Research Article
How does a Personalized Rehabilitative Model influence the Functional Response of Different Ankle Foot Orthoses in a Cohort of Patients Affected by Neurological Gait Pattern?

Maurizio Falso1*, Eleonora Cattaneo1, Elisa Foglia1, Marco Zucchini2 and Franco Zucchini2
1Section of Neurological Rehabilitation, Clinical Institute Città di Brescia, Brescia, Italy
2Il Podologo S.r.l., Brescia, Italy
*Address for Correspondence: Maurizio Falso (MD), Physical Medicine and Rehabilitation, Section of Neurological Rehabilitation-Clinical Institute, Città di Brescia-Via Gualla 15, 25128, Brescia, Italy,Tel: 349.4971729, Email: falsomaurizio@libero.it
Dates: Submitted: 22 June 2017; Approved: 28 August 2017; Published: 30 August 2017
How to cite this article: Falso M, Cattaneo E, Foglia E, Zucchini M, Zucchini F. How does a Personalized Rehabilitative Model influence the Functional Response of Different Ankle Foot Orthoses in a Cohort of Patients Affected by Neurological Gait Pattern?. J Nov Physiother Rehabil. 2017; 1: 072-092.
DOI: 10.29328/journal.jnpr.1001010
Copyright License: © 2017 Falso M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Ankle foot orthoses; Neurological gait pattern; Kinematic gait analysis; Proprioceptive rehabilitation
Abbreviations: AFO: Ankle Foot Orthoses, SAFOs: Solid AFOs, FRAFO: Floor Reaction AFO, HAFO: Hinged AFO, PLS-AFO: Posterior Leaf Spring AFO, DAFONS: Dynamic Hinged Ankle Foot Orthoses with Neuroswing, EMG: Electromyography, SEMG: Surface EMG, CNS: Central Nervous System, PNS: Peripheral Nervous System, VGA: Visual Gait analysis, MAS: Modified Ashworth Scale, MRC: Medical Research Council, BBS: Berg Balance Scale, P: Patient, BTS: BTS Bioengineering Company
Abstract
Background: Orthoses need to support physiotherapy as well as surgical treatment. Related to patient’s rehabilitative goals and pathological gait pattern, orthotists have to produce an orthoses that using an adjustable ankle joint system with preloaded disc springs can store the energy brought in by the body weight and produce a tuning effect on patient’s gait and sense of balance. The purpose of this study was to establish how a personalized proprioceptive individualized rehabilitative treatment could influence the functional response of different AFOs (Ankle Foot Orthoses) in a cohort of patients affected by neurological gait pattern.
Methods: Five patients affected by different neurological gait pattern and volunteered to participate to this study were recruited. The comparative spatio-temporal and functional effect on gait pattern of 3 types of AFOs was investigated under 4 study conditions: 1) without AFO or free-walk (FW); 2) wearing a Codivilla spring, 3) wearing a carbon unjointed AFO (“Toe-Off”); 4) wearing an innovative carbon-kevlar dynamic joint DAFO (DAFONS=Dynamic Ankle Foot Orthoses with Neuroswing). In line with our rehabilitative model, patients underwent to a weekly treatment session, 80 minutes duration per session, for 4 weeks. Evaluation was made before (time T3=time of recruitment) and after our individualized rehabilitative treatment course (time T4=1 month from T3) by using: a. G-Walk sensor (by BTS) spatio-temporal measures in different gait performances; b. clinical/functional outcome measures (Modified Ashworth Scale or MAS for the affected upper and lower limb; Medical Research Council or MRC; orthostatic stability evaluation by using the Berg Balance Scale or BBS).
Findings: A comparative analysis of clinical and instrumental data, performed in the pre-defined four investigational conditions, showed:
√ a statistical insignificant change of MRC and MAS scales at time T4, with a significance trend outcome observed at the same time by using the Wilcoxon Signed Rank Test
√ a statistical significant difference between test duration (sec) by using Toe-Off vs DAFONS and by using Codivilla spring vs Toe-Off
√ a statistical significant increase of the stride length on the left side (% cycle length) by using DAFONS compared to Toe-Off for patient P1, P3 and P5 with a parameter decrease by using DAFONS compared to Codivilla spring and Toe-Off use for patient P2
√ a statistical significant correlation between BBS trend and test duration (sec) by using Codivilla spring at time T3 and T4
√ a statistical significant correlation between the BBS trend and the double gait support duration on the right side (% cycle) with number of left step cycles by using DAFONS at time T3 and T4
√ in a comparative post-treatment visual gait analysis a modification of each patient’s static and dynamic postural assessment by using 3 different types of orthoses
Interpretation: In line with our study design we noted at the end of the proposed rehabilitative treatment an amelioration of gait quality with the use of DAFONS in all those patients (P1, P3 and P5) who showed a neurocognitive competence with a related functional grade of neurorehabilitative re-learning attitude of the physiological gait pattern and with a compromised perceptive control of gait and core stability. The proprioceptive profile of our rehabilitative program could promote the pro-adaptive and facilitation properties of a personalized gait control, induced by an innovative dynamic ankle foot orthoses with a modulable ankle joint system called Neuroswing. In the daily clinical practice, the personalized integration of a neurorehabilitative program and DAFONS can perform an individualized peripheral neuro-facilitation of gait cycle (peripheral perceptive facilitation), a neurorehabilitative re-learning process of physiological gait pattern (peripheral assisted neuroplasticity facilitation DAFONS induced) and an increase of patient’s motor abilities and quality of life in all daily performances.
Introduction
In a common “gait-lab”, ambulation can be kinematically quantified through spatio-temporal parameters as the stride length, gait cadence and gait velocity, defined by Fritz S et al. [1], as “the sixth sense of life morbility and mortality”. Clinicians used, in the last years, different technical devices for the computerized movement analysis in patients affected by neurological gait pattern: Elite, stabilometric platforms, surface electromyography (SEMG) and wireless devices as the BTS G-Walk sensor device [2]. In the daily rehabilitative practice, each of these devices can help physiotherapists to optimize their diagnostic approach and treatment options of all common neurological gait disorders. Similarly, clinicians and physioterapists made use of different types of ankle foot orthoses (AFO) in the short or long-term rehabilitative treatment of mechanical or neurological gait disturbance [3,4]. In the daily clinical and rehabilitative activity, a single ankle foot orthoses (or AFO) cannot satisfy all functional goals that can be assumed in a neuromodulated and assisted treatment of a pathological gait pattern [5]. We know that the ankle joint control plays a personal role during locomotion and is frequently altered after a brain or spinal damage [6]. The ‘‘traditional’’ankle-foot orthoses (AFO) are rigid and designed to immobilize the ankle joint at a defined angle. Different studies demonstrated that immobilization of the ankle joint reduces pain [7,8], stimulate proprioception [8] and enhance gait for many patients with severe locomotive disorders [9-11]. The current modern design of AFOs includes articulated devices capable of assisting plantarflexion during stance. Whereas some studies confirmed the benefits of assistive AFOs [12,13], other studies demonstrated a minimal effect of traditional AFOs on global gait kinematics in hemiplegic patients [14]. For this reason, taken into consideration the economic cost and the bulkiness of some articulated AFOs, often the clinical attitude is to use standard rigid model in the daily rehabilitation practices.
One of the aims of orthotic management is to produce a normal gait pattern by positioning joints in the proper position to reduce pathological reflex or spasticity. Using the right modern materials (carbon, kevlar and other synthetics of hardness grades) and material properties in the right place of an individualized and dynamic custom-made orthoses, many physiotherapists can be supported today by a gait device with an ergonomic and individualized orthotic design, more in line with patient’s functional and individual rehabilitative needs [15,16]. The critical role of a personalized rehabilitative course is to aim at a perfect balance between “induction to a pro-adaptive facilitation and inhibition to a maladaptive facilitation of pathological gait pattern”. In the daily clinical and physiotherapic practice, the introduction of an ankle foot orthoses always induce this effect that we cannot ignore. In a recent study, Falso et al. [16], proposed and demonstrated the pro-adaptive functional effect of a singular dynamic ankle foot orthosis (DAFONS) that, designed with an ankle joint system with preloaded disc springs, can store the energy brought in by the body weight during gait and produce and individualized tuning effect on patient’s gait and sense of balance. The authors highlighted the functional uniqueness of DAFONS by demonstrating how personalization of esoscheletal design, plurimodulation of the ankle biomechanical properties, task and function specific regulation of the dynamic lever spring force with an optimization and storage of the energy brought in by the body weight which support in this way ankle’s push-off when released and control the step length on the affected and unaffected limb, can really help physiotherapists in their practice as a neurorehabilitative re-learning device of physiological gait pattern (peripheral assisted neuroplasticity facilitation).
