Abstract
Purpose
Due to mass population movements driven by internal conflicts and wars, cutaneous leishmaniasis (CL) is becoming increasingly important in Turkey. This study is aimed at determining the clinical aspects, diagnosis and genotyping of CL patients coming to Turkey from abroad.
Methods
In our study, the clinical materials obtained from the patients or sent for diagnostic purposes from other centers to our laboratory between years 2012 and 2016 were assessed retrospectively. In total, there were 38 patients from Syria, Iraq, Afghanistan, Iran, and Turkmenistan.
Results
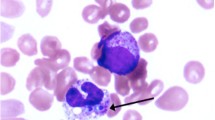
29 (76%), 28 (73%) and 33 (87%) samples were positive by light microscopy, Novy-McNeal-Nicolle(NNN), and enriched medium, respectively. By ITS-1 gene region PCR, 31 (81%) of the cases were positive. 35 of the patients were tested positive by at least one of the diagnostic methods. By genotyping, 21 Leishmania tropica, 8 Leishmania major, 3 Leismania infantum, 2 Leishmania donovani, and 1 Leishmania aethopica were detected.
Conclusion
This study is aimed at informing the clinicians working in the field for the import CL cases and recording the changing epidemiological features of CL in the region as well as discussing the possible focus for L. aethiopica infection which has not been shown in the region before.




Similar content being viewed by others
References
Reyburn H, Rowland M, Mohsen M, Khan B, Davies C (2003) The prolonged epidemic of anthroponotic cutaneous leishmaniasis in Kabul, Afghanistan: ‘bringing down the neighbourhood’. Trans R Soc Trop Med Hyg 97:170–176. https://doi.org/10.1016/S0035-9203(03)90111-8
Okwor I, Uzonna J (2016) Social and economic burden of human leishmaniasis. Am J Trop Med Hyg 94:489–493. https://doi.org/10.4269/ajtmh.15-0408
World Health Organization/Department of Control of Neglected Tropical Diseases (2017) Global leishmaniasis update, 2006–2015: a turning point in leishmaniasis surveillance. Wkly Epidemiol Rec 92:557–565. https://doi.org/10.1016/S0140-6736(09)61877
Schweiger G (2016) The duty to bring children living in conflict zones to a safe haven. https://doi.org/10.1080/17449626.2016.1247744
Raleigh C, Jordan L, Salehyan I (2008) Assessing the ımpact of climate change on migration and conflict. Social Development, The World Bank, Washington, DC
McMichael C (2015) Climate change-related migration and infectious disease. Virulence 6:548–553. https://doi.org/10.1080/21505594.2015.1021539
Demirel R, Erdoğan S (2009) Determination of high risk regions of cutaneous leishmaniasis in Turkey using spatial analysis. Turk Parazitol Derg 33:8–14
Zeyrek FY, Gürses G, Uluca N, Doni NY, Toprak Ş, Yeşilova Y, Çulha G (2014) Şanlıurfa’ da Şark Çıbanı Etkeni Değişiyor mu ? İlk Leishmania major Vakaları Is the agent of Cutaneous Leishmaniasis in Sanliurfa changing ? First Cases Leishmania Major. https://doi.org/10.5152/tpd.2014.3820
Harman M (2017) Leishmaniasis in Turkey: visceral and cutaneous leishmaniasis caused by Leishmania donovani in Turkey. Acta Trop. https://doi.org/10.1016/j.actatropica.2017.05.032
Özbilgin A, Çulha G, Uzun S, Harman M, Topal SG, Okudan F, Zeyrek F, Gündüz C, Östan İ, Karakuş M, Töz S, Kurt Ö, Akyar I, Erat A, Güngör D, Kayabaşı Ç, Çavuş İ, Bastien P, Pratlong F, Kocagöz T, Özbel Y (2016) Leishmaniasis in Turkey: first clinical isolation of Leishmania major from 18 autochthonous cases of cutaneous leishmaniasis in four geographical regions. Trop Med Int Health 21:783–791. https://doi.org/10.1111/tmi.12698
