Relationship Between First 24-h Mean Body Temperature and Clinical Outcomes of Post-cardiac Surgery Patients
- 1Department of Anesthesiology, The Affiliated Hospital, School of Medicine, Chengdu Women's & Children's Central Hospital, UESTC, Chengdu, China
- 2West China of Medical School, Sichuan University, Chengdu, China
- 3Department of Cardiovascular Surgery, West China Hospital, Sichuan University, Chengdu, China
Background: This study was aimed to investigate the relationship between first 24-h mean body temperature and clinical outcomes of post cardiac surgery patients admitted to intensive care unit (ICU) in a large public clinical database.
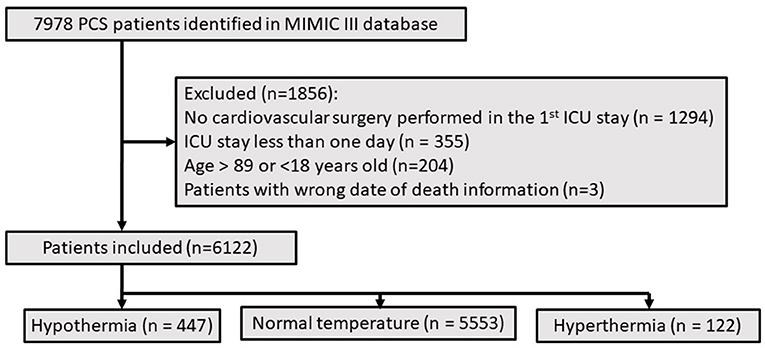
Methods: This is a retrospectively observational research of MIMIC III dataset, a total of 6,122 patients included. Patients were divided into 3 groups according to the distribution of body temperature. Multivariate cox analysis and logistic regression analysis were used to investigate the association between abnormal temperature, and clinical outcomes.
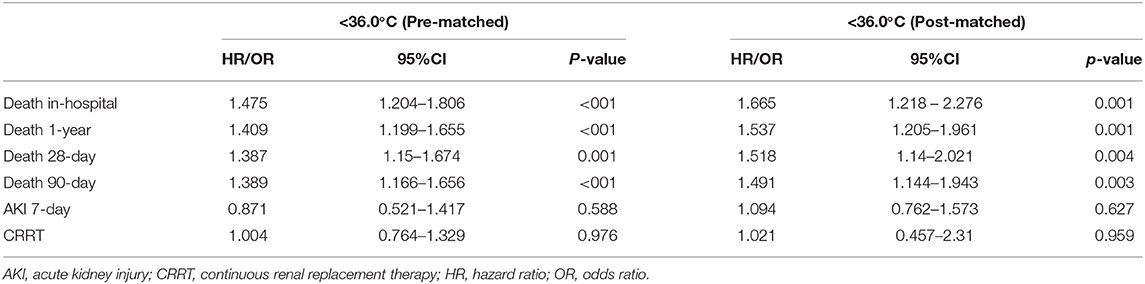
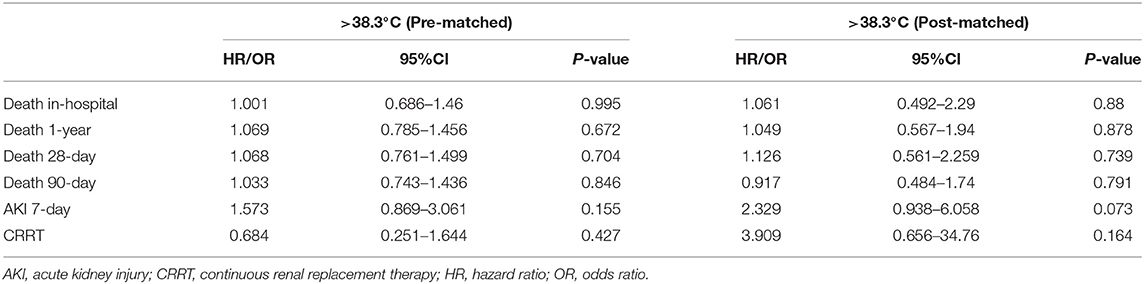
Results: Hypothermia (<36°C) significantly associated with increasing in-hospital mortality (HR 1.665, 95%CI 1.218–2.276; p = 0.001), 1-year mortality (HR 1.537, 95% CI 1.205–1.961; p = 0.001), 28-day mortality (HR 1.518, 95% CI 1.14–2.021; p = 0.004), and 90-day mortality (HR 1.491, 95% CI 1.144–1.943; p = 0.003). No statistical differences were observed between short-term or long-term mortality and hyperthermia (>38°C). Hyperthermia was related to the extended length of ICU stay (p < 0.001), and hospital stay (p < 0.001).
Conclusion: Hypothermia within 24h after ICU admission was associated with the increased mortality of post cardiac surgery patients. Enhanced monitoring of body temperature within 24h after cardiac surgery should be taken into account for improving clinical outcomes.
