Case Report
Unusual presentation of a bilateral basilar stroke: Bradycardia

Zidouh S*, Jidane S, Nabhani T, Chouaib N, Sirbou R, Belkouch A and Belyamani L
Department of Emergency, Military Hospital of Instruction, Mohammed V University Rabat, Morocco
*Address for Correspondence: Zidouh S, Department of Emergency, Military Hospital of Instruction, Mohammed V University Rabat, Morocco, Email: sazi26@hotmail.fr
Dates: Submitted: 11 August 2017; Approved: 06 September 2017; Published: 07 September 2017
How to cite this article: Zidouh S, Jidane S, Nabhani T, Chouaib N, Sirbou R, et al. Unusual presentation of a bilateral basilar stroke: Bradycardia. J Clin Intensive Care Med. 2017; 2: 040-041. DOI: 10.29328/journal.jcicm.1001008
Copyright License: © 2017 Zidouh S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
We report a case of 79-year-old man who presented to our emergency department (ED) for lipothymia. The patient developed significant bradycardia with hypotension. His EKG objectified a slow atrial fibrillation .the patient rapidly installed a coma. A non-contrast CT brain scan showed a bilateral vertebrobasilar ischemic stroke.
Case Report
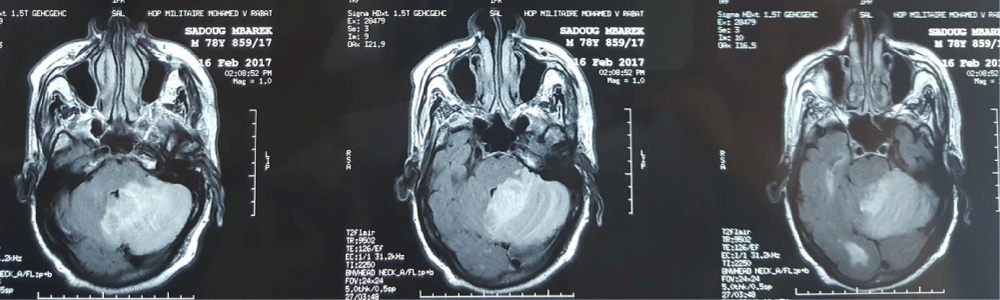
A 79-year-old male, with a history of hypertension and ischemic cardiopathy, presented to the emergency department (ED) for confusion and lipothymia without fever. Few minutes after his admission the patient developed significant bradycardia; the heart rate decreased from 97 to 32 beats per minute and blood pressure of 73/41mmHg. The patient recovered quickly after a bolus of atropine. the patient’s vital signs were noted as a temperature of 37.2ºC, pulse 85 beats per minute, and blood pressure of 133/54 mmHg. Neurological examination revealed no anomaly. His EKG showed a slow atrial fibrillation. The echocardiography found dyskinesia, septal akinesia and left atrial dilatation. However, he rapidly installed a coma with a GCS at 6. He was immediately intubated for airway protection. A non contrast CT brain scan showed a bilateral vertebrobasilar ischemic stroke and vascular leucoencephalopathy (Figure 1). He was admitted to the intensive care unit. Three days later, he suffered a massive hemorrhagic infarction compressing the fourth ventricle and died shortly after.
Discussion
Among all cases of stroke, 80% are ischemic, and 25% of infarcts are located in the vertebrobasilar arterial territory [1]. Posterior circulation stroke can have diverse presentations that are different from stroke signs in the anterior circulation due to their etiology, clinical features, and prognosis. Posterior circulation stroke can present with vertigo, ataxia, vomiting, headache in respectively, 56.25%, 48.75%, 41% and 31% of cases but also with cranial nerve abnormalities, bilateral long tract neurological sign, ‘‘locked in’’ syndrome or impaired consciousness, and complex ocular signs or cortical blindness. Ataxia in these cases is due to the involvement of cerebellum or its connections and it is responsible of high rates of mortality and morbidity, [2]. Our patient presented initially with only confusion.
Patients with acute ischemic stroke can develop cardiac manifestations as stress-induced cardiomyopathy mimicking myocardial infarction [3]. This may explain the bradycardia developed shortly after the admission in our case. It has been tried to understand the complex, yet mostly unknown, regulatory relationship between the heart and the brain and damage in brain in any form can impede normal cardiovascular function [4]. Considering risk factors, Veotsch objectived in her medical registry that hypertension was the most frequent risk factor, (66.7%), followed by hyperlipidemia (37.9%) and coronary artery disease (33.3%). Our patient had a history of hypertension. Overall, the most common findings were bulbar and pseudobulbar signs (64 patients [73.6%]), weakness (49 patients [56.3%]), and vertigo or dizziness (47 patients [54.0%]).When considering clinical symptoms and signs, decreased level of consciousness, tetraparesis or tetraplegia, and pupillary abnormalities were significantly associated with worse outcome. Outcome was much better than previously assumed. The mortality rate was 2.3%, [5]. In our case the death was caused by a common complication of ischemic: stroke infarction.
References
- Campanholo KR, Conforto AB, Rimkus CM, Miotto EC. Cognitive and Functional Impairment in Stroke Survivors with Basilar Artery Occlusive Disease. Behavioural Neurology. 2015. Ref.: https://goo.gl/j3YAz8
- Mehndiratta M, Pandey S, Nayak R, Alam A. Posterior Circulation Ischemic Stroke Clinical Characteristics, Risk Factors, and Subtypes in a North Indian Population: A Prospective Study. The Neurohospitalist. 2012; 2: 46-50. Ref.: https://goo.gl/Z2DZZD
- Lee JS, Pyung Chun Oh PC, Koh KK. Acute ischemic stroke mimicking acute coronary syndrome. International Journal of Cardiology. 2016; 221: 560-561. Ref.: https://goo.gl/GNHqss
- Bybee KA, A Prasad. Stress-related cardiomyopathy syndromes. Circulation. 2008; 118: 397-409. Ref.: https://goo.gl/c2nWzY
- Voetsch B, DeWitt LD, Pessin MS, Caplan LR. Basilar Artery Occlusive Disease in the New England Medical Center Posterior Circulation Registry. Arch Neurol. 2004; 61: 496-504. Ref.: https://goo.gl/cyZtDm