The purpose of this interventional study was to establish how a personalized proprioceptive rehabilitative treatment could influence the functional response of different AFOs in a cohort of patients affected by neurological gait pattern.
Methods
Subjects
In line with an informed consent and simple inclusion criteria (cooperating patient, evidence of pathological gait pattern, bearer of a DAFONS) and exclusion criteria (not cooperating patient, evidence of a physiological gait pattern, not bearer of a DAFONS), five patients (3 males and 2 females; mean age 33+/-18yy) affected by different neurological gait pattern were recruited for the aim of this study. At baseline (time T0), a clinical and functional evaluation of all patients was made by MF in the Spasticity and Movement Disorders Ambulatory of the Clinical Institute of Città di Brescia. In a restricted way, we recruited only patients affected by neurological gait disorders (Table 1) who were candidate to use our innovative dynamic hinged Ankle-Foot-Orthoses designed with an innovative ankle joint system called Neuroswing (DAFONS), provided by the Prosthetic and Orthothic Lab - Il Podologo S.r.l (Brescia).
| Table 1: Overview of the study population SNC damages, related movement disorders and ankle/foot attitudes. | |
| Patient | SNC damage, related movement disorder and ankle/foot attitude |
| P1 | . Compressive foot trauma with a secondary local neuroalgodystrophy that caused a right foot supination during gait and a related spontaneous distal limb clonus . Unilateral hypotonic drop-foot |
| P2 | . Multiple sclerosis with a right supination gait pattern and a double swing attitude during walking . Unilateral spastic foot supination |
| P3 | . Lumber ischemic spine lesion, with a right knee hyperextension and a flat foot pattern during the stance phase of gait . Spinal stiff gait with a distal foot supination |
| P4 | . Left hemisperic brain stroke with a related right hemiplegia, characterized by a distal flexed wrist and flexed elbow on the upper limb and a right knee hyperextension and a toe walking pattern during the stance phase of gait . Spastic right hemiparesis with a typical distal equinovarus ankle-foot attitude |
| P5 | . Cerebral plasy with a double hemiplegic gait pattern characterized by an asymmetric proximal limb adduction and a distal abnormal "scissors limb attitude" during the single and double lever support of gait . Valgus-pronated ankle attitude in stance bilaterally with a flat foot gait schema distally and a related knee recurvatum proximally during gait |
Instrumentation: For the aim of this study we used:
• BTS (BTS Bioengeenering Company)G-Walk sensor device
BTS G Walk sensor is an accurate and quick measurement device of spatio-temporal gait parameters. From a technical and functional point of view, the BTS G Walk sensor is a wireless system (Figure 1) consisting of an inertial sensor composed by a:
a. triaxial accelerometer
b. triaxial gyroscope
c. magnetometer
This device is able to communicate with the software of a computer using a Bluetooth connection with a range up to a distance of 20m. The device provide automatically normative data for an automatic comparison of acquired parameters with “normal” class allowing an immediate visual result showing the difference between the patient and average. The quick to execute tests that do not require any subject’s preparation, together with the automatic report generation make BTS G-WALK suitable for a wide range of applications: prevention, diagnosis and follow-up of rehabilitative or pharmacological intervention. During our trial (Figure 2) the device will be positioned on level L5 of patient’s spine and secured by an ergonomic belt allowing free body movement.
• AFOs
- SAFO (Solid Ankle Foot Orthoses)Codivilla spring (Figure 3)
• Univalve orthoses with a posterior leg shell
• Polipropylene plastic material
• High flexible orthoses with a low spring control in push-off phase of gait
• Prefabricated AFO
- FRAFO (Floor Reaction Ankle Foot Orthoses)
Toe-Off (Figure 4)
• Univalve orthoses with an anterior leg shell
• Preresinated carbon fiber AFO
• Low deformability and medium flexibility AFO; the effect produced during the gait cycle by this kind of orthoses will be the low capability of control of spring effect deriving by the energy brought in by the body weight during the push-off phase of gait
• Low ergonomic orthoses design that offers a very low ankle ROM and cannot be adapted to patient’s pathological foot attitude (equinovarus foot, pronated foot, flat foot, toe walking); this property can be explained by the low deformability and medium flexibility offered by the design and material of this kind of orthoses
- DAFONS (Dynamic Ankle Foot orthoses designed with Neuroswing)
• Bivalve orthoses (Figure 5) with a dorsal or ventral leg component and a foot component and an innovative ankle joint system called Neuroswing
• Not pre-resinated carbon fiber AFO with a 1/3 anterior plantar aramidic fiber component (KEVLAR) with an high elastic response
• Task and functional specific custom-made orthosis, with an high ergonomic profile, respect of patient’s ankle joint attitude and with a singular modulable and reciprocant lateral malleolar ankle joint system
• Dynamism, plasticity and stability as technical properties of the esoskeletal unit
• A device that allowes to optimize the lever control of gait during the so called heel contact phase, modulate, optimize and store the energy brought in by the body weight during gait and that can be considered as usefullness energy save system.
Neuroswing (Figure 6) represents an innovative ankle joint system, having a plurimodulate regulation property of ankle “attitude”, that integrated in the carbon scheleton of an AFO - DAFO or KAFO, can be used in the rehabilitative treatment of pathological gait schema secondary to central nervous system damage (CNS) like stroke, PC, several brain or spinal damage or secondary to peripheral nervous system damage (PNS) like peripheral nervous deafferentation, neuropathy, etc.
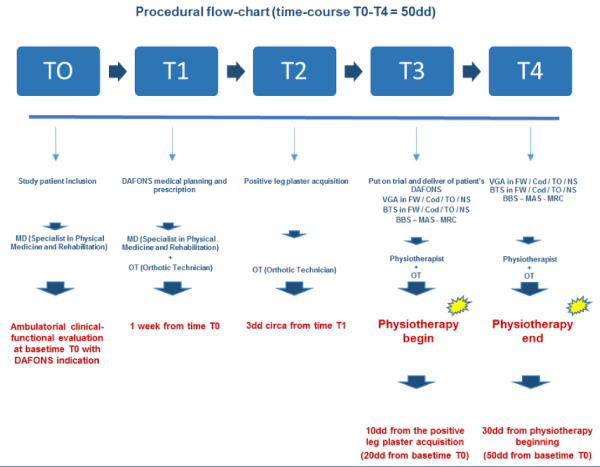
Evaluation procedure: Our personalized operating flow-chart (Figure 7), can be divided in two time-related phases: a. a clinical-orthotic phase in which each patient underwent a task-specific evaluation at time T0, T1, T2 and time T3; b. a rehabilitative phase in which patients recruited were evaluated by the Physioterapist at time T3 and began a rehabilitative treatment course with an outcome evaluation at time T4.
In particular:
- T0 (baseline), patients underwent a clinical and functional evaluation (made by the Specialist Doctor in Physical Medicine and Rehabilitation);
- T1 (1 week from baseline T0), a DAFO manufacturing project for each patient was established with the observation of their pathological limb attitude and realizing an ergonomic and individualized custom-made AFO;
- T2 (3 days from T1), the orthotic technician begin the DAFONS manufacturing that goes on for one week; each patient was invited to wear the DAFONS and, if appropriate, to use it during walking;
- T3 (10 days from T2), the orthotic technician and the physiotherapist will define the appropriateness and functional profile of the AFOs by a) evaluating patients’ compliance and ergonomic sensation in the use of the manufactured AFO; b) analyzing patients’ individual spatio-temporal gait pattern during a free walk condition and wearing our 3 types of orthoses, by using the BTS G-Walk sensor device. After gait analysis, patients recruited underwent a clinical/functional evaluation (evaluation of muscle tone by using the Modified Ashworth Scale or MAS for the affected upper and lower limb; evaluation of muscle recruitment by using the Medical Research Council or MRC scale; evaluation of patient’s orthostatic stability by using the Berg Balance Scale or BBS) made by the Physioterapist and began a rehabilitative treatment course.
- T4 (30 days from T3), after 1 month from the rehabilitative treatment start, each patient underwent a:
a. instrumental (BTS G walk sensor device) spatio-temporal evaluation in each different study condition;
b. clinical/functional outcome evaluation (MAS for the affected upper and lower limb; MRC scale; orthostatic stability evaluation by using the Berg Balance Scale).