Introduction
The management of body temperature (BT) was very important to the recovery of postoperative patients, especially for critically ill patients who have relatively severe physical conditions. Almost 57.1% patients were exposed to hypothermia (BT <36.0°C) among the patients admitted to intensive care unit (ICU) after operation (1) which claimed to be associated with mortality (2). Postoperative hyperthermia might be relevant to adverse clinical outcomes (3), and infection (4) in critically ill patients. Previous studies had indicated general anesthesia and surgical influence disturbed normal temperature regulation mechanism (5). Without preventative actions, influence of abnormal body temperature could be exaggerated with serious consequences.
As a special operation type, cardiac surgery had a great impact on circulation and physiology, and also brought enormous challenges to reduce mortality. Hypothermia and hyperthermia might occur after cardiac surgery attributed to long-term anesthesia and surgery exposure, the failure of the temperature maintenance, special hypothermia treatment and inflammatory response, and so on. Hyperthermia after cardiovascular surgery with cardiopulmonary bypass (CPB) could cause cognitive decline (3, 6). Grocott and colleagues revealed that postoperative high fever was associated with cognitive impairment at 6 weeks after coronary artery bypass grafting (6). Besides, there was study reporting that hypothermia effectively promoted endotoxin release through ischemic intestinal mucosa and had bad effects on brain tissue (7). Abnormal body temperature is disadvantageous to the prognosis of patients.
There were few studies explored the relationship between body temperature and adverse outcomes of patients after cardiac surgery, and no unified conclusion was obtained. Body temperature at single point in time raised bias risk inevitably (8), and could not fully reflect the overall effect of early postoperative body temperature. The object of this study was to investigate the association between first 24-h mean body temperature and clinical outcomes of post cardiac surgery patients admitted to ICU in a large public clinical database.
Materials and Methods
Data Source
The study is a retrospective study with data collected from Medical Information Mart for Intensive Care-III (MIMIC-III) database (9, 10). This is a large intensive care database open to the public including more than 40,000 patients admitted to ICU from Beth Israel Deaconess Medical Center (Boston, Massachusetts, USA) between 2001 and 2012. Beth Israel Deaconess Medical Center and the Beth Israel Deacon Medical Center's institutional review board approved the application of the database (approval code 40043439) and personal informed consent was abandoned.
Study Population
Patients with cardiac surgery were identified using current procedural terminology numbered from 33,010 to 37,799. 18 to 89 years old patients were enrolled into the study. If patients were admitted to hospital or ICU multiple times, only the first record was analyzed. Patients stayed ICU <24h were excluded. Based on the attribution of temperature and existing research (11), Patients were divided into 3 groups: hypothermia group (BT <36.0°C), normal group (36.0°C ≤ BT ≤ 38.3°C), hyperthermia group (BT > 38.3°C).
Data Collection and Definitions
The data was extracted from database by using structure query language (PostgreSQL, version 9.4.6, www.postgresql.org),and the codes in MIMIC Code Repository (https://github.com/MIT-LCP/mimic-website). Variables of this study included demographics, comorbidities, scoring systems, laboratory tests, and vital signs. Calculate the average of vital signs and laboratory tests with multiple results within 24h after ICU admission. Data analysis excluded variables with missing values exceeding 30% to avoid potential bias. Multiple imputation method was used to process variables with missing values <30%.
Outcomes
The primary outcomes were in-hospital and 1-year mortality. The secondary outcomes included survival time, 28-day mortality, 90-day mortality, length of hospital stay and ICU stay, the intervention of continuous renal replacement therapy (CRRT) within 24h admitted to ICU, the incidence of acute kidney injury (AKI) within 7 days after ICU admission. The diagnosis of AKI was confirmed following the Kidney Disease: improving global outcomes (KDIGO) guideline (12).
Statistical Analysis
Most continuous variables in this research were checked to be non-normally distributed and described as medians with interquartile ranges (IQRs), the rest were reported as mean ± standard deviation. Categorical variables were described as number and rate. Comparisons were performed with Kruskal-Wallis test or Mann-Whitney U or Welch's t test for continuous variables and chi-square or Fisher's exact tests for categorical variables. Propensity score matching (PSM) (13) was performed to adjust the imbalance of baseline between different groups. All selected variables were analyzed by univariate analysis firstly. Multivariate cox analysis or multivariate logistic regression analysis were performed to investigate relationships between abnormal temperature and clinical outcomes through adjusting confounding factors post-matched which had been analyzed in univariate analysis models with P < 0.05. Kaplan-Meier survival curves of 1 year mortality in different groups were constructed and compared by the log-rank test.
Data cleaning, statistical analyses and illustrations were conducted by using SPSS software version 24.0 (IBM Corporation, Armonk, NY, USA) and R software (version 4.0.3) consisted of “tableone” (14), “ggplot2” (15), “survival” (16), “survminer” (17), “lubridate” (18), “tidyverse” (19). P < 0.05 was considered statistically significant.
