Early Results of Comparison of Hydrophilic Anatomical Mesh and Polypropylene Mesh for Laparoscopic Total Extraperitoneal (TEP) Inguinal Hernia Repair
By Mikail Uyan1, Ismail Alper Tarim2Affiliations
doi: 10.29271/jcpsp.2022.07.915ABSTRACT
Objective: To compare the results, feasibility, and effectiveness of laparoscopic total extraperitoneal (TEP) hernia repair made using anatomical hydrophilic mesh and polypropylene mesh.
Study Design: Descriptive study.
Place and Duration of Study: Department of General Surgery, Recepc Tayyip Erdoğan University Training and Research Hospital, Rize, Turkey and Department of General Surgery, Ondokuz Mayıs University Medical Faculty, Samsun, Turkey from January 2017 to October 2020.
Methodology: Comparative analysis on patient who had TEP for inguinal hernia. Group 1 included repairs using hydrophilic anatomical mesh, Group 2 included repairs using polypropylene mesh. Both were compared for operation times, complications, and return to work.
Results: There were 34 patients in Group 1 and 31 patients in Group 2. The average operation time was shorter in Group 1 (p = 0.001). Postoperative complications, were significantly less common in Group 1 (p = 0.045). Patients were able to return to their work-life earlier in Group 1 after surgery (p = 0.001).
Conclusion: Both anatomic mesh and polypropylene mesh can be used in TEP hernia repair. These two materials stand out with their different properties. Whereas anatomical mesh shortens the operation time, decreases the rate of postoperative complications, and enables the early return to work, polypropylene mesh is cost-effective and easily accessible.
Key words: Inguinal hernia, Postoperative complication, Laparoscopic total extraperitoneal (TEP).
INTRODUCTION
Inguinal hernia repair, one of the most common surgical procedures performed by general surgeons, is performed in approximately 20 million patients annually worldwide.1
The fact that inguinal hernia surgeries are performed so often has important in terms of both labor loss and cost. Many different techniques have been used over the years in operations performed for inguinal hernia. While tension techniques were used in the past, the tension-free Lichtenstein technique was first used in 1984 and the recurrence rates decreased significantly.2
With the advent of laparoscopic surgery, minimally invasive techniques have begun to be used in inguinal hernia repairs. The laparoscopic total extraperitoneal (TEP) repair technique, which was first performed in 1992, is one of the common inguinal hernia repair methods, together with the transabdominal preperitoneal (TAPP) and Lichtenstein open repair techniques. Since the surgical procedure is performed without opening the peritoneum in the TEP technique, the possibility of injury to the abdominal organs is low.3 In addition, the possibility of postoperative adhesions is less. The use of the TEP technique provides less postoperative pain and a faster recovery process.4 Laparoscopic procedures are being preferred more frequently in cases of recurrence after anterior repair, bilateral inguinal hernias, youth, and athletes.5
In the TEP method, surgeons have been using polypropylene mesh for years. Recently, anatomically shaped meshes suitable for the structure of the groin have begun to be preferred in the TEP method. The aim of this study was to compare the results, feasibility, and effectiveness of TEPs made using anatomical hydrophilic mesh and polypropylene mesh.
METHODOLOGY
This study was conducted retrospectively with the approval of the Ethics Committee of the University Faculty of Medicine (Approval No. 2021/86). The study includes a comparative analysis of patients who underwent TEP between January 2017 and October 2020, using different meshes, in two separate tertiary care university hospitals. Patients who were operated on using hydrophilic anatomical mesh is created from a macroporous polyester material were included in Group 1, and patients who were operated on using polypropylene mesh were included in Group 2. Patients' age, gender, direction of the hernia, body mass index (BMI), American Society of Anesthesia (ASA) score, type of hernia, whether the hernia was recurrent or primary, operation time, length of stay, peroperative and postoperative complications, postoperative pain status, the time to return to normal life, and recurrence rates were recorded separately for Group 1 and Group 2. Differences between groups were compared. Postoperative pain status, time to return to work or normal life, and questions about recurrence were asked on telephone. Patients younger than 18 years of age, patients who could not tolerate general anesthesia, surgeries performed with patches other than hydrophilic anatomical mesh and polypropylene mesh, and patients who used multiple staples to fix the mesh were excluded from the study.
