by the surgeon (41, 42). In this study, we found that the duration of the procedure was not related to RLN injury and was associated with patients’ postoperative pharyngeal discomfort. The duration of surgery has a direct correlation with the incidence of postoperative pharyngeal discomfort, with longer surgeries resulting in a higher likelihood of patients experiencing this discomfort. Additionally, those who do experience postoperative pharyngeal discomfort are more likely to report moderate to severe pain. Therefore, IONM might play a role in patients’ postoperative pharyngeal pain. In this study, all patients underwent postoperative nebulization and oral inclusions and were discharged with significant symptom relief.
4.2.1 Protection of other nerves by IONM
Patients with damage to the outer branch of the SLN tend to have decreased pitch (43). There are several anatomical variants between the outer branch of the SLN and the superior(STA) thyroid artery, and there are many ways of typing. The accepted international typing standard is the Cernea (44). The outer branch of the SLN may pass below the upper margin of the superior thyroid pole and cross the STA, which is known as Cernea 2B, with an incidence of about 5% to 48.3% (45–47), in which the outer branch of the SLN passes in close relation to the superior parathyroid gland. Treatment of an abnormally enlarged upper parathyroid gland in patients with SHPT and PHPT can lead to nerve injury if not performed correctly. Cernea 2B SLN accounted for 25.39% (82/323) of cases in this group. IONM was used to monitor the continuity of the SLN throughout the procedure without injury. As there is currently no method to study SLN injury, only the patient’s complaints of choking on water or change in tone were used and no complications occurred. Very few enlarged parathyroid glands in SHPT patients are ectopic near the cervical sheath in the lateral neck, and there is a risk of vagus nerve boot injury with PTX. The relationship between the vagus nerve, the carotid artery, and the internal jugular vein in the cervical sheath is variable (48, 49), so intraoperative attention must be paid to ectopic parathyroid glands and the course of the nerve carefully determined. Intraoperative IONM improves the identification of the vagus nerve and reduces identification time (50, 51). In our group of SHPT patients, two patients had two parathyroid glands in the unilateral cervical sheath, and one of the preoperative patients had a parathyroid gland near the vagus nerve, which could be removed without injury to the vagus nerve by using IONM.
This study has the following limitations: it is a single-center retrospective study, which may introduce selection bias and cannot exclude the effect of single-center. The sample size of patients with SHPT (53 cases) is relatively small, and all of them received IONM. Data from patients with SHPT who did not receive IONM were not obtained, nor were clinical data from thyroid cancer patients who did not use IONM collected. Therefore, no analysis was performed on the data of patients with SHPT and thyroid cancer, whether they used or did not use IONM, to investigate the protective effect of IONM on the recurrent laryngeal nerve during surgery for SHPT and thyroid cancer. In the future, large-sample, multi-center, and prospective studies with random sampling are needed to better understand the role of IONM in the surgical treatment of SHPT and thyroid cancer, and to obtain more definitive research conclusions.
5 Conclusion
In this retrospective study, it was found that the use of IONM in PTX of PHPT and SHPT patients can rapidly identify and localize the laryngeal nerve intraoperatively, determine the functional integrity of the nerve by electromyographic signals, analyze the mechanism of nerve injury, and reduce the risk of laryngeal nerve injury due to irregular parathyroid hyperplasia, anatomical abnormalities of the laryngeal nerve, and tissue adhesions. IONM is undoubtedly a better tool in PTX of SHPT and PHPT patients. More clinicians and patients will benefit from the comprehensive and accurate application of IONM in PTX.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding authors.
Ethics statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part are appropriately investigated and resolved. The study was conducted by the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of China-Japan Union Hospital of Jilin University (approval number: 20230630016). The patients or their legal guardians sign a detailed informed consent form before surgery.
Author contributions
YM: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. XB: Writing – original draft, Writing – review & editing. JY: Data curation, Formal Analysis, Validation, Visualization, Writing – original draft. YL: Writing – review & editing. YuZ: Writing – review & editing. GD: Writing – review & editing. YiZ: Funding acquisition, Methodology, Supervision, Writing – review & editing. HS: Funding acquisition, Investigation, Methodology, Resources, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by Science and Technology Research Project of Education Department of Jilin Province, China, No.JJKH20221065KJ; Jilin Province Health Research Talent Special Project (No.2020SCZ03); Beijing Cihua Medical Development Foundation (J2023107004).