Result
Baseline Characteristics
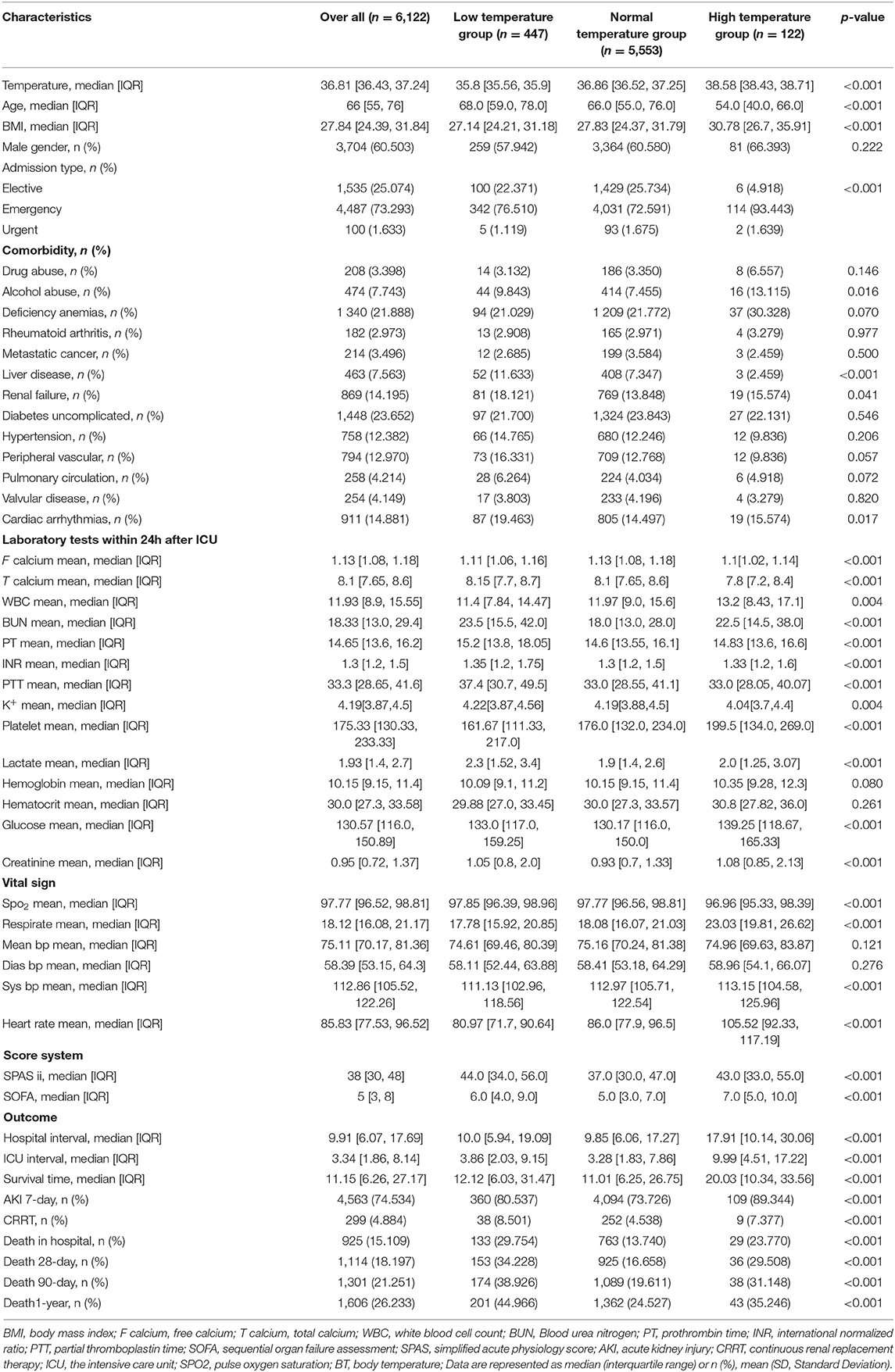
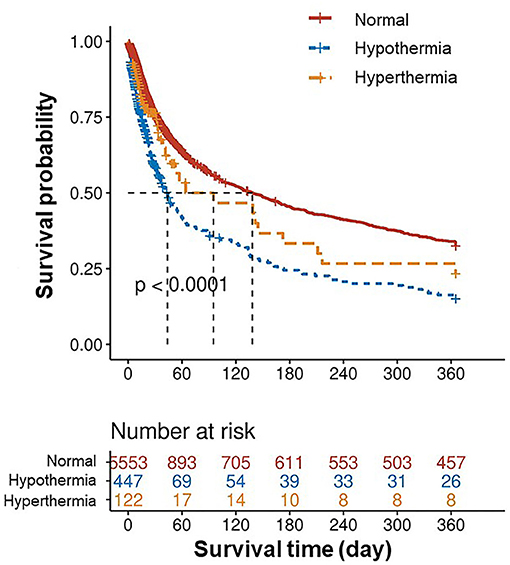
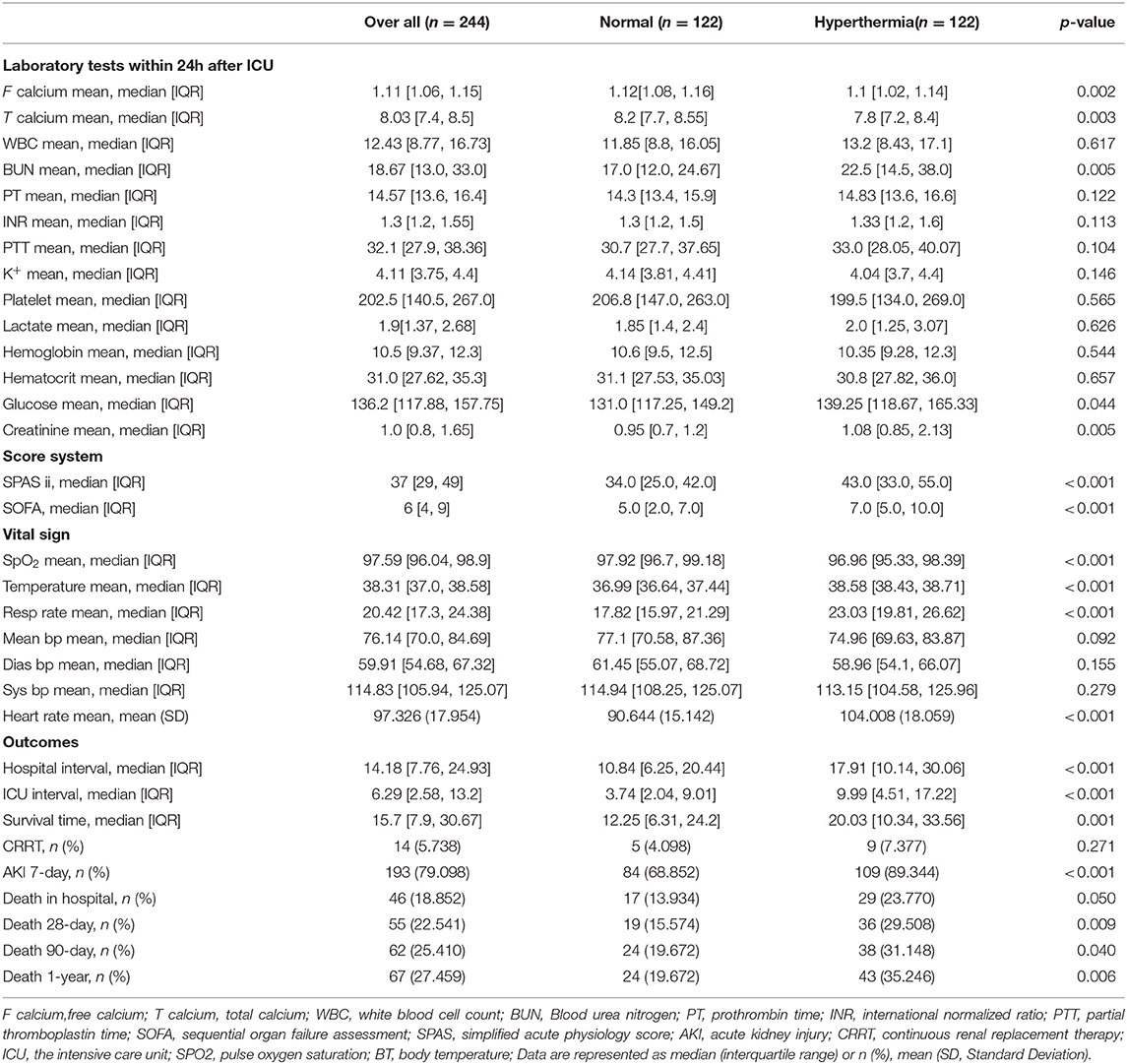
There were 6,122 patients concluded in our study (Figure 1), 447 patients (7.3%) belonged to hypothermia, 122 patients (2.0%) belonged to hyperthermia, 5,553 patients (90.7%) belonged to normal group. Clinical and laboratory test baseline characteristics of the populations were reported in Table 1. The association between body temperature and in-hospital mortality was described in Figure 2A (95% CI −0.043, −0.016, p < 0.001). The relationship between body temperature and 1-year mortality was shown in Figure 2B (95% CI −0.065, −0.032, p < 0.001). There were statistical differences between body temperature distribution of first 24- h after ICU admission and long-term mortality, that was described in Figure 3 (log-rank p < 0.001).