The most commonly used surgical technique is the multi-trocar procedure, but single-incision surgery (SILS-TEP)6 or robotic surgery can also be performed.7 The authors performed the operations using multiple trocars. The patient was anesthetised in the Trendelenburg position. The anterior rectus fascia was reached by passing the layers with a semicircular incision made from under the umbilicus in the region corresponding to the hernia side. Skin and subcutaneous tissues were retracted with s-shaped retractor. Anterior rectus sheath was fully revealed. After the incision was made on the anterior rectus sheath, the rectus muscle was laterally slanted, a balloon trocar was inserted, and the operative field was created without damaging the posterior sheath. The operative field was then visualised with carbon dioxide insufflation at 8-10 mm Hg. Two 5 mm trocars were inserted either from the midline or one trocar from the midline and the other one at the umbilical level over the lineasemilunaris (Figure 1). Blunt dissection was performed under the view of the 30° telescope until the symphysis pubis was clearly visible. Inferior epigastric vessels were clearly visualised laterally on the posterior surface of the rectus muscle. The retropubic space of Retzius and the space of Bogros were expanded. Hernia defect was identified. In cases with medially located direct inguinal hernia, laterally located indirect inguinal hernia, or combined inguinal hernia, dissection of the peritoneal sac off the cord structures was performed. The femoral canal was explored in all cases. No additional trocar was required in bilateral hernias. Subsequently, 15x10 cm hydrophilic anatomical polyester mesh was placed in the patients in the first group, and a 15x10 cm polypropylene mesh prepared outside for the patients in the second group was placed in the preperitoneal area from the 10 mm trocar site. The mesh was opened in the preperitoneal space and placed to cover three areas. In both groups, the mesh was fixed to the pubis and / or Cooper ligament at only one point.
Statistical analyses were performed using IBM SPSS V22 (Chicago, USA). Pearson's chi- square test was used to compare qualitative data. Normality analyses of the quantitative data were performed using the Kolmogorov-Smirnov test. Data conforming to normal distribution were compared with t-test, and non-conforming data were compared with the Mann-Whitney U-test. Data were presented as mean ± standard deviation for normally distributed variables, and median (min – max) for non-normally distributed variables. Categorical data were expressed as count and frequency (n, %). This statistical significance value was accepted as p <0.05.
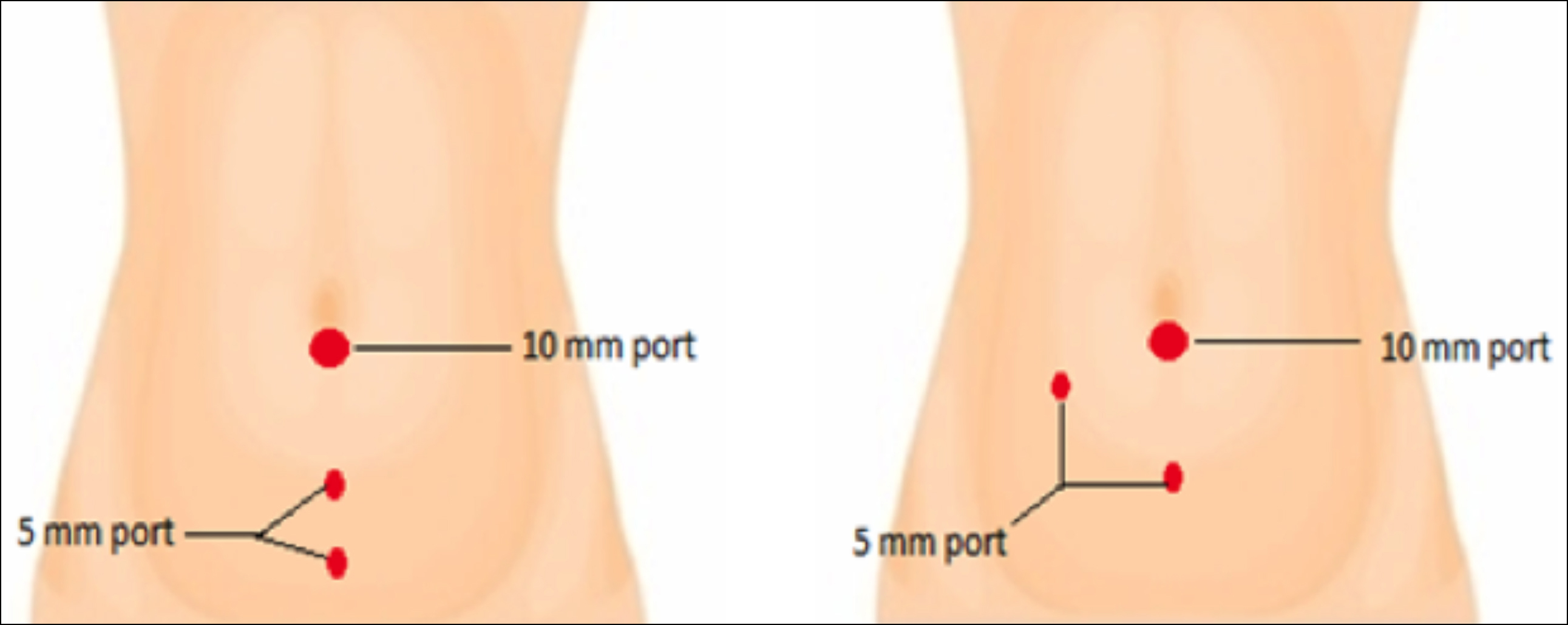 Figure 1: Position of laparoscopic ports during TEP procedure.
Figure 1: Position of laparoscopic ports during TEP procedure.
RESULTS