Outcome measures
• Clinical-functional outcome measures
- MAS (Modified Ashworth Scale) to evaluate grade of muscle tone of the affected upper and lower limb
- MRC (Medical Research Council) to evaluate muscle recruitment of lower limbs
- BBS (Berg Balance Scale) to evaluate patient’s orthostatic stability
• Visual Gait Analysis (VGA)
At time T3 and time T4, each patient underwent an off line visual gait analysis (VGA), made by the same MD, which consists in a simple observational gait evaluation with an attention on specific aspects of patient’s gait pattern; the term “off-line” indicates the indirect evaluation of gait pattern by using a video registration made before. We observed the gait performance in four study conditions: in free-walk (FW) (without orthoses), with Codivilla spring, with Toe-Off and with a custom-made DAFONS. At time T3 and time T4, each patient underwent an off line visual gait analysis (VGA), made by the same MD, which consists in a simple observational gait evaluation with an attention on specific aspects of patient’s gait pattern; the term “off-line” indicates the indirect evaluation of gait pattern by using a video registration made before. We observed the gait performance in four study conditions: in free-walk (FW) (without orthoses), with Codivilla spring, with Toe-Off and with a custom-made DAFONS.
• Spatio-temporal BTS parameters
At time T3 and time T4, we evaluated patients’ individual spatio-temporal gait pattern in each study condition by using the BTS G-Walk sensor device. The spatio-temporal parameters acquired were:
- Test duration (sec)
- Gait speed (m/sec)
- Gait cadence (steps/min)
- Number of step cycle on the left side
- Number of step cycle on the right side
- Stride length on the left and on the right (% cycle length)
- Stance phase duration on the left and on the right (% cycle)
- Swing phase duration on the left and on the right (% cycle)
- Double gait support duration on the left and on the right (% cycle)
In each study condition, we asked our patients to walk with a self-selected speed along a 10m walkway for three times; during the trial, patients were authorized to use an ambulation aid or to be supported by a caregiver.
Rehabilitative approach: In line with our rehabilitative model, patients underwent at time T3 to a weekly rehabilitative treatment session, 80 minutes duration per session, for 4 weeks. In table 2, we resume the checklist of all exercises proposed in our rehabilitative protocol to each patient recruited. To optimize and individualize our rehabilitative approach, the physiotherapist realized a checklist of exercises in line with patient’s functional impairment.
Rehabilitative approach: In line with our rehabilitative model, patients underwent at time T3 to a weekly rehabilitative treatment session, 80 minutes duration per session, for 4 weeks. In table 2, we resume the checklist of all exercises proposed in our rehabilitative protocol to each patient recruited. To optimize and individualize our rehabilitative approach, the physiotherapist realized a checklist of exercises in line with patient’s functional impairment.
| Table 2. Checklist of excercises proposed in the study rehabilitative protocol. | ||
| Patient……………… | Date……/………../…………. | |
| Goals | Treatment approach | |
| . Manual proprioceptive feet stimulation | Tactile, proprioceptive and postural stimulation | |
| Passive limb mobilization | ||
| Active limb mobilization | ||
| Stretching | ||
| Muscle activation redressing | ||
| Pathological postural and gait pattern inhibition | ||
| . Orthostatic control facilitation | Balance training without assisted devices | |
| Balance training with Bobath ball | ||
| Balance training with Freeman tables | ||
| Core stability stimulation | ||
| Static and dynamic trunck and hip control facilitation | ||
| Lower limb muscle stretching | ||
| . Pathological gait pattern reset | Gait training with and without assisted devices | |
| Gait training with an optimization of the: | ||
| stride length on the left and right side | ||
| stance and swing control | ||
| single and double gait support control on the left and right side | ||
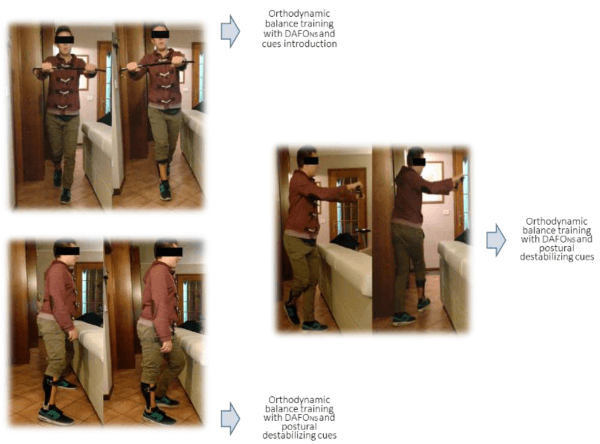
| . Orthodynamic control facillitation | Orthodynamic balance training with and without cues | |
| Gait training with and without assisted devices | ||
| Linear gait training with and without obstacles | ||
| Lateral gait training with and without obstacles | ||
| Gait training with parallel bars | ||
| Gait training on unstable ground | ||
| Gait training with direction differentiation | ||
| Notes……………………………………………………………………… | ||
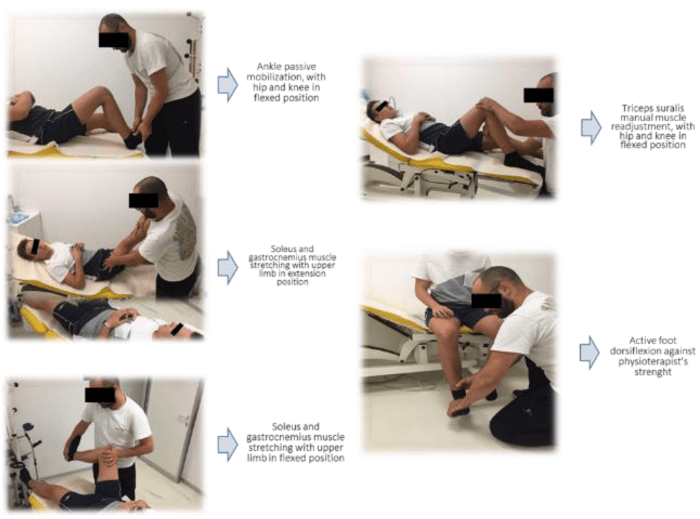
a. manual proprioceptive feet stimulation (Figure 8)
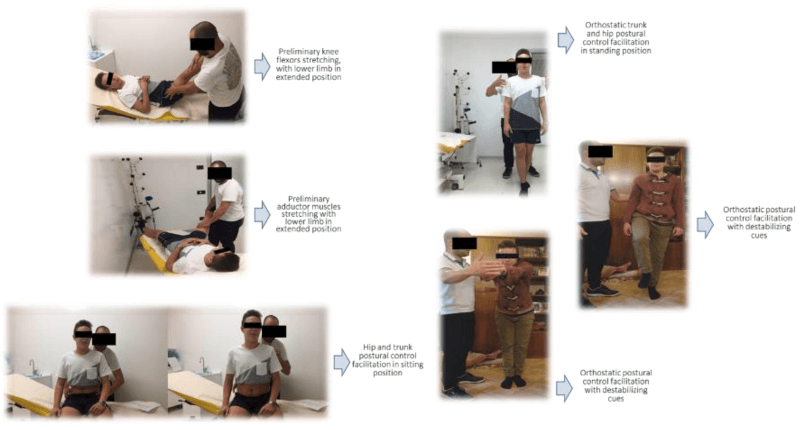
b. orthostatic control facilitation (Figure 9)
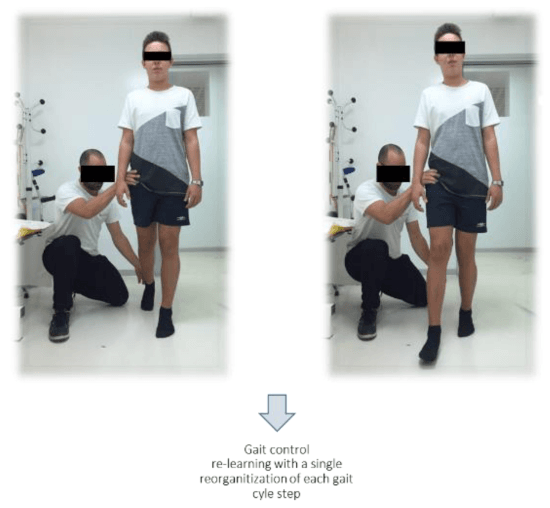
c. pathological gait pattern reset (Figure 10)
d. orthodynamic control facilitation (Figure 11)
Data processing and statistics: Spatio-temporal gait analysis was made using the statistical software SPSS (version 22). Friedman non-parametric tests with Wilcoxon post-hoc test were used to realize at time T3 and T4 a comparative analysis between our spatio-temporal and clinical variables. The significance level was set to p<0.05.