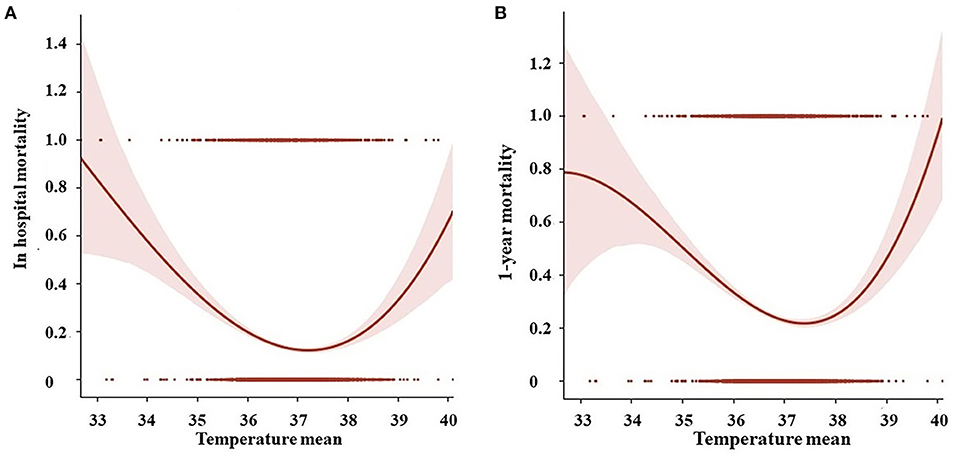
Figure 2. The relationship between (A) body temperature and in-hospital mortality; (B) body temperature and 1-year mortality by Polynomial regression.
Hypothermia
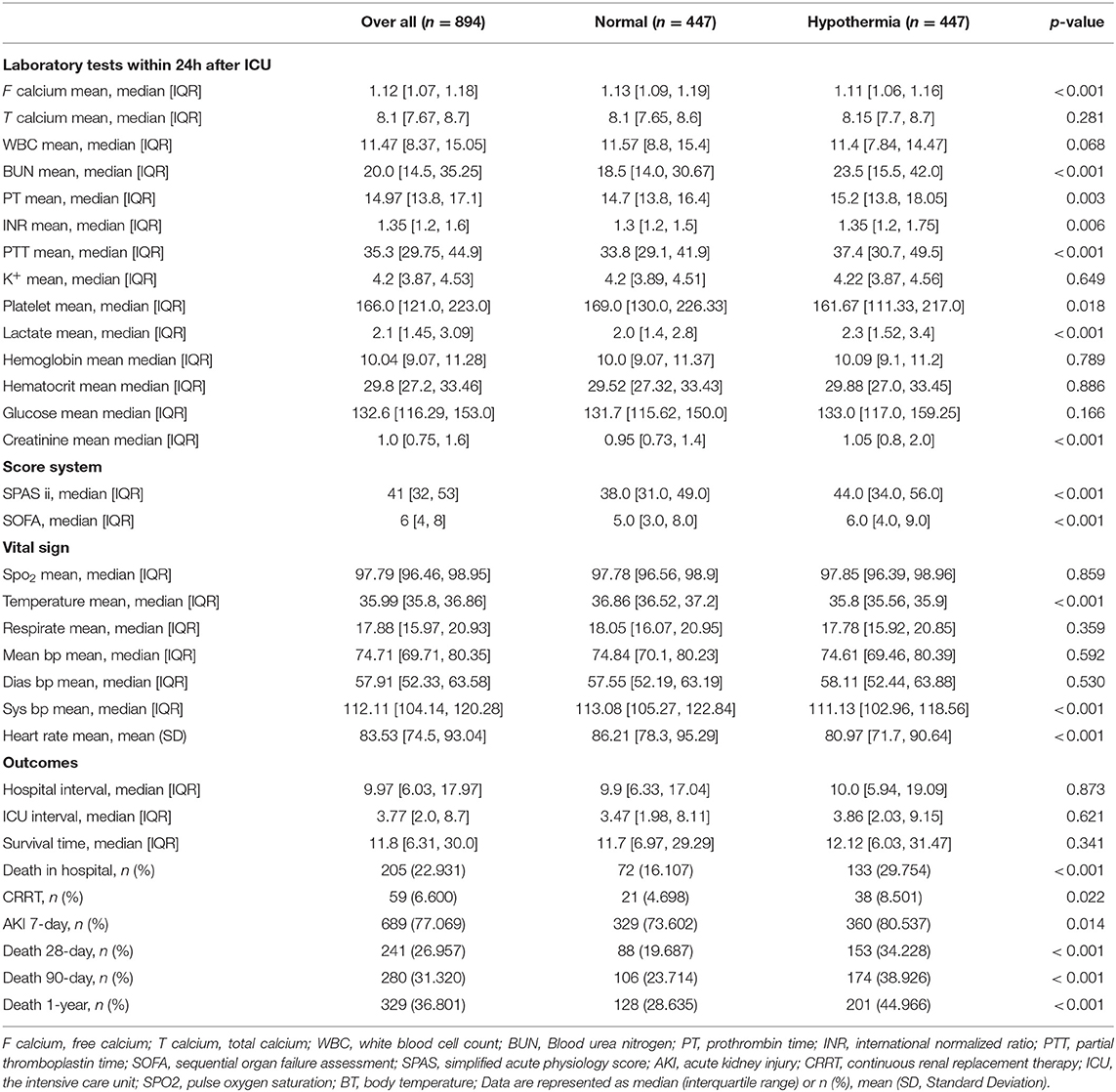
The comparison between hypothermia and normal group was performed before (Supplemental Table 1) and after (Supplemental Table 2, Table 2) PSM. There were no significant differences in hospital interval, ICU interval and survival time (Table 2) across univariate analysis. After adjusting potential confounding factors, the results of multivariate cox analysis and multivariate logistic regression analysis were that in-hospital mortality (HR 1.665, 95% CI 1.218–2.276; p = 0.001) and 1-year mortality (HR 1.537, 95% CI 1.205–1.961; p = 0.001) significantly increased in hypothermia group. There were higher 28-day mortality (HR 1.518, 95% CI 1.14–2.021; p = 0.004) and 90-day mortality (HR 1.491, 95% CI 1.144–1.943; p = 0.003) compared to normal group. The incidence of AKI within 7-day and intervention of CRRT within the first day after ICU admission were both showed no significant differences between 2 groups (Table 3).
Hyperthermia
The comparison between hyperthermia and normal group was conducted before (Supplemental Table 3) and after (Supplemental Table 4, Table 4) PSM. The length of hospital stay and ICU stay were longer in hyperthermia group than normal group, respectively (p < 0.001,Table 4) across univariate analysis. After adjustment for potential confounding factors, there were no statistical differences in in-hospital mortality, 28-day mortality, 90-day mortality, 1-year mortality, the incidence of AKI within 7-day or the intervention of CRRT within the first day after ICU admission between hyperthermia group and normal group across multivariate analysis (Table 5).
Discussion
This study demonstrated hypothermia within first 24-h after ICU admission was significantly associated with the increased short-term mortality and long-term mortality of post-cardiac surgery patients. Otherwise, no statistical associations were observed between hyperthermia and mortality. Hyperthermia was related to the prolonged length of hospital stay and ICU stay. Incidence of acute renal injury and intervention of continuous renal replacement therapy were not associated with hypothermia or hyperthermia.
