Abstract
Background: Pharmacokinetic studies of antiretroviral drugs are often conducted in adult healthy subjects, and the results are extrapolated to HIV/AIDS patients. HIV/AIDS, however, is known to cause morphological and physiological changes that may alter the pharmacokinetics of antiretroviral drugs. We examined the effect of HIV/AIDS on the pharmacokinetics of efavirenz in Ugandans.
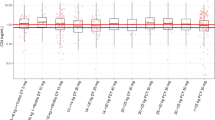
Methods: After a first oral dose of efavirenz 600 mg in treatment-naïve HIV-infected patients, blood samples were collected at nine time points up to 24 hours. The plasma-concentration time data from these patients were merged with previously reported data from adult healthy subjects. Population pharmacokinetic models were fitted to the data, using NONMEM VI software. Covariate analyses were performed to estimate the effects of HIV/AIDS disease, demographic characteristics (sex, bodyweight, age), biochemical variables (serum creatinine, urea, alanine aminotransferase) and pharmacogenetic variation in cytochrome P450 (CYP) 2B6, CYP3A5 and adenosine triphosphate-binding cassette, sub-family B, member 1 (ABCB1) on the population pharmacokinetic parameters.
Results: Efavirenz plasma concentration-time data obtained from 29 HIV-1-infected, treatment-naïve patients were merged with previously reported data from 32 adult healthy subjects. The model identified sex and HIV/AIDS disease as statistically significant categorical predictors of efavirenz pharmacokinetics. Females were predicted to have a 2-fold higher volume of distribution of the peripheral compartment after oral administration (V2/F) than males (95% CI 1.53,2.63), while HIV/AIDS patients were found to have 30% lower relative bioavailability (95% CI 18.7, 40.7) than healthy subjects. The increased V2/F in females resulted in a 2-fold longer elimination half-life than in males.
Conclusion: On the basis of the findings of this analysis, we conclude that, apart from bodyweight-based differences, both HIV/AIDS disease and sex affect efavirenz pharmacokinetics in Ugandans. HIV/AIDS disease is associated with reduced relative bioavailability of efavirenz. We recommend that findings from healthy subject studies be confirmed in HIV/AIDS patients and that caution be applied in direct extrapolation of exposure data to the target patient population.







Similar content being viewed by others
References
Abdel-Razzak Z, Loyer P, Fautrel A, et al. Cytokines down-regulate expression of major cytochrome P-450 enzymes in adult human hepatocytes in primary culture. Mol Pharmacol 1993; 44: 707–15
Chow HH, Tang Y, Li P, et al. The effect of chronic retrovirus infection and immune dysfunction on the P-450-mediated activation of acetaminophen in mouse liver microsomes. Biopharm Drug Dispos 1998; 19: 9–15
Welage LS, Carver PL, Revankar S, et al. Alterations in gastric acidity in patients infected with human immunodeficiency virus. Clin Infect Dis 1995; 21: 1431–8
Sadler BM, Gillotin C, Lou Y, et al. In vivo effect of alpha (1)-acid glycoprotein on pharmacokinetics of amprenavir, a human immunodeficiency virus protease inhibitor. Antimicrob Agents Chemother 2001; 45: 852–6
Laine L, Garcia F, McGilligan K, et al. Protein-losing enteropathy and hypoalbuminemia in AIDS. AIDS 1993; 7: 837–40
Sabin CA, Griffioen A, Yee TT, et al. Markers of HIV-1 disease progression in individuals with haemophilia coinfected with hepatitis C virus: a longitudinal study. Lancet 2002; 360: 1546–51
Brenchley JM, Douek DC. HIV infection and the gastrointestinal immune system. Mucosal Immunol 2008; 1: 23–30
Cummins AG, LaBrooy JT, Stanley DP, et al. Quantitative histological study of enteropathy associated with HIV infection. Gut 1990; 31: 317–21
Dickinson L, Khoo S, Back D. Differences in the pharmacokinetics of protease inhibitors between healthy volunteers and HIV-infected persons. Curr Opin HIV AIDS 2008; 3: 296–305
Dickinson L, Boffito M, Back D, et al. Population pharmacokinetics of ritonavir-boosted atazanavir in HIV-infected patients and healthy volunteers. J Antimicrob Chemother 2009; 63: 1233–43
Ward BA, Gorski JC, Jones DR, et al. The cytochrome P450 2B6 (CYP2B6) is the main catalyst of efavirenz primary and secondary metabolism: implication for HIV/AIDS therapy and utility of efavirenz as a substrate marker of CYP2B6 catalytic activity. J Pharmacol Exp Ther 2003; 306: 287–300
Burger D, van der Heiden I, la Porte C, et al. Interpatient variability in the pharmacokinetics of the HIV non-nucleoside reverse transcriptase inhibitor efavirenz: the effect of gender, race, and CYP2B6 polymorphism. Br J Clin Pharmacol 2006; 61: 148–54