Acknowledgments
Thanks to all the members of the Pathology Department of China-Japan Union Hospital of Jilin University for their strong support to this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Khan AA, Hanley DA, Rizzoli R, Bollerslev J, Young JE, Rejnmark L, et al. Primary hyperparathyroidism: review and recommendations on evaluation, diagnosis, and management. A Canadian and international consensus. Osteoporos Int (2017) 28(1):1–19. doi: 10.1007/s00198-016-3716-2
2. Hiramitsu T, Hasegawa Y, Futamura K, Okada M, Goto N, Narumi S, et al. Treatment for secondary hyperparathyroidism focusing on parathyroidectomy. Front Endocrinol (Lausanne) (2023) 14:1169793. doi: 10.3389/fendo.2023.1169793
3. Liu Y, Guo S, Wu J, Wang R, Liu J, Liu Y, et al. Changes in clinical patterns of Chinese patients with primary hyperparathyroidism in the past 12 years: a single-center experience. Endocr Connect. (2021) 10(11):1428–34. doi: 10.1530/EC-21-0382
4. Zhang L, Wang F, Wang L, Wang W, Liu B, Liu J, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey [published correction appears in Lancet. Lancet (2012) 380(9818):815–22. doi: 10.1016/S0140-6736(12)60033-6
5. Zhao WJ, Luo H, Zhou YM, Gou ZH, Wang B, Zhu JQ. Preoperative ultrasound-guided carbon nanoparticles localization for metastatic lymph nodes in papillary thyroid carcinoma during reoperation: A retrospective cohort study. Med (Baltimore) (2017) 96(10):e6285. doi: 10.1097/md.0000000000006285
6. Hiramitsu T, Tomosugi T, Okada M, Futamura K, Goto N, Narumi S, et al. Intraoperative recurrent laryngeal nerve monitoring using endotracheal electromyography during parathyroidectomy for secondary hyperparathyroidism. J Int Med Res (2021) 49(3):3000605211000987. doi: 10.1177/03000605211000987
7. Dionigi G, Wu CW, Kim HY, Rausei S, Boni L, Chiang FY. Severity of recurrent laryngeal nerve injuries in thyroid surgery. World J Surg (2016) 40(6):1373–81. doi: 10.1007/s00268-016-3415-3
8. Astl J, Hložek J, Holý R, Rotnágl J. : Morbidity and mortality of parathyroid surgery - a retrospective analysis. Rozhl Chir (2021) 100(3):126–32. doi: 10.33699/pis.2021.100.3.126-132
9. Joliat GR, Guarnero V, Demartines N, Schweizer V, Matter M. Recurrent laryngeal nerve injury after thyroid and parathyroid surgery: Incidence and postoperative evolution assessment. Med (Baltimore) (2017) 96(17):e6674. doi: 10.1097/md.0000000000006674
10. Fowler GE, Chew PR, Lim CBB, Balasubramanian SP. Is there a role for routine laryngoscopy before and after parathyroid surgery? Surgeon (2019) 17(2):102–6. doi: 10.1016/j.surge.2018.08.002
11. Lin JX, Wen D, Sharma A, van der Werf B, Martin RCW, Harman R. Morbidity following thyroid and parathyroid surgery: Results from key performance indicator assessment at a high-volume centre in New Zealand. ANZ J Surg (2021) 91(9):1804–12. doi: 10.1111/ans.17099
12. Cleere EF, Davey MG, Young O, Lowery AJ, Kerin MJ. Intra-operative nerve monitoring and recurrent laryngeal nerve injury during thyroid surgery: a network meta-analysis of prospective studies. Langenbecks Arch Surg (2022) 407(8):3209–19. doi: 10.1007/s00423-022-02651-0
13. Kai H, Xixia L, Miaoyun L, Qinchang C, Xinzhi P, Dingyuan L, et al. Intraoperative nerve monitoring reduces recurrent laryngeal nerve injury in geriatric patients undergoing thyroid surgery. Acta Otolaryngol (2017) 137(12):1275–80. doi: 10.1080/00016489.2017.1354397