Previous study considered body temperature could be used to assess prognostic risk independently. Hypothermia increased one-year mortality and seemed more harmful than hyperthermia (20). This is in line with our results. The reason may be relative to the great physiological changes produced by hypothermia (such as left shift of oxygenation curve, decline of coagulation function and arrhythmia and so on), which may lead to aggravate tissue hypoxia, aggravation of multiple organ functions (21), and failure of fluid resuscitation (22). For patients who were diagnosed sepsis within 24h, hypothermia (<36.0°C) could increase 28-day mortality and 1-year mortality (23). Besides, hypothermia was also associated with the mortality of none-elderly sepsis patients (11). Moreover, patients whose bladder core temperature were <36°C after ICU admission associated with worse outcomes after coronary artery bypass grafting (CABG) under CPB (5). The results of these researches are consistent with ours. Contrary to our study, Jiwook Kim's study suggested hypothermia or hyperthermia were not interrelated with long-term mortality of severe surgery patients except cardiovascular surgery patients (24). This can be explained by the inconsistence at the key time of temperature. Owing to enlarge sample size in our study, association between the distribution of body temperature and long-term mortality was significant. Relative research confirmed that changes in body temperature could easily induce acute and further cardiovascular outcomes (25). Thus, temperature monitoring of critically ill patients is extremely necessary. Emphasizing the importance of temperature monitoring within first 24-h after ICU admission is a new sight to improve the clinical outcomes of post-cardiac surgery patients.
The effects of hyperthermia and hypothermia on human body were complicated (26, 27). Hyperthermia was likely a powerful factor in strengthening immunity to remove subsequent pathogen by itself (28). Infection (29) and systemic inflammatory response syndrome (SIRS) caused by CPB (30) both lead to hyperthermia after cardiac surgery (31). Recent study claimed that hyperthermia in first 24h can be used to diagnose inflammatory response and possible outcomes after CPB, in this study in-hospital mortality was not significantly different comparing SIRS with no SIRS patients, while length of ICU stay was longer in SIRS patients (30). Besides, earlier studies suggested hyperthermia was beneficial for some outcomes (23, 32) and did not improve 1-year mortality of post-cardiac surgery patients (24). In line with our research, relationship between hyperthermia and mortality was not statistically significant, but hyperthermia was related to the prolonged length of ICU and hospital stay.