Desta Z, Saussele T, Ward B, et al. Impact of CYP2B6 polymorphism on hepatic efavirenz metabolism in vitro. Pharmacogenomics 2007; 8: 547–58
Mukonzo JK, Roshammar D, Waako P, et al. A novel polymorphism in ABCB1 gene, CYP2B6*6 and sex predict single-dose efavirenz population pharmacokinetics in Ugandans. Br J Clin Pharmacol 2009; 68: 690–9
Haas DW, Smeaton LM, Shafer RW, et al. Pharmacogenetics of long-term responses to antiretroviral regimens containing efavirenz and/or nelfinavir: an Adult AIDS Clinical Trials Group study. J Infect Dis 2005; 192: 1931–42
Beal SL, Boeckmann AJ, Shiner LB, editors. NONMEM user’s guides. Ellicot City (MD): Icon Development Solutions, 1986–2006
Wilkins JJ. NONMEMory: a run management tool for NONMEM. Comput Methods Programs Biomed 2005; 78: 259–67
Jonsson EN, Karlsson MO. Xpose: an S-Plus based population pharmacokinetic/pharmacodynamic model building aid for NONMEM. Comput Methods Programs Biomed 1999; 58: 51–64
Lindbom L, Pihlgren P, Jonsson EN. PsN-Toolkit: a collection of computer intensive statistical methods for non-linear mixed effect modeling using NONMEM. Comput Methods Programs Biomed 2005; 79: 241–57
Anderson BJ, Holford NH. Mechanism-based concepts of size and maturity in pharmacokinetics. Annu Rev Pharmacol Toxicol 2008; 48: 303–32
Savic RM, Jonker DM, Kerbusch T, et al. Implementation of a transit compartment model for describing drug absorption in pharmacokinetic studies. J Pharmacokinet Pharmacodyn 2007; 34: 711–26
Wilkins JJ, Savic RM, Karlsson MO, et al. Population pharmacokinetics of rifampin in pulmonary tuberculosis patients, including a semimechanistic model to describe variable absorption. Antimicrob Agents Chemother 2008; 52: 2138–48
Lake-Bakaar G, Tom W, Lake-Bakaar D, et al. Gastropathy and ketoconazole malabsorption in the acquired immunodeficiency syndrome (AIDS). Ann Intern Med 1988; 109:471–3
Lake-Bakaar G, Elsakr M, Hagag N, et al. Changes in parietal cell structure and function in HIV disease. Dig Dis Sci 1996; 41: 1398–408
Gupta S, Gollapudi S. P-glycoprotein (MDR 1 gene product) in cells of the immune system: its possible physiologic role and alteration in aging and human immunodeficiency virus-1 (HIV-1) infection. J Clin Immunol 1993; 13: 289–301
Stormer E, von Moltke LL, Perloff MD, et al. Differential modulation of P-glycoprotein expression and activity by non-nucleoside HIV-1 reverse transcriptase inhibitors in cell culture. Pharm Res 2002; 19: 1038–45
Haas DW, Ribaudo HJ, Kim RB, et al. Pharmacogenetics of efavirenz and central nervous system side effects: an Adult AIDS Clinical Trials Group study. Aids 2004; 18: 2391–400
Elens L, Vandercam B, Yombi JC, et al. Influence of host genetic factors on efavirenz plasma and intracellular pharmacokinetics in HIV-1-infected patients. Pharmacogenomics 2010; 11: 1223–34
Sankatsing SU, Beijnen JH, Schinkel AH, et al. P glycoprotein in human immunodeficiency virus type 1 infection and therapy. Antimicrob Agents Chemother 2004; 48: 1073–81
Aitken AE, Morgan ET. Gene-specific effects of inflammatory cytokines on cytochrome P450 2C, 2B6 and 3A4 mRNA levels in human hepatocytes. Drug Metab Dispos 2007; 35: 1687–93
Ngaimisi E, Mugusi S, Minzi OM, et al. Long-term efavirenz autoinduction and its effect on plasma exposure in HIV patients. Clin Pharmacol Ther 2010; 88: 676–84
Acknowledgements
Jackson K. Mukonzo and Sarah Nanzigu contributed equally to this work.
This study was funded by Swedish International Development Cooperation Agency Department for Research Cooperation (SIDA/SAREC) grant nos. SWE 2004-098, HIV-2006-031 and SWE 2007-270; the Makerere University-Karolinska Institutet research collaboration; and European and Developing Countries Clinical Trials Partnership (EDCTP) grant no. CT.2005.32030.001.
Daniel Röshammar is an employee of AstraZeneca. However, this work was not funded or supported by any pharmaceutical company. All authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Additional information
An erratum to this article is available at http://dx.doi.org/10.2165/11595800-000000000-00000.
Rights and permissions
About this article
Cite this article
Mukonzo, J.K., Nanzigu, S., Rekić, D. et al. HIV/AIDS Patients Display Lower Relative Bioavailability of Efavirenz than Healthy Subjects. Clin Pharmacokinet 50, 531–540 (2011). https://doi.org/10.2165/11592660-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11592660-000000000-00000