Results
Visual gait analysis
A comparative visual gait analysis (VGA) was performed in each study condition (free-walk or without orthosis, with Codivilla spring, with Toe-Off orthosis and with DAFONS) at time T3 and time T4 (at the end of the rehabilitative treatment) with an analytical acquisition of patient’s performance reported respectively in tables 3 and 4.
| Table 3. Analytical visual gait analysis report in each study condition for each patient at time T3. | |||||
| Orthostatic and orthodynamic trunk attitude | Core stability and hip ROM in stance and swing phase | Knee attitude in stance and swing phase | Global movement attitude of the trunk-hip-lower limb unit | Ankle movement profile in stance and swing phase | |
| P1 (rl)* |
Asymmetric (FW)
C = ameliorated |
Present with an abnormal up and down and lateral hip tilt in stance and swing phase (FW)
C = ameliorated with decrease of the abnormal hip ROM TO = worsened NS = normalized |
Physiological eccentric right knee control in stance and natural ROM in swing ipsilaterally (FW) C = ameliorated TO = worsened NS = normalized |
Asymmetric (FW)
C = ameliorated |
Persistent varus-supination right ankle attitude during whole gait cycle with an abnormal and incomplete heel and stance phase control; physiological left ankle control (overpowered) in stance and swing (FW)
C = fairly good modified |
| P2 (rl)* |
Asymmetric (FW)
C = unmodified |
Present with an abnormal “up and down and lateral” hip tilt in stance and swing phase secondary to a lower limb dysmetry and a related orthostatic deep disperception (FW)
C = ameliorated with a decrease of the abnormal hip ROM |
Physiological eccentric right knee control in stance and natural ROM in swing ipsilaterally (FW)
C = ameliorated |
Asymmetric (FW)
C = unmodified |
Physiological bilateral ankle attitude in single and double support with an intercurrent steppage schema on the right lower limb in swing phase (FW)
C = ameliorated with a decrease of the right steppage |
| P3 (rl)* |
Symmetric (FW)
C = fairly good normalized |
Physiological left hip control in stance and swing phase; abnormal increase of the right hip “up and down” tilt in stance and push-off; core stability present in double contact (FW)
C = fairly good normalized |
Physiological eccentric right knee control in stance and natural ROM in swing ipsilaterally; intercurrent right knee recurvatum in stance (residual right quadriceps weakness ?!) (FW)
C = fairly good ameliorated |
Symmetric (FW)
C = fairly good normalized |
A fairly good hindfoot valgus attitude on the right foot in initial contact and midstance with a residual physiological gait excursion in stance and swing phase; prolonged swing phase duration on the right side (FW)
C = fairly good modified |
| P4 (rl)* |
Asymmetric (FW)
C = unmodified |
Abnormal proximal right hip vaulting to compensate the search of a distal ankle clearence in swing; proximal right hip retroversion secondary to a proximal muscle weakness and distal knee recurvatum; physiological left hip control in stance and swing phase; core instability during a long way gait performance (FW)
C = unmodified |
Right knee recurvatum in stance with a physiological left knee control in double stance (FW)
C = worsened |
Asymmetric (FW)
C = unmodified |
Constant valgus-pronated right ankle attitude in stance with a flat foot gait schema distally and a related knee recurvatum proximally during gait (FW)
C = ameliorated |
| P5 (dh)* |
Asymmetric (FW)
C = unmodified |
Abnormal hip antiversion in stance with an evident core instability and an high care-giving need during gait; a fairly good hip control in swing phase with a related abnormal up and down and lateral tilt of it, facilitated by a related knee hyperextension in stance (FW)
C = worsened |
With an high care-giving need, abnormal eccentric bilateral knee control in stance secondary to the proximal hip antiversion, the quadriceps weakness and the constant hyperextension lower limb attitude; fairly good the dynamic knee attitude in swing phase bilaterally (FW)
C = worsened |
Asymmetric with a constant proximal limb adduction and a distal abnormal “scissors limb attitude” during the single and double lever support of gait (FW)
C = worsened |
Constant valgus-pronated ankle attitude in stance bilaterally with a flat foot gait schema distally and a related knee recurvatum proximally during gait (FW)
C = worsened |
*rl = right lateralized; dh = double hemiplegia |
|||||
| Table 4. Analytical visual gait analysis report in each study condition for each patient at time T4. | |||||
| Orthostatic and orthodynamic trunk attitude | Core stability and hip ROM in stance and swing phase | Knee attitude in stance and swing phase | Global movement attitude of the trunk-hip-lower limb unit | Ankle movement profile in stance and swing phase | |
| P1 (rl)* | Asymmetric (FW)
C = ameliorated TO = worsened NS = normalized |
Present with an abnormal up and down and lateral hip tilt in stance and swing phase (FW)
C = ameliorated with decrease of the abnormal hip ROM TO = worsened NS = normalized |
Physiological eccentric right knee control in stance and natural ROM in swing ipsilaterally (FW)
C = ameliorated TO = worsened NS = normalized |
Asymmetric (FW)
C = ameliorated TO = worsened NS = normalized |
A fairly amelioration of varus-supination of the right ankle attitude during whole gait cycle with a better heel and stance phase control; physiological left ankle control (overpowered) in stance and swing (FW)
C = fairly good modified TO = worsened NS = normalized |
| P2 (rl)* | Asymmetric (FW)
C = unmodified TO = unmodified NS = normalized |
Present with an amelioration “up and down and lateral” hip tilt in stance and swing phase related to an orthostatic deep disperception decrease (FW)
C = ameliorated with a decrease of the abnormal hip ROM TO = worsened NS = amelioration of the perceptive gait control |
Physiological eccentric right knee control in stance and natural ROM in swing ipsilaterally (FW)
C = unmodified TO = worsened NS = normalized |
Asymmetric (FW)
C = unmodified TO = unmodified NS = normalized |
Physiological bilateral ankle attitude in single and double support with an intercurrent steppage schema on the right lower limb in swing phase (FW)
C = unmodified TO = unmodified NS = normalized |
| P3 (rl)* | Symmetric (FW)
C = fairly good normalized TO = fairly good normalized NS = normalized |
Physiological left hip control in stance and swing phase; amelioration of the right hip “up and down” tilt in stance and push-off; core stability present in double contact (FW)
C = unmodified TO = unmodified NS = normalized |
Physiological eccentric right knee control in stance and natural ROM in swing ipsilaterally; intercurrent right knee recurvatum in stance (residual right quadriceps weakness ?!) (FW)
C = fairly good ameliorated TO = fairly good modified NS = normalized |
Symmetric (FW)
C = fairly good normalized TO = fairly good normalized NS = normalized |
A fairly good hindfoot valgus attitude on the right foot in initial contact and midstance with a residual physiological gait excursion in stance and swing phase; prolonged swing phase duration on the right side (FW)
C = fairly good modified TO = worsened NS = normalized |
| P4 (rl)* | Asymmetric (FW)
C = unmodified TO = unmodified NS = unmodified |
Abnormal proximal right hip vaulting to compensate the search of a distal ankle clearence in swing; proximal right hip retroversion secondary to a proximal muscle weakness and distal knee recurvatum; physiological left hip control in stance and swing phase; core instability during a long way gait performance (FW)
C = unmodified TO = unmodified NS = fairly good normalized |
Right knee recurvatum in stance with a physiological left knee control in double stance (FW)
C = worsened TO = worsened NS = fairly good modified |
Asymmetric (FW)
C = unmodified TO = unmodified NS = fairly good modified |
Constant valgus-pronated right ankle attitude in stance with a flat foot gait schema distally and a related knee recurvatum proximally during gait (FW)
C = ameliorated TO = unmodified NS = normalized |
| P5 (dh)* | Alignment ameliration (FW)
C = unmodified TO = worsened NS = normalization of the trunk control in feedforward with no care giving need |
Decreased hip antiversion in stance with an amelioration of core stability and decrease of care-giving need during gait; a better hip control in swing phase with a related amelioration of up and down and lateral tilt of it, facilitated by a better knee control in stance (FW)
C = worsened TO = worsened NS = increased with a global normalization increase of the postural orthostatic and orthodynamic hip and trunk control |
Decrease care-giving need, constant abnormal eccentric bilateral knee control in stance secondary to the proximal hip antiversion, the quadriceps weakness and the constant hyperextension lower limb attitude; amelioration of the dynamic knee attitude in swing phase bilaterally (FW)
C = worsened TO = worsened NS = normalized the knee hyperextension secondary to the orthotic tibialis pivot remodulation of the orthostatic and orthodynamic limb alignment |
Asymmetric with a constant proximal limb adduction and a distal abnormal “scissors limb attitude” during the single and double lever support of gait (FW)
C = worsened TO = worsened NS = normalized, no care giving need, recover of a correct orthostatic and ortodynamic trunk-hip and lower limb alignment in stance and swing phase |
Amelioration of ankle attitude in stance bilaterally with a persistent flat foot gait schema distally and a minimally decrease of knee recurvatum proximally during gait (FW)
C = worsened TO = worsened NS = normalized with a physiological recover of the stance feet control during gait performance (1°-2°-3° rocker) and ankle alignment in the heel contact phase |
| *rl = right lateralized; dh = double hemiplegia FW = free-walk condition; C = Codivilla spring condition; TO = Toe-Off orthesis condition; NS = DAFO with Neuroswing joint condition. |
|||||
Spatio-temporal BTS G-Walk sensor gait analysis
• Objective spatio-temporal data
A spatio-temporal gait analysis, using the BTS G-Walk sensor device, was performed in each study condition (free-walk or without orthosis, with Codivilla spring, with Toe-Off orthosis and with DAFONS) at time T3 and time T4, with an analytical acquisition of patient’s raw data. An objective intrapersonam spatio-temporal raw data comparison, performed in our 4 study conditions, showed a different trend in each patient recruited from time T3 to time T4.