The strength of our study is focusing on the impact of overall body temperature changes within 24h after cardiac surgery on clinical outcomes rather than emphasizing the adverse results associated with a single time point. This study may be of beneficial in alleviating the adverse outcomes of hypothermia in post-cardiac surgery patients. Our study also has some limitations. Firstly, number of hyperthermia samples is relatively small, enlarging sample size and multicenter database are necessary for verification in future. Secondly, method and site of body temperature measurement were not clarified in MIMIC-III database which could cause bias to results, more researches deserve to carry out to clarify details. Thirdly, this is a retrospective single center study, results should be explained with caution in other populations and regions.
Conclusion
This retrospective observational study confirmed hypothermia within 24-h after ICU admission was associated with the elevated mortality of post-cardiac surgery patients while hyperthermia was not. The importance of temperature monitoring is worthy of attention to improve clinical outcomes after cardiac surgery in clinical treatment.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
FX, CL, and SB gathered and processed the data. CL and CZ prepared the results. FX and SB contributed in writing the manuscript. JG put forward the idea and revised the manuscript. All authors have read and approved the final manuscript.
Funding
Current project is supported by the Sichuan Science and Technology Program, China (Grant no. 2019YFS0352), Post-Doctor Research Project, West China Hospital, Sichuan University (20HXBH171).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.746228/full#supplementary-material
References
1. Kongsayreepong S, Chaibundit C, Chadpaibool J, Komoltri C, Suraseranivongse S, Suwannanonda P, et al. Predictor of core hypothermia and the surgical intensive care unit. Anesth Analg. (2003) 96:826–33. doi: 10.1213/01.ANE.0000048822.27698.28
2. Karalapillai D, Story DA, Calzavacca P, Licari E, Liu YL, Hart GK. Inadvertent hypothermia and mortality in postoperative intensive care patients: retrospective audit of 5050 patients. Anesthesia. (2009) 64:968–72. doi: 10.1111/j.1365-2044.2009.05989.x
3. Grocott HP, Mackensen GB, Grigore AM, Mathew J, Reves JG, Phillips-Bute B, et al. Postoperative hyperthermia is associated with cognitive dysfunction after coronary artery bypass graft surgery. Stroke. (2002) 33:537–41. doi: 10.1161/hs0202.102600
4. Vermeulen H, Storm-Versloot MN, Goossens A, Speelman P, Legemate DA. Diagnostic accuracy of routine postoperative body temperature measurements. Clin Infect Dis. (2005) 40:1404–10. doi: 10.1086/429621
5. Insler SR, O'Connor MS, Leventhal MJ, Nelson DR, Starr NJ. Association between postoperative hypothermia and adverse outcome after coronary artery bypass surgery. Ann Thorac Surg. (2000) 70:175–81. doi: 10.1016/S0003-4975(00)01415-6
6. Nathan HJ, Wells GA, Munson JL, Wozny D. Neuroprotective effect of mild hypothermia in patients undergoing coronary artery surgery with cardiopulmonary bypass: a randomized trial. Circulation. (2001) 104:I85–91. doi: 10.1161/hc37t1.094710
7. Gercekoglu H, Tarim O, Agar I, Korukcu A, Karabulut H, Soydemir H, et al. Effects of hypothermia on blood endogenous endotoxin levels during cardiopulmonary bypass. J Card Surg. (1997) 12:223–7. doi: 10.1111/j.1540-8191.1997.tb00129.x
8. Shen Y, Lou Y, Zhu S. Hyperthermia is a predictor of high mortality in patients with sepsis. Crit Care. (2020) 24:543. doi: 10.1186/s13054-020-03263-0
9. Goldberger AL, Amaral LA, Glass L, Hausdorff JM, Ivanov PC, Mark RG, et al. PhysioBank, PhysioToolkit, and PhysioNet: components of a new research resource for complex physiologic signals. Circulation. (2000) 101:E215–20. doi: 10.1161/01.CIR.101.23.e215
10. Johnson AE, Pollard TJ, Shen L, Lehman LW, Feng M, Ghassemi M, et al. MIMIC-III, a freely accessible critical care database. Sci Data. (2016) 3:160035. doi: 10.1038/sdata.2016.35
11. Shimazui T, Nakada TA, Walley KR, Oshima T, Abe T, Ogura H, et al. Significance of body temperature in elderly patients with sepsis. Crit Care. (2020) 24:387. doi: 10.1186/s13054-020-02976-6
12. Levin A, Stevens PE, Bilous RW, Coresh J, Winearls CG. Kidney disease: Improving global outcomes (KDIGO) CKD work group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. (2013) Supplements 3:1–150. doi: 10.1038/kisup.2012.73
13. McCaffrey DF, Griffin BA, Almirall D, Slaughter ME, Ramchand R, Burgette LF. A tutorial on propensity score estimation for multiple treatments using generalized boosted models. Stat Med. (2013) 32:3388–414. doi: 10.1002/sim.5753