A total of 83 TEP repairs were performed on 65 patients. There were 34 patients in Group 1 and 31 patients in Group 2. Sixty patients (92%) were male and 5 (8%) were female.
There was no significant difference between the groups in terms of gender (p = 0.132; Table I). There was no difference in mean age in both groups (55±10.7 versus 50±11.3 years, respectively, p = 0.054; Table I). The BMI of the patients in Group 1 was significantly higher (p = 0.031, Table I). There was no difference in terms of comorbid diseases in both groups according to ASA scores (p = 0.870, Table I). There was no difference between the groups in terms of the direction of the hernia (p = 0.135, Table I). There was no difference between the groups in terms of hernia type (p = 0.311, Table I). The operation time was significantly shorter in the group using anatomical mesh (p <0.001, Table I).
In terms of peroperative complications, there was no difference between the groups (p = 0.560, Table II). Postoperative complications were significantly higher in Group 2 (p = 0.045, Table II).
All the operated patients were contacted by phone and questioned about their pain and the duration after which they returned to work and their normal lives. There was no difference between the two groups in terms of postoperative pain (p = 0.934, Table II). Return to work-life was significantly shorter in Group 1 (p=0.001, Table II). There was no difference between the two groups in terms of returning to their normal daily lives after surgery (p = 0.468, Table II). There was no difference between the groups in terms of recurrence (p = 0.664, Table II).
Table I: Demographic characteristics and characteristics of hernia.
|
|
Group 1 |
Group 2 |
p |
||||||||||||||||||||||||||||||||
|
Number of patients,n(%) |
34(52) |
31(48) |
|||||||||||||||||||||||||||||||||
|
Gender,n(%) Male Female |
33(97) 1(3) |
27(87) 4(13) |
0.132 |
||||||||||||||||||||||||||||||||
|
Age (years) mean± s.d |
55±10.7 |
50±11.3 |
0.054 |
||||||||||||||||||||||||||||||||
|
BMI (kg/m2) n(%) Weak Normal Over weight Obese |
0(0) 9(26) 19(56) 6(18) |
2(7) 13(42) 16(51) 0(0) |
0.031 |
||||||||||||||||||||||||||||||||
|
ASA, n(%) ASA1 ASA2 ASA3 |
11(32) 19(56) 4(12) |
10(32) 16(52) 5(16) |
0.870 |
||||||||||||||||||||||||||||||||
|
Direction, n(%) Right Left Bilateral Total |
16(47) 12(35) 6(18) 40(100) |
9(29) 10(32) 12(39) 43(100) |
0.135 |
||||||||||||||||||||||||||||||||
|
Herniatype, n(%) Direct Indirect Complex |
15(37.5) 14(35) 11(27.5) |
10(23) 21(49) 12(28) |
0.311 |
||||||||||||||||||||||||||||||||
|
Recurrence/primary, n(%) Relapse Primary |
5(15) 29(85) |
5(16) 26(84) |
0.874 |
||||||||||||||||||||||||||||||||
|
Operationtime (min) median(Range) |
40(30-75) |
60(40-120) |
<0.001 |
||||||||||||||||||||||||||||||||
|
Hospitalization time (days) median(Range) |
1(1-5) |
1(1-3) |
0.714 |
||||||||||||||||||||||||||||||||
|
BMI: Body mass index, ASA: American society of anesthesia.