Akilov OE, Khachemoune A, Hasan T (2007) Clinical manifestations and classification of Old World cutaneous leishmaniasis. Int J Dermatol 46:132–142. https://doi.org/10.1111/j.1365-4632.2007.03154.x
Harman M (2015) Kutanöz leishmaniasis. Turk Dermatol Derg 9:168–179. https://doi.org/10.4274/tdd.2880
Durdu M, Akyol M, Uzun S, Mehmet SG, Ozbel Y, Yes Y (2018) Tropical medicine rounds Clinical practice guidelines for the diagnosis and treatment of cutaneous leishmaniasis in Turkey dem Asena Do g ß i g ß e Akman-Karakas. https://doi.org/10.1111/ijd.14002
Chouihi E, Amri F, Bouslimi N, Siala E, Selmi K, Zallagua N, Ben Abdallah R, Bouratbine A, Aoun K (2009) Les cultures sur milieu NNN dans le diagnostic biologique des leishmanioses. Pathol Biol 57:219–224. https://doi.org/10.1016/j.patbio.2008.03.007
Garin YJF, Meneceur P, Sulahian A, Derouin F (2002) Microplate method for obtaining Leishmania clonal populations. J Parasitol 88:803–804. https://doi.org/10.1645/0022-3395(2002)088%5b0803:mmfolc%5d2.0.co;2
Toz SO, Culha G, Zeyrek FY, Ertabaklar H, Alkan MZ, Vardarli AT, Gunduz C, Ozbel Y (2013) A real-time ITS1-PCR based method in the diagnosis and species identification of Leishmania parasite from human and dog clinical samples in Turkey. PLoS Negl Trop Dis 7:1–8. https://doi.org/10.1371/journal.pntd.0002205
Hide M, Bañuls AL (2006) Species-specific PCR assay for L. infantum/L. donovani discrimination. Acta Trop 100:241–245. https://doi.org/10.1016/j.actatropica.2006.10.012
BCr M, İbrahim Çavuş F, Dırrı Çam AÖ (2018) Leishmania spp. CPB Gen Bölgesine Özgü Primer ile Leishmania infantum/Leishmania donovani Tür Ayrımı. In: XXXVIII. International Turkish Microbiology Congress
Ashford RW, Rioux JA, Jalouk L, Khiami A, Dye C (1993) Evidence for a long-term increase in the incidence of Leishmania tropica in Aleppo, Syria. Trans R Soc Trop Med Hyg 87:247–249
EWARS Review (2013), vol 7, no 2. http://www.moh.gov.sy/pages/EpidemicBulletin/pdf_archive/2013/4-2013.pdf
McDowell MA, Rafati S, Ramalho-Ortigao M, Ben Salah A (2011) Leishmaniasis: middle East and North Africa research and development priorities. PLoS Negl Trop Dis 5:e1219. https://doi.org/10.1371/journal.pntd.0001219
AlSamarai AM, AlObaidi HS (2009) Cutaneous leishmaniasis in Iraq. J Infect Dev Ctries 3:123–129
Faulde M, Schrader J, Heyl G, Amirih M, Hoerauf A (2008) Zoonotic cutaneous leishmaniasis outbreak in Mazar-e Sharif, northern Afghanistan: an epidemiological evaluation. Int J Med Microbiol 298:543–550. https://doi.org/10.1016/j.ijmm.2007.07.015
Sharifi I, Aflatoonian MR, Fekri AR, Hakimi Parizi M, Aghaei Afshar A, Khosravi A, Sharifi F, Aflatoonian B, Khamesipour A, Dowlati Y, Modabber F, Nadim A (2015) A comprehensive review of cutaneous leishmaniasis in kerman province, southeastern Iran-narrative review article. Iran J Public Health 44:299–307
Çizmeci Z, Karaku M (2019) Acta tropica leishmaniasis in Istanbul; a new epidemiological data about refugee leishmaniasis. Acta Trop 195:23–27. https://doi.org/10.1016/j.actatropica.2019.04.008
Karaku M (2019) The impact of refugees on leishmaniasis in Turkey : a new Syrian/Turkish Leishmania tropica population structure described by multilocus microsatellite typing (MLMT). Parasitol Res 118:2679–2687
Özkeklikçi A, Karakuş M, Özbel Y, Töz S (2016) The new situation of Cutaneous Leishmaniasis after Syrian civil war in Gaziantep city, Southeastern region of Turkey. Acta Trop. https://doi.org/10.1016/j.actatropica.2016.10.019