14. Barczyński M, Konturek A, Pragacz K, Papier A, Stopa M, Nowak W. Intraoperative nerve monitoring can reduce prevalence of recurrent laryngeal nerve injury in thyroid reoperations: results of a retrospective cohort study. World J Surg (2014) 38(3):599–606. doi: 10.1007/s00268-013-2260-x
15. Randolph GW, Dralle H, Abdullah H, Barczynski M, Bellantone R, Brauckhoff M, et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope (2011) 121 Suppl 1:S1–16. doi: 10.1002/lary.21119
16. Dream S, Kuo LE, Kuo JH, Sprague SM, Nwariaku FE, Wolf M, et al. The american association of endocrine surgeons guidelines for the definitive surgical management of secondary and tertiary renal hyperparathyroidism. Ann Surg (2022) 276(3):e141–76. doi: 10.1097/SLA.0000000000005522
17. Chiang FY, Lu IC, Kuo WR, Lee KW, Chang NC, Wu CW. The mechanism of recurrent laryngeal nerve injury during thyroid surgery–the application of intraoperative neuromonitoring. Surgery (2008) 143(6):743–9. doi: 10.1016/j.surg.2008.02.006
18. Kim WW, Lee J, Jung JH, Park HY, Tufano RP, Kim HY. A comparison study of the transoral and bilateral axillo-breast approaches in robotic thyroidectomy. J Surg Oncol (2018) 118(3):381–7. doi: 10.1002/jso.25175
19. Guilmette J, Sadow PM. Parathyroid pathology. Surg Pathol Clin (2019) 12(4):1007–19. doi: 10.1016/j.path.2019.08.006
20. Mohebati A, Shaha AR. Anatomy of thyroid and parathyroid glands and neurovascular relations. Clin Anat (2012) 25(1):19–31. doi: 10.1002/ca.21220
21. Henry JF, Audiffret J, Denizot A, Plan M. The nonrecurrent inferior laryngeal nerve: review of 33 cases, including two on the left side. Surgery (1988) 104(6):977–84.
22. Ardito G, Manni R, Vincenzoni C, Modugno P, Guidi ML. [The non-recurrent inferior laryngeal nerve. Surgical experience]. Ann Ital Chir (1998) 69(1):21–4.
23. Toniato A, Mazzarotto R, Piotto A, Bernante P, Pagetta C, Pelizzo MR. Identification of the nonrecurrent laryngeal nerve during thyroid surgery: 20-year experience. World J Surg (2004) 28(7):659–61. doi: 10.1007/s00268-004-7197-7
24. Niu ZX, Zhang H, Chen LQ, Shi H, Peng J, Su LW, et al. Preoperative computed tomography diagnosis of non-recurrent laryngeal nerve in patients with esophageal carcinoma. Thorac Cancer (2017) 8(1):46–50. doi: 10.1111/1759-7714.12409
25. Hisham AN, Lukman MR. Recurrent laryngeal nerve in thyroid surgery: a critical appraisal. ANZ J Surg (2002) 72(12):887–9. doi: 10.1046/j.1445-2197.2002.02578.x
26. Shindo ML, Wu JC, Park EE. Surgical anatomy of the recurrent laryngeal nerve revisited. Otolaryngol Head Neck Surg (2005) 133(4):514–9. doi: 10.1016/j.otohns.2005.07.010
27. Yalçin B. Anatomic configurations of the recurrent laryngeal nerve and inferior thyroid artery. Surgery (2006) 139(2):181–7. doi: 10.1016/j.surg.2005.06.035
28. Kulekci M, Batioglu-Karaaltin A, Saatci O, Uzun I. Relationship between the branches of the recurrent laryngeal nerve and the inferior thyroid artery. Ann Otol Rhinol Laryngol (2012) 121(10):650–6. doi: 10.1177/000348941212101005
29. Jonas J, Boskovic A. Intraoperative neuromonitoring (IONM) for recurrent laryngeal nerve protection: comparison of intermittent and continuous nerve stimulation. Surg Technol Int (2014) 24:133–8.
