- Department of Neurosurgery, Dr. Rajendra Prasad Government Medical College, Tanda Medical College, Kangra, Himachal Pradesh, India.
- Department of Neurosurgery, All India Institute of Medical Sciences, New Delhi, India.
Correspondence Address:
Mukesh Kumar, Department of Neurosurgery, Dr. Rajendra Prasad Government Medical College, Tanda Medical College, Kangra, Himachal Pradesh, India.
DOI:10.25259/SNI_774_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mukesh Kumar1, Amit Joshi1, Rajesh Kumar Meena2, Shrish Nalin1. Atypical intradiploic meningioma: A case report and review of the literature. 11-Feb-2022;13:46
How to cite this URL: Mukesh Kumar1, Amit Joshi1, Rajesh Kumar Meena2, Shrish Nalin1. Atypical intradiploic meningioma: A case report and review of the literature. 11-Feb-2022;13:46. Available from: https://surgicalneurologyint.com/surgicalint-articles/11384/
Abstract
Background: Intradiploic meningiomas with osteolytic bony changes are rarely reported in the literature. Intradiploic meningiomas are usually slow-growing benign lesions but atypical histopathology predicts aggressive behavior. Atypical intradiploic meningiomas (WHO Grade II) have some controversies in the management which are highlighted in this article.
Case Description: A 40-year-old male, with a history of trauma to the head 12 years back, presented with a hard, slow-growing painless swelling exactly at the site of trauma. On imaging, lesion was intradiploic one with osteolytic margins and homogeneously enhancing on contrast magnetic resonance imaging. Biopsy was that of atypical meningioma (WHO Grade II).
