Abstract
Background: Comparative evidence for second-step treatment strategies in severe depression is scarce. Up-titrating a well tolerated selective serotonin reuptake inhibitor (SSRI) versus switching to a serotonin norepinephrine reuptake inhibitor (SNRI) after initial SSRI non-response are possible treatment options. It is often unclear whether relevant tolerability and efficacy differences exist between SSRI up-titration versus switch to an SNRI.
Objective: The objective of this study was to evaluate tolerability and efficacy of up-titration of escitalopram versus switch to duloxetine in patients who failed to respond to escitalopram 10mg/day.
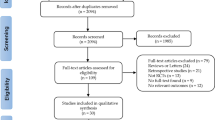
Methods: This was an active-controlled, parallel-group, double-blind, randomized study in a general community comparing escitalopram and duloxetine in patients with severe depression; patients who did not respond (<50% Montgomery-Åsberg Depression Rating Scale [MADRS] improvement) to 2 weeks of single-blind escitalopram 10 mg/day during the lead-in period were randomized to 8 weeks of double-blind treatment. 571 male and female outpatients aged 18–65 years with severe depression (MADRS total score ≥30) participated in the study and received at least one dose of escitalopram 10 mg/day in the single-blind lead-in phase. During the double-blind randomized phase, 474 patients who did not respond to lead-in escitalopram were randomized and received treatment with escitalopram 20 mg (n = 229) or duloxetine 60 mg (n=245). Treatment was single-blind escitalopram 10 mg/day during a 2-week lead-in followed by 8-week double-blind escitalopram 20 mg/day or duloxetine 60 mg/day. The main outcome measure was time to all-cause premature study discontinuation.
Results: There was no difference in time to all-cause discontinuation between groups (hazard ratio escitalopram/duloxetine = 0.95 [95% CI 0.64, 1.41]; p = 0.727). Treatment with escitalopram compared with duloxetine resulted in significant improvement in MADRS total score at the end of week 8 (least squares mean difference [LSMD] = −1.87 [95% CI −3.60, −0.14]; p = 0.034) using last observation carried forward (LOCF) analysis. Significantly more escitalopram (54%) than duloxetine (42%) patients achieved remission (MADRS <-10) by week 8 (p = 0.013). Adverse events were similar between the two treatment groups.
Conclusion: In initial non-responders to escitalopram 10 mg/day, dose escalation to 20 mg/day provided better efficacy than switching to duloxetine 60 mg/day, while discontinuations for any reasons and adverse events were similar.
Clinical Trial Registration: Registered at ClinicalTrials.gov as NCT00384436.









Similar content being viewed by others
References
Nemeroff The burden of severe depression: a review of diagnostic challenges and treatment alternatives. J Psychiatr Res 2007 Apr-Jun; 41 (3–4): 189-206
Thase ME. Treatment of severe depression. J Clin Psychiatry 2000; 61 Suppl. 1: 17–25
Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry 2006 Nov; 163(11): 1905–17
Kurian Greer TL, Trivedi MH. Strategies to enhance the therapeutic efficacy of antidepressants: targeting residual symptoms. Expert Rev Neurother 2009 Jul; 9(7): 975–84
Thase ME. Are SNRIs more effective than SSRIs? A review of the current state of the controversy. Psychopharmacol Bull 2008; 41(2): 58–85
Rush AJ, Warden D, Wisniewski SR, et al. STAR*D: revising conventional wisdom. CNS Drugs 2009 Aug 1; 23(8): 627–47
Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 12 new-generation antidepressants: a multiple-treatments meta-analysis. Lancet 2009 Feb 28; 373(9665): 746–58
Fredman SJ, Fava M, Kienke AS, et al. Partial response, nonresponse, and relapse with selective serotonin reuptake inhibitors in major depression: a survey of current “next-step” practices. J Clin Psychiatry 2000 Jun; 61(6): 403–8
Wade A, Friis Andersen H. The onset of effect for escitalopram and its relevance for the clinical management of depression. Curr Med Res Opin 2006 Nov; 22(11): 2101–10
Henkel V, Seemuller F, Obermeier M, et al. Does early improvement triggered by antidepressants predict response/remission? Analysis of data from a naturalistic study on a large sample of inpatients with major depression. J Affect Disord 2009 Jun; 115(3): 439–49
Khan A, Bose A, Alexopoulos GS, et al. Double-blind comparison of escitalopram and duloxetine in the acute treatment of major depressive disorder. Clin Drug Investig 2007; 27(7): 481–92
Nierenberg AA, Greist JH, Mallinckrodt CH, et al. Duloxetine versus escitalopram and placebo in the treatment of patients with major depressive disorder: onset of antidepressant action, a non-inferiority study. Curr Med Res Opin 2007 Feb; 23(2): 401–16
Pigott TA, Prakash A, Arnold LM, et al. Duloxetine versus escitalopram and placebo: an 8-month, double-blind trial in patients with major depressive disorder. Curr Med Res Opin 2007 Jun; 23(6): 1303–18