Eroglu F, Ozgoztasi O (2019) The increasead of neglected cutaneous leishmaniasis in Gaziantep province of Turkey after mass human migration. Acta Trop 192:138–143. https://doi.org/10.1016/j.actatropica.2019.01.026
Koltas IS, Eroglu F, Alabaz D, Uzun S (2014) The emergence of Leishmania major and Leishmania donovani in southern Turkey. Trans R Soc Trop Med Hyg 108:154–158. https://doi.org/10.1093/trstmh/trt119
Özbilgin A, Harman M, Karakuş M, Bart A, Töz S, Kurt Ö, Çavuş İ, Polat E, Gündüz C, Van Gool T, Özbel Y (2017) Leishmaniasis in Turkey: visceral and cutaneous leishmaniasis caused by Leishmania donovani in Turkey. Acta Trop 173:90–96. https://doi.org/10.1016/j.actatropica.2017.05.032
Rioux JA, Léger N, Haddad N, Desjeux P (1998) Natural infestation of Phlebotomus tobbi (Diptera, Psychodidae) by Leishmania donovani s.st (Kinetoplastida, Trypanosomatidae) in Syria. Parasitologia 40:148
Antoniou M, Haralambous C, Mazeris A, Pratlong F, Dedet J-P, Soteriadou K (2008) Leishmania donovani leishmaniasis in Cyprus. Lancet Infect Dis 8:6–7. https://doi.org/10.1016/S1473-3099(07)70297-9
Zahangir M, Haralambous C, Kuhls K, Gouzelou E, Sgouras D, Soteriadou K, Schnur L, Pratlong F, Scho G (2009) The paraphyletic composition of Leishmania donovani zymodeme MON-37 revealed by multilocus microsatellite typing. Microbes Infect 11:707–715. https://doi.org/10.1016/j.micinf.2009.04.009
Hotez PJ, Savioli L, Fenwick A (2012) Neglected tropical diseases of the Middle East and North Africa: review of their prevalence, distribution, and opportunities for control. PLoS Negl Trop Dis 6:e1475. https://doi.org/10.1371/journal.pntd.0001475
Magill AJ (2013) Leishmaniasis. Hunter’s tropical medicine and emerging infectious disease. Elsevier, Amsterdam, pp 739–760
Gebre-Michael T, Balkew M, Ali A, Ludovisi A, Gramiccia M (2004) The isolation of Leishmania tropica and L. aethiopica from Phlebotomus (Paraphlebotomus) species (Diptera: Psychodidae) in the Awash Valley, northeastern Ethiopia. Trans R Soc Trop Med Hyg 98:64–70
Kaya A, Kıraç A (2016) Vulnerabılıty assessment of Syrıan refugees ın Istanbul. Support to Life. https://pdfs.semanticscholar.org/d741/172235b92bcd44801ab4e743c59d7826dc6c.pdf?_ga=2.134267569.1945614679.1573032697-1076109234.1563615396
Edge S, Newbold B (2013) Discrimination and the health of immigrants and refugees: exploring Canada’s evidence base and directions for future research in newcomer receiving countries. J Immigr Minor Health 15:141–148. https://doi.org/10.1007/s10903-012-9640-4
Reithinger R, Aadil K, Kolaczinski J, Mohsen M, Hami S (2005) Social impact of leishmaniasis, Afghanistan. Emerg Infect Dis 11:634–636. https://doi.org/10.3201/eid1104.040945
Acknowledgements
We would like to thank ManisaCelal Bayar University Parasite Bank. Turkish Society of Microbiology Study Group for Infections Related to Migration and Travel contributed to this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this paper certify that they have NO affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Özbilgin, A., Gencoglan, G., Tunali, V. et al. Refugees at the Crossroads of Continents: A Molecular Approach for Cutaneous Leishmaniasis Among Refugees in Turkey. Acta Parasit. 65, 136–143 (2020). https://doi.org/10.2478/s11686-019-00139-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.2478/s11686-019-00139-4