Conclusion: Atypical meningiomas with osteolytic changes are rarely reported in the literature. Because of potential aggressive behavior, they need a regular follow-up with radiological imaging.
Keywords: Atypical, Intradiploic, Meningioma, Primary extradural meningioma
INTRODUCTION
Intradiploic meningiomas or intraosseous meningiomas are a subtype of primary extradural meningiomas (PEMs) that have been rarely reported in the literature, accounting for 1–2% of all meningiomas.[
CASE REPORT
A 40-year-old male patient presented with a history of large bony swelling over the right parietal region. He had a history of trauma to the head 12 years back, following which he started noticing a gradually progressive, painless swelling over the right parietal eminence. On examination, the swelling was bony hard, immobile, and globular in shape with an approximate size of 8.0 × 9.0 cm [
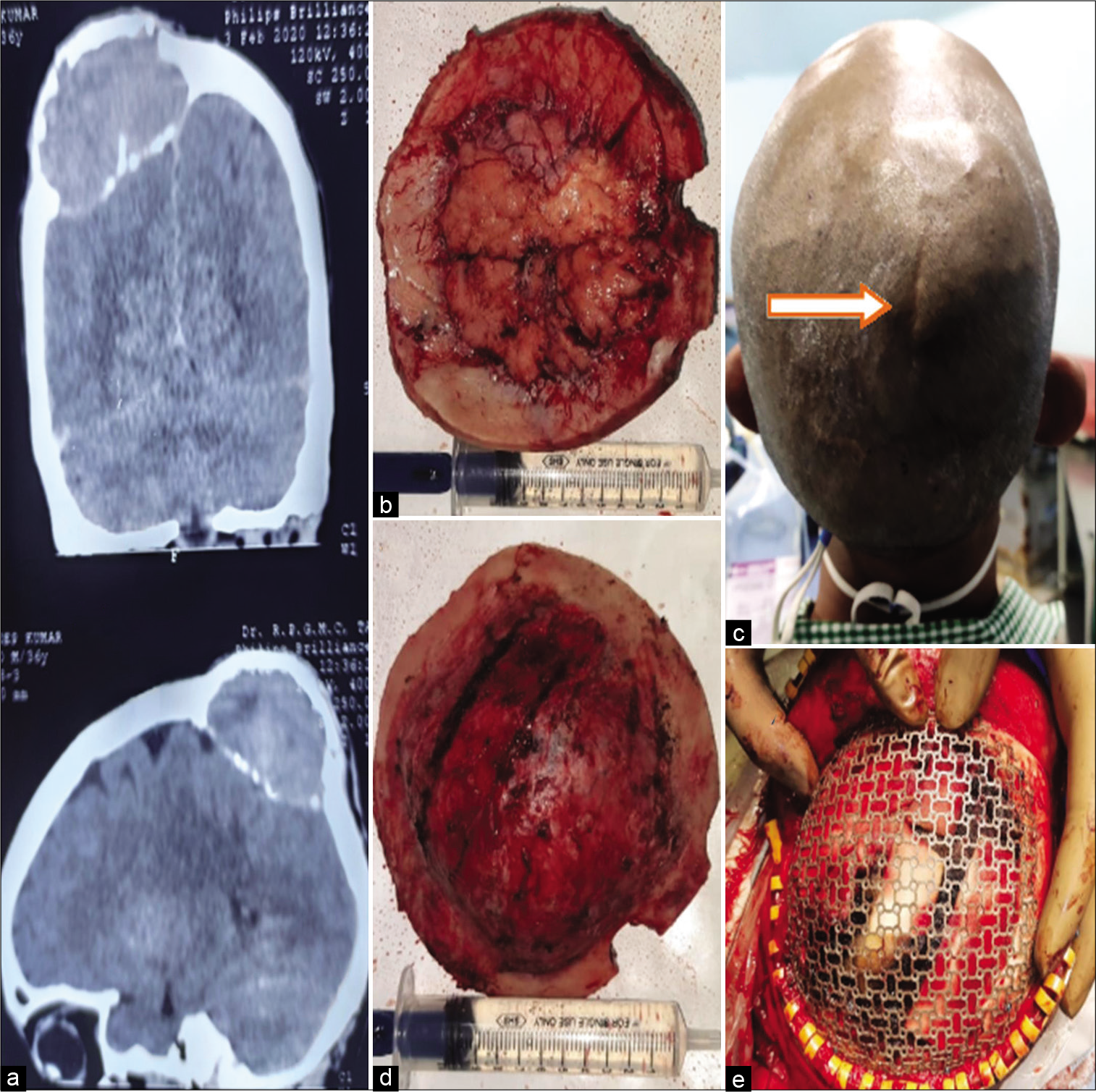
Figure 1:
Noncontrast computerized tomography head showing lesion within the outer and inner table of the skull with osteolytic margins (a). Meningioma eroded both the tables (b and d). Scalp showing evidence of scar mark (Arrow) induced by trauma over the lesion (c). The defect created is reconstructed by mesh (e).
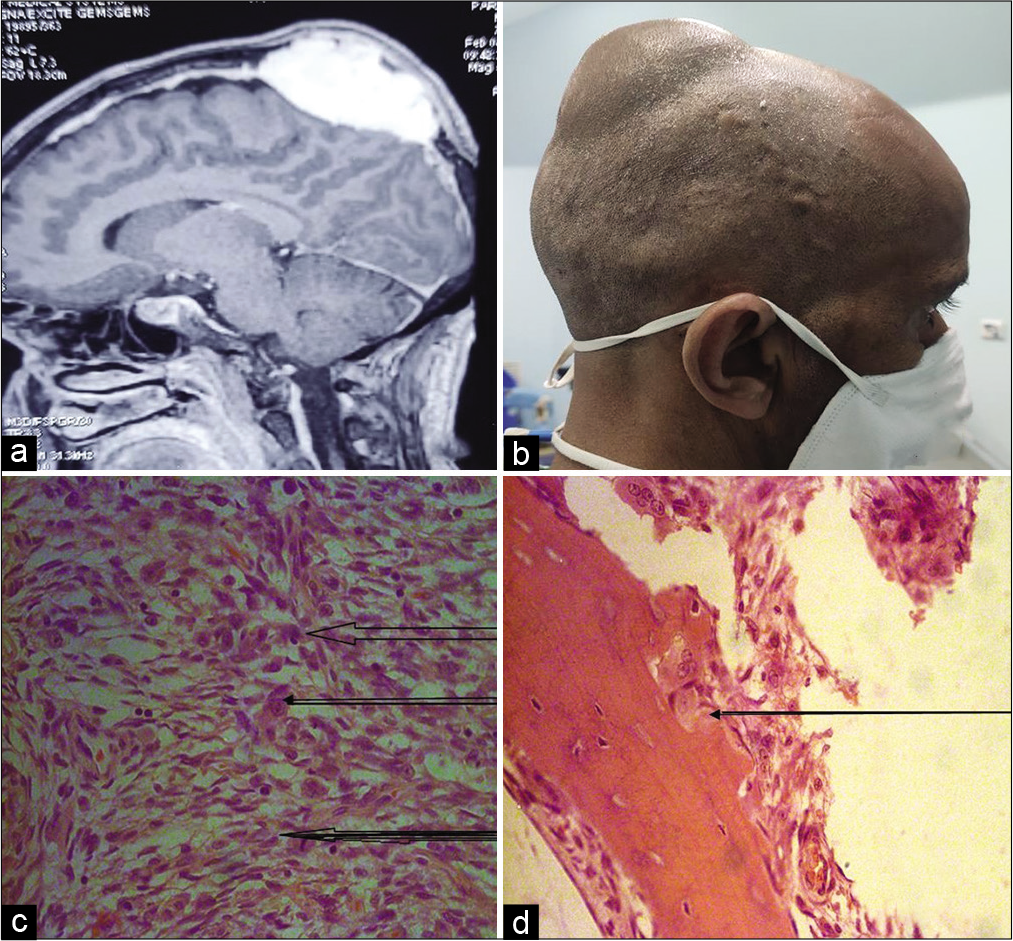
Figure 2:
Magnetic resonance imaging brain showing intradiploic meningioma (a). Patient having external swelling of tumor (b). Histopathology showing whorl of meningothelial cells (upper large arrow), prominent nucleoli (middle arrow), atypical mitosis (lower dark arrow) suggestive of atypical meningioma (c). Infiltration of meningothelial cells into the bony tissue with H and E 200× (d).