In particular:
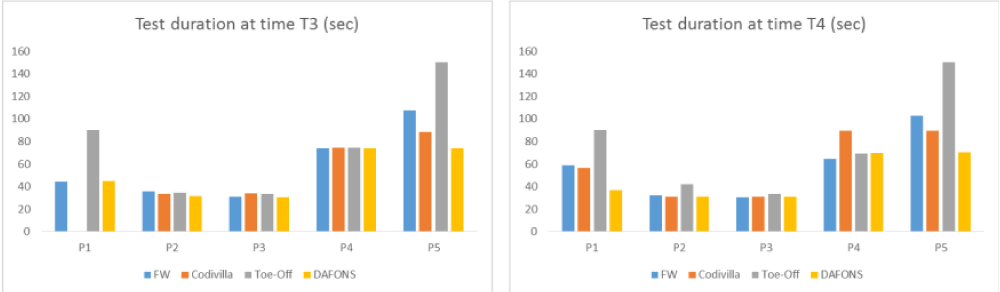
Test duration (sec) (Figure 12)
√ all patients showed a decrease of test duration by using DAFONS at time T3 that remained unchanged at time T4
√ at time T3 patient P1 and P5 (> in P5) showed an increase of test duration compared to patients P2, P3 and P4 by using Toe-Off orthosis that we cannot observe by using Codivilla spring and DAFONS; this trend remained unchanged at time T4.
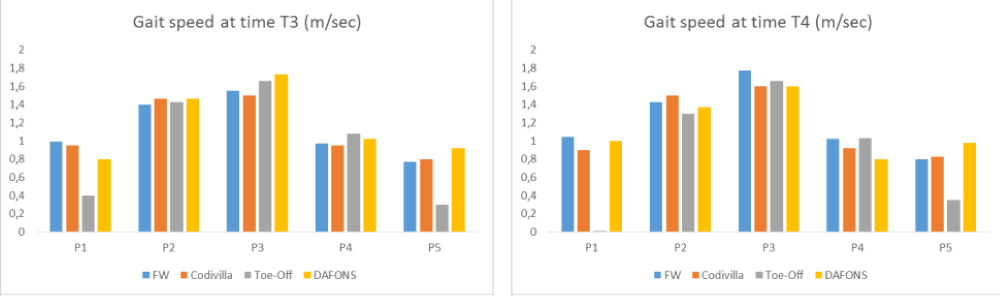
Gait speed (m/sec) (Figure 13)
√ patients P2, P3 and P4 showed a similar gait speed trend in all study conditions at time T3; this trend decreased in the same patients at time T4;
√ A selective increase of gait speed was observed for patient P5 by using DAFONS at time T3 with a trend that remained unchanged at time T4.
Number of left step cycles
√ similar trend in each study condition for patient P2, P3 and P4 was observed at time T3 with a trend that remained unchanged at time T4 (except for patient P4);√ similar trend in each study condition for patient P2, P3 and P4 was observed at time T3 with a trend that remained unchanged at time T4 (except for patient P4);
√ Parameter increase by using Codivilla spring and Toe-Off for patient P1 and by using DAFONS for patient P5 at time T3 with a trend that remained unchanged at time T4. /p>
Number of right step cycles
√ similar trend in each study condition for patient P2, P3 and P4 at time T3 that remained unchanged at time T4 (except for patient P4);
√ Parameter increase by using Codivilla spring and Toe-Off for patient P1 and by using DAFONS for patient P5 at time T3 that remained unchanged at time T4.
Gait cadence (steps/min)
√ similar trend in each study condition for patient P1, P2, P3 and P4 at time T3 that remained unchanged at time T4;
√ Parameter increase by using DAFONS for patient P5 that remained unchanged at time T4.
Stride length on the right side (% cycle length)
√ similar trend in each study condition for patient P3 and P4 was observed at time T3 and for patient P2, P3 and P4 at time T4;
√ parameter increase by using DAFONS compared to Codivilla spring and Toe-Off use with a similar trend in free-walk (FW) condition for patient P1,P2 and P5 at time T3 that unchanged at time T4.
Stride length on the left side (% cycle length)
√ parameter increase by using DAFONS compared to Toe-Off use for patient P1,P3 and P5 at time T3 that unchanged at time T4; √ parameter increase by using DAFONS compared to Toe-Off use for patient P1,P3 and P5 at time T3 that unchanged at time T4;
√ Parameter decrease by using DAFONS compared to Codivilla spring and Toe-Off use for patient P2 at time T3 that unchanged at time T4.
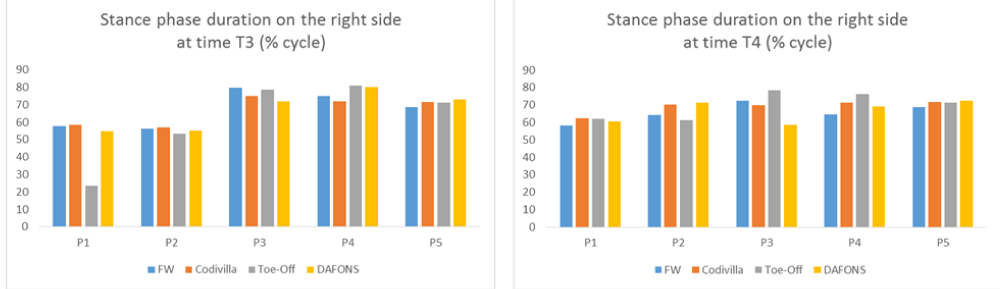
Stance phase duration on the right side (% cycle) (Figure 14)
Figure 14: Stance phase duration trend on the right side for each patient in each study condition at time T3 vs time T4.
√ parameter increase by using DAFONS vs Toe-Off use for patient P1, P2 and P5 at time T3 that remained unchanged at time T4;
√ Similar trend in each study condition for patient P3 and P4 at time T3 that unchanged at time T4.
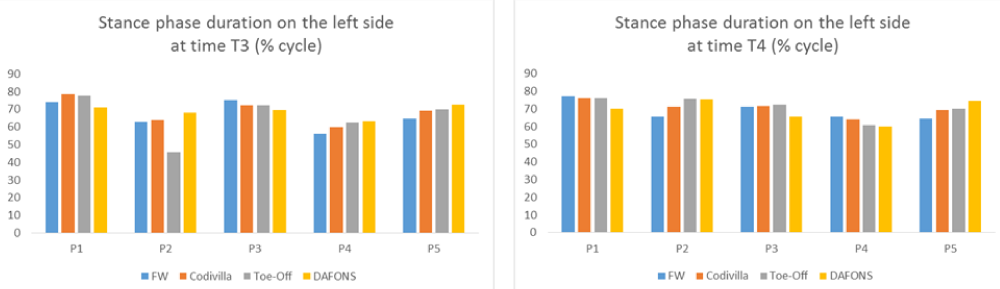
Stance phase duration on the left side (% cycle) (Figure 15)
Figure 15: Stance phase duration trend on the left side for each patient in each study condition at time T3 vs time T4.
√ parameter increase by using DAFONS for patient P2, P4 and P5 at time T3 that remained unchanged at time T4 for patient P2 and P5 (with a decrease for patient P4);
√ Similar trend in each study condition for patient P1 and P3 at time T3 that remained unchanged at time T4.