|
|||||||||||||||||||||||||||||||||||
DISCUSSION
The probability of a person having an inguinal hernia is estimated to be 27-43% in men and 3-6% in women.8 Most of the patients in this study were male (Table I).
Patient selection plays an important role in the early stages of the learning curve. Schouten et al. reported that the selection of primary patients with the small hernia and low BMI would be more appropriate for the first cases to undergo TEP hernia.9 In this study, the patients in Group 2 were significantly weaker (Table I). It is thought that the anatomy of this region will be revealed more easily by entering the preperitoneal area more easily in weak patients, and patients with low BMI may be selected accordingly.
Open repair with spinal anesthesia will be more appropriate for those who are at risk in terms of comorbid diseases that are not suitable for general anesthesia. In this study, the patients were generally selected from those with no comorbidities or those with low-risk ASA 1 or 2, and there was no significant difference between the two groups (Table I).
In this study, the majority of patients were primary cases who had not been operated on before (Table I). Since the authors were at the beginning of the learning curve, they may have selected patients with small hernias who did not recur due to the concern that the hernia sac may be more attached due to previous surgery.
Suguita et al. reported that the learning curve was obtained after 65 cases and that the complication rates and treatment durations decreased after this period.10Aliyazicioglu et al. reported that the average operative time was 38 minutes in unilateral cases and 55 minutes in bilateral cases.11 In this study, the operation time was significantly shorter in Group 1. Operators in both groups were at the beginning of the learning curve. While creating the preperitoneal area, a balloon trocar was used in both groups and similar procedures were performed in other procedures. The only difference between the two groups was the mesh types used. Accordingly, it can be thought that the anatomical mesh can be placed in the preperitoneal area more easily and shorten the duration of the operation.
Another advantage of endoscopic procedures over open repairs is their short hospitalisation and recovery times. In this study, the average length of stay in both groups was 1 day (Table I). Peritoneal injury is one of the intraoperative complications that can occur during totally extraperitoneal (TEP) endoscopic repair for adult inguinal hernia.12 If the peritoneal injury is large, it may be necessary to return to exposure or TAPP. However, minor injuries can be repaired with stitches, staples, or clips during the procedure. Vascular injuries and deep mesh infections are rare complications.13 In this study, peritoneal injury and bleeding occurred in both groups, but no difference was observed between the groups (Table II). In indirect hernias, it may be thought that peritoneal injury or bleeding occurred during the separation of the sac from the cord structures or during the dissection performed to create a preperitoneal area, but there was no conversion to open procedure or conversion to TAPP in both groups. The most common postoperative complications after inguinal hernia repairs are hematoma, seroma, urinary retention, and surgical site infections.1 Compared to open repair, hematoma, and surgical site infections are less common in TEP, whereas seroma formation is more common.14 In this study, postoperative complications were significantly less in the group using anatomical mesh (Table II). This may suggest that the anatomically shaped mesh we use may cause less complications due to better tissue penetration.
Liew et al. reported that mesh fixation was associated with higher postoperative pain.15Additionally, Buyukasik et al. reported that fixing mesh did not reduce recurrence and increased the rate of postoperative complications (pain, narcotic use).16 In this study, there was no difference between the two groups in terms of postoperative pain. In both groups, the mesh was fixed with a single stapler placed in the sypmphysis pubis and there was no difference in terms of postoperative pain.