14. Yoshida K, Bohn J and Yoshida MK. Package ‘tableone'. Vienna: R Foundation for Statistical Computing (2019).
15. Ginestet C. ggplot2. Elegant graphics for data analysis. J R Stat Soc. (2011) 174:245–6. doi: 10.1111/j.1467-985X.2010.00676_9.x
18. Grolemund G, Wickham H. Dates and times made easy with lubridate. J StatSoftw. (2011) 40:1–25. doi: 10.18637/jss.v040.i03
19. Wickham H, Averick M, Bryan J, Chang W, Yutani H. Welcome to the tidyverse. J Open Source Softw. (2019) 4:1686. doi: 10.21105/joss.01686
20. Erkens R, Wernly B, Masyuk M, Muessig JM, Franz M, Schulze PC, et al. Admission body temperature in critically ill patients as an independent risk predictor for overall outcome. Med Princ Pract. (2020) 29:389–95. doi: 10.1159/000505126
21. Martini WZ. The effects of hypothermia on fibrinogen metabolism and coagulation function in swine. Metabolism. (2007) 56:214–21. doi: 10.1016/j.metabol.2006.09.015
22. Leisman DE, Doerfler ME, Schneider SM, Masick KD, D'Amore JA, D'Angelo JK. Predictors, prevalence, and outcomes of early crystalloid responsiveness among initially hypotensive patients with sepsis and septic shock. Crit Care Med. (2018) 46:189–98. doi: 10.1097/CCM.0000000000002834
23. Drewry AM, Fuller BM, Skrupky LP, Hotchkiss RS. The presence of hypothermia within 24 hours of sepsis diagnosis predicts persistent lymphopenia. Crit Care Med. (2015) 43:1165–9. doi: 10.1097/CCM.0000000000000940
24. Kim J, Oh TK, Lee J, Kim S, Song IA. Association of immediate postoperative temperature in the surgical intensive care unit with 1-year mortality: retrospective analysis using digital axillary thermometers. Acute Crit Care. (2019) 34:53–9. doi: 10.4266/acc.2019.00255
25. Kawashima C, Matsuzawa Y, Akiyama E, Konishi M, Suzuki H, Hashiba K, et al. Prolonged fever after st-segment elevation myocardial infarction and long-term cardiac outcomes. J Am Heart Assoc. (2017) 6:e005463. doi: 10.1161/JAHA.116.005463
26. Launey Y, Nesseler N, Malledant Y, Seguin P. Clinical review: fever in septic ICU patients–friend or foe? Crit Care. (2011) 15:222. doi: 10.1186/cc10097
27. Annane D. Body temperature in sepsis: a hot topic. Lancet Respir Med. (2018) 6:162–3. doi: 10.1016/S2213-2600(18)30003-1
28. Evans SS, Repasky EA, Fisher DT. Fever and the thermal regulation of immunity: the immune system feels the heat. Nat Rev Immunol. (2015) 15:335–49. doi: 10.1038/nri3843
29. Sessler DI. Temperature monitoring and perioperative thermoregulation. Anesthesiology. (2008) 109:318–38. doi: 10.1097/ALN.0b013e31817f6d76
30. Squiccimarro E, Labriola C, Malvindi PG, Margari V, Guida P, Visicchio G, et al. Prevalence and clinical impact of systemic inflammatory reaction after cardiac surgery. J Cardiothorac Vasc Anesth. (2019) 33:1682–90. doi: 10.1053/j.jvca.2019.01.043
31. Zakkar M, Guida G, Suleiman MS, Angelini GD. Cardiopulmonary bypass and oxidative stress. Oxid Med Cell Longev. (2015) 2015:189863. doi: 10.1155/2015/189863
Keywords: hypothermia, hyperthermia, clinical outcome, post-cardiac surgery, intensive care unit
Citation: Xu F, Zhang C, Liu C, Bi S and Gu J (2021) Relationship Between First 24-h Mean Body Temperature and Clinical Outcomes of Post-cardiac Surgery Patients. Front. Cardiovasc. Med. 8:746228. doi: 10.3389/fcvm.2021.746228
Received: 23 July 2021; Accepted: 26 August 2021;
Published: 23 September 2021.
Edited by:
Hendrik Tevaearai Stahel, Bern University Hospital, SwitzerlandReviewed by:
Maruti Haranal, National Heart Institute, MalaysiaHe Wei, Capital Medical University, China
Copyright © 2021 Xu, Zhang, Liu, Bi and Gu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jun Gu, gujun@wchscu.cn
 Fei Xu
Fei Xu Cheng Zhang
Cheng Zhang Chao Liu
Chao Liu Siwei Bi2
Siwei Bi2  Jun Gu
Jun Gu