Swing phase duration on the right side (% cycle)
√ parameter increase by using DAFONS compared to the other study conditions for patient P1 and P3 at time T3 that remained unchanged at time T4 only for patient P3;
√ Parameter decrease by using DAFONS compared to Toe-Off use for patient P2 and P5 at time T3 that unchanged at time T4.
Swing phase duration on the left side (% cycle)
√ parameter increase by using DAFONS compared to the other study conditions for patient P1, P3 and P4 at time T3 that unchanged at time T4;
√ Parameter decrease by using DAFONS compared to Toe-Off use for patient P2 and P5 at time T3 that unchanged at time T4.
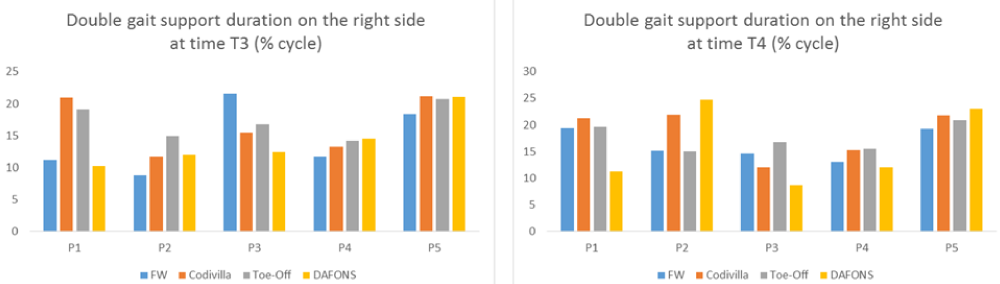
Double gait support duration on the right side (% cycle) (Figure 16)
Figure 16: Double gait support duration trend on the right side for each patient in each study condition at time T3 vs time T4.
√ parameter increase by using DAFONS compared to the other study conditions for patient P4 and P5 at time T3 that remained unchanged at time T4 for patient P5 and P2;
√ Parameter decrease by using DAFONS compared to Codivilla spring and Toe-Off use for patient P1 and P3 at time T3 that unchanged at time T4.
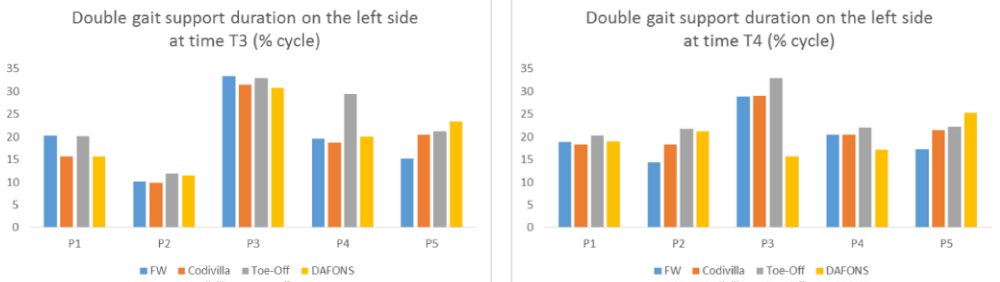
Double gait support duration on the left side (% cycle) (Figure 17)
Figure 17: Double gait support duration trend on the left side for each patient in each study condition at time T3 vs time T4.
√ parameter increase by using DAFONS compared to the other study conditions for patient P5 at time T3 that unchanged at time T4;
√ parameter decrease by using DAFONS compared to Codivilla spring and Toe-Off use for patient P1 and P3 at time T3 that unchanged at time T4;
√ a linear trend of this parameter was observed for patient P2 at time T3 with a decrease by using Toe-Off and DAFONS at time T4;
√ A selective increase of this parameter by using Toe-Off for patient P4 by using at time T3 with a trend that remained unchanged at time T4.
• Comparative analysis of BTS-G walk sensor spatio-temporal data acquired at time T3 and T4
Using a Friedman non-parametric test, we realized a comparative analysis of our spatio-temporal gait mean data acquired at time T3 (pre-treatment) versus the same data acquired at time T4 (1 month after rehabilitative treatment).
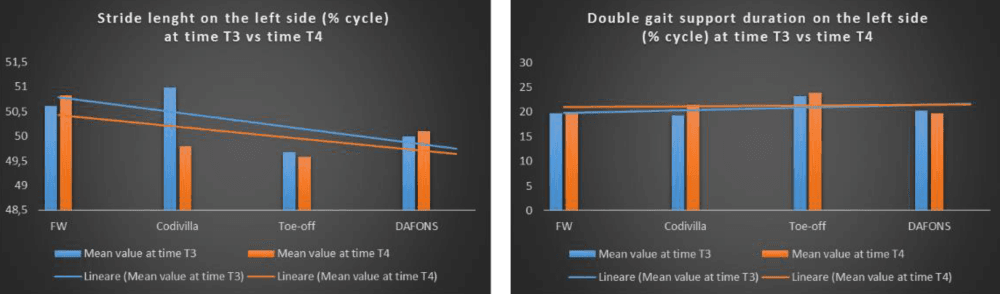
At the end of our rehabilitative treatment course (time T4) we observed (Figure 18):
Figure 18: Comparative trend of the mean values of the stride length on the left side (see the left figure) and of the double gait support duration on the left side (see figure on the right side) at time T3 vs time T4 with a relative evidence of the linear trend for each study condition per time.
- a statistical significant increase of the stride length on the left side (% cycle length) by using DAFONS vs Toe-Off in patient P1, P3 and P5 and a statistical significant decrease of this parameter by using DAFONS vs Codivilla spring and Toe-Off orthosis in patient P2 [Χ2(3)=7,159; p=0,067];
- a statistical significant increase of the double gait support duration on the left side (% cycle) by using DAFONS vs Toe-Off and Codivilla spring in patient P5 and a statistical significant decrease of this parameter by using DAFONS vs Codivilla spring and Toe-Off orthosis in patient P1 and P3 [Χ2(3)=7,32; p=0,062];
- No statistical significant differences were observed in the comparative BTS spatio-temporal analysis of the other parameters from time T3 to time T4.
The inter-time comparison between our four study conditions (FW, Codivilla spring, Toe-Off orthosis and DAFONS) and related BTS spatio-temporal gait parameters showed:
- in free-walk condition (FW), a statistical significant modification of gait speed from time T3 to time T4 [Z=-2,041; p=0,041];
- no statistical significant modifications of the spatio-temporal gait parameters by using Codivilla spring and DAFONS from time T3 to time T4 (p>0,05);
- A statistical significant modification of the double gait support duration on the right side by using Toe-off orthosis [Z=-1,826; p=0,068].
Clinical-functional outcome profile
In line with our study design, we realized a comparative analysis of our clinical-functional data acquired at time T3 (pre-treatment) versus the same data acquired at time T4. Particularly:
- MRC scale trend from time T3 to time T4
√ we observed, in all study conditions, a different grade of muscle recruitment modification of hip flexors, knee flexors, planti and dorsi-flexors of the foot at time T3 that we did not found for the hip and knee extensors; this trend showed no statistical significant modification at time T4 (p>0,05);
- MAS scale trend from time T3 to time T4
√ we found, in all study conditions, a different grade of muscle hypertonous in all lower limb muscles analyzed at time T3; this trend showed no statistical significant modification at time T4 (p>0,05);
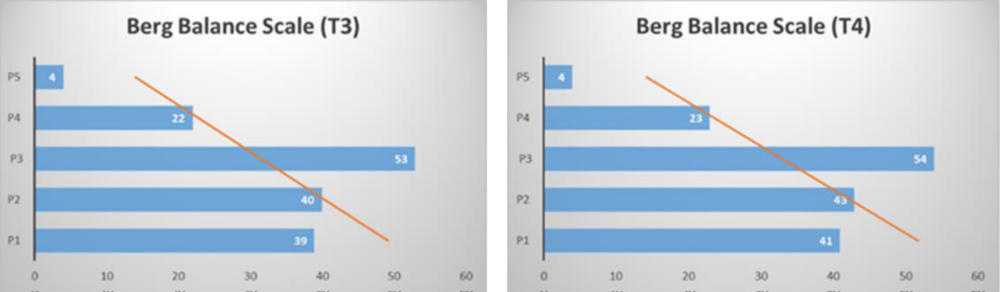
- Berg Balance scale trend from time T3 to time T4 (Figure 19)
√ we observed, in all study conditions, a different grade of orthostatic balance control analyzed with the BBS at time T3; this trend unchanged at time T4 even if a statistical significant modification was found using the Wilcoxon Signed Rank test [Z=-1,841; p=0,066].