Inguinal hernia is a common condition in working people. It is also important for these people to return to their normal activities in socioeconomic terms. Meta-analyses reported in the literature have shown that the recovery times of endoscopic techniques were shorter than classical techniques.17,18 Hedberg et al. demonstrated a significant improvement in quality of life after laparoscopy in inguinal hernia repair.19 In this study, patients in Group 1 significantly improved in the early period and were able to return to their business life. There was no difference between the two groups in the period of returning to their previous activities and normal life before the operation (Table II). The reason why patients recover in the early period and return to their work-life may be due to the fact that the anatomical mesh we put in the preperitoneal area fits better and causes less inflammation.
Recent systematic reviews and meta-analyses have reported that there is no difference between TEP and the Lichtenstein technique in terms of recurrence.20 In this study, there was no difference between the two groups in terms of recurrence (Table II). This shows that there is no difference in ensuring tissue integrity in both meshes.
This study has several limitations. The authors were not be able to detect early postoperative complications, as the vast majority of patients with TEP are discharged within a day or two. We reached all patients by phone and inquired about post-discharge pain, time to return to work and normal life, and relapse. However, patients who have undergone surgery a long time ago may have given erroneous information. In addition, even if the disease has recurred, patients may not be aware of it in the early period.
CONCLUSION
In laparoscopic total extraperitoneal (TEP) inguinal hernia repair, the use of both anatomic mesh and polypropylene mesh is appropriate surgical options. These two separate medical materials have advantages over each other. While anatomical mesh shortens the operation time with its ease of use, decreases the rate of postoperative complications, and enables an earlier return to work-life, polypropylene mesh stands out in terms of affordable cost and easy accessibility.
COMPETING INTEREST:
The authors declared no competing interest.
ETHICAL APPROVAL:
The study was approved by the University’s Non-Invasive Clinical Research Ethics Committee (Approval No. 2021/86, date: 29.04.2021).
PATIENT’S CONSENT:
Since the study was a retrospective archive search, informed consent was not obtained from the patients.
AUTHORS’ CONTRIBUTION:
MU: Concept, design, supervision, data collection and / or processing, literature review, and writing.
IAT: Interpretation, critical revision.
All authors approved the final version of the manuscript to be published.
REFERENCES
- Lomnicki J, Leszko A, Kulis D, Szura M. Current treatment of the inguinal hernia - the role of the totally extra-peritoneal (TEP) hernia repair. Folıa Medıca Cracovıensıa 2018; 58(3):103-14. doi: 10.24425/fmc.2018.125076.
- Amid PK , Shulman AG, Lichtenstein IL. The Lichtenstein open "tension-free" mesh repair of inguinal hernias. Surg Today 1995; 25(7):619-625. doi: 10.1007/BF00311436.
- Meyer A, Blanc P, Balique JG, Kitamura M, Juan RT, Delacoste F, et al. Laparoscopic totally extraperitoneal inguinal hernia repair: Twenty-seven serious complications after 4565 consecutive operations. Rev Col Bras Cir 2013; 40(1):32-6. doi: 10.1590/s0100-6991201 30001 00006.
- Garofalo F, Mota-Moya P, Munday A, Romy S. Total extraperitoneal hernia repair: Residency teaching program and outcome evaluation. World J Surg 2017; 41(1):100-105. doi: 10.1007/s00268-016-3710-z.
- Miserez M, Peeters E, Aufenacker T, Bouillot JL, Campanelli G, Conze J, et al. Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia 2014; 18(2):151-63. doi: 10.1007/s10029-014-1236-6.
- Dapri G, Gerard L, Paesmans M, Cadière GB, Saussez S. First 200 consecutive transumbilical single-incision laparoscopic TEPs. Hernia 2017; 21(1):29-35. doi: 10. 1007/s10029-016-1564-9.