DISCUSSION
Meningiomas are the most common primary brain tumors.[
Origin of intradiploic meningiomas
The hypothesis regarding their origin is still controversial. Entrapment of arachnoid cap cells or meningocytes along the cranial suture’s lines during molding of the head at birth has been proposed; however, it was found that only 8.3% of the calvarial meningiomas were related to the cranial suture line.[
Clinical presentations
They usually present as a hard, painless, and slow-growing swelling over the scalp. Mild headache and dizziness, along with neurological deficits, may also be present depending on the size, type, and location of the tumor.
On imaging
Although, these tumors delineate well on contrast magnetic resonance imaging (MRI), noncontrast computerized tomography head with bone window is often required to rule out sclerotic margins/osteolytic margins and further characterization of the lesion. These tumors are usually hypointense on T1-weighted MRI imaging and hyperintense on T2-weighted MRI imaging and show vivid and homogeneous enhancement after gadolinium administration [
Differential diagnosis
Intradiploic meningiomas are generally misdiagnosed as bony tumors of skull and fibrous dysplasia’s. Other differential diagnosis for osteolytic intraosseous meningiomas includes metastatic cancer, plasmacytoma, giant cell tumor, osteogenic sarcoma, eosinophilic granuloma, and aneurysmal bone cyst.
Histopathologically, the most of the intraosseous meningiomas are WHO Grade 1 lesion with psammomatous and meningothelial subtypes being the most frequently seen.[
Treatment of choice
The treatment modality of choice is en bloc wide resection. When there is suspicion of having an atypical/malignant component because of extracalvarial extension, one should do wide en bloc resection of the lesion with 1 cm resection of normal bone margin,[
CONCLUSION
Atypical intradiploic meningiomas with osteolytic changes are rare entities among all meningiomas. One should go for a wide en bloc resection with at least 1 cm apparently healthy bony margin and should strongly consider adjuvant radiotherapy/chemotherapy for unresectable, partially resectable, residual, or recurrent lesions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Nil.
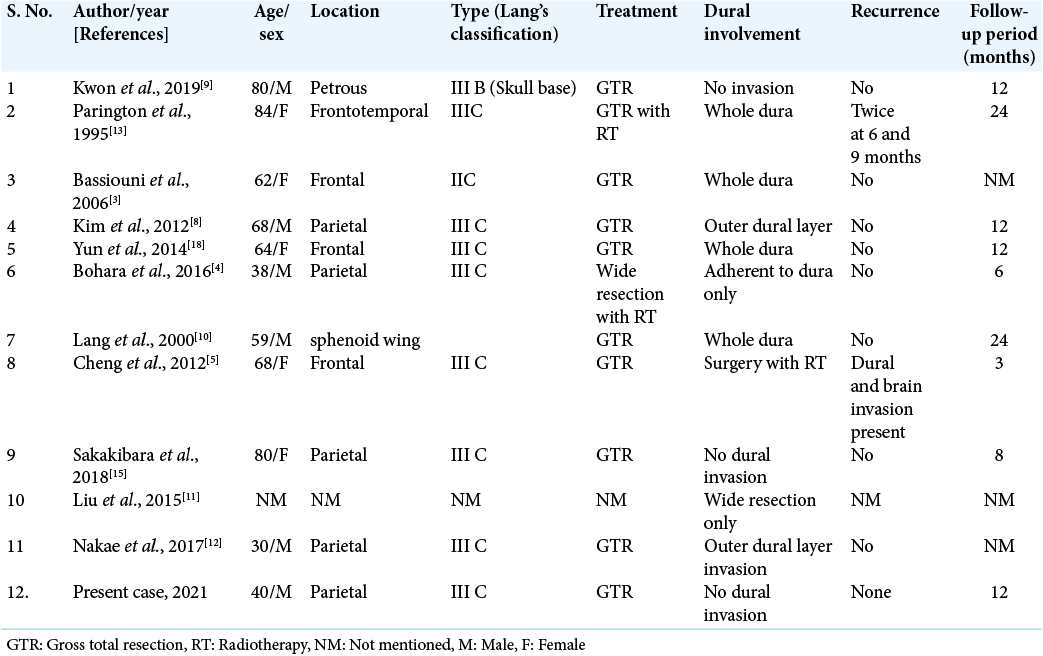
References
1. Agrawal V, Ludwig N, Agrawal A, Bulsara KR. Intraosseous intracranial meningioma. Am J Neuroradiol. 2007. 28: 314-5
2. Austin M, Betsy H, James O, David R, McLendon R, Cory A. Treatment recommendations for primary extradural meningiomas. Cancer. 2011. 117: 24-38
3. Bassiouni H, Asgari S, Hubschen U, Konig HJ. Dural involvement in primary extradural meningiomas of the cranial vault. J Neurosurg. 2006. 105: 51-9