Comparative analysis of spatio-temporal mean data vs clinical-functional data
In line with our four study conditions (FW, Codivilla spring, Toe-Off orthosis and DAFONS), we realized a comparative and time-related analysis between BTS spatio-temporal gait parameters and clinical-functional data (MRC, MAS, BBS). Particularly: at time T3, BBS trend showed a statistical significant correlation with the test duration by using Codivilla spring (r=-0,935; p=0,020); at time T4, BBS trend showed a statistical significant correlation with the test duration by using Codivilla spring (r=-0,900; p=0,038); BBS trend at time T3 showed a statistical significant correlation with the test duration by using Codivilla spring at time T4 (r=-0,893; p=0,042); BBS trend at time T4 showed a statistical significant correlation with the test duration by using Codivilla spring at time T3 (r=-0,943; p=0,016); at time T3 and T4 MAS trend showed a statistical significant correlation with the number of left step cycles acquired by using Codivilla spring at time T4 (p=0,014) and time T3 (r=0,880; p=0,049); at time T3 and T4, MAS trend showed a statistical significant correlation with the number of right step cycles acquired by using Codivilla spring at time T4 (r=0,953; p=0,012); at time T3 and T4, MAS trend showed a statistical significant correlation with the number of right step cycles acquired by using Codivilla spring at time T3 (r=0,904; p=0,035); at time T3 and T4, MAS trend showed a statistical significant correlation with the stance phase duration on the left side by using Codivilla spring at time T4 (r=0,880; p=0,049); at time T4, BBS trend showed a statistical significant correlation with the test duration acquired by using Toe-Off orthosis at time T3 (r=-0,883; p=0,047); at time T3 and T4, MAS trend showed a statistical significant correlation with the number of left step cycles acquired by using Toe-Off orthosis at time T3 (r=0,881; p=0,049); at time T3 and T4, MAS trend showed a statistical significant correlation with the number of right step cycles acquired by using Toe-Off orthosis at time T3 (r=0,923; p=0,025); at time T3 and T4, MAS trend showed a statistical significant correlation with the number of left step cycles acquired by using Toe-Off orthosis at time T4 (r=0,984; p=0,002); at time T3 and T4, MAS trend showed a statistical significant correlation with the number of right step cycles acquired by using Toe-Off orthosis at time T4 (r=0,982; p=0,003); at time T3, BBS trend showed a statistical significant correlation with the test duration acquired by using DAFONS at time T3 (r=-0,911; p=0,031); at time T4, BBS trend showed a statistical significant correlation with the test duration acquired by using DAFONS at time T3 (r=-0,918; p=0,028); at time T3 and T4, MAS trend showed a statistical significant correlation with the test duration acquired by using DAFONS at time T3 (r=0,888; p=0,044) and time T4 (r=0,918; p=0,028); at time T3, BBS trend showed a statistical significant correlation with number of left step cycles acquired by using DAFONS at time T3 (r=-0,953; p=0,012) and time T4 (r=-0,975; p=0,005); at time T4, BBS trend showed a statistical significant correlation with number of left step cycles acquired by using DAFONS at time T3 (r=-0,960; p=0,010) and time T4 (r=-0,983; p=0,003); at time T3, MAS trend showed a statistical significant correlation with the number of left step cycles acquired by using DAFONS at time T3 (r=0,915; p=0,029); at time T4, BBS trend showed a statistical significant correlation with the double gait support duration on the right side by using DAFONS at time T3 (r=-0,888; p=0,044); ); at time T3 and T4, MAS trend showed a statistical significant correlation with the number of right step cycles by using DAFONS at time T3 (r=0,933; p=0,020); at time T3, BBS trend showed a statistical significant correlation with the test duration by using DAFONS at time T4 (r=-0,915; p=0,029); at time T4, BBS trend showed a statistical significant correlation with the test duration by using DAFONS at time T4 (r=-0,924; p=0,025); at time T3 and T4, BBS trend showed a statistical significant correlation with the number of right step cycles acquired by using DAFONS at time T4 (r=-0,979; p=0,004) and T3 (r=-0,986; p=0,002).
Discussion
A careful evaluation of the literature, showed how clinicians and technicians tried to demonstrate in the last years the perceptive value and rehabilitative usefulness of DAFOs to influence the gait profile of adults and children affected by central or peripheral nervous system damages [7-12]. The original aspect of this study was to investigate, for the first time, the influence of a personalized rehabilitative model on the functional response of different ankle foot orthoses in a cohort of patients affected by neurological gait pattern. In line with our study design, we observed some very interesting conclusions. First of all, an analytical inter-personam comparison of our raw spatio-temporal data, acquired in each study condition by using the BTS-G-Walk sensor device, showed a different trend from time T3 to time T4 (1 month after rehabilitative treatment). This result demonstrated how clinical and functional heterogeneous profile of our patients influenced the different gait response induced by our three different ankle foot orthoses. Moreover, it was clear that a standardized rehabilitative model could not perform on very different gait pattern of our study patients in a short time (in 1 month). To investigate these results, we realized a comparative analysis of our spatio-temporal gait mean data acquired at time T3 (pre-treatment) versus the same data acquired at time T4 (1 month after rehabilitative treatment proposed). At the end of our rehabilitative treatment course (time T4) we observed a statistical significant increase of the stride length on the left side (% cycle lenght) by using DAFONS vs Toe-Off in patient P1, P3 and P5 and a statistical significant decrease of this parameter by using DAFONS vs Codivilla spring and Toe-Off orthosis in patient P2. Similarly, a statistical significant increase of the double gait support duration on the left side (% cycle) by using DAFONS vs Toe-Off and Codivilla spring in patient P5 and a statistical significant decrease of this parameter by using DAFONS vs Codivilla spring and Toe-Off orthosis in patient P1 and P3 was observed. No statistical significant differences were observed in the comparative BTS spatio-temporal analysis of the other parameters proceeding from time T3 to time T4. We tried to resume the interpretation of these data in six points: 1) we can modulate and realize different motor rehabilitative outcomes in relation with patient’s pathological gait pattern, lateralized body damage and grade of orthostatic and orthodynamic perceptive disorder; 2) patients who need a predominant ankle strategy balance control (feedback and feedforward ankle balance control strategy) showed a significant postural and proprioceptive response by using DAFOS (dynamic ankle foot orthoses) at the end of our rehabilitative treatment; 3) by using DAFONS, we realized an individualized remodulation of patient’s different spatio-temporal gait parameters with a predominant and similar significant effect in patient P1 and P5; according with these observations, we presume that different pathological and asimmetrical gait schema required individualized biomechanical joint calibration for each patient with an inevitable different gait response; 4) by using Neuroswing, we observed a significant “bilateral” modification of some spatio-temporal gait parameters; according to this data we highlighted the importance to perform a rehabilitative course which aims at a perfect balance between “induction to a pro-adaptive facilitation and inhibition to a maladaptive facilitation of pathological motor pattern”; 5) we presume that, related to patient’s pathological gait schema and rehabilitative goals, we used a dynamic foot orthosis (DAFONS) that, designed with an ankle joint system with preloaded disc springs, can store the energy brought in by the body weight during gait and produce and individualized tuning effect on patient’s gait and sense of balance; 6) personalization of esoscheletal design, plurimodulation of the ankle biomechanical properties, task and function specific regulation of the dynamic lever spring force with an optimization and storage of the energy brought in by the body weight which support in this way ankle’s push-off when released and control the step length on the affected and unaffected limb, defined the uniqueness of our DAFONS that we didn’t observed with Codivilla spring and Toe-Off orthosis. An inter-time comparison between our study conditions (FW, Codivilla, Toe-Off and Neuroswing) and the raw BTS spatio-temporal gait data showed an unusual and not uniform trend: a) in free-walk condition we observed a statistical significant modification of gait velocity from time T3 to time T4; b) no statistical significant modification of our raw spatio-temporal data was observed by using Codivilla spring and DAFONS from time T3 to time T4; c) a statistical significant modification of double gait support duration on the right side was noted by using Toe-Off. We presume that a short-term rehabilitative treatment and an extreme variable response secondary to different orthoses used in this study, can explain the significative gait velocity change in free-walk condition