- Cestari A, Galli AC, Sangalli MN, Zanoni M, Ferrari M, Roviaro G. Totally extraperitoneal (TEP) bilateral hernioplasty using the Single Site® robotic da Vinci platform (DV-SS TEP): description of the technique and preliminary results. Hernia 2017; 21(3):383-89. doi: 10.1007/s10029-016-1552-0.
- The Hernia Surge Group. International guidelines for groin hernia management. Hernia 2018; 22(1):1-165. doi: 10.1007/s10029-017-1668-x.
- Schouten N, Simmermacher RKJ, van Dalen T, Smakman N, Clevers GJ, Davids PHP, et al. Is there an end of the “learning curve” of endoscopic totally extra-peritoneal (TEP) hernia repair? Surg Endosc 2013; 27(3):789-94. doi: 10.1007/s00464-012-2512-0.
- Suguita FY, Essu FF , Oliveira LT , Luamoto LR , Kato JM, Torsani MB, et al. Learning curve takes 65 repetition of totally extraperitoneal laparoscopy on inguinal hernias for reduction of operating time and complications. Surg Endosc 2017; 31(10):3939-45. doi: 10.1007/s00464- 017-5426-z.
- Aliyazicioglu T, Yalti T, Kabaoglu B. Laparoscopic total extraperitoneal (TEP) inguinal hernia repair using 3-dimensional mesh without mesh fixation. Surg Laparos Endosc Percutan Tech 2017; 27(4):282-4. doi: 10.1097/ SLE.0000000000000423.
- Koyama T, Xiang Z, Nagai T, Komoto M, Osawa N, Fujiwara I. Causes of peritoneal injury during laparoscopic totally extraperitoneal inguinal hernia repair and methods of repair. Asian J Endosc Surg 2021; 14(3):353-60.doi: 10.1111/ases.12869.
- McCormack K, Wake BL, Fraser C, Vale L, Perez J, Grant A. Transabdominal pre-peritoneal (TAPP) versus totally extraperitoneal (TEP) laparoscopic techniques for inguinal hernia repair: A systematic review. Hernia 2005; 9(2):109-14. doi: 10.1007/s10029-004-0309-3.
- Simons MP, Aufenacker T, Bay-Nielse M, Bouillot JL, Campanelli G, Conze J, et al. European hernia society guidelines on the treatment of inguinal hernia in adult patients. Hernia 2009; 13(4):343-403. doi: 10.1007/ s10029-009-0529-7.
- Liew W, Wai YY, Kosai NR, Gendeh HS. Tackers versus glue mesh fixation: An objective assessment of post-operative acute and chronic pain using inflammatory markers. Hernia 2017; 21(4):549-54.doi: 10.1007/ s10029-017-1611-1.
- Buyukasik K, Ari A, Akce B, Tatar C, Segmen O, Bektas H. Comparison of mesh fixation and non-fi xation in laparoscopic totally extraperitoneal inguinal hernia repair. Hernia 2017; 21(4):543-48. doi: 10.1007/s10029-017- 1590-2.
- Bringman S, Ramel S, Heikkinen TJ, Englund T, Westman B, Anderberg B. Tension-free inguinal hernia repair: TEP versus mesh-plug versus Lichtenstein: A prospective, randomised and controlled trial. Ann Surg 2003; 237(1):142-7. doi: 10.1097/00000658-200301000-00 020.
- Kuhry E, van Veen RN, Langeveld HR, Steyerberg EW, Jeekel J, Bonjer HJ. Open or endoscopic total extraperitoneal inguinal hernia repair? A systematic review. Surg Endosc 2007; 21(2):161-6. doi: 10.1007/ s00464-006-0167-4.
- Hedberg HM, Hall T, Gitelis M, Lapin B, Butt Z, Linn JG, et al. Quality of life after laparoscopic totally extraperitoneal repair of an asymptomatic inguinal hernia. Surg Endosc 2018; 32(2):813-9. doi: 10.1007/s00464-017-5748-x.
- Burgmans JP, Voorbrood CE, van Dalen T, Boxhoorn RN , Clevers GJ , Sanders FBM, et al. Chronic pain aft er TEP inguinal hernia repair, does MRI reveal a cause? Hernia 2016; 20:55-62. doi: 10.1007/s10029-015-1448-4.