Wade A, Gembert K, Florea I. A comparative study of the efficacy of acute and continuation treatment with escitalopram versus duloxetine in patients with major depressive disorder. Curr Med Res Opin 2007 Jul; 23(7): 1605–14
Wohlreich MM, Mallinckrodt CH, Watkin JG, et al. Immediate switching of antidepressant therapy: results from a clinical trial of duloxetine. Ann Clin Psychiatry 2005 Oct–Dec; 17(4): 259–68
Forest Laboratories Clinical Trial Registry Web site. MD-39: Fixed dose comparison of escitalopram to an active comparator in severely depressed patients [online] http://www.forestclinicaltrials.com/CTR/CTRController/CTRViewPdf?_file_id=scsr/SCSR_SCT-MD-39_final.pdf [Accessed 2012 Jan 3]
Montgomery SA, Åsberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry 1979 Apr; 134: 382–9
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed, text revision. Washington, DC: American Psychiatric Association, 2000
Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998; 59 Suppl. 20: 22–33
Guy W. The clinician global severity and impression scales. ECDEU assessment manual for psychopharmacology. Rockville (MD): National Institute of Mental Health, 1976; 218–2. DHEW Publication No. 76–338
Cymbalta [package insert]. Indianapolis (IN): Eli Lilly and Company; 2011
Trivedi MH, Rush AJ, Ibrahim HM, et al. The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: a psychometric evaluation. Psychol Med 2004 Jan; 34(1): 73–82
Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol 1959; 32(1): 50–5
Endicott J, Nee J, Harrison W, et al. Quality of Life Enjoyment and Satisfaction Questionnaire: a new measure. Psy-chopharmacol Bull 1993; 29(2): 321–6
Wisniewski SR, Rush AJ, Balasubramani GK, et al. Self-rated global measure of the frequency, intensity, and burden of side effects. J Psychiatr Pract 2006 Mar; 12(2): 71–9
Boulenger JP, Huusom AK, Florea I, et al. A comparative study of the efficacy of long-term treatment with escitalopram and paroxetine in severely depressed patients. Curr Med Res Opin 2006 Jul; 22(7): 1331–41
Moore N, Verdoux H, Fantino B. Prospective, multicentre, randomized, double-blind study of the efficacy of escitalopram versus citalopram in outpatient treatment of major depressive disorder. Int Clin Psychopharmacol 2005 May; 20(3): 131–7
Kennedy SH, Andersen HF, Lam RW. Efficacy of escitalopram in the treatment of major depressive disorder compared with conventional selective serotonin reuptake inhibitors and venlafaxine XR: a meta-analysis. J Psychiatry Neurosci 2006 Mar; 31(2): 122–31
Lam RW, Andersen HF, Wade AG. Escitalopram and duloxetine in the treatment of major depressive disorder: a pooled analysis of two trials. Int Clin Psychopharmacol 2008 Jul; 23(4): 181–7
Kornstein SG, Li D, Mao Y, et al. Escitalopram versus SNRI antidepressants in the acute treatment of major depressive disorder: integrative analysis of four double-blind, randomized clinical trials. CNS Spectr 2009 Jun; 14(6): 326–33
Bech P, Andersen HF, Wade A. Effective dose of escitalopram in moderate versus severe DSM-IV major depression. Pharmacopsychiatry 2006 Jul; 39(4): 128–34
Posternak MA, Zimmerman M. Is there a delay in the anti-depressant effect? A meta-analysis. J Clin Psychiatry 2005 Feb; 66(2): 148–58
Lepola UM, Loft H, Reines EH. Escitalopram (10–20mg/day) is effective and well tolerated in a placebo-controlled study in depression in primary care. Int Clin Psychopharmacol 2003 Jul; 18(4): 211–7
Burke WJ, Gergel I, Bose A. Fixed-dose trial of the single isomer SSRI escitalopram in depressed outpatients. J Clin Psychiatry 2002 Apr; 63(4): 331–6
Wade A, Michael Lemming O, Bang Hedegaard K. Escitalopram 10mg/day is effective and well tolerated in a pla-cebo-controlled study in depression in primary care. Int Clin Psychopharmacol 2002 May; 17(3): 95–102
Acknowledgements
This study was supported by Forest Laboratories, Inc. Forest Laboratories, Inc. was involved in the design and conduct of the study, and collection, management, analysis and interpretation of data. Forest Laboratories, Inc. was involved in the preparation, review and approval of the manuscript.
Joyce Tsai was employed by Forest Research Institute at the time of the study.
We would like to acknowledge Heather Dworak, at Forest Research Institute at the time of the study, for her contribution to the conduct of this study and Yongcai Mao of Forest Research Institute for his contribution to the statistical analysis of this study. Writing assistance and editorial support for the preparation of this manuscript were provided by Carol Dyer of Prescott Medical Communications Group.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bose, A., Tsai, J. & Li, D. Early Non-Response in Patients with Severe Depression. Clin Drug Investig 32, 373–385 (2012). https://doi.org/10.2165/11631890-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11631890-000000000-00000