30. Ahn D, Kwak JH, Lee GJ, Sohn JH. Parathyroidectomy for primary hyperparathyroidism: A retrospective analysis of localization, surgical characteristics, and treatment outcomes. Asian J Surg (2023) 46(2):788–93. doi: 10.1016/j.asjsur.2022.07.032
31. Karakas E, Müller HH, Schlosshauer T, Rothmund M, Bartsch DK. Reoperations for primary hyperparathyroidism–improvement of outcome over two decades. Langenbecks Arch Surg (2013) 398(1):99–106. doi: 10.1007/s00423-012-1004-y
32. Noussios G, Anagnostis P, Natsis K. Ectopic parathyroid glands and their anatomical, clinical and surgical implications. Exp Clin Endocrinol Diabetes (2012) 120(10):604–10. doi: 10.1055/s-0032-1327628
33. Untch BR, Adam MA, Danko ME, Barfield ME, Dixit D, Scheri RP, et al. Tumor proximity to the recurrent laryngeal nerve in patients with primary hyperparathyroidism undergoing parathyroidectomy. Ann Surg Oncol (2012) 19(12):3823–6. doi: 10.1245/s10434-012-2495-z
34. Canu GL, Medas F, Podda F, Tatti A, Pisano G, Erdas E, et al. Thyroidectomy with energy-based devices: surgical outcomes and complications-comparison between Harmonic Focus, LigaSure Small Jaw and Thunderbeat Open Fine Jaw. Gland Surg (2020) 9(3):721–6. doi: 10.21037/gs.2020.03.31
35. Zhao Y, Li C, Wang T, Zhou L, Liu X, Xin J, et al. Translational study to standardize the safe use of bipolar forceps, ligaSure™, sonicision™ and plasmaBlade™ Around the recurrent laryngeal nerve in thyroid surgery. Surg Technol Int (2018) 31:sti32/990.
36. Steurer M, Passler C, Denk DM, Schneider B, Niederle B, Bigenzahn W. Advantages of recurrent laryngeal nerve identification in thyroidectomy and parathyroidectomy and the importance of preoperative and postoperative laryngoscopic examination in more than 1000 nerves at risk. Laryngoscope (2002) 112(1):124–33. doi: 10.1097/00005537-200201000-00022
37. de Danschutter SJ, Schreinemakers JM, Smit LH, van der Laan L, Nuytinck HK. Thyroid surgery and the usefulness of intraoperative neuromonitoring, a single center study. J Invest Surg (2015) 28(2):86–94. doi: 10.3109/08941939.2014.975876
38. Sarı S, Erbil Y, Sümer A, Agcaoglu O, Bayraktar A, Issever H, et al. Evaluation of recurrent laryngeal nerve monitoring in thyroid surgery. Int J Surg (2010) 8(6):474–8. doi: 10.1016/j.ijsu.2010.06.009
39. Maneeprasopchoke P, Chongkolwatana C, Pongsapich W, Iwata AJ, Kamani D, Randolph GW. Intraoperative nerve monitoring in thyroid surgery: Analysis of recurrent laryngeal nerve identification and operative time. Laryngoscope Investig Otolaryngol (2021) 6(2):354–61. doi: 10.1002/lio2.543
40. Zhao Y, Zhao Z, Zhang D, Han Y, Dionigi G, Sun H. Improving classification of the external branch of the superior laryngeal nerve with neural monitoring: a research appraisal and narrative review. Gland Surg (2021) 10(9):2847–60. doi: 10.21037/gs-21-518
41. Cernea CR, Ferraz AR, Nishio S, Dutra A Jr., Hojaij FC, dos Santos LR. Surgical anatomy of the external branch of the superior laryngeal nerve. Head Neck (1992) 14(5):380–3. doi: 10.1002/hed.2880140507
42. Ahmad R, Saraf A, Kishore K, Kalsotra P. Relation of superior laryngeal nerve and superior thyroid artery with superior pole of thyroid during thyroid surgery. Indian J Otolaryngol Head Neck Surg (2022) 74(Suppl 2):2095–8. doi: 10.1007/s12070-020-01949-z