rather than using an orthoses device. In line with the purpose of this study, we also tried to establish how our personalized proprioceptive rehabilitative treatment could influence the clinical response of different AFOs in a cohort of patients affected by neurological gait pattern. For this reason we evaluated in each study condition (free-walk, with Codivilla spring, with Toe-Off and with DAFONS) patient’s multisegmental muscle recruitment by using MRC scale, patient’s multisegmental muscle hypertonous by using MAS scale and patient’s own grade of postural balance, by using the Berg Balance scale, in an ortostatic resting position and inducing a body destabilization. This clinical evaluation was made at time T3 and repeated at time T4 (after one month of rehabilitative treatment) and without any surprise we observed, in all study conditions, a different clinical response at time T3 that unchanged at time T4. In line with our four study conditions (FW, Codivilla spring, Toe-Off orthosis and DAFONS), we also realized a comparative and time-related analysis between BTS spatio-temporal gait parameters and clinical-functional data (MRC, MAS, BBS). Particularly, BBS trend showed a statistical significant correlation with the test duration by using Codivilla spring at time T3, T4 and from T3 to time T4. From an interpretative point of view, we presume that patient’s pre and post-treatment orthostatic and orthodynamic postural balance modification correlates with the BTS test duration by using a static and low elastic lever reactive orthosis as Codivilla spring. This result suggests that:
- feedback and feedforward balance strategy control can be influenced by a singular type of AFO (Codivilla spring) that showes a low elastic lever reaction and destabilization effect during stance and swing phase of gait;
- the proposed rehabilitative protocol increases orthodynamic stability, by using Codivilla spring, in all different patients treated;
- the clinical-functional correlation was significant for the test duration after the rehabilitative treatment by showing a variable increase of this parameter in all patients of this study (induction to a pro-adaptive facilitation and inhibition to a maladaptive facilitation of pathological gait pattern). Moreover, we observed a statistical significant correlation between BBS trend and double gait support duration on the right side and number of left step cycles, by using DAFONS, at time T3 and T4 and proceeding from time T3 to time T4. Most of our patients were affected by a right lateralized body damage. The use of DAFONS on the right ankle can justify the increase of patient’s orthodynamic balance in term of double gait support duration decrease on the right side (it means an increase of ankle strategy control of orthodynamic balance) and number of left step cycles increase (it means a facilitation of orthodynamic ankle control induced on the unaffected left side). Unsurprised, we demonstrated how the rehabilitative program proposed could promote the pro-adaptive and facilitation properties of a personalized gait control, induced by our Neuroswing joint system. DAFONS express properties as personalization of orthoses design, multimodulation of the biomechanic ankle/knee/hip properties during the gait cycle that we cannot realize with other orthoses (Codivilla spring and Toe-Off). A significant statistical correlation between MAS trend and number of left and right step cycles, by using Codivilla spring and Toe-Off, was also observed at time T3, T4 and proceeding from time T3 to T4. If we consider the relative significant multisegmental muscle hypertonous modification (by using Codivilla spring and Toe-Off) at the end of our rehabilitation course, the mentioned correlation could not be consider clinically significant. Contrary, in all those patients (P1, P3 and P5) affected by spastic motor pattern, we observed at the end of the rehabilitative treatment an absolute amelioration of patient’s gait quality by using DAFONS. The reciprocant joint system regulation of stance and swing phase of gait and the induction of a soft-stop effect during the so-called heel load response phase of gait are significant biomechanical properties of DAFONS that allow to realize a very singular type of orthoses with an high functional and pro-rehabilitative profile. In line with our study design, we also used a simple video off-line evaluation of our patient’s gait pattern in each study condition defined (Visual Gait Analysis) to analyze the specific malajusted and proadjusted functional effect derived from the use of the three types of orthoses considered in this study. Unsurprised, we noted an amelioration of gait quality, from time T3 to time T4, with the use of DAFONS in all those patients (P1, P3 and P5) who showed a neurocognitive competence with a related functional grade of neurorehabilitative re-learning attitude of the physiological gait pattern and with a compromised perceptive control of gait and core stability. For the umpteenth time, this result demonstrated how the proprioceptive profile of our rehabilitative program could promote the pro-adaptive and facilitation properties of a personalized gait control, induced by the Neuroswing joint system.
Conclusions
The proprioceptive profile of our rehabilitative program could promote the pro-adaptive and facilitation properties of a personalized gait control, induced by a personalized and innovative dynamic ankle foot orthoses with a modulable ankle joint system called Neuroswing. In the daily neurorehabilitative practice, DAFONS can be considered as an individualized peripheral neuro-facilitation of gait cycle (peripheral perceptive facilitation), a neurorehabilitative re-learning device of physiological gait pattern (peripheral assisted neuroplasticity facilitation) and a device that can increase patient’s motor abilities and quality of life in all daily performances. For this reason, the combined use of AFOs and rehabilitative treatment of neurological gait disorders can only be realized by a multidisciplinary equipé with technical attitudes and biomechanical and neurorehabilitative clinical knowledge.
References
- Fritz S, Lusardi M. White paper: ‘‘walking speed: The sixth vital sign”. J Geriatr Phys Ther. 2009; 32: 46-49. Ref.: https://goo.gl/cDXLgC
- Muro-de-la-Herran A, Garcia-Zapirain B, Mendez-Zorrilla A. Gait Analysis Methods: An Overview of Wearable and Non-Wearable Systems, highlighting clinical applications. Sensors (Basel). 2014; 14: 3362-3394. Ref.: https://goo.gl/GAZYXR
- Guerra Padilla M, Molina Rueda F, Alguacil D. Effect of ankle-foot orthosis on postural control after stroke: a systematic review. Neurologia. 2014; 29: 423-432. Ref.: https://goo.gl/dMQcxY
- Bleyenheuft C, Deltombe T, Detrembleur C. Influence of ankle-foot orthoses on kinematic segmental covariation among stroke patients. Ann Phys Rehabil Med. 2013; 56: 3-13. Ref.: https://goo.gl/MHpKCY
- Novacheck TF, Trost JP, Sohrweide S. Examination of the child with cerebral palsy. Orthop Clin North Am. 2010; 41: 469-488. Ref.: https://goo.gl/w7DK8X
- Fuchs S, Sandmann C, Skwara A, Chylarecki C. Quality of life 20 years after arthrodesis of the ankle. J Bone Joint Surg Br. 2003; 85: 994-998. Ref.: https://goo.gl/aycwbc
- Thoumie P, Sautreuil P, Faucher M. Evaluation des propriétés physiologiques des orthèses de cheville. Revue de littérature. Ann Readapt Med Phys. 2004; 47: 225-232. Ref.: https://goo.gl/FfzQhc
- Richie DH Jr. Effects of foot orthoses on patients with chronic ankle instability. J Am Podiatr Med Assoc. 2007; 97: 19-30. Ref.: https://goo.gl/EAHM9t
- Brehm MA, Harlaar J, Schwartz M. Effect of ankle-foot orthoses on walking efficiency and gait in children with cerebral palsy. J Rehabil Med. 2008; 40: 529-534. Ref.: https://goo.gl/kgwhjM
- Abe H, Michimata A, Sugawara K, Sugaya N, et al. Improving gait stability in stroke hemiplegic patients with a plastic ankle-foot orthosis. Tohoku J Exp Med. 2009; 218: 193-199. Ref.: https://goo.gl/8kYGKP
- Fatone S, Gard SA, Malas BS. Effect of ankle-foot orthosis alignment and foot-plate length on the gait of adults with poststroke hemiplegia. Arch Phys Med Rehabil. 2009; 90: 810-818. Ref.: https://goo.gl/vVnWac
- Kerkum YL, Brehm MA, Buizer AI, van den Noort JC, Becher JG, et al. Defining the mechanical properties of a spring-hinged foot orthosis to assess its potential use in children with spastic cerebral palsy. J Appl Biomech. 2014; 30: 728-731. Ref.: https://goo.gl/qBgeQU
- Kim ES, Yoon YS, Sohn MK, Kwak SH, Choi JH, et al. Effect of pneumatic compressing powered orthosis in stroke patients preliminary study. Ann Rehabil Med. 2015; 39: 226-233. Ref.: https://goo.gl/7q77Re
- Mulroy SJ, Eberly VJ, Gronely JK, Weiss W, Newsam CJ. Effect of AFO design on walking after stroke: impact of ankle plantar flexion contracture. Prosthet Orthot Int. 2010; 34: 277-292. Ref.: https://goo.gl/23SH7V
- Slijper A, Danielsson A, Willen C. Ambulatory Function and Perception of Confidence in Persons with Stroke with a Custom-Made Hinged versus a Standard Ankle Foot Orthosis. Rehabil Res Pract. 2012; 2012: 206495. Ref.: https://goo.gl/iRaL1a
- Falso M, Cattaneo E, Zucchini M, Zucchini F. Influence of a custom-made dynamic ankle-foot orthosis with a reciprocant ankle joint system called Neuroswing on walking spatio-temporal parameters in patients affected by neurological gait schema: a comprehensive investigational study. JJ Physical Rehab Med. 2017; 3: 029.