4. Bohara S, Agarwal S, Khurana N, Pandey PN. Primary intraosseous atypical inflammatory meningioma presenting as a lytic skull lesion: Case report with review of literature. Indian J Pathol Microbiol. 2016. 59: 386-8
5. Cheng HT, Cheng CH, Chio CC, Chang ST. Atypical intraossoeous osteolytic meningioma mimicking calvarial metastasis. Form J Surg. 2012. 45: 69-72
6. Cirak B, Guven MB, Ugras S, Kutluhan A, Unal O. Frontoorbitonasal intradiploic meningioma in a child. Pediatr Neurosurg. 2000. 32: 48-51
7. Cushing H, Eisenhardt L.editors. Meningiomas: Their Classification, Regional Behavior, Life History and Surgical End Results. Springfield, Ill: Charles C Thomas; 1938. p.
8. Kim H, Jung TY, Kim IY, Lee JK. Two cases of primary osteolytic intraosseous meningioma of the skull metastasizing to whole skull and the spine. J Korean Neurosurg Soc. 2012. 51: 151-4
9. Kwon SM, Ko Y, Bang SS. Primary intraosseous osteolytic meningioma: A case report and review of the literature. BMC Neurol. 2019. 19: 176
10. Lang FF, Macdonald OK, Fuller GN, DeMonte F. Primary extradural meningiomas: A report on nine cases and review of the literature from the era of computerized tomography scanning. J Neurosurg. 2000. 93: 940-50
11. Liu Y, Wang H, Shao H, Wang C. Primary extradural meningiomas in head: A report of 19 cases and review of literature. Int J Clin Exp Pathol. 2015. 8: 5624-32
12. Nakae S, Uchida H, Takayanagi T, Hasegawa M. Atypical intraosseous meningioma with growth hormone deficiency and hyperparathyroidism after craniospinal irradiation. Childs Nerv Syst. 2017. 33: 2077-8
13. Partington MD, Scheithauer BW, Piepgras DG. Carcinoembryonic antigen production associated with an osteolytic meningioma. J Neurosurg. 1995. 82: 489-92
14. Rogers L, Barani I, Chamberlain M, Kaley TJ, McDermott M, Raizer J. Meningiomas: Knowledge base, treatment outcomes, and uncertainties. A RANO review. J Neurosurg. 2015. 122: 4-23
15. Sakakibara Y, Taguchi Y, Nakamura H, Onodera H, Wakui D. A case of primary extradural meningioma located at the high convexity: A case report and review of the literature. No Shinkei Geka. 2018. 46: 523-8
16. Shuangshotis S.editors. Primary Meningioma Outside the Central Nervous System: Meningioma. New York: Raven Press; 1991. p. 107-28
17. Thompson LD, Bouffard JP, Sandberg GD, Mena H. Primary ear and temporal bone meningiomas: A clinicopathologic study of 36 cases with a review of the literature. Mod Pathol. 2003. 16: 236-45
18. Yun JH, Lee SK. Primary osteolytic intraosseous atypical meningioma with soft tissue and dural invasion: Report of a case and review of literatures. J Korean Neurosurg Soc. 2014. 56: 509-12