43. Menon RR, Murali S, Nair CG, Babu MJC, Jacob P. Correlation between the cernea classification of external branch of superior laryngeal nerve in relation to the ultrasound-based volume of thyroid gland. Indian J Endocrinol Metab (2017) 21(6):845–7. doi: 10.4103/ijem.IJEM_230_17
44. Pagedar NA, Freeman JL. Identification of the external branch of the superior laryngeal nerve during thyroidectomy. Arch Otolaryngol Head Neck Surg (2009) 135(4):360–2. doi: 10.1001/archoto.2009.9
45. Planitzer U, Hammer N, Bechmann I, Glätzner J, Löffler S, Möbius R, et al. Positional relations of the cervical vagus nerve revisited. Neuromodulation (2017) 20(4):361–8. doi: 10.1111/ner.12557
46. Cunningham CJ, Martínez JL. The wandering nerve: positional variations of the cervical vagus nerve and neurosurgical implications. World Neurosurg (2021) 156:105–10. doi: 10.1016/j.wneu.2021.09.090
47. Phelan E, Potenza A, Slough C, Zurakowski D, Kamani D, Randolph G. Recurrent laryngeal nerve monitoring during thyroid surgery: normative vagal and recurrent laryngeal nerve electrophysiological data. Otolaryngol Head Neck Surg (2012) 147(4):640–6. doi: 10.1177/0194599812447915
48. Wang Y, Wang P, Yu X. [The exposure of vagus nerve and continuous intraoperative neural monitoring in thyroid surgery]. Zhonghua Wai Ke Za Zhi (2016) 54(11):828–32. doi: 10.3760/cma.j.issn.0529-5815.2016.11.008
49. More Y, Shnayder Y, Girod DA, Sykes KJ, Carlisle MP, Chalmers B, et al. Factors influencing morbidity after surgical management of Malignant thyroid disease. Ann Otol Rhinol Laryngol (2013) 122(6):398–403. doi: 10.1177/000348941312200609
50. Snyder SK, Lairmore TC, Hendricks JC, Roberts JW. Elucidating mechanisms of recurrent laryngeal nerve injury during thyroidectomy and parathyroidectomy. J Am Coll Surg (2008) 206(1):123–30. doi: 10.1016/j.jamcollsurg.2007.07.017
51. Mahoney RC, Vossler JD, Murayama KM, Woodruff SL. Predictors and consequences of recurrent laryngeal nerve injury during open thyroidectomy: An American College of Surgeons National Surgical Quality Improvement Project database analysis. Am J Surg (2021) 221(1):122–6. doi: 10.1016/j.amjsurg.2020.07.023
Keywords: primary hyperparathyroidism, secondary hyperparathyroidism, parathyroidectomy, intraoperative neural monitoring, IONM, recurrent laryngeal nerve, morbidity, pain
Citation: Mu Y, Bian X, Yang J, Li Y, Zhang Y, Dionigi G, Zhao Y and Sun H (2023) Recurrent laryngeal never monitoring versus non-monitoring in parathyroid surgery. Front. Endocrinol. 14:1299943. doi: 10.3389/fendo.2023.1299943
Received: 23 September 2023; Accepted: 13 November 2023;
Published: 28 November 2023.
Edited by:
Takahisa Hiramitsu, Japanese Red Cross Nagoya Daini Hospital, JapanReviewed by:
Claudio Casella, University of Brescia, ItalyEliana Piantanida, University of Insubria, Italy
Pietro Princi, Ospedale Cristo Re, Italy
Copyright © 2023 Mu, Bian, Yang, Li, Zhang, Dionigi, Zhao and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yishen Zhao, zhaoys1203@jlu.edu.cn; Hui Sun, s_h@jlu.edu.cn
†These authors have contributed equally to this work
 Yongliang Mu
Yongliang Mu Xuehai Bian1†
Xuehai Bian1† Yushuai Zhang
Yushuai Zhang Gianlorenzo Dionigi
Gianlorenzo Dionigi